Non-invasive ventilation
The introduction and widespread use of non-invasive ventilation (NIV) has revolutionised the management and survival of patients with an acidotic exacerbation of chronic obstructive pulmonary disease (COPD). Indeed, it is difficult to justify admitting patients with an exacerbation of COPD to hospitals where NIV is not readily available. A close fitting facemask or nose mask connected to a portable ventilator facilitates a non-invasive method of providing respiratory support to a spontaneously breathing patient. The mask can be removed easily, allowing patients to communicate, eat, drink, and take nebulised and oral drugs.
Figure 1.
Non-invasive ventilation can be given using a full facemask or nose mask
How non-invasive ventilation works
NIV provides a two level form of respiratory support, supplying inspiratory and expiratory positive airways pressure.
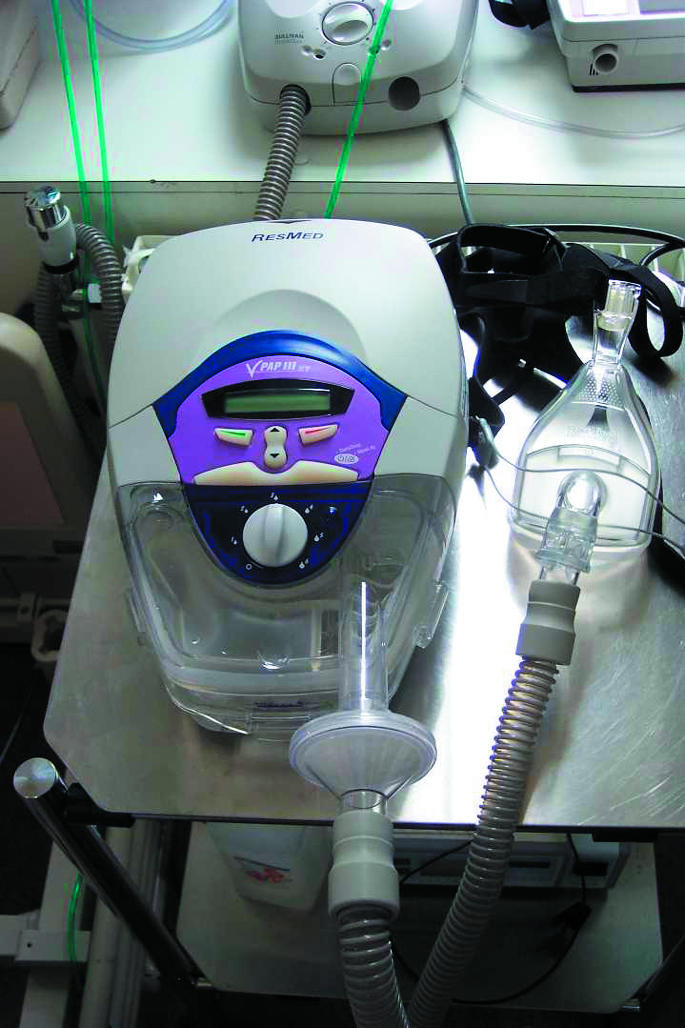
Figure 2.

Non-invasive ventilation can be used in hospital wards and in high dependency and intensive care units
Inspiratory positive airways pressure, which is usually titrated up to 15-20 cm H2O, helps offload tiring respiratory muscles and reduce the work of breathing, improves alveolar ventilation and oxygenation, and increases elimination of CO2.
Table 1.
Advantages of non-invasive ventilation over invasive mechanical ventilation
| • Patients can eat and drink |
| • Patients can communicate and make decisions about management |
| • A physiological cough is maintained |
| • Physiological warming and humidification occurs |
| • No sedatives are required |
| • Reduced risk of ventilator associated pneumonia |
| • Less expensive, and intensive care bed not necessarily required |
| • Allows intermittent use, which facilitates weaning |
Expiratory positive airways pressure, usually at 4-6 cm H2O, helps “splint open” the airway and flushes CO2 from the mask. It also reduces the work of breathing by overcoming intrinsic positive end expiratory pressure, thereby reducing atelectasis and increasing the end tidal volume.
Oxygen is introduced either through a port in the facemask or through a more proximal channel in the ventilator system. It is not usually necessary to deliver humidified oxygen, but humidifiers can be added to the circuit.
