Abstract
The dengue virus type 2 structures probably involved in human virulence were previously defined by sequencing the complete genome of both American and Southeast (SE) Asian genotype templates in patient serum (K. C. Leitmeyer et al., J. Virol. 73:4738-4747, 1999). We have now evaluated the effects of introducing a mutation in the envelope glycoprotein (E) gene and/or replacement of 5′- and 3′-nontranslated regions on dengue virus replication in human primary cell cultures. A series of chimeric infectious clones were generated containing different combinations of American and SE Asian genotype sequences. Some of the chimeric viruses had altered plaque morphology in mammalian cells; however, they replicated at similar rates in mosquito cells as measured by quantitative reverse transcription-PCR and plaque assay. Although susceptibility to virus infection varied from donor to donor in experiments using human macrophage and dendritic cells, we were able to measure consistent differences in viral RNA output per infected cell. Using this measurement, we demonstrated that the chimeric virus containing the E mutation had a lower virus output compared to the parental infectious clone. A larger reduction in virus output was observed for the triple mutant and the wild-type, American genotype virus from which chimeric inserts were derived. It appears that the three changes function synergistically, although the E mutation alone gives a lower output compared to the 5′- and 3′-terminal mutations. The data suggest that these changes may be responsible for decreased dengue virus replication in human target cells and for virulence characteristics during infection.
Dengue viruses are members of the genus Flavivirus (family Flaviviridae) and are grouped into four distinct serotypes, 1 through 4. In addition to producing subclinical dengue virus infection, illnesses range from dengue fever (DF), a mild, flu-like syndrome with rash, to dengue hemorrhagic fever (DHF), a severe and sometimes fatal disease, characterized by capillary leakage, thrombocytopenia, and occasionally hypovolemic shock (for a review, see reference 14). It is estimated that more than 50 million human dengue virus infections occur annually and 2.5 billion people are at risk of dengue virus infection worldwide (61).
The lack of an in vitro or animal model for severe dengue disease has hampered the identification of mechanisms by which dengue progresses to DHF. However, a number of models have been proposed, based on epidemiologic and experimental data, to explain severe disease pathogenesis. One proposed mechanism, antibody-dependent enhancement (ADE), arose from the observation that secondary infection with a heterotypic dengue virus is associated with an increased risk of developing DHF and experiments demonstrating that subneutralizing concentrations of antibodies can increase virus titers in primates and in vitro (15, 18, 21, 31). The role of host immune factors has been examined in a number of studies that have implicated different cytokines, interferon, and abnormalities in coagulation, which may increase capillary permeability, the hallmark of DHF (3, 25, 26, 38, 50, 60).
Recent reports have indicated that viral factors are also involved in increased pathogenesis (37, 51, 52). In some areas of the world, secondary infection by some dengue type 2 viruses does not produce severe disease, in contrast to the aforementioned ADE model (23, 24, 45, 59). Within dengue virus serogroups, viruses can be classified, by nucleotide sequence comparisons, into genotypes. The first cases of DHF in the Americas were reported in Cuba in 1981, and this coincided with the introduction of the Southeast (SE) Asian genotype of serotype 2 into this hemisphere (51). Since then, other countries in the Americas have reported DHF associated with dengue serotype 2 viruses of the SE Asian genotype and not the indigenous American genotype (52). These data suggest that, within serotype 2 viruses, a specific genotype may have the propensity to cause DHF, whereas other genotypes are associated with the less severe DF.
To understand the differences between SE Asian and American dengue virus genotypes, 11 viral genomes were sequenced directly from patient plasma (37). A number of mutations conserved among genotype representatives were identified throughout the RNA genomes in both protein coding and nontranslated regions (ntr's). Amino acid differences that altered the charge were observed in the premembrane protein (prM; amino acid 28 Glu→Lys), the envelope glycoprotein (E; amino acid 390 Asn→Asp), the nonstructural protein 4B (NS4B; amino acid 17 Ser→His), and NS5 (amino acids 645 Asn→Asp, 676 Ser→Arg, and 800 Lys→Ser). Changes within the ntr's were predicted to alter secondary structures at both ends of the genome. Although these differences were observed between the genotypes, no specific mutations were identified that correlated with DHF versus DF, as had been shown by comparison of strains of the SE Asian genotype alone (43).
In support of the hypothesis that specific structural differences between the SE Asian and American genotypes may affect pathogenesis, it has been reported that substitutions at amino acid 390 within the E gene results in a reduction of virus output from monocyte-derived macrophage (MDM) cultures (48). However, dengue virus has been shown to infect dendritic cells (DCs), including endogenous human skin Langerhans cells and monocyte-derived DCs at much higher rates (62). These cells are the likely initial targets of dengue virus infection, and this event results in DC maturation and activation (25, 38). Thus, we chose to use primary human cell cultures to test the effect of different dengue virus structures on replication in its presumed natural infection targets. In addition to evaluating the American genotype amino acid substitution within the E glycoprotein at amino acid 390, both the 5′- and 3′-terminal American sequences were inserted into a SE Asian-derived infectious clone. Chimeras were then examined in relevant cell cultures, specifically mosquito and human primary cultures (MDMs and DCs), to determine whether American genotype structures alter the efficiency of replication of an infectious clone.
MATERIALS AND METHODS
Cell lines and viruses.
African green monkey kidney cells (Vero E6), were maintained in minimum essential media (MEM) with Eagle salts (Sigma, St. Louis, Mo.) supplemented with 5% heat-inactivated fetal calf serum (FCS; Atlanta Biologicals, Norcross, Ga.), 2 mM glutamine, 100 U of penicillin/ml, and 100 μg of streptomycin/ml (Gibco-BRL, Rockville, Md.). The Aedes albopictus cell line (C6/36) was maintained in MEM with Eagle salts supplemented with 5% FCS, 2 mM glutamine, 0.1 mM nonessential amino acids, 1 mM sodium pyruvate (Gibco-BRL), 100 U of penicillin/ml, and 100 μg of streptomycin/ml. Dengue virus strain 16681 (passaged several times in BS-C-1 cells, LLC-MK2 p.8, rhesus macaque p.1, Toxorhynchites amboinensis mosquito p.2, PGMK p.1, and C6/36 p.4) was obtained from Richard Kinney (Centers for Disease Control, Fort Collins, Colo.) and was passaged one additional time in C6/36 cells. Human serum, which had been used to recover full-length genome sequences (37), was used to isolate strain IQT2913, and this was passaged up to four times to generate high-titer stocks. A 16681-derived infectious clone, D2/IC-30P-A (30), was obtained as plasmid DNA from Richard Kinney and virus stock was prepared as described below.
