Abstract
Cancer of the exocrine pancreas represents the fifth leading cause of cancer death in the Western population with an average survival after diagnosis of 3 to 6 months and a five-year survival rate under 5%. Our understanding of the molecular carcinogenesis has improved in the last few years due to the development of novel molecular biological techniques. Pancreatic cancer is a multi-stage process resulting from the accumulation of genetic changes in the somatic DNA of normal cells. In this article we describe major genetic alterations of pancreatic cancer, mutations in the proto-oncogene K-RAS and the tumor suppressors INK4A, TP53 and DPC4/SMAD4. The accumulation of these genetic changes leads to a profound disturbance in cell cycle regulation and continuous growth. The knowledge of the underlying molecular mechanisms will offer new therapeutic and diagnostic options and hopefully improve the outcome of this aggressive disease.
Review
Cancer of the exocrine pancreas represents the fifth leading cause of cancer death in the Western population with a five-year survival rate under 5% [1]. Because of the few treatment options, understanding of the molecular pathology is prerequisite to identify potential molecular targets for drug therapy.
The PanIN (Pancreatic intraepithelial neoplasia) classification describes various changes in the pancreatic duct system distinguishing three PanIN grades (PanIN 1 – PanIN 3) according to the degree of structural dysplasia and cytological atypia present in the lesions [2]. Microdissection techniques revealed genetic alteration in cancer-causing genes in the putative premalignant lesions similar to pancreatic carcinomas (see table 1). The combination of morphological and genetic observations leads to a tumor progression model for pancreatic carcinoma, comparable to the adenoma-carcinoma sequence in colorectal carcinomas [3]. The sequential acquisition of mutations in the proto-oncogene K-RAS and the tumor suppressors INK4A, TP53 and DPC4/SMAD4 leads to a profound disturbance in cell cycle regulation, a hallmark of pancreatic cancer. Mutations in K-RAS, INK4A, TP53 and DPC4/SMAD4 are frequent, whereas mutations in the tumor suppressor BRCA2, mismatch repair genes and the serine-threonine kinases AKT2 and LKB1/STK11 are rare genetic events. Table 1 summarizes the reported frequencies of major genetic alterations in the pancreatic tumor progression model.
Table 1.
Frequency of major genetic alterations in pancreatic carcinoma.
| Gene | Reference | Normal | PanIN1A | PanIN1B | PanIN2 | PanIN3 | Carcinoma |
| K-RAS | [6] | 0% | 38% | 44% | 87% | ||
| [36] | 3% | 30% | 31% | 73% | |||
| ~90% | |||||||
| INK4a | [19] | 0% | 30% | 27% | 55% | 71% | 100% |
| [14] | 33% | 40% | |||||
| TP53 | [37] | 0% | 12% | 40% | |||
| [35] | 0% | 35% | 36% | 40% | |||
| [36] | 0% | 0% | 0% | 9,1% | 87% | ||
| [9] | 0% | 0% | 0% | 20% | 57% | 47% | |
| DPC4/Smad4 | [47] | 0% | 0% | 0% | 31% | 55% | |
| [9] | 0% | 0% | 0% | 0% | 33% | 66% |
Genetic alterations with high frequency
Pancreatic cancer has the highest incidence of RAS mutations in human tumors identified to date [4]. The mutations of the K-RAS gene, H-RAS and N-RAS are not affected, are generally found in codon 12. Dependent on the used technique the frequencies of codon 12 mutations reported range from 20 to 100% and occur early in the tumor progression model [5,6]. The RAS family proteins encode small GTP-binding cytoplasmic proteins that mediate pleiotropic effects including cell proliferation, survival and migration [7]. Mutation of codon 12 in K-RAS results in a gain of function, because the RAS protein remains trapped in the activated state. Considering RAS transforming potential, tissue and species differences come into question. In general epithelial human cells are not very sensitive to oncogene transformation. In contrast primary murine fibroblasts can be efficiently transformed by mutated RAS in concert with a second oncogene or loss of a tumor suppressor, like p53 or p16NK4a. The sole expression of oncogenic RAS in primary rodent and human cells results in a permanent G1 arrest accompanied by accumulation of p53, p16INK4A and p21CIP1 [8]. This senescence is thought to be a defense mechanism against oncogenic stress. Whether the observed overexpression of p21CIP1, whose frequency parallels that of K-RAS Mutation in the pancreatic tumor progression model, is part of this defense mechanism or directly linked to the cell cycle by working as an assembly factor for the cyclin D1/CDK4 complex, is not known [9,10]. Placing p21CIP1 in a defence program is speculative but attractive, because it could explain in part the observation that oncogenic K-RAS mutations are not specific for malignancy, being present in benign diseases of the pancreas and in early clonal lesions. Moreover, the risk of progression to malignancy is low in the absence of co-operating genetic events [11-14]. Despite the high mutation frequency in human pancreatic carcinoma, mice which harbor a latent allele of K-Ras G12D capable of spontaneous activation in vivo, develop multiple early onset lung tumors but not pancreatic cancer, further demonstrating the species differences of RAS function [15]. The complexity of RAS function is amplified through recent data suggesting tumor suppressor properties of RAS. Transfection of wildtype Ras into rat fibroblasts inhibits anchorage-independent growth and colony formation, induced by the oncogenic Ras gene [16]. Furthermore – in vivo – Kras2 can inhibit lung carcinogenesis in mice [17]. A tumor suppressor function of K-RAS might also exist in the pancreas. Loss of the wildtype K-RAS allele was observed in some pancreatic carcinoma cell lines with mutation in K-RAS (ASPC1, Capan1 and MiaPaca) and there was underexpression of the mutanted allele in comparison to the wildtype allele in two other cell lines (Su8686 and Panc1) [5]. A further species difference affects the signaling pathway utilized by oncogenic RAS. Whereas in rodent cells the Raf/MAPK and the PI3K are thought to mediate many effects of oncogenic Ras, there are hints that in human cells the guanine nucleotide exchange factor Ral is sufficient for Ras transformation [18]. Therefore, the net outcome of RAS activation in a specific setting is not easy to predict and further studies, including primary cultures of epithelial pancreas cells, are needed.
