Abstract
Bacillus anthracis is a bacterial pathogen of great importance, both historically and in the present. This study presents data collected from several investigations and indicates that B. anthracis virulence is associated with the clonality and virulence of plasmids pXO1 and pXO2. Guinea pigs vaccinated with Anthrax Vaccine Adsorbed were challenged with 20 B. anthracis isolates representative of worldwide genetic diversity. These same isolates were characterized with respect to plasmid copy number by using a novel method of quantitative PCR developed for rapid and efficient detection of B. anthracis from environmental samples. We found that the copy numbers for both pXO1 and pXO2 differed from those in previously published reports. By combining the data on survival, plasmid copy numbers, and clonality, we developed a model predicting virulence. This model was validated by using a randomly chosen set of 12 additional B. anthracis isolates. Results from this study will be helpful in future efforts to elucidate the basis for variation in the virulence of this important pathogen.
The etiologic agent of anthrax, Bacillus anthracis, is a gram-positive, rod-shaped, spore-forming bacterium. The disease primarily affects ungulate herbivores, occasionally affects carnivores, and less frequently affects humans (30). Anthrax is a disease well documented throughout human history, with suggestive reports in the Bible and Sanskrit manuscripts (5). Koch, Pasteur, and others revolutionized the field of microbiology with their studies using B. anthracis as a model organism (27). Though anthrax has not been eradicated, the development of effective animal and human vaccines has reduced its importance for humans and animals in developed countries over the last century. Recently, however, anthrax research has become increasingly important due to this pathogen's central role in biological warfare and biological terrorism (14). The importance of the disease in humans has been underscored by the bioterrorism events of October 2001 in the United States. Now more than ever, there is a need for rapid, reliable, and highly specific detection assays.
Identification and detection systems based on real-time quantitative PCR (QPCR) have been described for several bacteria, including B. anthracis (1, 2, 13, 22). These techniques are easy to design, simple to carry out, and commonly applied to monitor and detect the microbial status of sample specimens. With proper design and careful application, diagnostic QPCR systems can be applied to reliably estimate and, in the present study, absolutely enumerate target organisms as well as nucleic acid elements, such as plasmids, within those organisms (20).
The virulence of B. anthracis has been associated with two megaplasmids, pXO1 and pXO2 (30). Plasmid pXO2 (60 MDa) carries the genes required for synthesis of an antiphagocytic poly-d-glutamic acid capsule facilitating host immune system evasion (9, 16, 21, 31, 32, 35). The 110-MDa plasmid pXO1 is required for synthesis of the three anthrax toxin proteins, edema factor (EF), lethal factor (LF), and protective antigen (PA) (31). These proteins act in binary combinations to produce the two anthrax toxins: edema toxin (PA and EF) and lethal toxin (PA and LF) (17). Although the roles of the capsule and toxin in disease pathogenesis have been well characterized, the copy numbers of these plasmids have not been investigated (7, 18). A recently published study has alluded to the copy number of each plasmid per cell of the Ames isolate of B. anthracis (26). While differences have been observed in the virulence of various isolates of B. anthracis, only a portion of these differences can be attributed to plasmid-related effects (35).
Previous studies have shown that the virulence of B. anthracis can differ among isolates or strains (6, 8, 19). Some variation in virulence can be related to the presence or absence of the plasmids. Isolates lacking either the pX01 or pX02 plasmid are considered either avirulent or significantly attenuated (23, 33). However, this does not explain the variation in virulence observed in studies comparing fully virulent isolates such as the Ames and Vollum 1B strains (11, 12). Explanations for these differences in virulence have never been fully substantiated. In a challenge study using guinea pigs vaccinated with the human vaccine currently licensed in the United States, anthrax vaccine adsorbed (AVA), 20 genetically diverse B. anthracis isolates, as defined by multilocus variable-number tandem repeat analysis (MLVA), yielded survival rates ranging from 0 to 100% (results presented below). Several possible mechanisms that may be responsible for the modulation of virulence exist, including the copy number of plasmids per cell and transcription regulation of the anthrax toxins and capsule, and additional variation may be mediated by the generation time and germination efficiency. These factors are likely to be associated with mutations that could be clonally heritable.
In this study, we show that B. anthracis virulence is related to clonality and pXO1 and pXO2 copy number. We modeled the percentage of survival of guinea pigs vaccinated with AVA and challenged by 20 genetically diverse B. anthracis isolates as defined by the MLVA. Absolute QPCR analysis was used to determine the plasmid copy number present per cell (pXO1 and pXO2) for each of the isolates. Our model describing the virulence of B. anthracis isolates in AVA-vaccinated guinea pigs by using MLVA cluster association, clonality, and plasmid copy number was then verified by using a randomly chosen group of 12 isolates.
MATERIALS AND METHODS
Bacterial isolates.