Construction of chimeric infectious clones.
A SE Asian genotype virus backbone, 16681, was modified at three sites by inserting SE Asian or American genotype virus sequences, obtained by reverse transcription-PCR (RT-PCR) amplification, to generate six different infectious clones, as follows (Fig. 1).
FIG. 1.
Schematic of chimeric dengue type 2 infectious clones. The D2/IC-30P-A SE Asian infectious clone is depicted showing viral proteins, ntr's (5′ ntr and 3′ ntr), and two restriction sites (SalI and HpaI) used for the cloning of the chimeric viruses. Chimeric viruses are depicted with parental sequences shown as open boxes, with inserts in gray or black. The SE Asian insert from K0008 is depicted as a gray box for virus D2/IC-3ntrK. American genotype inserts from IQT2913 are depicted as black boxes for the viruses D2/IC-3ntrIQT, D2/IC-5ntrIQT, D2/IC-5+3ntrIQT, D2/IC-Em, and D2/IC-5E3IQT.
(i) 3′-End chimeras were generated by replacing nucleotides (nt) 10130 to 10723 of 16681 (GenBank accession number U87411) with sequences from another SE Asian strain (K0008; GenBank accession number AF100459) or an American strain (IQT2913; GenBank accession number AF100468). In addition to replacing the 3′ ntr, this cassette substitution replaced 184 nt of the NS5 terminus. Primer RC001 (5′-CTC ACG AATTCG GTT AAC AAG CAG-3′) and primer Xbal (5′-GCT CTA GAG AAC CTG TTG ATT CAA C-3′) were used to PCR amplify a 620-nt fragment from the 3′ end of dengue virus strain K0008 (37). Primer RC002 (5′-CTC ACG AAT TCG GTT AAC AAG CAG AGC-3′) and primer Xbal were used to PCR-amplify a 610-nt fragment from the 3′ end of dengue virus strain IQT2913 (37). Both PCR fragments were cloned into pGEM-11Zf+ (Promega, Madison, Wis.) by using EcoRI and XbaI restriction sites introduced during the PCR amplification, generating plasmids pD2/3ntrK and pD2/3ntrIQT. Sequences were confirmed by using methods previously described (37). The 1.8-kb EcoRI-HindIII fragment from pD2/IC-30P-A, nt 8959 to 10726, which includes a terminal portion of NS5 and all of the 3′ ntr, was cloned into pGEM-11Zf+ to generate the plasmid pD2/EH. The HpaI-XbaI fragment (nt 10125 to 10722) from pD2/EH was replaced with the HpaI-XbaI fragments from pD2/3ntrK and pD2/3ntrIQT, generating pD2/EHK and pD2/EHIQT, respectively. Lastly, the AvrII-XbaI fragments from pD2/EHK and pD2/EHIQT were cloned into pD2/IC-30P-A to generate full-length clones pD2/IC-3ntrK and pD2/IC-3ntrIQT (Fig. 1). Within the NS5 coding region, pD2/IC-3ntrK differed from pD2/IC-30P-A by 4 nt at positions 10143 (C→A), 10185 (C→T), 10200 (A→G), and 10263 (T→C), and all of these were silent mutations. Plasmid pD2/IC-3ntrIQT differed from pD2/IC-30P-A by 15 nt in the NS5 coding region: positions 10137 (G→A), 10149 (A→G), 10155 (C→T), 10161 (A→G), 10162 (G→A), 10173 (T→C), 10179 (T→C), 10188 (T→C), 10191 (A→T), 10200 (A→G), 10236 (C→T), 10242 (A→G), 10254 (A→G), 10256 (C→T), and 10264 (C→T). Only the nucleotide change at position 10162 resulted in a coding change at position 865 (Ala→Thr) within the NS5 protein; this change from a nonpolar, hydrophobic amino acid to an uncharged polar, hydrophilic amino acid was not unique to the American genotype; an identical change has been found in other SE Asian genotype viruses (including strain New Guinea C).
(ii) 5′-End chimeras were generated by replacing nt 1 to 165 of 16681 with sequences from American genotype strain IQT2913. In addition to replacing the 96 nt of the 5′ ntr, 69 nt of the capsid protein (C) open reading frame (ORF) were substituted during the cloning process. Initially, the 1,400-nt SacI-SphI fragment from pD2/IC-30P-A was cloned into the homologous restriction sites within the pUC18 plasmid to generate the plasmid pD2/Sac-Sph. PCR was used to amplify a 165-nt fragment from the 5′ region of dengue virus strain IQT2913, with primers D2/11v (37) and GN001 (5′-GCA CAG TCG ACA CGC GG-3′). The GN001 primer introduced a point mutation at nt 168 to generate a SalI restriction site that is present in the D2-IC/30P-A infectious clone. The PCR fragment was then digested with BlpI and SalI, and the resulting 120-nt fragment was used to replace the BlpI-SalI fragment of pD2/Sac-Sph, generating plasmid pD2/5ntrIQT. Lastly, the SacI-SphI fragment from pD2/5ntrIQT was used to replace the homologous fragments from pD2/IC-30P-A and pD2/IC-3ntrIQT to generate the full-length clones pD2/IC-5ntrIQT and pD2/IC-5+3ntrIQT, respectively (Fig. 1). This substitution resulted in a single nucleotide change within C that produced a point mutation at amino acid 9 (Lys→Arg); however, this change did not affect the basic charge of the amino acid at that position.
(iii) E mutants were also generated. Initially, the 3,113-nt SphI-KpnI fragment from pD2/IC-30P-A was cloned into pUC18 to generate the plasmid pD2/SK. To introduce the A→G point mutation at nt 2104 (resulting in the Asn-to-Asp mutation within the E glycoprotein at amino acid 390), an upstream PCR product was generated with primers D2/616v (37) and RC-BAK (5′-CTT TCT TAA ACC AGT CGA GCT TCA GTT GTC C-3′). A downstream PCR product was generated with primers D2/2578 (37) and RC-FOR (5′-GGA CAA CTG AAG CTC GAC TGG TTT AAG AAA G-3′). The 1,962-nt PCR fragment was then amplified by using only the outside primers, D2/616v and D2/2578, in a reaction with both the upstream and the downstream PCR products described above. The 507-nt BamHI fragment, containing the E glycoprotien mutation, was cloned into pD2/SK to generate pD2/SKEm. Once the sequence was confirmed, the SphI-KpnI fragment from pD2/SKEm was cloned into pD2/IC-30P-A and pD2/IC-5+3ntrIQT to generate plasmids pD2/IC-Em and pD2/IC-5E3IQT (Fig. 1).
