Abstract
Objectives
To assess the impact of NHS walk-in centres on the workload of local accident and emergency departments, general practices, and out of hours services.
Design
Time series analysis in walk-in centre sites with no-treatment control series in matched sites.
Setting
Walk-in centres and matched control towns without walk-in centres in England.
Participants
20 accident and emergency departments, 40 general practices, and 14 out of hours services within 3 km of a walk-in centre or the centre of a control town.
Main outcome measures
Mean number (accident and emergency departments) or rate (general practices and out of hours services) of consultations per month in the 12 month periods before and after an index date.
Results
A reduction in consultations at emergency departments (–175 (95% confidence interval –387 to 36) consultations per department per month) and general practices (–19.8 (−53.3 to 13.8) consultations per 1000 patients per month) close to walk-in centres became apparent, although these reductions were not statistically significant. Walk-in centres did not have any impact on consultations on out of hours services.
Conclusion
It will be necessary to assess the impact of walk-in centres in a larger number of sites and over a prolonged period, to determine whether they reduce the demand on other local NHS providers.
What is already known on this topic
One of the objectives for NHS walk-in centres was to reduce demand on other NHS services, particularly general practitioners' services and accident and emergency departments
Studies of walk-in centres in North America have indicated that such centres do not reduce demand on other healthcare services
Studies of minor injuries units in the United Kingdom (which have some similarities with walk-in centres) indicate that these units substitute mainly for consultations in accident and emergency departments
What this study adds
The data imply that walk-in centres may moderate the increasing demand on general practice and reduce the number of consultations in accident and emergency departments
The high level of background variability in consultation rates means that any impact of a walk-in centre is not statistically significant
To draw robust conclusions about the impact of walk-in centres on other health providers will require study of a large number of sites over an extended period of time
Introduction
Forty NHS walk-in centres have been established as part of the government's commitment to modernise the NHS.1 These centres are primarily nurse led and offer a drop-in service with wide opening hours in convenient locations. One aim of NHS walk-in centres is to reduce demand on other NHS providers, particularly general practitioners and accident and emergency departments in hospitals, by providing advice and treatment for minor illnesses and injuries that do not require the attention of a doctor. However, critics of walk-in centres have indicated that increasing the accessibility of care may increase total demand on the NHS, without reducing the workload of existing services.2 People may attend walk-in centres when they would have previously managed the problem themselves, or they may attend walk-in centres as well as, rather than instead of, existing services.
Studies of walk-in centres in North America have not shown that the centres are likely to reduce the workload of other neighbouring health services.3,4 In the United Kingdom research on nurse led units for minor injuries (which have some similarities with walk-in centres) has shown that people use the units mainly as an alternative to accident and emergency departments rather than as an alternative to general practice.5,6 Whether these findings are relevant to the introduction of walk-in centres in the NHS is not clear.
The implementation of NHS walk-in centres has been subject to a comprehensive independent national evaluation. We describe one component of this evaluation, the impact of walk-in centres on the workload of other NHS providers in the surrounding area.
Methods
We identified a purposive sample of 10 walk-in centre sites in England, taking into account both the geographical spread of locations and the type of services offered by the centre. For each site we selected as a control site a town of similar size, in the same region, but as distant as possible from any existing walk-in centre.
We asked the health authorities for each of these 20 sites to provide lists of all general practitioners' surgeries within 3 km of the walk-in centre (or town centre in control sites), the accident and emergency department closest to the walk-in centre or town centre, and the largest general practitioners' out of hours service covering the walk-in centre or town centre. We randomly selected eight general practices in each location, stratified by size (three or fewer partners and four or more partners). These eight practices, together with the relevant emergency department and out of hours provider in each of the 20 chosen sites, formed the sampling frame of healthcare providers for the study. We asked each provider to supply anonymised data relating to their workload in the 12 month periods before and after an index date. This index date varied from location to location since it reflected the opening date of the local walk-in centre or, in the case of control sites, the opening date of the walk-in centre in the matched site. All face to face consultations involving general practitioners were included, along with any consultations with a practice nurse where practices recorded these throughout the whole period.
Analyses
The primary workload variable for general practitioners' surgeries and out of hours services was the monthly consultation rate (the number of consultations each month divided by the size of the respective list of patients). For accident and emergency departments, where no suitable denominator was available, we used the number of consultations per month for each department as the indicator of workload.