A total of 36 isolates of B. anthracis were included in this study (Table 1). All of these isolates have been previously genotyped using MLVA (14). Initially, 20 isolates were chosen for animal challenge studies and plasmid copy number characterization based on their representation of genetic diversity from a worldwide collection. Genetic diversity was determined by MLVA cluster assignment and was based on genotypic allele patterns described previously for eight variable-number tandem repeat loci (15). The isolates used in this study are representative of all seven major MLVA clusters. An additional 12 isolates that were previously genetically characterized using MLVA for the purpose of model validation were later chosen at random from the worldwide collection.
TABLE 1.
B. anthracis isolates by country and cluster, the survival of AVA-vaccinated guinea pigs, and the calculated number of plasmids pXO1 and pXO2
| Isolate | Country or strain | Cluster | % Survival | No. of pXO1 (rpXO1) | No. of pXO2 (rpXO2) |
|---|---|---|---|---|---|
| Model isolate set | |||||
| 1 | China | A3b | 0 | 185 (30.9) | 9 (1.5) |
| 2 | Australia | A3a | 0 | 121 (20.2) | 32 (5.4) |
| 3 | Namibia | A3a | 19 | 242 (40.3) | 5 (0.9) |
| 4 | Ames | A3b | 38 | 65 (10.8) | 2 (0.3) |
| 5 | Germany | A3a | 25 | 113 (18.9) | 5 (0.9) |
| 6 | Turkey | A3a | 31 | 131 (21.8) | 11 (1.8) |
| 7 | France | B2 | 31 | 243 (40.5) | 4 (0.6) |
| 8 | Turkey | A1b | 38 | 236 (39.4) | 27 (4.5) |
| 9 | Pakistan | A2 | 38 | 120 (20.0) | 1 (0.2) |
| 10 | South Africa | B1 | 44 | 66 (11.0) | 2 (0.4) |
| 11 | Zambia | A3a | 44 | 242 (40.4) | 15 (2.5) |
| 12 | Turkey | A1b | 44 | 172 (28.7) | 6 (1.0) |
| 13 | United States | A3a | 44 | 109 (18.1) | 4 (0.7) |
| 14 | South Africa | A3b | 50 | 212 (35.3) | 16 (2.6) |
| 15 | Argentina | A3a | 50 | 104 (17.4) | 7 (1.2) |
| 16 | Mozambique | B1 | 75 | 95 (15.9) | 1 (0.2) |
| 17 | Canada | A1a | 69 | 24 (40.5) | 18 (3.0) |
| 18 | United States | A1a | 69 | 128 (21.4) | 5 (0.8) |
| 19 | Pakistan | A4 | 75 | 191 (31.9) | 14 (2.3) |
| 20 | Vollum | A4 | 94 | 69 (11.5) | 10 (1.6) |
| Test isolate set | |||||
| A | Indonesia | A4 | 13 | 44.4 (7.4) | 4 (0.6) |
| B | South Korea | A3a | 19 | 62 (10.4) | 3 (0.5) |
| C | United States | A3a | 19 | 89 (14.8) | 3 (0.5) |
| D | South Africa | A4 | 25 | 94 (15.6) | 11 (1.9) |
| E | India | A3a | 25 | 33 (5.5) | 2 (0.4) |
| F | United States | A3b | 31 | 44 (7.3) | 2 (0.4) |
| G | Mozambique | B1 | 44 | 86 (14.4) | 10 (1.6) |
| H | Norway | B1 | 44 | 218 (36.3) | 1 (0.2) |
| I | Croatia | B1 | 44 | 49 (8.2) | 3 (0.5) |
| J | Canada | A1a | 50 | 83 (13.9) | 5 (0.9) |
| K | United States | A1a | 50 | 65 (10.8) | 4 (0.7) |
| L | United States | A1a | 56 | 115 (19.2) | 9 (1.5) |
DNA preparation.
DNA from each isolate was obtained by heat lysis of a single colony. The isolates were streaked onto blood agar plates and then incubated at 37°C overnight. A single colony from each plate was transferred into a 0.22 μm-pore-size microcentrifuge tube containing 200 μl of Tris-EDTA (Tris-HCl [pH 8.0], 1.0 mM EDTA). The colony was resuspended by repetitive pipetting. The cellular suspension was heated to 95°C for 20 min and then cooled to room temperature. Cellular debris and any possible contamination by spores were removed by centrifugation at 6,000 × g for 1 min. Centrifugation was conducted inside a biosafety cabinet to contain any aerosols. The supernatant was then transferred to a new tube for storage. One microliter of the lysate contained sufficient template to support a single PCR.
Oligonucleotide design of probes and primers.