Generation of chimeric virus stocks.
The protocol for generating virus stocks from the infectious clones was followed as described previously (30), with minor modifications. Plasmid DNAs, including the D2/IC-30P-A parental clone, were linearized with XbaI, and capped, in vitro transcripts were produced by using 7mG-A cap analogue (Epicentre Technologies, Madison, Wis.) with the T7 MegaScript kit (Ambion, Austin, Tex.). Transcription reactions for capped RNAs were set up as described by the manufacturer, with the exception that ATP was diluted 1:1 instead of 1:6, to increase the yield of full-length RNAs. After the reactions were incubated for 6 h at 37°C, DNA strands were removed by digestion with DNase for 15 min at 37°C. RNAs were precipitated by using LiCl2, and the pellets were washed once with 70% ethanol. A sample from each of the transcription reactions was electrophoresed on 1% agarose, 0.25× Tris-borate-EDTA gels and stained with ethidium bromide to demonstrate that the RNAs were intact prior to electroporation. All of the RNAs were electroporated into C6/36 cells under conditions described previously (30). The electroporated cells were seeded in maintenance media (MEM, 2.0 mM glutamine, 0.1 mM nonessential amino acids, 1 mM sodium pyruvate, 100 U of penicillin/ml, 100 mg of streptomycin/ml, 2% FCS), and 7 days later dengue virus infection was confirmed by using an indirect fluorescent antibody assay (55); virus stocks were harvested when >90% of the cells were positive for dengue virus antigen (usually 7 to 9 days). Some of the chimeric viruses were passaged one additional time in C6/36 cells to generate high-titer stocks.
Virus quantitation. (i) Plaque assay.
Vero cells were seeded at a density of 3.0 × 104 to 4.0 × 104 cells/cm2 and allowed to attach overnight in either 6- or 12-well plates. Virus dilutions, prepared in MEM without FCS and either 0.4 ml or 0.1 ml of the inoculum, for 6- and 12-well plates, respectively, were incubated on the cells for 90 min. The inoculum was removed from the six-well plates, and 4.0 ml of overlay (1× MEM containing Eagle salts, 2% FCS, 2 mM glutamine, 100 U of penicillin/ml, 100 μg of streptomycin/ml, and 1% SeaKem LE agarose [FMC Bioproducts, Rockland, Maine]) was added to each well. The inoculum was not removed from the 12-well plates prior to the addition of 2.0 ml of carboxymethylcellulose (CMC) overlay (MEM containing Eagle salts, 2% FCS, 2 mM glutamine, 100 U of penicillin/ml, 100 μg of streptomycin/ml, and 8.4 g CMC/liter [1,500 cP; Sigma]) to each well. Cells were fixed 7 to 9 days postinfection with 10% formaldehyde and stained with crystal violet, and plaques were counted.
(ii) Quantitative, real-time RT-PCR.
The conditions used for the quantitative RT-PCR were described previously (2). In brief, 5 μl of Trizol-extracted (Invitrogen, Rockville, Md.) RNA in diethyl pyrocarbonate-treated water was amplified in a 50-μl final reaction volume by using the Brilliant Single-Step Quantitative RT-PCR kit (Stratagene, La Jolla, Calif.). Each reaction contained final concentrations of 1× core RT-PCR buffer, 5.5 mM MgCl2, 0.8 mM deoxynucleoside triphosphates (dATP, dGTP, dCTP, and dTTP), 100 nM PA-1, 100 nM PA-4, and 100 nM PRB, plus 1.25 U of StrataScript RT, 80 pM reference dye, 10 U of RNase inhibitor, and 2.5 U of SureStart Taq DNA polymerase. Amplification and detection were performed on an ABI Prism 770 sequence detection instrument (PE Biosystems, Foster City, Calif.) by using the following conditions: 50°C for 30 min (1 cycle), 95°C for 10 min (1 cycle), and then 35 cycles of 95°C for 15 s and 64°C for 1 min. A standard curve generated by using an in vitro-transcribed RNA (2) was used to estimate the RNA copy number present in each sample.
Infection of C6/36 cells.
Genome equivalents were used to standardize the input amounts or infectious dose for all of the viruses since some chimeric dengue viruses did not produce distinct plaques. Cells were seeded at 1.5 × 104 to 2.5 × 104 cells per well in 24-well plates and the following day were infected with 1,000 genome Eq/cell in MEM without FCS. The inoculum was allowed to adsorb to the cells for 1 h at 28°C, with occasional rocking; cells were washed three times with 1.0 ml of phosphate-buffered saline (PBS) to remove residual, cell-free virus, and 1.0 ml of maintenance medium was added to each well. Cell supernatants were harvested every 24 h for 6 days, and all of the samples were monitored for viral RNA accumulation by using quantitative RT-PCR. In addition, some of the samples were titrated by plaque assay to validate the quantitative RT-PCR results. Cell supernatant was clarified by low-speed centrifugation at 800 × g for 5 min, and 100 μl was Trizol extracted according to the manufacturer's protocol, with 15 μg of glycogen used as the carrier for pelleting. FCS was added to the remaining supernatant to a final concentration of 15% prior to storage at −70°C for plaque assay.
Primary human MDM and DC cultures.