For each of the three service types, we calculated the mean workload for each month for walk-in centre sites and control sites. We plotted this against time on a graph that also included best fit trend lines. These were obtained from generalised linear models applied separately—to data over 24 months from control sites, to data from the 12 months before opening for walk-in centre sites, and to data from the 12 months after opening for walk-in centre sites. The independent variables were index month (coded from –11 to +11, where 0 was the month of opening) and site status (walk-in centre or control sites).
A second set of models estimated change in workload for control and for walk-in centre sites, with a binary timing variable (before or after the index month of opening) included as the only independent variable in models estimated separately for the two types of site.
A third model included index month, site status, timing, and the interaction between timing and site status as independent variables, with the interaction term giving an estimate of the difference in change in workload between the control sites and walk-in centre sites. We also estimated final models with calendar month, consultation type, and matched set included as covariates, to adjust for seasonal effects or any variation in the type of consultations included in the data.
All models reflected the correlated nature of the repeated measures data by adjusting for the relatedness of sequential observations over time, using generalised estimating equation models that identify the best autoregressive structure to fit the data. All models also took account of the small number of services sampled by using robust variance estimators. Finally, we examined all residuals and re-estimated certain models to check that the findings were substantively unaffected by the omission or inclusion of highly influential observations.
Results
For both walk-in centre sites and control sites, we received data from 20 general practitioners' surgeries (25% response rate), 10 emergency departments (100% response rate), and seven out of hours services (70% response rate) (table 1). Of the 20 general practitioners' responses in both groups, seven were from practices with four or more partners and 13 were from practices with two or three partners. None of the responding practices was single handed.
Table 1.
Numbers of responding general practices
| Walk-in centre location
|
No in each walk-in centre location (n=20)
|
No in matched control location (n=20)
|
|---|---|---|
| A | 5 | 5 |
| B | 5 | 4 |
| C | 3 | 1 |
| D | 1 | 3 |
| E | 0 | 2 |
| F | 0 | 1 |
| G | 1 | 1 |
| H | 2 | 1 |
| I | 2 | 1 |
| J | 1 | 1 |
Impact on accident and emergency departments
Among the 10 accident and emergency departments in towns with walk-in centres the mean number of consultations per month increased slightly, from 5267 in the year before the walk-in centre opened to 5316 in the following year (table 2). However, this increase was driven largely by an artefactual increase in consultations at one site, where the accident and emergency department merged with another department during the 10th month of our data collection at that particular site. Once this had been adjusted for by including in the model a fixed term indicator variable for all measurements in one site after the 10th month, consultations were estimated to have fallen by 173.3 (95% confidence interval –334 to –12) per month per site after the walk-in centre opened.
Table 2.
Consultations per healthcare provider before and after opening of walk-in centres
| Mean No of consultations per month
|
Rate per 1000 registered patients per month (95% CI)
|
Change (95% CI)
|
||||
|---|---|---|---|---|---|---|
| Before*
|
After*
|
Before*
|
After*
|
|||
| Walk-in centre sites: | ||||||
| Emergency departments† | 5267 | 5316 | — | — | −173.3 (−334 to −12) | |
| Out of hours services | 2690 | 2650 | 11.4 (7.2 to 15.7) | 11.3 (6.6 to 16.1) | −0.09 (−0.63 to 0.44) | |
| General practitioners | 1661 | 1686 | 258 (229 to 286) | 261 (229 to 293) | 3.9 (−13.9 to 21.7) | |
| Control sites: | ||||||
| Emergency departments | 5769 | 5766 | — | — | −3 (−145 to 139) | |
| Out of hours services | 2296 | 2200 | 12.3 (8.8 to 15.8) | 11.8 (8.4 to 15.1) | −0.5 (−0.95 to −0) | |
| General practitioners | 1867 | 2040 | 256 (217 to 295) | 279 (247 to 312) | 23.7 (−8.0 to 55.3) | |
Based on 12 months of data.
Model includes fixed effect indicator variable for all measurements from month 10 onwards at one site.
We anticipated that the impact of walk-in centres on the workload of accident and emergency departments would be greatest where the walk-in centre shared its location with the accident and emergency department, as was the case in three of the sites. An analysis of change in consultations in these three sites alone showed a reduction of 349 (–696 to –2) consultations per site per month. By contrast, the change in workload among the 10 accident and emergency departments in control sites over the 24 months for which data were collected was negligible (–3 (–145 to 139) consultations per site per month).