The loci sequences used for the QPCR assay primer and probe development on the chromosome and plasmids pXO1 and pXO2 have previously been reported (25, 29). Probe and primer sequences (Table 2) were designed with the Primer Express software program (Perkin-Elmer Applied Biosystems, Foster City, Calif.) according to the manufacturer's instructions. The sequence of the probe was selected based on previously described criteria: predicted cross-reactivity to B. anthracis, the melting temperature of the probe at 69°C, lack of predicted dimer formation with corresponding primers and of self-annealing, a 10°C higher melting temperature of the probe than of the primers, and no stretches of identical nucleotides longer than four and no G at the 5′ end of the probe (10). The fluorescent reporter dye at the 5′ end of the probe was 6-carboxy-fluorescein (FAM); the quencher at the 3′ end was 6-carboxy-tetramethyl-rhodamine (TAMRA).
TABLE 2.
QPCR primers and probes
| Target | Primer | Sequence (5′-3′) | Amplicon size (bp) |
|---|---|---|---|
| pXO1 plasmid (pagA) | BApXO1-PR | 6FAM-TCGAATTACTAAATCCTGCAGATACACTCCCACC-TAMRA | 84 |
| BApXO1-FP | AATGATCAATTGCGACCGTACTT | ||
| BApXO1-RP | TGCATGCGTCGTTCTTTGATA | ||
| pXO2 plasmid (capA) | BApXO2-PR | 6FAM-TACTGCTTCTGTACGTTGTACCCATGTCGC-TAMRA | 131 |
| BApXO2-FP | TCACCAACCATCGTCATCGT | ||
| BApXO2-RP | CGTTATGTAGCAATCGTATTACCTCTTAT | ||
| Chromosome | BA813-PR | 6FAM-AATGCCAGGTTCTATACCGTATCAGCAAGCTATTC-TAMRA | 123 |
| BA813-FP | GGAGGGAATACAGCAAACACAGA | ||
| BA813-RP | TGCAACTGATGGGATTTCTTTCT |
Standards for absolute quantitation.
The standards for absolute quantitation of each primer and probe grouping (pXO1, pXO2, and BA813) were prepared as follows. The PCR-amplified fragment obtained with the primers for each grouping was cloned by using pcDNA3.1/V5-His-TOPO TA and transformed into Escherichia coli TOPO10 (Topo TA cloning kit; Invitrogen, NV Leek, The Netherlands). Purification of the plasmid DNA was carried out with a commercial plasmid DNA isolation kit (Qiagen, Basel, Switzerland). The DNA concentration was determined with a spectrophotometer (Beckman DU-600; Beckman Coulter, Inc., Fullerton, Calif.) and was diluted to 1010 templates/5 μl. Dilutions were made equivalent to 109, 107, 105, 103, 10, and 1 copy of template per 5 μl. For bidirectional DNA sequencing of the insert, the forward primer and reverse primer were used. The nucleotide sequence was determined by using a fluorescence-based automated sequencing system (ABI 377A DNA sequencer) obtained from Microsynth, Balgach, Switzerland. The plasmid insert was sequenced to confirm its identity with B. anthracis.
Test of detection limit for the QPCR assay.
The detection limit of the QPCR assays for B. anthracis was determined by making serial dilutions of overnight cultures of two isolates, isolate 4 and isolate 17 (Table 1), suspended in 0.9% NaCl. The suspension was adjusted to a density corresponding to that of a McFarland 1.0 standard, and from this, serial dilutions were made. Plate counts from each dilution were performed in triplicate on 5% sheep blood agar (Remel). A total of 200 μl of culture from each dilution was heat lysed as described above, and 5 μl was used for the 5′ nuclease assay. Each test was repeated three times.
Specificity of the QPCR assays.
Ten isolates of closely related Bacillus spp. were used to examine the specificity of the QPCR assay. These isolates were B. cereus ATCC 4381 and ATCC 14579, B. subtilis ATCC 6051, B. megaterium ATCC 14580, and four confirmed environmental isolates and two environmental isolates of B. thuringiensis. The environmental isolates were confirmed by 16S rRNA sequencing.
QPCR assay.
Each 25-μl PCR mixture contained 1× TaqMan universal PCR master mix (part number 4304437; Applied Biosystems), 16 μM concentrations of each primer, a 100 nM concentration of fluorogenic probe, and 5 μl of template or plasmid standard. DNA amplification was carried out in MicroAmp optical 96-well reaction plates (part number N801-0560; Applied Biosystems) sealed with MicroAmp optical caps (part number N801-0935; Applied Biosystems). The cycling program consisted of heating for 2 min at 50°C and then 10 min at 95°C followed by a two-stage temperature profile of 95°C for 15 s and 60°C for 1 min, repeated for 40 cycles. Amplification, data acquisition, and data analysis were carried out with an ABI 7700 sequence detector (Applied Biosystems). All QPCR tests were repeated at least three times for each of three individual colonies from each isolate in the study.
Vaccination and challenge.