Conditions similar to those described elsewhere were used to culture MDMs and DCs (25, 48, 62). Peripheral blood mononuclear cells were isolated on Histopaque (Sigma) from buffy coats prepared from one pint of blood (South Texas Region Blood and Tissue Center, San Antonio, Tex.). They were washed three times with PBS without Ca or Mg (PBS−), resuspended in incomplete RPMI 1640 media (containing 2.0 mM glutamine, 100 U of penicillin/ml, and 100 μg of streptomycin/ml), plated onto petri dishes (150 by 25 mm), and allowed to attach for 90 min. Nonadherent cells were removed by washing the plates three times with PBS−; adherent cells were scraped into complete RPMI 1640 medium (incomplete medium containing 10% FCS), counted, and placed in 24-well plates at a density of 1.0 × 105 to 3.0 × 105 cells per well. MDM cultures were stimulated with granulocyte-macrophage colony-stimulating factor (GM-CSF) at a final concentration of 500 U/ml; DC cultures were stimulated with GM-CSF and interleukin-4 (IL-4; Peprotech, Rocky Hill, N.J.) at a final concentration of 500 U/ml. Every other day one-half of the medium was replaced with medium containing 1,000 U of GM-CSF/ml for MDM cultures and with medium containing 1,000 U of GM-CSF and IL-4/ml for DC cultures. Cells were maintained under these conditions for 6 to 7 days prior to infection with dengue virus.
Infection of MDM and DC cultures.
MDM and DC cells (one well each) were eluted and counted prior to infection to estimate the multiplicity of infection (MOI) in genome equivalents per cell. Typically, 1.0 × 105 to 3.0 × 105 cells were infected per virus sample for every time point. Virus was adsorbed to cells for 90 min at 37°C in incomplete media. In addition to mock-infected cultures, heat-inactivated virus (60°C for 30 min) was used as a negative control for virus infection. The inoculum was removed from the MDM cells, the wells were washed three times with PBS−, and 0.5 ml of complete medium with 500 U of GM-CSF/ml was added to each well. Since the DC cultures are loosely adherent, cells were collected in centrifuge tubes, pelleted at 800 × g for 2 min to remove the inoculum, and then washed three times with PBS−. Cells were then resuspended in complete medium containing 500 U of GM-CSF and IL-4/ml and placed in 24-well plates. For sample harvesting, supernatant was clarified by centrifugation, and extracellular RNA was extracted as described for C6/36 cell infections and stored at −70°C for quantitative RT-PCR. Adherent cells were eluted in PBS− containing 1% FCS and 10 mM EDTA, collected by centrifugation, washed once in PBS−, and processed for either intracellular or extracellular immunostaining.
Immunostaining and flow cytometry.
MDM cultures were recovered by incubating the cells in fluorescence-activated cell sorting (FACS) elution buffer (PBS−, 1% FCS, 10 mM EDTA) for 10 min on ice. Cells were gently scraped into the medium and pelleted by centrifugation at 800 × g for 3 min. DCs were loosely adherent but collected as described for MDM cultures. Cells were then washed once in FACS staining buffer (PBS− containing 1% FCS), and cells processed for detection of intracellular dengue virus antigen were fixed and permeabilized by using the CytoFix/CytoPerm kit (BD Biosciences Pharmingen, San Diego, Calif.). Two different sources of anti-dengue virus antibodies were used during the course of these experiments: anti-dengue 2 virus ascites fluid was obtained from the Centers for Disease Control (Fort Collins, Colo.), and monoclonal anti-dengue virus antibody (cross-reactive with all four serotypes) was purchased from Chemicon International (La Jolla, Calif.). Both antibodies were fluorescein isothiocyanate-conjugated by using the FluoroTag FITC Conjugation Kit according to the manufacturer's protocol (Sigma). The fluorescein/protein molar ratios were 2.2 and 7, respectively, and both antibodies were diluted 1:100 prior to use. Anti-dengue virus staining was performed on ice for 2 h, the samples were washed with CytoPerm/CytoWash buffer and resuspended in FACS/flow buffer containing 2% formaldehyde. Cells processed for cell surface markers were resuspended in FACS staining buffer with either anti-human marker antibody HLA-DR (MDMs) or CD1a (DCs). Cells were incubated with cell surface marker antibodies in a volume of 40 μl for 2 h on ice, washed with FACS staining buffer, and resuspended in 300 μl of FACS/flow buffer containing 2% formaldehyde. All samples were acquired (3,000 to 6,000 gated events) and analyzed on a FACScalibur flow cytometer (Becton Dickinson, Franklin Lakes, N.J.) within 24 h of staining. Typically, 95 to 98% of the gated MDMs stained positive for HLA-DR; ca. 80 to 95% of the gated DCs stained positive for CD1a.
Calculations and statistics.
The numbers of genome equivalents per milliliter were estimated by multiplying the RNA copy number in a 5-μl sample by 200. The virus output per infected cell was calculated by dividing the RNA copy number present in a 500-μl sample by the fraction of cells positive for dengue virus antigen by FACS analysis. Statistical analyses using InStat version 3 were performed by pooling data from three different cell donors for a total of nine samples per virus, and these values were compared by a nonparametric analysis of variance test (Kruskal-Wallis) (33). Pairwise comparisons were performed by Dunn's multiple comparison tests (12) to determine which virus outputs were significantly different from those of the parental infectious clone (D2/IC-30P-A).
RESULTS
Replacement with American genotype sequences does not abolish replication of a SE Asian-derived infectious clone.
A previous comparison of genome sequences of representative SE Asian and American genotype viruses revealed conserved amino acids and conserved secondary structure predictions for the 5′ and 3′ ntr's (37). In the present study, site-directed mutagenesis was used to change amino acid 390 (Asn→Asp) in D2/IC-30P-A, a SE Asian virus backbone. In addition, convenient restriction sites were used to replace sequences in D2/IC-30P-A at both 5′ and 3′ ends. These substitutions included the entire 5′ and 3′ ntr's that were predicted to alter RNA secondary structures and additional sequences within the adjacent coding regions. Replacement of 3′-end sequences, from the HpaI restriction site to the 3′ terminus, resulted in substitution of the entire 3′ ntr and 184 nt of the carboxy-terminal NS5 ORF for D2/IC-3ntrK, D2/IC-3ntrIQT, D2/IC-5+3ntrIQT, and D2/IC-5E3IQT (Fig. 1). Within the 594 nt that were replaced, D2/IC-3ntrK and D2/IC-30P-A had a similarity of 98.48%. D2/IC-3ntrK had nine nucleotide changes resulting in seven transitions, one transversion, and one insertion compared to nt 10130 to 10723 of D2/IC-30P-A. All of the mutations within the NS5 ORF were silent. Within the 3′-terminal 594 nt of D2/IC-30P-A that were replaced with IQT2913 sequences, there was a similarity of 92.76%. D2/IC-3ntrIQT, D2/IC-5+3ntrIQT, and D2/IC-5E3 had the same 594-nt 3′-end sequences replaced, which had 43 nucleotide differences (resulting in 28 transitions, 4 transversions, 10 nucleotide deletions, and one nucleotide insertion) compared to nt 10130 to 10723 of D2/IC-30P-A. One of the mutations within the NS5 ORF resulted in an amino acid change at position 865 (Ala→Thr). Replacing 5′-end sequences, up to the SalI restriction site, resulted in substitution of the entire 5′ ntr and 68 nt from the amino terminus of the C ORF for D2/IC-5ntrIQT, D2/IC5+3ntrIQT, and D2/IC-5E3IQT. Within the 5′-terminal 164 nt of D2/IC-30P-A that were replaced with IQT2913 sequences, there was a similarity of 97.56%. These American genotype replacements had four nucleotide differences resulting in two transitions, one transversion and one nucleotide deletion. The transversion at nt 122 resulted in a point mutation within C at amino acid 8 (Lys→Arg). After electroporation of in vitro-transcribed RNA, all of the chimeras produced virus in C6/36 cells, indicating that none of the nucleotide or amino acid changes abolished replication of the infectious clones.