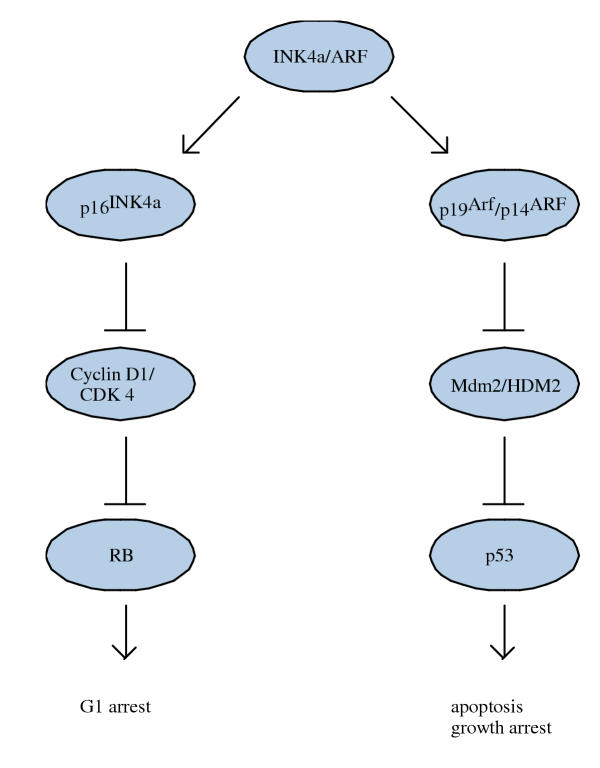
Homozygous deletion of p16INK4A/p14ARF locus is a characteristic genetic alteration observed in 80% – 95% of human pancreatic cancer and usually occurs in later stages of the tumor progression model [19-21]. This locus on chromosom 9q21 encodes the two related tumor suppressor genes INK4a and ARF, who's coding sequence partially overlap. INK4a and ARF are generated by the use of a different first exon and an alternative reading frame in exon 2. Whereas INK4a regulates cell cycle progression as an inhibitor of the cyclin D/CDK 4/6 kinase complex, ARF directly interacts with Mdm 2/HDM 2 to block the interaction with p53 by localizing Mdm 2/HDM 2 to the nucleolus and by inhibiting directly Mdm 2/HDM 2's E3 ubiquitin ligase activity, contributing to p53 activation (figure 1) [22]. Gene deficient mice for p19Arf, the mouse homologue of human p14ARF, strongly suggest that Arf is the major tumor suppressor in mice [23,24]. The specific mutation of the Ink4a gene in mice also etablishes p16Ink4a as a tumor suppressor in mice [25,26]. Germline mutations in the exon 1α of INK4a are associated with the Familial Atypical Mole-Malignant Melanoma syndrome, implicating INK4a in human tumor susceptibility [27]. This mutation also predispose to pancreatic cancer, but in contrast to very high penetrance and early onset of melanoma, the penetrance of pancreatic cancer is very low and displays latency similar to the sporadic disease [28-30]. In humans INK4a seems to be the more important tumor suppressor for pancreatic cancer development, because germline and sporadic mutations have been identified that target INK4a, but omit ARF [21,31,32]. Mutations that selectively target ARF are rare findings [33]. In sporadic tumors INK4a is inactivated by homozygous deletions and intragenic mutation and in the remaining cases the INK4a gene is turned off through promoter methylation [20,34].
Figure 1.
The INK4a/ARF locus. The two products of the INK4a/ARF locus encodes for p16INK4a and p14ARF (p19Arf in mice). p16INK4a indirectly regulates RB function and p14ARF indirectly stabilizes p53.