Hartley guinea pigs (Charles River, Wilmington, Mass.) were vaccinated intramuscularly (i.m.) at 0 and 4 weeks with 0.5 ml of AVA (Bioport, Lansing, Mich.). At 10 weeks after the first vaccination, the guinea pigs were challenged i.m. with 10,000 spores of virulent B. anthracis. Survival was noted for 14 days postchallenge. The research described in this report complied with all relevant federal guidelines and institutional policies and adhered to the Guide for the Care and Use of Laboratory Animals as promulgated by the Institute of Laboratory Animal Resources of the National Research Council (24).
Absolute copy number of loci, statistical analysis, and modeling.
All calculations of means, statistical analyses, and modeling were performed by using SPSS software, version 10.2. The mean absolute copy number of chromosomal loci per cell was determined by back calculation using the total number of cells in a series of dilution trials analyzed with the QPCR assay. Cross-validation of the mean number of plasmid loci per cell was performed using the same methodology. The mean number of cells per trial was determined by using most-probable-number methods and was confirmed with direct spore counts. The ratios of plasmid copies to chromosomal DNA copies were derived by first dividing the total estimated copy number of chromosomal loci determined using the QPCR assay by the mean absolute copy number of chromosomal loci per cell (determined as described above) and then dividing the estimated total copy number of plasmid loci (for each of the two plasmids individually) by the adjusted chromosomal copy number.
After the data set had been assembled and the ratios of plasmid copies to chromosome copies had been calculated, the means of the MLVA clusters were estimated in conjunction with a one-way analysis of variance (ANOVA). The percentage of survival of guinea pigs was modeled by using a univariate general linear model. The dependent variable, percentage of survival, was modeled with two covariates, ratio of pXO1 to chromosome (rpXO1) and ratio of pXO2 to chromosome (rpXO2), and the factor MLVA cluster, which had seven levels corresponding to the seven major MLVA clusters (16). The model examined the main effects of the covariates and factor only. No interactions were examined for the model. Parameter estimates and 95% confidence intervals were calculated for each covariate, factor level, and model intercept term. Statistical significance levels for evaluation of the model were set a priori at an alpha value of 0.05. Post-hoc tests were conducted by using the Student-Newman-Keuls method.
RESULTS
Specificity and sensitivity of the 5′ nuclease assay.
The three unique primer-probe sets designed for the specific identification and target quantification of B. anthracis correctly discriminated all isolates tested. The analytical sensitivity of the QPCR assays was comparable to that of a previously described nested PCR (3). The assay system resolution was sufficient to detect one copy of the standard plasmid. The samples containing no template gave a negative result.
Chromosome, pXO1, and pXO2 loci per bacteria and plasmid ratios.
The average number of chromosomal loci detected per cell was approximately six for all of the isolates examined. The number of loci detected per cell for each of the virulence plasmids, however, varied greatly among the isolates, ranging from 33 (isolate E) to 243 (isolates 7 and 17) for pXO1 and from 1 (isolates 9, 16, and H) to 32 (isolate 2) for pXO2. The plasmid/chromosome loci ratios for each isolate are listed in Table 1.
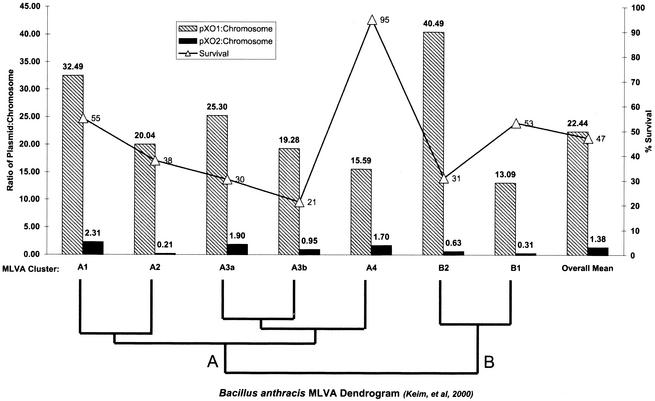
The mean plasmid/chromosome loci ratios calculated over the seven MLVA clusters were significantly different as indicated by the results of an ANOVA (P < 0.05) (Fig. 1). Post-hoc tests indicated that there were three overlapping groups for pXO1. Group 1 included MLVA clusters A2, A3a, A3b, A4, and B1; group 2 included MLVA clusters A1, A2, A3a, and A3b; and group 3 included MLVA clusters A1 and B2. Post-hoc tests indicated that there were two overlapping groups for pXO2. Group 1 included MLVA clusters A2, A3a, A3b, A4, B1, and B2, and group 2 included MLVA clusters A1, A3a, A3b, B1, and B2.
FIG. 1.
Mean ratios of plasmids (pXO1 and pXO2) to chromosomes and percentage of survival of AVA-vaccinated guinea pigs by MLVA clusters. There is a wide range of variability for all of the means across MLVA clusters, and it is difficult to detect any apparent associations between mean plasmid ratios and percentage of survival. The dendrogram below the graph is adapted from previous published genetic typing results (15) and indicates the genetic relationships among the MLVA clusters shown.