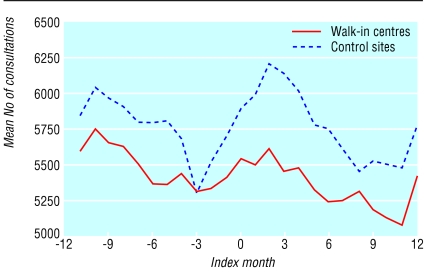
Figure 1 shows the mean consultations per month for both the walk-in centre and control sites separately; data from one site were excluded. The lines, although irregular (representing fluctuations in workload from month to month) are roughly in parallel. A slight divergence is, however, indicated in the year after the opening of the walk-in centres, with consultation numbers slightly lower in the walk-in centre sites.
Figure 1.
Mean number of consultations per month across nine emergency departments in the 12 months before and after the opening of a walk-in centre
The trend towards a reduction in the number of consultations is further supported by the final model of accident and emergency departments' workload, which estimates that, since a term for observations after month 10 was included at one site (as well as consultation type, calendar month, baseline difference, and matched set), 175 fewer consultations per month took place in accident and emergency departments in walk-in centre towns than in control towns in the year after opening. However, this difference is not statistically significant (95% confidence interval –387 to 36, P=0.11). Even when we re-estimated this final model, taking into account only those three pairs of sites where the walk-in centre shared its location with an accident and emergency department, the overall effect was larger (264 (–651 to 122) fewer consultations per month), but it was not significant (P=0.18) because of the small sample size.
Impact on general practice
Among general practices in sites with walk-in centres, we noted a small increase in workload in the year after the centre had been opened of 3.9 (–13.9 to 21.7) consultations per 1000 patients per month, compared with a larger increase of 23.7 (–8.0 to 55.3) among practices in control sites.
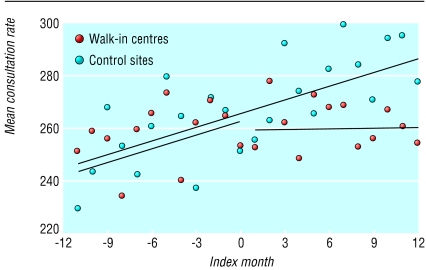
Figure 2 shows that in the year before the walk-in centres opened consultation rates increased steadily in practices in both control and walk-in centre locations. After the centres opened, however, the increasing trend continued in control sites but levelled off in the walk-in centre sites.
Figure 2.
Consultation rate per month in general practices in walk-in centre sites and control sites. The lines represent the mean
The final model of the workload of general practices estimated that in the year after the walk-in centres opened the practices in walk-in centre sites had 19.8 fewer consultations per 1000 patients per month than control sites (–53.3 to 13.8, P=0.25).
Impact on out of hours services
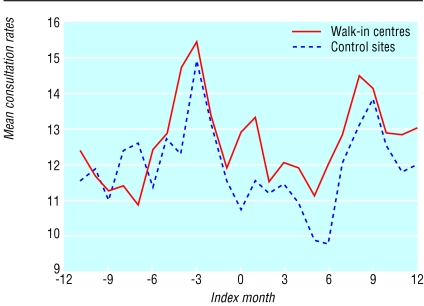
Consultation rates for out of hours services decreased slightly at both walk-in centre sites and control sites over the period of the study (table 1). Figure 3 shows the data for all out of hours sites over the 24 month monitoring period.
Figure 3.
Mean consultation rate per month across out of hours services in the 12 months before and after the opening of walk-in centres
The final adjusted model estimated the net difference in consultation rates between the control and walk-in centre sites as a reduction that is 0.38 per 1000 per month greater in control sites than in walk-in centre sites (–0.26 to 1.02, P=0.242). This effect is not statistically significant, nor do the graphs show any impact of walk-in centre opening on rates of consultations of out of hours services.
Discussion
Consultation rates at accident and emergency departments in towns with walk-in centres may be reduced slightly, especially in towns where the walk-in centre shares its location with the emergency department. In general practices, workload increased in both walk-in centre sites and control sites in the 12 months before walk-in centres opened, but this rise continued for the following 12 months only at control sites. Out of hours services showed little change in consultation rates at either walk-in centre or control sites. However, none of these apparent changes was statistically significant, and the research has several important limitations.
Limitations of the study
Firstly, the relatively short period of follow up (providing few data points for analysis), combined with the small number of sites and the wide variation between them in workload, leads to findings that do not reach statistical significance. Secondly, although walk-in centre sites were matched to control sites to account for seasonal and regional effects on workload, other local confounding factors may have influenced activity at one or more sites. Thirdly, the results for general practices may not be representative, for several reasons. Only a minority (25%) of general practices were able or willing to supply data about the number of consultations at their practices, and the responding practices were not evenly distributed across our chosen 20 sites. However, sites with four or five responding practices will not have an undue influence on the results since the statistical analyses are appropriately conservative, taking full account of the clustering of practices within sites and of the matched sites. Furthermore, none of the responding practices was single handed, possibly because practices may not have been able to supply the data we requested unless they had computerised appointment systems. However, it is difficult to conceive that any impact of walk-in centres on workload would have a differential effect on those practices able to supply data, so the low response rate may be less of a problem than it would be in a questionnaire survey of opinion. Fourthly, this study was based on routinely collected data extracted by the sites themselves and may be of uncertain reliability.