When to use non-invasive ventilation in COPD
NIV is particularly successful in patients with hypercapnic respiratory failure (especially in those with an arterial blood pH of 7.25-7.35). It can also be used as a therapeutic trial before proceeding to mechanical ventilation or when more invasive ventilatory support is inappropriate. In the latter circumstance, NIV is therefore considered the “ceiling of treatment.”
Studies with various end points—such as mortality, need for intubation, arterial blood gases, and cost effectiveness—have consistently shown significant benefits with NIV. For example, a meta-analysis of eight randomised controlled trials evaluated effects of NIV in patients admitted with an exacerbation of COPD with an arterial CO2 pressure (PaCO2) of > 6 kPa. Compared with standard treatment alone, concomitant NIV reduced mortality, need for intubation, likelihood of treatment failure, and complication rate. It also produced improvements in blood pH, PaCO2, and respiratory rate within an hour and resulted in a shorter stay in hospital.
This is the 10th in a series of 12 articles
Setting
NIV can be used in hospital wards and in high dependency and intensive care units. It can be started in accident and emergency departments, but in many such cases, patients will not have had sufficient time to respond to conventional treatment. The exact setting is less important than the availability of experienced nurses, physiotherapists, and medical staff to start treatment, monitor progress, and troubleshoot. In the treatment of COPD, there is little to guide choice of ventilator other than familiarity, cost, and local preference. If NIV is used for hypoxic respiratory failure the ventilator unit needs an intrinsic blender to ensure delivery of high fractions of inspired oxygen. Intensive care ventilators are often difficult to use non-invasively as they are poorly tolerant of leaks and alarm readily.
Figure 3.
A variety of face masks sizes or, less commonly, nose masks are available for use with NIV
How to use non-invasive ventilation
Before starting NIV, decide whether the patient is a suitable candidate for invasive mechanical ventilation and document the decision. Also discuss with the patient and his or her family whether they would wish further respiratory support if NIV proves unsuccessful.
Figure 4.

Patients receiving NIV can easily become dehydrated and undernourished; adequate hydration and nutrition should not be forgotten in the overall management
Explain what you are about to do. Providing the clinical condition permits, show the patient the ventilator, facemask, and tubing. Choose an appropriately sized facemask (sizing rings are usually provided by the manufacturer). Nasal masks are more comfortable, but require patients to breathe through their nose. Most patients with acute exacerbations of COPD breathe through their mouth, and full facemasks are therefore preferable. It is useful if the mask is firstly placed on the patient's face for several minutes before securing it with straps.
Table 2.
Factors to consider in deciding a patient's suitability for invasive mechanical ventilation
| • Presence of concomitant medical conditions |
| • Premorbid functional status |
| • Severity of existing airflow obstruction |
| • Presence of potentially reversible precipitant (such as pneumonia or pneumothorax) |
| • Patient and family wishes |
Set the oxygen to an appropriate initial flow rate (typically 1-2 l/min) and titrate it upwards to maintain a saturation of at least 90%. Set both inspiratory and expiratory positive airways pressures, usually starting at 10 and 4 cm H2O respectively. The inspiratory pressure can then be titrated up to 15-20 cm H2Oor to the maximum pressure comfortably tolerated by the patient. Depending on the type of ventilator, other parameters may be set, such as the sensitivity of the inspiratory and expiratory triggers and maximum inspiratory and expiratory times. These may need adjustment to maximise synchrony between the ventilator and the patient's efforts. Good synchrony makes for efficient ventilation and greater comfort for the patient. For some patients with shallow breathing or low respiratory rates, it may be necessary to programme the ventilator to deliver a minimum number of breaths per minute.
Monitoring non-invasive ventilation
Irrespective of PaO2 or PaCO2, the arterial blood pH is a reliable marker of severity in exacerbations of COPD and is closely linked to mortality and need for intubation. As well as regularly recording pulse, blood pressure, and respiratory rate, continuously monitor oxygen saturation.
Check arterial blood gases one hour after starting NIV; an improvement in blood pH or PaCO2 and reduction in respiratory rate are good prognostic signs. If no improvement occurs, check that the patient is wearing the mask, that it is comfortable without excessive leak, and that the ventilator is in synchrony with the patient's respiratory effort, and then consider adjusting the ventilator settings (such as inspiratory pressure or oxygen flow rate). Blood gases should be rechecked within four hours of a change in setting, or earlier in the event of a clinical deterioration.
Weaning from NIV is rarely a problem, as patients normally “auto wean” by progressively decreasing their use after a few days.
