Abstract
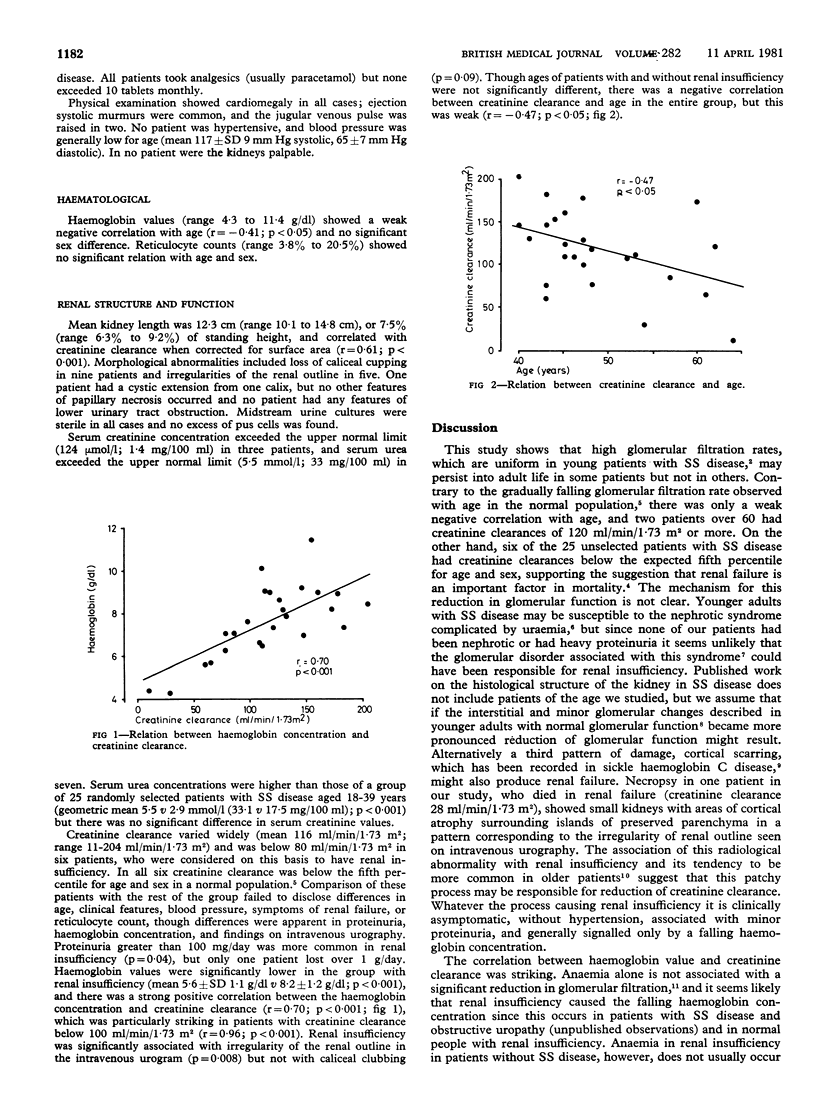
Renal function was examined in 25 patients aged 40-64 with homozygous sickle-cell (SS) disease. Investigations included intravenous urography and measurement of blood urea and creatinine concentrations and creatinine and protein excretion in 24-hour collections of urine. Serum creatinine concentrations did not differ significantly from those of 25 other patients with SS disease aged 18-39 years, but serum urea concentrations were significantly higher (p less than 0.001). Intravenous urography showed loss of caliceal cupping (nine patients), irregular renal outline (five), and cystic extension from the calix (one). Six patients had creatinine clearances below the fifth percentile for age and sex. Proteinuria was more common in these patients, and haemoglobin concentrations were much lower than in the 19 patients without renal insufficiency (mean 5.6 v 8.2 g/dl; p less than 0.001). Haemoglobin concentration was strongly correlated with creatinine clearance (r=0.70), particularly with clearances below 100 ml/min/1.73 m2 (r=0.96; p less than 0.001). A possible mechanism of renal insufficiency in SS disease is cortical scarring, which is asymptomatic, not associated with hypertension, and accompanied by only minor proteinuria. A falling haemoglobin concentration is a sensitive and early indicator of renal impairment in SS disease.