The TP53 tumor suppressor gene is mutated, especially by missense mutations in sequences coding for the DNA binding domain, in greater than 50% of pancreatic adenocarcinomas. The mutations are often accompanied by loss of the wildtyp allele and occur late in the progression model [21,35-39]. The transcription factor p53 regulates an essential growth checkpoint that both protects against genomic rearrangement or the accumulation of mutations, and suppresses cellular transformation caused by oncogene activation or the loss of tumor suppressor pathways. p53 is stabilized and activated by extracellular stress including γ irradiation and intracellular stress such as deregulation of cellular oncogenes. Once activated, p53 can induce cell cycle arrest or apoptosis [40]. Loss of p53 is associated with aneuploidy, an outstanding feature of pancreatic cancer, indicating that p53 function maintains genomic stability [41,42]. Germline mutations in TP53 have been described as Li-Fraumeni syndrome, predisposing to several neoplasms, but pancreatic carcinomas are rare findings [43,44]. SMAD4, which was initially named DPC4, deleted in pancreatic carcinoma, was originally identified as a candidate tumor suppressor that is frequently inactivated in pancreatic tumors [45]. The transcription factor SMAD4 is an important regulator of the transforming growth factor β (TGF-β) signaling pathway [46]. Upon receptor activation SMAD proteins get phosphorylated and heterodimerize with Smad4 to transmit upstream signals to the nucleus and transactivate transcription of specific target genes. The SMAD4 gene is deleted or mutated in over 50% of pancreatic carcinoma, an event occurring late in the tumor progression model [9,47]. The most prominent biological activity of TGF-β is its potent inhibition of cell growth, mediated by a cell cycle G1 arrest, in a wide variety of cells. It is assumed that the growth-inhibitory function of TGF-β is important for SMAD4 tumor suppressor activity. But recent data also suggest TGF-β independent SMAD4 function. Restoration of SMAD4 in human pancreatic carcinoma cells suppressed tumor formation in vivo and did not restore TGF-β sensitivity. Furthermore a decrease in pro-angiogenic VEGF expression and an increase in the angiogenesis inhibitor TSP-1 was observed, so that regulation of an angiogenic switch might contribute to the tumor suppressor function of SMAD4 [48]. Epigenetic inactivation of the TGF-β/SMAD4 pathway occurs in the presence of activated RAS, whereby explaining the reduced selection pressure for LOH at the SMAD4 locus [49]. Recent studies suggest a more aggressive behavior of SMAD4 negative pancreatic cancers [50,51].
Genetic alterations with low frequency
BRCA2 on chromosome 13q encodes for a protein that is needed for the maintenance of genomic stability by regulating DNA repair processes. Normal cells, deficient for BRCA2, accumulate lethal chromosomal aberrations [52]. Inherited BRCA2 mutation predispose to early onset familiar breast and ovarian cancer [53]. Albeit with lower penetrance and equal age of onset, inherited BRCA2 mutations also increase the risk for pancreatic cancer [54,55]. In sporadic pancreatic cancer BRCA2 is inactivated in 7 to 10% and lately the biallelic inactivation in a high-grade duct lesion was demonstrated, so that it is assumed that BRCA2 mutation occur late in the neoplastic progression in the pancreas [56].
The autosomal dominant inherited Peutz-Jeghers syndrome, caused by mutation of the serine-threonine kinase LKB1/STK11 that maps to chromosom 19p13, is associated with an increased incidence of pancreatic carcinoma [57-60]. The signaling pathway of LKB1/STK1 is so far unknown, but this gene was shown to be inactivated in 5% of sporadic pancreatic cancer, suggesting a possible role in tumor suppression [61,62].
The serine-treonine kinase AKT2 is a candidate oncogene for human pancreatic cancer and was found to be amplified and overexpressed in pancreatic adenocarcinoma and cell lines in up to 20% [63-65]. AKT2 is a downstream effector of the PI3 kinase and can be activated by epidermal growth factor, platelet-derived growth factor and basic fibroblast growth factor, all known to be overexpressed in pancreatic carcinoma [66,67]. Recently AKT signaling was linked to enforced insulin-like growth factor I receptor expression, promoting invasiveness of pancreatic cancer cells [68].
Autosomal dominant inherited Lynch syndrome is characterized by an increased risk of developing colorectal, endometrial, ovarian and breast cancers, transitional carcinoma of the ureter and renal pelvis [69]. Mutations in the DNA mismatch repair genes, including hMLH1, hMSH2 and hMSH6, cause this syndrome. Pancreatic cancer is included in the tumor spectrum, however, it seems to be a rare finding [70,71]. Pancreatic cancers occurring in context of the Lynch syndrome are different compared to sporadic pancreatic carcinomas in terms of the superior clinical course, histopathology and distinct molecular genetic profiles, including retention of wildtyp RAS [72-74]. Furthermore, microsattellite instability is unlikely to participate in the oncogenesis of spontaneous pancreatic cancer [75-77].
Conclusion
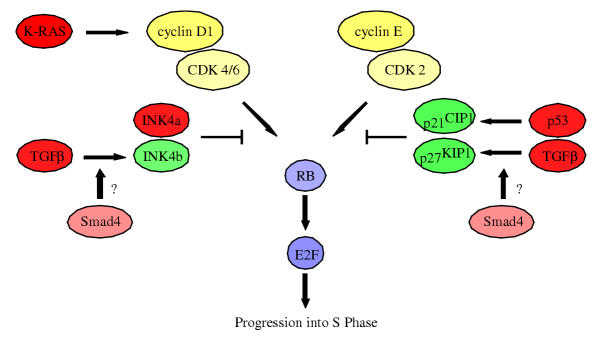
Molecular investigations of pancreatic cancer are complicated by the restricted accessibility of the organ for biopsies. The findings in molecular research on pancreatic carcinoma of the last years is now integrated in a pancreatic tumor progression model, with genetically, epigenetically and morphological defined precursor lesions. Pancreatic cancer is a genetic disease, but the transition between cancer and non-cancer is not regulated by a simple switch activated by a single gene. In fact, multiple mutations must accumulate in a single cell, including overexpression of receptor-ligand systems, oncogene activation and loss of tumor suppressor genes, to develop pancreatic carcinoma. But where are the diverse genetic alterations, whose number is increasing, integrated? Deregulated cell cycle is the hallmark of many human tumors, including pancreatic carcinoma, and therefore the cell cycle could be placed into the center of pancreatic oncogenesis. As figure 2 illustrates, each of the major genetic alteration mentioned above is involved in cell cycle regulation and leads together to the acceleration of the cell cycle progression and continuous growth.