Vaccination challenge and survival.
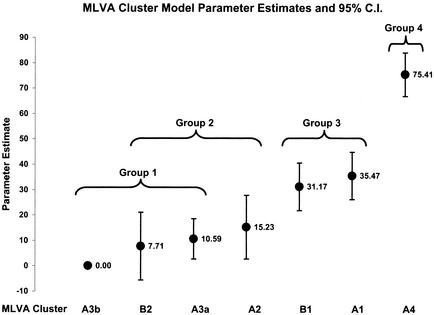
The survival of the vaccinated guinea pigs ranged from 0 to 94%. The percentages of survival of the vaccinated guinea pigs challenged with each of the isolates used in this study are listed in Table 1. The overall average survival was approximately 40%. The average time to death was 5 days for all isolates tested and ranged from 3 to 7 days. The mean percentage of survival of guinea pigs for each MLVA cluster is shown in Fig. 1. The results of an ANOVA indicated that the means were different (P < 0.05). Post-hoc testing showed four groups, two of which had overlapping membership (Fig. 2). The most virulent MLVA cluster (cluster A3b), indicated by lowest survival, had a mean survival of 21.3% and included an isolate of the Ames strain.
FIG. 2.
MLVA cluster factor model of virulence parameter estimates and their 95% confidence intervals (C.I.), along with groupings as indicated by post-hoc testing. MLVA cluster A3b was the arbitrarily set referent factor level and therefore is set at 0. Groups 1 and 2 are overlapping, indicating that there may be as few as three statistically significant different virulence groups or as many as five.
Model of virulence.
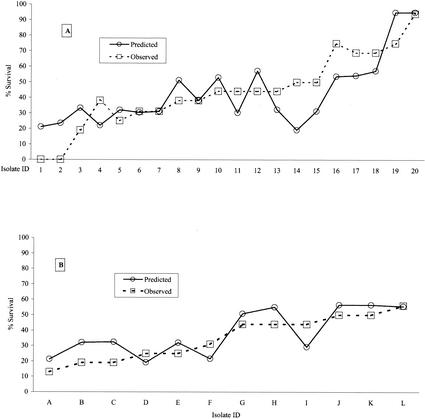
We analyzed the combined data set of percentage of survival, ratio of plasmid to chromosome (rpXO1 and rpXO2), and MLVA cluster assignment by using a general linear univariate model. The overall model statistics indicated that rpXO1 was not a significant predictor of survival (P > 0.05) but that rpXO2 and MLVA cluster were significant (P < 0.05 for both). The parameter estimate obtained for rpXO1 was not significant; however, the estimate obtained for rpXO2 was significant (rpXO1 = 0.06, P > 0.05; rPXO2 = −1.93, P < 0.05). The magnitude of the parameter estimates obtained for each of the seven MLVA clusters, ranging from 0.00 (A3b) to 75.41 (A4) (Fig. 2), indicates a much greater influence on survival outcome than that observed with either plasmid ratio. As previously mentioned, post-hoc testing revealed two overlapping and two distinct statistical groups (Fig. 2), indicating that there are potentially as many as five or as few as three separate groups among the MLVA clusters. Graphs of the observed and predicted percentages of survival for both of the isolates with which the model was constructed and a test set of 12 randomly chosen isolates indicate a good model fit (Fig. 3).
FIG. 3.
Observed and predicted survival rates of AVA-vaccinated guinea pigs challenged with diverse B. anthracis isolates. Twenty isolates were used to construct the model of virulence (A), and a set of 12 isolates was then used to validate the model (B). While there is some deviation between the predicted and observed percentages of survival of guinea pigs when an MLVA cluster factor and plasmid ratio covariates were used, the model is surprisingly robust in performance.
Figures 1 and 2 show a grouping of the MLVA clusters into three overlapping groups. The least virulent group, A4, contains isolates from the United States, Norway, Europe, and Asia (15). This group also contains the Vollum strain, which was used in the United Kingdom biological warfare program (14). The middle group is made up of clusters A1 and B1 and is of medium virulence. Clusters A1 and B1 are similar in virulence but are geographically diverse. Isolates in the A1 cluster were found predominantly in the region stretching from Wood Bison National Park in Canada south to Texas in the United States. Southern African isolates make up the majority of the B1 cluster (15). The most virulent group consists of four clusters, A2, A3a, A3b, and B2. This group is also geographically diverse. B2 has been found almost exclusively in southern Africa (15). A3a is associated with isolates from around the world, especially Turkey and Namibia. A3b is dominated by isolates from China, yet this cluster also contains the Ames strain.