Full text
PDF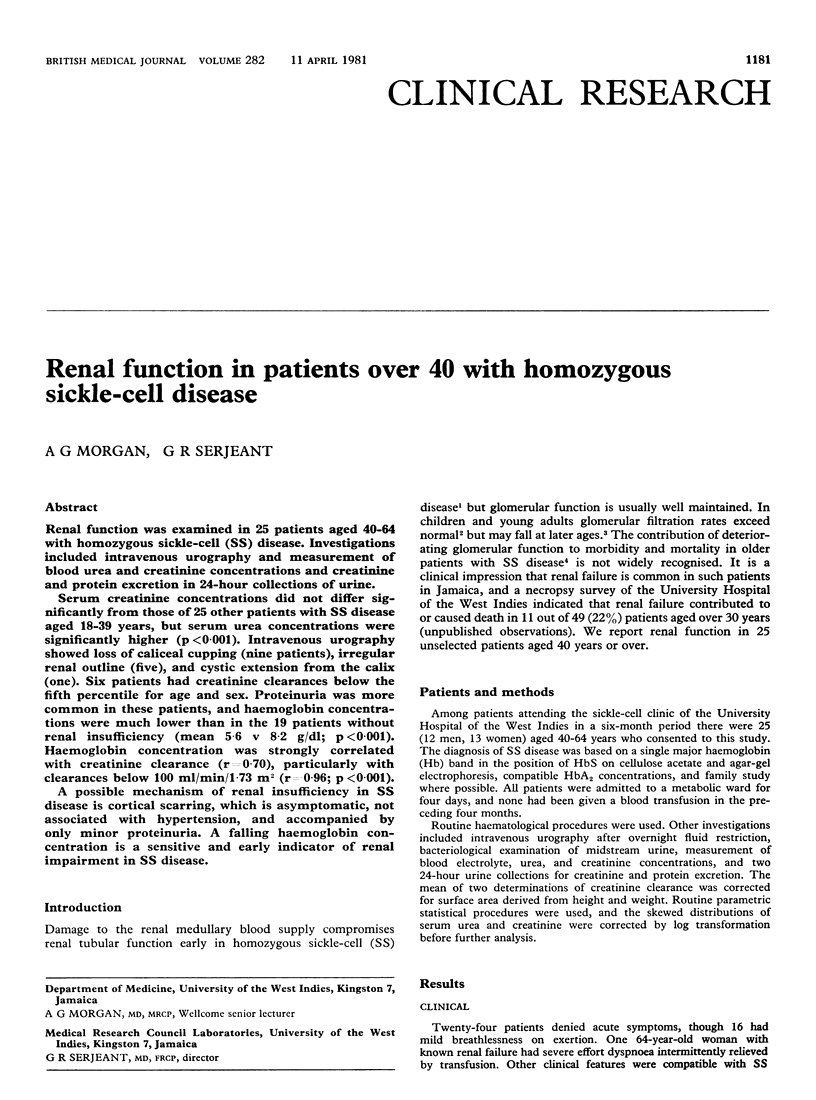
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- ETTELDORF J. N., SMITH J. D., TUTTLE A. H., DIGGS L. W. Renal hemodynamic studies in adults with sickle cell anemia. Am J Med. 1955 Feb;18(2):243–248. doi: 10.1016/0002-9343(55)90239-4. [DOI] [PubMed] [Google Scholar]
- ETTELDORF J. N., TUTTLE A. W., CLAYTON G. W. Renal function studies in pediatrics. 1. Renal hemodynamics in children with sickle cell anemia. AMA Am J Dis Child. 1952 Feb;83(2):185–191. doi: 10.1001/archpedi.1952.02040060051005. [DOI] [PubMed] [Google Scholar]
- ITANO H. A., KEITEL H. G., THOMPSON D. Hyposthenuria in sickle cell anemia: a reversible renal defect. J Clin Invest. 1956 Sep;35(9):998–1007. doi: 10.1172/JCI103360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- KASANEN A., KALLIOMAKI J. L. Correlation of some kidney function tests with hemoglobin in chronic nephropathies. Acta Med Scand. 1957 Sep 6;158(3-4):213–219. doi: 10.1111/j.0954-6820.1957.tb15484.x. [DOI] [PubMed] [Google Scholar]
- McCall I. W., Moule N., Desai P., Serjeant G. R. Urographic findings in homozygous sickle cell disease. Radiology. 1978 Jan;126(1):99–104. doi: 10.1148/126.1.99. [DOI] [PubMed] [Google Scholar]
- McCoy R. C. Ultrastructural alterations in the kidney of patients with sickle cell disease and the nephrotic syndrome. Lab Invest. 1969 Aug;21(2):85–95. [PubMed] [Google Scholar]
- Pardo V., Strauss J., Kramer H., Ozawa T., McIntosh R. M. Nephropathy associated with sickle cell anemia: an autologous immune complex nephritis. II. Clinicopathologic study of seven patients. Am J Med. 1975 Nov;59(5):650–659. doi: 10.1016/0002-9343(75)90226-0. [DOI] [PubMed] [Google Scholar]
- Pitcock J. A., Muirhead E. E., Hatch F. E., Johnson J. G., Kelly B. J. Early renal changes in sickle cell anemia. Arch Pathol. 1970 Nov;90(5):403–410. [PubMed] [Google Scholar]
- ROSCOE M. H. Anaemia and nitrogen retention in patients with chronic renal failure. Lancet. 1952 Mar 1;1(6705):444–445. doi: 10.1016/s0140-6736(52)91954-5. [DOI] [PubMed] [Google Scholar]
- Rowe J. W., Andres R., Tobin J. D. Letter: Age-adjusted standards for creatinine clearance. Ann Intern Med. 1976 May;84(5):567–569. doi: 10.7326/0003-4819-84-5-567. [DOI] [PubMed] [Google Scholar]