Figure 2.
Interplay of the major genetic alteration in pancreatic carcinoma with the cell cycle. All four major genetic alteration, K-RAS, INK4a, TP53 and the TGF-β/SMAD4 tumor suppressor pathway, observed in pancreatic carcinoma, regulate directly or indirectly G1 progression, leading to E2F dependent S phase entry.
Further analysis of the underlying molecular mechanism will offer new diagnostic and therapeutic options and, hopefully improve the outcome of this dismal disease in the future.
Contributor Information
Gunter Schneider, Email: guenter.schneider@lrz.tum.de.
Roland M Schmid, Email: roland.schmid@lrz.tum.de.
References
- Jemal A, Thomas A, Murray T, Thun M. Cancer statistics, 2002. CA Cancer J Clin. 2002;52:23–47. doi: 10.3322/canjclin.52.1.23. [DOI] [PubMed] [Google Scholar]
- Hruban RH, Adsay NV, Albores-Saavedra J, Compton C, Garrett ES, Goodman SN, Kern SE, Klimstra DS, Kloppel G, Longnecker DS, et al. Pancreatic intraepithelial neoplasia: a new nomenclature and classification system for pancreatic duct lesions. Am J Surg Pathol. 2001;25:579–86. doi: 10.1097/00000478-200105000-00003. [DOI] [PubMed] [Google Scholar]
- Hruban RH, Wilentz RE, Kern SE. Genetic progression in the pancreatic ducts. Am J Pathol. 2000;156:1821–5. doi: 10.1016/S0002-9440(10)65054-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Almoguera C, Shibata D, Forrester K, Martin J, Arnheim N, Perucho M. Most human carcinomas of the exocrine pancreas contain mutant c-K-ras genes. Cell. 1988;53:549–54. doi: 10.1016/0092-8674(88)90571-5. [DOI] [PubMed] [Google Scholar]
- Caldas C, Kern SE. K-ras mutation and pancreatic adenocarcinoma. Int J Pancreatol. 1995;18:1–6. doi: 10.1007/BF02825415. [DOI] [PubMed] [Google Scholar]
- Terhune PG, Phifer DM, Tosteson TD, Longnecker DS. K-ras mutation in focal proliferative lesions of human pancreas. Cancer Epidemiol Biomarkers Prev. 1998;7:515–21. [PubMed] [Google Scholar]
- Shields JM, Pruitt K, McFall A, Shaub A, Der CJ. Understanding Ras: 'it ain't over 'til it's over'. Trends Cell Biol. 2000;10:147–54. doi: 10.1016/S0962-8924(00)01740-2. [DOI] [PubMed] [Google Scholar]
- Serrano M, Lin AW, McCurrach ME, Beach D, Lowe SW. Oncogenic ras provokes premature cell senescence associated with accumulation of p53 and p16INK4a. Cell. 1997;88:593–602. doi: 10.1016/S0092-8674(00)81902-9. [DOI] [PubMed] [Google Scholar]
- Biankin AV, Kench JG, Morey AL, Lee CS, Biankin SA, Head DR, Hugh TB, Henshall SM, Sutherland RL. Overexpression of p21(WAF1/CIP1) is an early event in the development of pancreatic intraepithelial neoplasia. Cancer Res. 2001;61:8830–7. [PubMed] [Google Scholar]
- LaBaer J, Garrett MD, Stevenson LF, Slingerland JM, Sandhu C, Chou HS, Fattaey A, Harlow E. New functional activities for the p21 family of CDK inhibitors. Genes Dev. 1997;11:847–62. doi: 10.1101/gad.11.7.847. [DOI] [PubMed] [Google Scholar]
- Tada M, Omata M, Kawai S, Saisho H, Ohto M, Saiki RK, Sninsky JJ. Detection of ras gene mutations in pancreatic juice and peripheral blood of patients with pancreatic adenocarcinoma. Cancer Res. 1993;53:2472–4. [PubMed] [Google Scholar]
- Tada M, Ohashi M, Shiratori Y, Okudaira T, Komatsu Y, Kawabe T, Yoshida H, Machinami R, Kishi K, Omata M. Analysis of K-ras gene mutation in hyperplastic duct cells of the pancreas without pancreatic disease. Gastroenterology. 1996;110:227–31. doi: 10.1053/gast.1996.v110.pm8536861. [DOI] [PubMed] [Google Scholar]
- Yanagisawa A, Ohtake K, Ohashi K, Hori M, Kitagawa T, Sugano H, Kato Y. Frequent c-Ki-ras oncogene activation in mucous cell hyperplasias of pancreas suffering from chronic inflammation. Cancer Res. 1993;53:953–6. [PubMed] [Google Scholar]
- Moskaluk CA, Hruban RH, Kern SE. p16 and K-ras gene mutations in the intraductal precursors of human pancreatic adenocarcinoma. Cancer Res. 1997;57:2140–3. [PubMed] [Google Scholar]
- Johnson L, Mercer K, Greenbaum D, Bronson RT, Crowley D, Tuveson DA, Jacks T. Somatic activation of the K-ras oncogene causes early onset lung cancer in mice. Nature. 2001;410:1111–6. doi: 10.1038/35074129. [DOI] [PubMed] [Google Scholar]