Other measures
Institute maximal drug treatment—such as nebulised bronchodilators, corticosteroids, and antibiotics—in patients starting NIV. Check whether patients are using sedative drugs such as benzodiazepines and opiates: if so, these may require pharmacological reversal, especially if the respiratory rate is low. Keep patients adequately hydrated and maintain an adequate calorific intake.
Before the introduction of NIV, doxapram was often used as a respiratory stimulant. Few studies have made direct comparisons with NIV, but doxapram has only limited ability to improve blood gas tensions. Moreover, a high incidence of adverse effects means that it is often poorly tolerated. Its role alongside NIV is not established, and it should not be used except under specialist supervision. However, it may be used as a temporising measure if NIV is not immediately available or cannot be tolerated.
Figure 5.

Deciding when to abandon NIV and start invasive mechanical ventilation is often difficult
Problems with non-invasive ventilation
Most patients tolerate NIV without serious problems, but some have difficulty “breathing with the machine.” The facemask can cause problems such as claustrophobia, facial sores, and persistent air leaks. There are few absolute contraindications to NIV, and all patients' suitability should be assessed on an individual basis. With moribund patients, however, consider whether either intubation or a palliative approach might be more appropriate. Patients who recover from an exacerbation treated with NIV are at high risk of a future exacerbation and should be asked whether they would wish ventilatory support in the future.
Table 3.
Relative contraindications to using non-invasive ventilation
| • Orofacial burns |
| • Recent orofacial surgery |
| • Bowel obstruction |
| • Decreased consciousness |
| • Copious respiratory secretions |
| • Cardiovascular instability |
| • Untreated pneumothorax |
| • Agitation |
| • Persistent vomiting |
| • Unstable upper airway |
| • Severe respiratory acidosis |
Domiciliary non-invasive ventilation
The role of domiciliary NIV in COPD is controversial. Unlike patients with neuromuscular disorders, patients with COPD tend to be poorly compliant once at home. Randomised controlled trials have failed to show either a definite survival advantage or improvement in quality of life. However, for hypoxic patients with COPD who develop hypercapnia or acidosis while receiving long term oxygen therapy, domiciliary nocturnal NIV may be useful. It can also be useful for patients with hypercapnic respiratory failure who are frequently admitted to hospital with exacerbations associated with acidosis.
Mechanical ventilation
Invasive mechanical ventilation should be considered in patients whose pH, PaCO2, and respiratory rate have deteriorated or failed to improve within four hours of initiation of NIV. NIV is less likely to be successful in such patients, or in those with severe acidosis such as an initial pH < 7.26. Moreover, patients who remain acidotic 48 hours after starting treatment with NIV tend to have a poor prognosis. Such patients have a higher mortality if NIV is continued than if mechanical ventilation is initiated, and the latter treatment should therefore be considered.
Long term survival in patients with COPD who require mechanical ventilation is generally lower than in those who require NIV alone. However, failure of NIV should not be used as a reason to decline invasive mechanical ventilation and does not imply that these patients will be difficult to wean. For patients who cannot be weaned on to NIV within 48-72 hours of starting mechanical ventilation, early fashioning of a tracheostomy may facilitate weaning and reduce the time spent in intensive care.
The ABC of chronic obstructive pulmonary disease is edited by Graeme P Currie. The series will be published as a book by Blackwell Publishing in autumn 2006.
Competing interests: GPC has received funding for attending international conferences and honorariums for giving talks from pharmaceutical companies GlaxoSmithKline, Pfizer, and AstraZeneca.
The figure of invasive mechanical ventilation is supplied by Custom Medical Stock and the Science Photo Library.
Further reading and resources
- • Non-invasive ventilation in acute respiratory failure. Thorax 2002; 57: 192-211 [DOI] [PMC free article] [PubMed] [Google Scholar]
- • Plant PK, Owen JL, Elliott MW. Early use of non-invasive ventilation for acute exacerbations of chronic obstructive pulmonary disease on general respiratory wards: a multicentre randomised controlled trial. Lancet 2000;355: 1931-5 [DOI] [PubMed] [Google Scholar]
- • Lightowler JV, Wedzicha JA, Elliott MW, Ram FS. Non-invasive positive pressure ventilation to treat respiratory failure resulting from exacerbations of chronic obstructive pulmonary disease: Cochrane systematic review and meta-analysis. BMJ 2003;326: 185. [DOI] [PMC free article] [PubMed] [Google Scholar]