DISCUSSION
In this study, we present results demonstrating that B. anthracis virulence is related to clonality (as indicated by MLVA genotype cluster) and pXO1 and pXO2 copy number. By combining data collected from challenge studies of AVA-vaccinated guinea pigs and data concerning pXO1 and pXO2 plasmid copy number from a genetically diverse set of isolates, we developed a model that is predictive of virulence. We then used this model to compare the predicted and observed survival rates of AVA-vaccinated guinea pigs when challenged with a randomly chosen set of isolates. It is likely that factors affecting the variation in virulence we observed are due to mutations that are heritable and clonally passed on to daughter cells. This could also include a predisposition for stable plasmid copy number configurations of pXO1 and pXO2.
While we can offer no explanation for the association of higher or lower levels of virulence with specific MLVA clusters, the relationship is plausible from the standpoint of mutations and clonality. Other examples of genetic typing-based group differences in pathogen virulence have been observed (4). Further investigation to determine the underlying reasons for variation in virulence should center on the genetic differences between representative isolates from different MLVA clusters, such as A3b and A4, that showed extreme differences in mean survival and model parameter estimates. Although rpXO2 was found to be a significant contributor in the virulence model, there was no distinct difference in the numbers of plasmids per cell for clusters A3b and A4; therefore, we can conclude that the differences in the observed virulence were due to factors other than the number of plasmids per cell.
Our observations have revealed tremendous variation in pXO1 and pXO2 copy numbers per cell by using a genetically diverse collection of isolates. These observations were made possible by the use of a new method for molecular detection of B. anthracis, QPCR. Using QPCR, we were able to detect one copy of the standard plasmids for the chromosome, pXO1, and pXO2. A common belief in the research community has been that B. anthracis contains only one copy of each plasmid. Here, using a QPCR method, we have shown that there is more than one copy of each plasmid per cell and that there is tremendous variation among genetically diverse isolates. Our results indicate that there may be as many as 243 copies of pXO1 and 32 copies of pXO2 per cell. The apparent disparity between our results for the plasmid copy number-to-chromosome ratio and those of Read et al. may be due to a difference in the growth phase when the DNA was harvested (Timothy Read, personal communication). While the difference may seem extreme, it could be appropriate from a biochemical and virulence viewpoint.
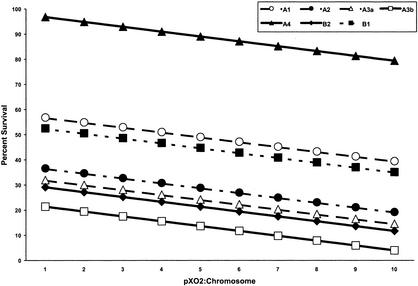
It has long been known that different isolates exhibit different levels of virulence (11, 19, 28). The factors responsible for the different levels of virulence in these isolates are unknown. We have shown that the number of pXO2 plasmids in each bacterial cell contributes to the level of virulence associated with that isolate (Fig. 4). Although the model that we developed indicated that pXO1 copy number does not contribute significantly to virulence, it is likely that in an experimental challenge of unvaccinated animals, one would find that the number of copies of pXO1 would also contribute to variations in virulence. However, the results of the present study indicate that pXO2 plays a significant role in virulence and can contribute to observed variation in virulence. An alternative interpretation for our results would be that the variation in the percentages of survival of guinea pigs represents differences in the ability of genetically diverse isolates to overcome immunity conferred by the AVA vaccine. This seems unlikely when we consider that the basis for protection and immunity is the antibodies formed to block the PA produced by pXO1. Furthermore, pXO2− strains are considered avirulent (or at least severely reduced) and injection into animals confers immunity. Indeed, this is the basis of livestock vaccines for protection against anthrax. In the mouse model, isolates that contain pXO2 only remained lethal at low doses (34). Welkos showed that the pXO2 plasmid contributes significantly to the virulence of the organism (33) and that mutants producing greater amounts of capsule exhibited a higher level of virulence than did the parental strain. Figure 4 shows an increasing gradation of virulence associated with an increase of pXO2.
FIG. 4.
Effect of pXO2/chromosome ratio on the percentage of survival across MLVA clusters. Each of the parallel lines shown represents virulence model performance (percentage of survival) for each MLVA cluster while rpXO1 was held constant and rpXO2 varied over the range observed. The figure dramatically illustrates the difference between the predicted percentages of survival for each MLVA cluster, as well as the more subtle effect of additional copies of pXO2 plasmids, which are not otherwise observable.
Virulence studies of anthrax are an important source of information, especially given the use of the organisms as an agent of bioterrorism and/or biowarfare. This study has put forward some interesting and significant information concerning the virulence of different isolates of B. anthracis and the testing of these same isolates in an animal system. Trends in the data with respect to plasmid copy number have revealed clues that will take us into the next paradigm of virulence testing. Hypotheses have been suggested that can now be tested because of technological advances in molecular biology techniques. Additional animal studies using unimmunized animals utilizing more representative isolates of all clusters are recommended to validate the model and the cluster effect observed in this study. Furthermore, validation of the model could lead to its use as a screening tool and complement the testing of vaccine efficacy.