- Spandidos DA, Frame M, Wilkie NM. Expression of the normal H-ras1 gene can suppress the transformed and tumorigenic phenotypes induced by mutant ras genes. Anticancer Res. 1990;10:1543–54. [PubMed] [Google Scholar]
- Zhang Z, Wang Y, Vikis HG, Johnson L, Liu G, Li J, Anderson MW, Sills RC, Hong HL, Devereux TR, et al. Wildtype Kras2 can inhibit lung carcinogenesis in mice. Nat Genet. 2001;29:25–33. doi: 10.1038/ng721. [DOI] [PubMed] [Google Scholar]
- Hamad NM, Elconin JH, Karnoub AE, Bai W, Rich JN, Abraham RT, Der CJ, Counter CM. Distinct requirements for Ras oncogenesis in human versus mouse cells. Genes Dev. 2002;16:2045–57. doi: 10.1101/gad.993902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilentz RE, Geradts J, Maynard R, Offerhaus GJ, Kang M, Goggins M, Yeo CJ, Kern SE, Hruban RH. Inactivation of the p16 (INK4A) tumor-suppressor gene in pancreatic duct lesions: loss of intranuclear expression. Cancer Res. 1998;58:4740–4. [PubMed] [Google Scholar]
- Caldas C, Hahn SA, da Costa LT, Redston MS, Schutte M, Seymour AB, Weinstein CL, Hruban RH, Yeo CJ, Kern SE. Frequent somatic mutations and homozygous deletions of the p16 (MTS1) gene in pancreatic adenocarcinoma. Nat Genet. 1994;8:27–32. doi: 10.1038/ng0994-27. [DOI] [PubMed] [Google Scholar]
- Rozenblum E, Schutte M, Goggins M, Hahn SA, Panzer S, Zahurak M, Goodman SN, Sohn TA, Hruban RH, Yeo CJ, et al. Tumor-suppressive pathways in pancreatic carcinoma. Cancer Res. 1997;57:1731–4. [PubMed] [Google Scholar]
- Sherr CJ. The INK4a/ARF network in tumour suppression. Nat Rev Mol Cell Biol. 2001;2:731–7. doi: 10.1038/35096061. [DOI] [PubMed] [Google Scholar]
- Serrano M, Lee H, Chin L, Cordon-Cardo C, Beach D, DePinho RA. Role of the INK4a locus in tumor suppression and cell mortality. Cell. 1996;85:27–37. doi: 10.1016/s0092-8674(00)81079-x. [DOI] [PubMed] [Google Scholar]
- Kamijo T, Zindy F, Roussel MF, Quelle DE, Downing JR, Ashmun RA, Grosveld G, Sherr CJ. Tumor suppression at the mouse INK4a locus mediated by the alternative reading frame product p19ARF. Cell. 1997;91:649–59. doi: 10.1016/s0092-8674(00)80452-3. [DOI] [PubMed] [Google Scholar]
- Sharpless NE, Bardeesy N, Lee KH, Carrasco D, Castrillon DH, Aguirre AJ, Wu EA, Horner JW, DePinho RA. Loss of p16Ink4a with retention of p19Arf predisposes mice to tumorigenesis. Nature. 2001;413:86–91. doi: 10.1038/35092592. [DOI] [PubMed] [Google Scholar]
- Krimpenfort P, Quon KC, Mooi WJ, Loonstra A, Berns A. Loss of p16Ink4a confers susceptibility to metastatic melanoma in mice. Nature. 2001;413:83–6. doi: 10.1038/35092584. [DOI] [PubMed] [Google Scholar]
- Gruis NA, van der Velden PA, Sandkuijl LA, Prins DE, Weaver-Feldhaus J, Kamb A, Bergman W, Frants RR. Homozygotes for CDKN2 (p16) germline mutation in Dutch familial melanoma kindreds. Nat Genet. 1995;10:351–3. doi: 10.1038/ng0795-351. [DOI] [PubMed] [Google Scholar]
- Goldstein AM, Fraser MC, Struewing JP, Hussussian CJ, Ranade K, Zametkin DP, Fontaine LS, Organic SM, Dracopoli NC, Clark WH, Jr, et al. Increased risk of pancreatic cancer in melanoma-prone kindreds with p16INK4 mutations. N Engl J Med. 1995;333:970–4. doi: 10.1056/NEJM199510123331504. [DOI] [PubMed] [Google Scholar]
- Whelan AJ, Bartsch D, Goodfellow PJ. Brief report: a familial syndrome of pancreatic cancer and melanoma with a mutation in the CDKN2 tumor-suppressor gene. N Engl J Med. 1995;333:975–7. doi: 10.1056/NEJM199510123331505. [DOI] [PubMed] [Google Scholar]
- Lynch HT, Fitzsimmons ML, Smyrk TC, Lanspa SJ, Watson P, McClellan J, Lynch JF. Familial pancreatic cancer: clinicopathologic study of 18 nuclear families. Am J Gastroenterol. 1990;85:54–60. [PubMed] [Google Scholar]
- Liu L, Dilworth D, Gao L, Monzon J, Summers A, Lassam N, Hogg D. Mutation of the CDKN2A 5' UTR creates an aberrant initiation codon and predisposes to melanoma. Nat Genet. 1999;21:128–32. doi: 10.1038/5082. [DOI] [PubMed] [Google Scholar]
- Lal G, Liu L, Hogg D, Lassam NJ, Redston MS, Gallinger S. Patients with both pancreatic adenocarcinoma and melanoma may harbor germline CDKN2A mutations. Genes Chromosomes Cancer. 2000;27:358–61. doi: 10.1002/(SICI)1098-2264(200004)27:4<358::AID-GCC4>3.0.CO;2-O. [DOI] [PubMed] [Google Scholar]