American genotype sequences alter plaque morphology.
Although virus stocks were generated for all of the chimeras in mosquito cells, changes in plaque morphology were observed for some of these viruses in monkey cells (Fig. 2). Neither D2/IC-3ntrK nor D2/IC-5ntrIQT appeared to have an altered plaque morphology compared to D2/IC-30P-A. Replacement of the 3′-terminal 594 nt of the infectious clone with sequences from American genotype generated virus D2/IC-3ntrIQT, which produced less-discrete, intermediate-sized plaques. Smaller, well-defined plaques were observed for D2/IC-Em. Plaques were not visible for D2/IC-5+3ntrIQT and D2/IC-5E3IQT when high dilutions of virus were used in the assay; however, partial clearing of the monolayer was observed at lower dilutions of the virus stocks. Although inserts were sequenced for all of the chimeras, the entire genome was sequenced directly from virus stock for D2/IC-Em, D2/IC-5+3ntrIQT and D2/IC-5E3IQT by using RT-PCR as described previously (37) to confirm that no extraneous mutations were present (data not shown). Therefore, only sequences purposely replaced could account for the changes in plaque morphology described here.
FIG. 2.
Plaque morphology for infectious clones. Vero cells were infected and overlaid with 1× MEM-2% FCS containing 1% agarose. At 9 days postinfection the plaque assay was developed and the wells were photographed.
Chimeric dengue virus replication is not altered in C6/36 cells.
To demonstrate that all of the chimeric viruses replicated well in C6/36 cell cultures in comparison to the parental infectious clone, accumulation of extracellular viral RNA was determined by using a real-time, quantitative RT-PCR assay (Fig. 3A). Peak viral RNA output occurred on day 4 postinfection and ranged from 1.1 × 109 to 3.9 × 109 genome Eq/ml for all infectious clones. Virus titers for D2/IC-30P-A (parent), D2/IC-3ntrK, D2/IC-5ntrIQT, and D2/IC-Em were also determined by plaque assay because these viruses produced well-defined plaques. Plaque titers also peaked 4 days postinfection and ranged from 1.1 × 106 to 3.8 × 106 PFU/ml (Fig. 3B). Although the absolute values for the plaque assays were much lower compared to the genome equivalents, the overall profiles for the two graphs were similar, indicating that quantitative RT-PCR was a valid method to measure virus output. From these data it appears that the replacement with American genotype sequences did not alter replication of the chimeras in mosquito cells. Specifically, the point mutation in E and the amino acid changes in C and NS5 that were introduced along with the ntr's did not reduce virus output from C6/36 cells.
FIG. 3.
Growth kinetics of chimeric viruses. Mosquito cells were infected at an MOI of 1,000 genome Eq/cell, and supernatants were collected every day for 6 days. Virus output was determined by quantitative RT-PCR from two experiments, and the graph represents the mean (with the standard deviations indicated in panel A). For one of these experiments, virus output for four viruses was determined by plaque assay and is shown in panel B.
Infection of MDMs and DCs with genome equivalents as a measure of input.
MDM and DC cultures were infected at different MOIs to optimize infection rates with genome equivalents as a measure of virus input. The percentage of infected MDMs and DCs was determined by flow cytometry over a 3-day time period, after infection with MOIs of 500, 1,000, and 1,500 (Table 1). Due to the large number of cells required for duplicates at all time points, only virus pairs could be tested simultaneously. The triple mutant chimera, D2/IC-5E3IQT, was compared to the parental infectious clone, D2/IC-30P-A, and the American genotype virus strain, IQT2913, was compared to 16681, the wild-type SE Asian parent of D2/IC-30P-A. In MDM cultures at 24 h postinfection 16681 produced the highest maximal infection rate of 9.14% at an MOI of 1500, whereas the maximal rate of MDM infection for IQT2913 was 1.83% under the same conditions (Table 1). A maximal infection rate of 3.07% was measured for D2/IC-30P-A at 48 h postinfection, whereas the triple mutant peaked at 1.73% at 72 h. Although the percentage of infected MDMs varied for all viruses over 3 days, the data showed that the highest infection rates were for the SE Asian infectious clone (3.07%) and its wild-type parent (9.14%), whereas the highest infection rates for the triple mutant (1.73%) and its wild-type, American genotype parent (1.83%) were much lower.
TABLE 1.