Settings
Walk-in centres vary considerably in terms of their setting and the services they provide. Some are located next to accident and emergency departments, some are in hospitals without this facility, and some are in shopping centres. Others share their location with primary care facilities such as general practitioners' cooperatives or health centres. In this study, centres of different types were purposively selected and analysed together. However, certain types of centre are likely to have differential impacts on the workload of other types of health service provider. A further sustained period of evaluation will be needed to disentangle the relation between setting, model of walk-in centre organisation, and impact on other local services, starting with a clear description of the theoretical basis by which different models of service may have predictable effects in different contexts.7
Even if walk-in centres reduce demand on other healthcare providers, this reduction is efficient only if walk-in centres provide care more economically. Consultations with nurses in walk-in centres are considerably longer than those with doctors in general practice,8 and nurse led care may therefore not necessarily be cheaper. This is consistent with other research about the work of nurse practitioners in primary care settings.9 It is also important to consider the overall efficiency of walk-in centres, taking into account the extent to which they act as an additional, substitute, or duplicate service, as well as the costs of care in different settings. These issues are considered in other components of the national evaluation of walk-in centres.10
Twelve months is a relatively short time in which to assess the impact of a walk-in centre. Throughput of patients at walk-in centres increased steadily over the first few months after centres opened, but it is still too early to predict how patients will use walk-in centres in the longer term until they have become used to the facilities that different healthcare services have to offer. Judging the true impact of a walk-in centre on the workload of other NHS providers will require the participation of a larger number of sites and a longer period of follow up.
This study illustrates the tension between the desire of policy makers to learn lessons at an early stage from a small sample of sites piloting a new initiative and the difficulty of obtaining robust quantitative evidence about the impact of the initiative.
Acknowledgments
We thank the staff at general practices, accident and emergency departments, and out of hours services who provided the data on which this study is based. This research was conducted on behalf of the National Evaluation of NHS Walk-in Centres Team in Bristol.
Footnotes
Funding: This research has been conducted independently by the University of Bristol, funded by the Department of Health. The views expressed in this publication are those of the authors and not necessarily those of the Department of Health.
Competing interests: None declared.
References
- 1.Department of Health. Up to £30 million to develop 20 fast access walk-in centres. Press release 1999/0226. London: DoH; 1999. [Google Scholar]
- 2.Royal College of General Practitioners. Discussion paper on the implications for general practice of NHS Direct and walk-in centres. London: RCGP, NHS Alliance; 1999. [Google Scholar]
- 3.Bell NR, Szafran O. Use of walk-in clinics by family-practice patients. Can Fam Physician. 1992;38:507–513. [PMC free article] [PubMed] [Google Scholar]
- 4.Ferber M, Becker L. Impact of freestanding emergency centers on hospital emergency department use. Ann Emerg Med. 1983;12:429–433. doi: 10.1016/s0196-0644(83)80340-0. [DOI] [PubMed] [Google Scholar]
- 5.Heaney D, Paxton F. Evaluation of a nurse-led minor injuries unit. Nurs Stand. 1997;12:35–38. doi: 10.7748/ns1997.10.12.4.35.c2484. [DOI] [PubMed] [Google Scholar]
- 6. Salisbury C, Munro J. Walk-in centres in primary care: a review of the international literature. Br J Gen Pract (in press). [PMC free article] [PubMed]
- 7.Pawson R, Tilley N. Realistic evaluation. London: Sage; 1997. [Google Scholar]
- 8.Salisbury C, Chalder M, Manku-Scott T, Pope C, Moore L. What is the role of walk-in centres in the NHS? BMJ. 2002;324:399–402. doi: 10.1136/bmj.324.7334.399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Horrocks S, Anderson E, Salisbury C. Systematic review of whether nurse practitioners working in primary care can provide equivalent care to doctors. BMJ. 2002;324:819–823. doi: 10.1136/bmj.324.7341.819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Coast J, Noble SM, Chalder M, Baxter K, Peters TJ, Salisbury C. Walk-in centres: a cost analysis. Submitted to Br J Gen Pract Sept 2002.