- Randerson-Moor JA, Harland M, Williams S, D Cuthbert-Heavens, Sheridan E, Aveyard J, Sibley K, Whitaker L, Knowles M, Bishop JN, et al. A germline deletion of p14(ARF) but not CDKN2A in a melanoma-neural system tumour syndrome family. Hum Mol Genet. 2001;10:55–62. doi: 10.1093/hmg/10.1.55. [DOI] [PubMed] [Google Scholar]
- Schutte M, Hruban RH, Geradts J, Maynard R, Hilgers W, Rabindran SK, Moskaluk CA, Hahn SA, Schwarte-Waldhoff I, Schmiegel W, et al. Abrogation of the Rb/p16 tumor-suppressive pathway in virtually all pancreatic carcinomas. Cancer Res. 1997;57:3126–30. [PubMed] [Google Scholar]
- Boschman CR, Stryker S, Reddy JK, Rao MS. Expression of p53 protein in precursor lesions and adenocarcinoma of human pancreas. Am J Pathol. 1994;145:1291–5. [PMC free article] [PubMed] [Google Scholar]
- Apple SK, Hecht JR, Lewin DN, Jahromi SA, Grody WW, Nieberg RK. Immunohistochemical evaluation of K-ras, p53, and HER-2/neu expression in hyperplastic, dysplastic, and carcinomatous lesions of the pancreas: evidence for multistep carcinogenesis. Hum Pathol. 1999;30:123–9. doi: 10.1016/s0046-8177(99)90265-4. [DOI] [PubMed] [Google Scholar]
- DiGiuseppe JA, Hruban RH, Goodman SN, Polak M, van den Berg FM, Allison DC, Cameron JL, Offerhaus GJ. Overexpression of p53 protein in adenocarcinoma of the pancreas. Am J Clin Pathol. 1994;101:684–8. doi: 10.1093/ajcp/101.6.684. [DOI] [PubMed] [Google Scholar]
- Redston MS, Caldas C, Seymour AB, Hruban RH, da Costa L, Yeo CJ, Kern SE. p53 mutations in pancreatic carcinoma and evidence of common involvement of homocopolymer tracts in DNA microdeletions. Cancer Res. 1994;54:3025–33. [PubMed] [Google Scholar]
- Barton CM, Staddon SL, Hughes CM, Hall PA, O'Sullivan C, Kloppel G, Theis B, Russell RC, Neoptolemos J, RC Williamson, et al. Abnormalities of the p53 tumour suppressor gene in human pancreatic cancer. Br J Cancer. 1991;64:1076–82. doi: 10.1038/bjc.1991.467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levine AJ. p53, the cellular gatekeeper for growth and division. Cell. 1997;88:323–31. doi: 10.1016/s0092-8674(00)81871-1. [DOI] [PubMed] [Google Scholar]
- Harada T, Okita K, Shiraishi K, Kusano N, Kondoh S, Sasaki K. Interglandular cytogenetic heterogeneity detected by comparative genomic hybridization in pancreatic cancer. Cancer Res. 2002;62:835–9. [PubMed] [Google Scholar]
- Gorunova L, Hoglund M, Andren-Sandberg A, Dawiskiba S, Jin Y, Mitelman F, Johansson B. Cytogenetic analysis of pancreatic carcinomas: intratumor heterogeneity and nonrandom pattern of chromosome aberrations. Genes Chromosomes Cancer. 1998;23:81–99. doi: 10.1002/(SICI)1098-2264(199810)23:2<81::AID-GCC1>3.0.CO;2-0. [DOI] [PubMed] [Google Scholar]
- Strong LC, Stine M, Norsted TL. Cancer in survivors of childhood soft tissue sarcoma and their relatives. J Natl Cancer Inst. 1987;79:1213–20. [PubMed] [Google Scholar]
- Li FP, Fraumeni JF, Jr, Mulvihill JJ, Blattner WA, Dreyfus MG, Tucker MA, Miller RW. A cancer family syndrome in twenty-four kindreds. Cancer Res. 1988;48:5358–62. [PubMed] [Google Scholar]
- Hahn SA, Schutte M, Hoque AT, Moskaluk CA, da Costa LT, Rozenblum E, Weinstein CL, Fischer A, Yeo CJ, Hruban RH, et al. DPC4, a candidate tumor suppressor gene at human chromosome 18q21.1. Science. 1996;271:350–3. doi: 10.1126/science.271.5247.350. [DOI] [PubMed] [Google Scholar]
- Massague J, Blain SW, Lo RS. TGFbeta signaling in growth control, cancer, and heritable disorders. Cell. 2000;103:295–309. doi: 10.1016/s0092-8674(00)00121-5. [DOI] [PubMed] [Google Scholar]
- Wilentz RE, Iacobuzio-Donahue CA, Argani P, McCarthy DM, Parsons JL, Yeo CJ, Kern SE, Hruban RH. Loss of expression of Dpc4 in pancreatic intraepithelial neoplasia: evidence that DPC4 inactivation occurs late in neoplastic progression. Cancer Res. 2000;60:2002–6. [PubMed] [Google Scholar]