Percentages of dengue virus-infected MDMs and DCs
| Virus | Expt | MOI (genome Eq/cell) | % Dengue virus-infected MDMs and DCs ± SDa
|
|||||
|---|---|---|---|---|---|---|---|---|
| MDMs
|
DCs
|
|||||||
| 24 hpi | 48 hpi | 72 hpi | 24 hpi | 48 hpi | 72 hpi | |||
| D2/IC-30P-A | 1 | 500 | 1.29 ± 0.21 | 1.19 ± 0.05 | 0.19 ± 0.06 | 33.27 ± 2.39 | 35.13 ± 2.56 | 27.02 ± 2.00 |
| 1,000 | 2.05 ± 0.46 | 2.51 ± 0.29 | 0.46 ± 0.45 | 49.09 ± 3.25 | 46.01 ± 0.98 | 42.97 ± 0.98 | ||
| 1,500 | 2.35 ± 1.61 | 3.07 ± 1.97 | 0.34 ± 0.36 | 55.52 ± 1.98 | 48.93 ± 4.08 | 42.89 ± 4.70 | ||
| D2/IC-5E3IQT | 1 | 500 | 0.67 ± 0.64 | 1.13 ± 0.04 | 0.73 ± 0.18 | 15.20 ± 1.97 | 22.07 ± 0.35 | 14.19 ± 1.70 |
| 1,000 | 0.58 ± 0.52 | 0.48 ± 0.22 | 1.12 ± 0.11 | 27.23 ± 0.78 | 28.69 ± 1.57 | 20.71 ± 2.64 | ||
| 1,500 | 0.61 ± 0.27 | 1.11 ± 0.90 | 1.73 ± 0.26 | 20.71 ± 2.64 | 28.74 ± 1.36 | 32.12 ± 2.36 | ||
| 16681 | 2 | 500 | 3.62 ± 0.19 | 4.83 ± 2.03 | 0.86 ± 0.04 | 36.28 ± 3.14 | 36.41 ± 0.03 | 24.47 ± 2.55 |
| 1,000 | 6.56 ± 0.56 | 5.19 ± 1.36 | 2.21 ± 0.82 | 56.08 ± 1.90 | 55.80 ± 1.63 | 41.47 ± 3.27 | ||
| 1,500 | 9.14 ± 1.01 | 6.55 ± 1.17 | 2.14 ± 0.99 | 61.61 ± 3.13 | 63.16 ± 1.53 | 58.60 ± 0.42 | ||
| IQT2913 | 2 | 500 | 0.06 ± 0.04 | 0.24 ± 0.16 | 0.07 ± 0.01 | 3.08 ± 0.52 | 7.38 ± 0.74 | 4.22 ± 0.01 |
| 1,000 | 0.56 ± 0.36 | 1.03 ± 0.25 | 0.24 ± 0.01 | 7.36 ± 1.30 | 12.82 ± 8.32 | 11.81 ± 0.96 | ||
| 1,500 | 1.83 ± 0.95 | 1.36 ± 0.28 | 0.35 ± 0.01 | 13.00 ± 1.30 | 23.86 ± 0.23 | 15.06 ± 0.62 | ||
hpi, hours postinfection.
As was seen in the MDMs, the maximal mean percentage of infected DCs was higher for D2/IC-30P-A (55.52%) and 16681 (63.16%) than for D2/IC-5E3IQT (32.12%) and IQT2913 (23.86%) (Table 1). These maximal infection rates were observed at 48 h postinfection for 16681 and IQT2913, at 24 h postinfection for D2/IC-30P-A, and at 72 h postinfection for D2/IC-5E3IQT. Virtually no cells in either the MDM or DC cultures were positive for dengue virus antigen with heat-inactivated D2/IC-30P-A or 16681, indicating that replication was required for detection by flow cytometry.
In addition to determining the number of infected cells, virus outputs from MDM and DC culture supernatants were estimated by using quantitative RT-PCR. In MDM cultures the highest mean peak titers were measured for D2/IC-30P-A (1.74 × 108 genome Eq/ml) and 16681 (1.17 × 108 genome Eq/ml); titers for D2/IC-5E3IQT (5.73 × 106 genome Eq/ml) and IQT2913 (5.37 × 106 genome Eq/ml) were lower. Similar results were obtained from DC cultures with D2/IC-30P-A (4.32 × 109 genome Eq/ml) and 16681 (1.26 × 109 genome Eq/ml), which replicated to higher mean peak titers than D2/IC-5E3IQT (8.97 × 107 genome Eq/ml) and IQT2913 (2.17 × 108 genome Eq/ml). Titers from DC cultures were at least 10-fold higher than titers from MDM cultures, and this was due to higher infection rates of DC cultures compared to MDM cultures. D2/IC-30P-A and 16681 replicated 5- to 40-fold higher than D2/IC-5E3IQT and IQT2913 in both cultures. These results were expected, since D2/IC-30P-A and 16681 infected more MDMs and DCs than either the triple mutant or IQT2913 (Table 1). Therefore, virus output was estimated as a function of the percentage of infected cells. Genome equivalents secreted (virus output) per infected cell were estimated for each sample, and these results were compared among viruses. This approach thus compensated for the variation in infection rates within and across experiments, which is thought to be due mainly to donor differences. The results indicated that, for any given MOI, the virus output per infected cell was very similar for MDM or DC cultures for each virus (Fig. 4, compare panel A to panel B and panel C to panel D). Virus output per infected cell did not appear to be influenced by MOI since most of the mean datum points overlap for each virus (Fig. 4, all panels). Peak virus output occurred at 48 h postinfection for most MDM and DC cell cultures, and the highest mean peak titers were reached by viruses with only SE Asian structures. The mean peak titers for D2/IC-30P-A and 16681 ranged from 19,870 to 26,141 and 39,082 to 54,587 genome Eq secreted per infected cell, respectively, whereas those for D2/IC-5E3IQT and IQT2913 ranged from 2,620 to 2,937 or from 7,257 to 10,491 genome Eq secreted per infected cell, respectively (Fig. 4B and D). The same trend was observed in MDM cultures, although more variability occurred as indicated by larger standard deviations for most of the time points examined (Fig. 4A and C). Overall, these results indicated that virus replication could be evaluated for all viruses, independent of cell susceptibility, by normalizing the virus output by the number of infected cells.
FIG. 4.
Virus output for MDM and DC cultures. MDM (A and C) and DC (B and D) cultures were infected at MOIs of 500 (circles), 1,000 (squares), or 1,500 (triangles) genome Eq/cell. The graphs in panels A and B represent the mean virus output per infected cell, with the standard deviations indicated, for duplicate wells infected with D2/IC 30P-A (solid symbols, solid lines) or D2/IC-5E3IQT (open symbols, dashed lines). The graphs in panels C and D represent the mean virus output per infected cell, with the standard deviations indicated, for duplicate wells infected with 16681 (solid symbols, solid lines) or IQT2913 (open symbols, dashed lines).
Significant reduction in virus output requires all three American genotype structures.