REFERENCES
- 1.Angen, O., J. Jensen, and D. T. Lavritsen. 2001. Evaluation of 5′ nuclease assay for detection of Actinobacillus pleuropneumoniae. J. Clin. Microbiol. 39:260-265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bach, H. J., J. Tomanova, M. Schloter, and J. C. Munch. 2002. Enumeration of total bacteria and bacteria with genes for proteolytic activity in pure cultures and in environmental samples by quantitative PCR mediated amplification. J. Microbiol. Methods 49:235-245. [DOI] [PubMed] [Google Scholar]
- 3.Beyer, W., P. Glockner, J. Otto, and R. Bohm. 1995. A nested PCR method for the detection of Bacillus anthracis in environmental samples collected from former tannery sites. Microbiol. Res. 150:179-186. [DOI] [PubMed] [Google Scholar]
- 4.Farlow, J., K. L. Smith, J. Wong, M. Abrams, M. Lytle, and P. Keim. 2001. Francisella tularensis strain typing using multiple-locus, variable-number tandem repeat analysis. J. Clin. Microbiol. 39:3186-3192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Farrar, W. E. 1995. Anthrax: from Mesopotamia to molecular biology. Pharos 58:35-38. [PubMed] [Google Scholar]
- 6.Fellows, P. F., M. K. Linscott, B. E. Ivins, M. L. Pitt, C. A. Rossi, P. H. Gibbs, and A. M. Friedlander. 2001. Efficacy of a human anthrax vaccine in guinea pigs, rabbits, and rhesus macaques against challenge by Bacillus anthracis isolates of diverse geographical origin. Vaccine 19:3241-3247. [DOI] [PubMed] [Google Scholar]
- 7.Friedlander, A. M. 2000. Anthrax: clinical features, pathogenesis, and potential biological warfare threat. Curr. Clin. Top. Infect. Dis. 20:335-349. [PubMed] [Google Scholar]
- 8.Friedlander, A. M., S. L. Welkos, M. L. Pitt, J. W. Ezzell, P. L. Worsham, K. J. Rose, B. E. Ivins, J. R. Lowe, G. B. Howe, and P. Mikesell. 1993. Postexposure prophylaxis against experimental inhalation anthrax. J. Infect. Dis. 167:1239-1243. [DOI] [PubMed] [Google Scholar]
- 9.Green, B. D., L. Battisti, T. M. Koehler, C. B. Thorne, and B. E. Ivins. 1985. Demonstration of a capsule plasmid in Bacillus anthracis. Infect. Immun. 49:291-297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Heid, C. A., J. Stevens, K. J. Livak, and P. M. Williams. 1996. Real time quantitative PCR. Genome Res. 6:986-994. [DOI] [PubMed] [Google Scholar]
- 11.Ivins, B. E., P. F. Fellows, and G. O. Nelson. 1994. Efficacy of a standard human anthrax vaccine against Bacillus anthracis spore challenge in guinea-pigs. Vaccine 12:872-874. [DOI] [PubMed] [Google Scholar]
- 12.Ivins, B. E., M. L. Pitt, P. F. Fellows, J. W. Farchaus, G. E. Benner, D. M. Waag, S. F. Little, G. W. Anderson, Jr., P. H. Gibbs, and A. M. Friedlander. 1998. Comparative efficacy of experimental anthrax vaccine candidates against inhalation anthrax in rhesus macaques. Vaccine 16:1141-1148. [DOI] [PubMed] [Google Scholar]
- 13.Jauregui, L. H., J. Higgins, D. Zarlenga, J. P. Dubey, and J. K. Lunney. 2001. Development of a real-time PCR assay for detection of Toxoplasma gondii in pig and mouse tissues. J. Clin. Microbiol. 39:2065-2071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kaufmann, A. F., M. I. Meltzer, and G. P. Schmid. 1997. The economic impact of a bioterrorist attack: are prevention and postattack intervention programs justifiable? Emerg. Infect. Dis. 3:83-94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Keim, P., L. B. Price, A. M. Klevytska, K. L. Smith, J. M. Schupp, R. Okinaka, P. J. Jackson, and M. E. Hugh-Jones. 2000. Multiple-locus variable-number tandem repeat analysis reveals genetic relationships within Bacillus anthracis. J. Bacteriol. 182:2928-2936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Keppie, J. P., P. W. Harris-Smith, and H. Smith. 1963. The chemical basis of the virulence of Bacillus anthracis. IX. Its aggressins and their mode of action. Br. J. Exp. Pathol. 44:446-453. [PMC free article] [PubMed] [Google Scholar]
- 17.Leppla, S. H. 1995. Bacterial toxins and virulence factors in disease, p. 543-572. Marcel Dekker, New York, N.Y.