- Schwarte-Waldhoff I, Volpert OV, Bouck NP, Sipos B, Hahn SA, Klein-Scory S, Luttges J, Kloppel G, Graeven U, C Eilert-Micus, et al. Smad4/DPC4-mediated tumor suppression through suppression of angiogenesis. Proc Natl Acad Sci U S A. 2000;97:9624–9. doi: 10.1073/pnas.97.17.9624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kretzschmar M, Doody J, Timokhina I, Massague J. A mechanism of repression of TGFbeta/ Smad signaling by oncogenic Ras. Genes Dev. 1999;13:804–16. doi: 10.1101/gad.13.7.804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tascilar M, Skinner HG, Rosty C, Sohn T, Wilentz RE, Offerhaus GJ, Adsay V, Abrams RA, Cameron JL, Kern SE, et al. The SMAD4 protein and prognosis of pancreatic ductal adenocarcinoma. Clin Cancer Res. 2001;7:4115–21. [PubMed] [Google Scholar]
- Biankin AV, Morey AL, Lee CS, Kench JG, Biankin SA, Hook HC, Head DR, Hugh TB, Sutherland RL, Henshall SM. DPC4/Smad4 Expression and Outcome in Pancreatic Ductal Adenocarcinoma. J Clin Oncol. 2002;20:4531–42. doi: 10.1200/JCO.2002.12.063. [DOI] [PubMed] [Google Scholar]
- Venkitaraman AR. Cancer susceptibility and the functions of BRCA1 and BRCA2. Cell. 2002;108:171–82. doi: 10.1016/s0092-8674(02)00615-3. [DOI] [PubMed] [Google Scholar]
- Lancaster JM, Wooster R, Mangion J, Phelan CM, Cochran C, Gumbs C, Seal S, Barfoot R, Collins N, Bignell G, et al. BRCA2 mutations in primary breast and ovarian cancers. Nat Genet. 1996;13:238–40. doi: 10.1038/ng0696-238. [DOI] [PubMed] [Google Scholar]
- Ozcelik H, Schmocker B, Di Nicola N, Shi XH, Langer B, Moore M, Taylor BR, Narod SA, Darlington G, Andrulis IL, et al. Germline BRCA2 6174delT mutations in Ashkenazi Jewish pancreatic cancer patients. Nat Genet. 1997;16:17–8. doi: 10.1038/ng0597-17. [DOI] [PubMed] [Google Scholar]
- Goggins M, Schutte M, Lu J, Moskaluk CA, Weinstein CL, Petersen GM, Yeo CJ, Jackson CE, Lynch HT, Hruban RH, et al. Germline BRCA2 gene mutations in patients with apparently sporadic pancreatic carcinomas. Cancer Res. 1996;56:5360–4. [PubMed] [Google Scholar]
- Goggins M, Hruban RH, Kern SE. BRCA2 is inactivated late in the development of pancreatic intraepithelial neoplasia: evidence and implications. Am J Pathol. 2000;156:1767–71. doi: 10.1016/S0002-9440(10)65047-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowlby LS. Pancreatic adenocarcinoma in an adolescent male with Peutz-Jeghers syndrome. Hum Pathol. 1986;17:97–9. doi: 10.1016/s0046-8177(86)80163-0. [DOI] [PubMed] [Google Scholar]
- Giardiello FM, Welsh SB, Hamilton SR, Offerhaus GJ, Gittelsohn AM, Booker SV, Krush AJ, Yardley JH, Luk GD. Increased risk of cancer in the Peutz-Jeghers syndrome. N Engl J Med. 1987;316:1511–4. doi: 10.1056/NEJM198706113162404. [DOI] [PubMed] [Google Scholar]
- Giardiello FM, Brensinger JD, Tersmette AC, Goodman SN, Petersen GM, Booker SV, Cruz-Correa M, Offerhaus JA. Very high risk of cancer in familial Peutz-Jeghers syndrome. Gastroenterology. 2000;119:1447–53. doi: 10.1053/gast.2000.20228. [DOI] [PubMed] [Google Scholar]
- Spigelman AD, Murday V, Phillips RK. Cancer and the Peutz-Jeghers syndrome. Gut. 1989;30:1588–90. doi: 10.1136/gut.30.11.1588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sato N, Rosty C, Jansen M, Fukushima N, Ueki T, Yeo CJ, Cameron JL, Iacobuzio-Donahue CA, Hruban RH, Goggins M. STK11/LKB1 Peutz-Jeghers gene inactivation in intraductal papillary-mucinous neoplasms of the pancreas. Am J Pathol. 2001;159:2017–22. doi: 10.1016/S0002-9440(10)63053-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Su GH, Hruban RH, Bansal RK, Bova GS, Tang DJ, Shekher MC, Westerman AM, Entius MM, Goggins M, Yeo CJ, et al. Germline and somatic mutations of the STK11/LKB1 Peutz-Jeghers gene in pancreatic and biliary cancers. Am J Pathol. 1999;154:1835–40. doi: 10.1016/S0002-9440(10)65440-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng JQ, Ruggeri B, Klein WM, Sonoda G, Altomare DA, Watson DK, Testa JR. Amplification of AKT2 in human pancreatic cells and inhibition of AKT2 expression and tumorigenicity by antisense RNA. Proc Natl Acad Sci U S A. 1996;93:3636–41. doi: 10.1073/pnas.93.8.3636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miwa W, Yasuda J, Murakami Y, Yashima K, Sugano K, Sekine T, Kono A, Egawa S, Yamaguchi K, Hayashizaki Y, et al. Isolation of DNA sequences amplified at chromosome 19q13.1-q13.2 including the AKT2 locus in human pancreatic cancer. Biochem Biophys Res Commun. 1996;225:968–74. doi: 10.1006/bbrc.1996.1280. [DOI] [PubMed] [Google Scholar]