To determine which of the American structures were responsible for the decrease in virus output per infected cell, DC cultures were infected since there was less variability in this culture system compared to the MDM cultures. All of the infections were done by using an MOI of 1,000 genome copies per cell as the standard, although differences in the MOI did not appreciably change the virus output per infected cell. In addition to examining the influence of American structures derived from IQT2913, we examined replacement of the 3′ ntr with another SE Asian-derived structure by substituting it with that of strain K0008. This control was included to determine whether D2/IC-30P-A required a specific 3′-ntr sequence or whether substitution with a similar structure altered virus output.
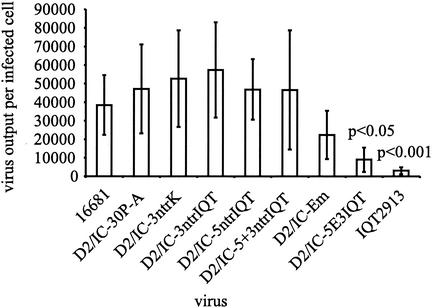
Three separate experiments were performed to examine replication of all chimeras with a total of nine samples per virus by using buffy coats from three donors. The results were presented as the mean virus output for all samples, with standard deviations included (Fig. 5). In all experiments, D2/IC-Em, D2/IC-5E3IQT, and IQT2913 had lower virus outputs than D2/IC-30P-A. D2/IC-5+3ntrIQT was the only chimera that had various outputs, leading to a very large standard deviation. The virus output per infected cell was statistically significant among individual virus samples as determined by the Kruskal-Wallis test (P < 0.0001). Pairwise comparisons revealed that the virus output of D2/IC-30P-A was significantly greater than that of D2/IC-5E3IQT (P < 0.05) and IQT2913 (P < 0.001). Although D2/IC-Em had decreased virus output (twofold reduction), this reduction was not statistically significant. From these results it appears that the E mutation was dominant in decreasing viral output, since the ntr changes alone or in combination did not significantly alter virus output. Only the triple mutant (fivefold reduction) had a significantly reduced virus output that approached that measured for a wild-type, American genotype virus (IQT2913).
FIG. 5.
Comparison of virus output in DC cultures. Data are from infected DC cultures at 48 h postinfection from three different donors with a total of nine samples for each virus. The bars represent the mean virus output per infected cell, and the error bars represent the standard deviation of the means. Statistical significance was determined by using the Kruskal-Wallis test, and pairwise comparisons with D2/IC-30P-A were used to calculate the P values for D2/IC-5E3IQT and IQT2913.
DISCUSSION
To identify viral determinants of dengue virus pathogenesis, this report describes the effects of naturally occurring dengue virus mutations on replication. The dengue virus type 2 structures probably involved in human virulence were defined previously by sequencing the complete genome of both American and SE Asian genotype templates in patient serum (37). This genetic information was used to determine how American genotype virus structures influence replication in mosquito and human target cells. In the present study, we examined the effect of three American genotype structures on virus replication in vitro and demonstrated that American structures reduced virus output from human MDM and DC cultures. This change in replicative ability was specific for relevant human target cells since no alteration in replication was observed in mosquito cell cultures.
We hypothesized that changes in 5′- and 3′-end secondary structures and an amino acid charge change that are consistent in the American genotype viruses would decrease the replication efficiency of an SE Asian-derived infectious clone. Of the American structures examined, the E mutation (amino acid 390 Asn→Asp) was the only structure that by itself reduced virus output, albeit not significantly. Previous studies with MDM cultures suggested that the Asn at amino acid 390, in an infectious clone derived from strain New Guinea C (SE Asian genotype), is optimal for efficient replication (48). Substitutions with a nonpolar (Ala), charged (Asp), or even a similar uncharged polar (Ser) side chain amino acid reduced virus output; however, the data were not normalized for any change in infectivity that might have occurred due to mutagenesis. Infectivity should be monitored since it has been shown that viral glycoproteins can affect tropism; for example, a single amino acid mutation at residue 160 of the Sindbis virus envelope glycoprotein E2 increases the efficiency of DC infection (13). In the work shown here, the decreased dengue virus output measured was not due to alterations in the infectivity since virus output was determined as a function of the number of infected cells. It is possible that mutation of E 390 affects the efficiency of glycoprotein maturation and virion assembly, thereby reducing virus output. Although the E 390 Asn is not located in a glycosylation domain, other co- and posttranslational events may affect the efficiency of protein maturation (for a review, see reference 11).
Results from the present study also indicated that changing E 390 to Asp was not sufficient to reduce virus output to the lower level measured for the wild-type American genotype dengue virus. Other changes were necessary to significantly reduce the dengue virus output from DC cultures. Sequences in ntr's have been shown to influence dengue virus replication. A single nucleotide substitution in the 5′ ntr of an SE Asian-derived virus, at nt 57, has been shown to decrease replication efficiency in mosquito cells and pathogenesis in mice (6). Deletions in the 5′ ntr have been shown to affect serotype 4 dengue virus replication in cultured cells (7). Construction of dengue viruses with alterations in the 3′ ntr resulted in viruses with restricted growth in vitro (44, 65). Efficient replication also requires interactions between the 5′ and 3′ termini (8, 44, 63-65). Although nucleotide changes present in American genotype termini are not expected to disrupt long-range interactions, they were predicted to change RNA secondary structures at both ends compared to SE Asian ntr's (37). Replacement of SE Asian with American terminal structures, either alone or in combination, did not reduce virus output but required the E mutation to significantly alter replication. One possible explanation for the requirement of the E mutation is that terminal structures decrease the replication or translation efficiency slightly, and this phenotype is more pronounced in the presence of the E mutation. In primary human foreskin fibroblasts, the replication of low-passage dengue type 2 viruses from Thailand generated less negative-strand RNA, suggesting a slightly reduced replication efficiency in comparison to 16681, whereas replication of Nicaraguan strains was blocked at a step prior to negative-strand synthesis (10). It is possible that sequence differences within the ends of the Nicaraguan strains affect translation efficiency compared to other SE Asian genotype viruses. Results from our study demonstrate that substitution of SE Asian with multiple American genotype structures was necessary to reduce the replication efficiency to a level approaching that of a wild-type American genotype virus in human DCs. The mechanism by which viral replication is altered and the contribution of other conserved genotype structures on replication efficiency merits further study.