- 18.Little, S. F., and B. E. Ivins. 1999. Molecular pathogenesis of Bacillus anthracis infection. Microbes Infect. 1:131-139. [DOI] [PubMed] [Google Scholar]
- 19.Little, S. F., and G. B. Knudson. 1986. Comparative efficacy of Bacillus anthracis live spore vaccine and protective antigen vaccine against anthrax in the guinea pig. Infect. Immun. 52:509-512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ludwig, W., and K. H. Schleifer. 2000. How quantitative is quantitative PCR with respect to cell counts? Syst. Appl. Microbiol. 23:556-562. [DOI] [PubMed] [Google Scholar]
- 21.Makino, S., I. Uchida, N. Terakado, C. Sasakawa, and M. Yoshikawa. 1989. Molecular characterization and protein analysis of the cap region, which is essential for encapsulation in Bacillus anthracis. J. Bacteriol. 171:722-730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Makino, S. I., H. I. Cheun, M. Watarai, I. Uchida, and K. Takeshi. 2001. Detection of anthrax spores from the air by real-time PCR. Lett. Appl. Microbiol 33:237-240. [DOI] [PubMed] [Google Scholar]
- 23.Mikesell, P., B. E. Ivins, J. D. Ristroph, M. H. Vodkin, T. Drier, and S. Leppla. 2002. Plasmids, Pasteur, and anthrax. ASM News 49:320-322. [Google Scholar]
- 24.National Research Council. 1996. Guide for the care and use of laboratory animals. National Academy Press, Washington, D.C.
- 25.Ramisse, V., G. Patra, H. Garrigue, J. L. Guesdon, and M. Mock. 1996. Identification and characterization of Bacillus anthracis by multiplex PCR analysis of sequences on plasmids pXO1 and pXO2 and chromosomal DNA. FEMS Microbiol. Lett. 145:9-16. [DOI] [PubMed] [Google Scholar]
- 26.Read, T. D., S. L. Salzberg, M. Pop, M. Shumway, L. Umayam, L. Jiang, E. Holtzapple, J. D. Busch, K. L. Smith, J. M. Schupp, D. Solomon, P. Keim, and C. M. Fraser. 2002. Comparative genome sequencing for discovery of novel polymorphisms in Bacillus anthracis. Science 296:2028-2033. [DOI] [PubMed] [Google Scholar]
- 27.Turnbull, P. C. 1991. Anthrax vaccines: past, present and future. Vaccine 9:533-539. [DOI] [PubMed] [Google Scholar]
- 28.Turnbull, P. C., M. G. Broster, J. A. Carman, R. J. Manchee, and J. Melling. 1986. Development of antibodies to protective antigen and lethal factor components of anthrax toxin in humans and guinea pigs and their relevance to protective immunity. Infect. Immun. 52:356-363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Turnbull, P. C. B. 1998. Guidelines for the surveillance and control of anthrax in humans and animals, p. 1-110. World Health Organization, Geneva, Switzerland.
- 30.Turnbull, P. C. B., and J. M. Kramer. 1995. Bacillus, p. 349-356. In P. R. Murray, E. J. Baron, M. A. Pfaller, F. C. Tenover, and R. H. Yolken (ed.), Manual of clinical microbiology, 6th ed. ASM Press, Washington, D.C.
- 31.Uchida, I., K. Hashimoto, and N. Terakado. 1986. Virulence and immunogenicity in experimental animals of Bacillus anthracis strains harbouring or lacking 110 MDa and 60 MDa plasmids. J. Gen. Microbiol. 132(Pt. 2):557-559. [DOI] [PubMed] [Google Scholar]
- 32.Uchida, I., J. M. Hornung, C. B. Thorne, K. R. Klimpel, and S. H. Leppla. 1993. Cloning and characterization of a gene whose product is a trans-activator of anthrax toxin synthesis. J. Bacteriol. 175:5329-5338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Welkos, S. L. 1991. Plasmid-associated virulence factors of non-toxigenic (pX01-) Bacillus anthracis. Microb. Pathog. 10:183-198. [DOI] [PubMed] [Google Scholar]
- 34.Welkos, S. L., D. Becker, A. Friedlander, and R. Trotter. 1990. Pathogenesis and host resistance to Bacillus anthracis: a mouse model. Salisbury Med. Bull. 68(Special Suppl.):49-52. [Google Scholar]
- 35.Welkos, S. L., N. J. Vietri, and P. H. Gibbs. 1993. Non-toxigenic derivatives of the Ames strain of Bacillus anthracis are fully virulent for mice: role of plasmid pX02 and chromosome in strain-dependent virulence. Microb. Pathog. 14:381-388. [DOI] [PubMed] [Google Scholar]