- Ruggeri BA, Huang L, Wood M, Cheng JQ, Testa JR. Amplification and overexpression of the AKT2 oncogene in a subset of human pancreatic ductal adenocarcinomas. Mol Carcinog. 1998;21:81–6. doi: 10.1002/(SICI)1098-2744(199802)21:2<81::AID-MC1>3.0.CO;2-R. [DOI] [PubMed] [Google Scholar]
- Franke TF, Yang SI, Chan TO, Datta K, Kazlauskas A, Morrison DK, Kaplan DR, Tsichlis PN. The protein kinase encoded by the Akt proto-oncogene is a target of the PDGF-activated phosphatidylinositol 3-kinase. Cell. 1995;81:727–36. doi: 10.1016/0092-8674(95)90534-0. [DOI] [PubMed] [Google Scholar]
- Friess H, Berberat P, Schilling M, Kunz J, Korc M, Buchler MW. Pancreatic cancer: the potential clinical relevance of alterations in growth factors and their receptors. J Mol Med. 1996;74:35–42. doi: 10.1007/BF00202070. [DOI] [PubMed] [Google Scholar]
- Tanno S, Mitsuuchi Y, Altomare DA, Xiao GH, Testa JR. AKT activation up-regulates insulin-like growth factor I receptor expression and promotes invasiveness of human pancreatic cancer cells. Cancer Res. 2001;61:589–93. [PubMed] [Google Scholar]
- Lynch HT, Lynch JF. Hereditary nonpolyposis colorectal cancer. Semin Surg Oncol. 2000;18:305–13. doi: 10.1002/(SICI)1098-2388(200006)18:4<305::AID-SSU5>3.0.CO;2-A. [DOI] [PubMed] [Google Scholar]
- Aarnio M, Mecklin JP, Aaltonen LA, M Nystrom-Lahti, Jarvinen HJ. Life-time risk of different cancers in hereditary non-polyposis colorectal cancer (HNPCC) syndrome. Int J Cancer. 1995;64:430–3. doi: 10.1002/ijc.2910640613. [DOI] [PubMed] [Google Scholar]
- Watson P, Lynch HT. Extracolonic cancer in hereditary nonpolyposis colorectal cancer. Cancer. 1993;71:677–85. doi: 10.1002/1097-0142(19930201)71:3<677::aid-cncr2820710305>3.0.co;2-#. [DOI] [PubMed] [Google Scholar]
- Wilentz RE, Goggins M, Redston M, Marcus VA, Adsay NV, Sohn TA, Kadkol SS, Yeo CJ, Choti M, Zahurak M, et al. Genetic, immunohistochemical, and clinical features of medullary carcinoma of the pancreas: A newly described and characterized entity. Am J Pathol. 2000;156:1641–51. doi: 10.1016/S0002-9440(10)65035-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goggins M, Offerhaus GJ, Hilgers W, Griffin CA, Shekher M, Tang D, Sohn TA, Yeo CJ, Kern SE, Hruban RH. Pancreatic adenocarcinomas with DNA replication errors (RER+) are associated with wild-type K-ras and characteristic histopathology. Poor differentiation, a syncytial growth pattern, and pushing borders suggest RER+. Am J Pathol. 1998;152:1501–7. [PMC free article] [PubMed] [Google Scholar]
- Yamamoto H, Itoh F, Nakamura H, Fukushima H, Sasaki S, Perucho M, Imai K. Genetic and clinical features of human pancreatic ductal adenocarcinomas with widespread microsatellite instability. Cancer Res. 2001;61:3139–44. [PubMed] [Google Scholar]
- Nakata B, Yashiro M, Nishioka N, Aya M, Yamada S, Takenaka C, Ohira M, Ishikawa T, Nishino H, Wakasa K, et al. Very low incidence of microsatellite instability in intraductal papillary-mucinous neoplasm of the pancreas. Int J Cancer. 2002;102:655–9. doi: 10.1002/ijc.10771. [DOI] [PubMed] [Google Scholar]
- Ghimenti C, Tannergard P, Wahlberg S, Liu T, Giulianotti PG, Mosca F, Fornaciari G, Bevilacqua G, Lindblom A, Caligo MA. Microsatellite instability and mismatch repair gene inactivation in sporadic pancreatic and colon tumours. Br J Cancer. 1999;80:11–6. doi: 10.1038/sj.bjc.6690314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kondo E, Furukawa T, Yoshinaga K, Kijima H, Semba S, Yatsuoka T, Yokoyama T, Fukushige S, Horii A. Not hMSH2 but hMLH1 is frequently silenced by hypermethylation in endometrial cancer but rarely silenced in pancreatic cancer with microsatellite instability. Int J Oncol. 2000;17:535–41. doi: 10.3892/ijo.17.3.535. [DOI] [PubMed] [Google Scholar]