The correlation between SE Asian genotype structures and increased replicative ability in vitro underscores the correlation between viremia and pathogenesis. Prospective studies have shown that progression to DHF is associated with higher mean plasma viremias (39, 40, 58). Progression to DHF has also been associated with increased levels of circulating NS1 (40), also implying an increase in dengue virus replication. Three models can be proposed to explain the higher mean viremias observed for patients who develop DHF: (i) more cells are infected in DHF patients, thus generating more virus; (ii) more virus is produced per infected cell; or (iii) the virus is cleared at a slower rate compared to patients who develop DF, resulting in an increase in blood-borne virus. Little is known about the number of infected monocytes or DCs during human infection. In vitro experiments have shown that subneutralizing concentrations of antibody increased the number of dengue virus-infected monocytes in vitro, and this is referred to as ADE (4, 10, 19, 20, 22, 31, 32, 41, 42). Data from dengue virus infection of primates indicated that increased viremias were associated with preexisting heterologous anti-dengue virus antibodies (17, 21), which may suggest that the increased viremia was due to an increase in the number of infected cells. ADE has been proposed as a mechanism for the increased risk of developing DHF associated with secondary dengue virus infection and may explain, in part, the increased viremias associated with DHF (5, 16, 53, 56, 58). However, for dengue type 2 American genotype viruses, secondary infection is not associated with an increased risk of developing DHF (59). Additionally, the likely initial targets for dengue virus replication are immature DCs in the skin (Langerhans cells) and infection efficiency is not influenced by the presence of anti-dengue virus antibodies, indicating that DCs are not susceptible to ADE (62). We were unable to correlate the number of infected MDMs or DCs with genotype, although data from Table 1 appear to suggest the opposite. In subsequent experiments, the number of infected cells varied considerably and sometimes the wild-type American genotype virus infected the highest percentage of cells. This may be due to infection rate variability observed between blood donors. Others have also reported that dengue virus infection rates vary among donors or cell lines and can be dependent on the differentiation state of cells (19, 35, 38, 47). A recent report compared the replication of four to eight SE Asian genotype isolates in different cell cultures and demonstrated that the number of infected cells varied between isolates in a human hepatoma cell line and primary human foreskin fibroblast cells (10). Although we do not rule out the possibility of ADE playing a role in dengue virus pathogenesis, dengue virus infectivity appears to be quite variable and may hinder direct comparisons of the number of infected cells either in vivo or in vitro to the pathogenic potential of different dengue viruses.
With respect to the second proposed model that higher mean viremias observed for patients who develop DHF is the result of increased virus production per infected cell, our results may offer part of the explanation why SE Asian genotype viruses are associated with DHF and the indigenous American genotype viruses are not associated with DHF in the Western hemisphere. Since American genotype structures decreased virus output per infected cell, humans infected with the American strains may have lower mean viremias than patients infected with SE Asian genotype strains and thus do not develop DHF. The third proposed model that higher mean viremias are associated with slower virus clearance has already been addressed, and clinical data indicate that DHF was associated with faster virus clearance (58). Although this may seem counterintuitive, this result is likely due to the association of DHF with secondary infections in Thailand and further supports the idea that the immune system is a factor in dengue virus pathogenesis.
In addition to viremia, elevated levels of other host factors have been shown to correlate with the development of DHF, including increased levels of liver enzymes, soluble adhesion molecules, and cytokines in plasma (28, 39, 46, 50). A number of reports have examined the production of immunomodulatory molecules after in vitro dengue virus infection of monocytes and endothelial cells (1, 3, 9, 34, 36). Induction of these molecules initiates a number of cascades that potentially influence both proinflammatory and anti-inflammatory immune responses. In addition to monocytes, dengue virus infection of monocyte-derived DCs has been shown to induce maturation and activation, as well as the release of a number of cytokines (25, 38). Another virus that causes hemorrhagic fever, Hantaan, has also been shown to infect and activate DCs in vitro, resulting in the release of tumor necrosis factor alpha and alpha interferon (49). Whether or not similar mechanisms are involved in the pathogenesis of DHF and Hantaan virus hemorrhagic fever with renal syndrome, the ability to infect target cells and modulate the immune system seems to be critical in the pathogenesis of both viruses. Our results suggest that, in comparison to American genotype viruses, some SE Asian genotype viruses replicate more efficiently. In turn, this could lead to the production of more virus and to increased infection of secondary sites resulting in increased levels of cytokines in plasma and more-severe disease symptoms. Clinical and immunologic data are needed from the Americas to determine whether there are distinguishing characteristics between the two genotypes that could be correlated with pathogenesis.
Replication in target cells is essential for dengue pathogenesis in the human host and is important for efficient transmission by the vector mosquito, Aedes aegypti. From an ecologic or epidemiologic perspective, the SE Asian genotype virus appears to be displacing American genotype virus in this hemisphere (52). This displacement could be the result of more efficient mosquito transmission by the SE Asian genotype viruses. Factors that influence mosquito transmission include the infection rate, the replicative ability, and the ability to disseminate to the salivary glands. Both host and viral determinants of dengue replication may affect viremia and thus contribute to the transmission potential of the virus to the mosquito. Some attenuated vaccine candidates have been shown to exhibit limited dissemination potential in mosquitoes (27, 29, 54, 57). Specifically, a 30-nt deletion in the 3′ ntr was shown to disrupt the ability of dengue virus to disseminate to the salivary gland after ingestion of a virus-spiked blood meal (57). It has also been shown that a lower percentage of mosquitoes had a disseminated infection after ingestion of a blood meal spiked with American genotype viruses compared with those belonging to the SE Asian genotype (2; P. M. Armstrong and R. Rico-Hesse, unpublished data). The ability to determine which American genotype structures influence infection and dissemination in the vector mosquito, thus providing an explanation for the displacement of the American genotype in this hemisphere, may be obtained by further utilizing the chimeric dengue viruses described here.
The mechanisms involved in severe dengue disease are complex and likely include viral and host determinants; these mechanisms may ultimately affect disease transmission and epidemiology. We have focused on identifying viral determinants associated with efficient replication in an attempt to correlate genotypic differences with the pathogenic potential of different viruses in this hemisphere. Our results indicate that American genotype structures decreased the replicative ability of an SE Asian-derived infectious clone and may provide part of the explanation of why the American genotype dengue viruses are not associated with the occurrence of DHF.
Acknowledgments
This research was supported by NIH grant AI59123 and the R. C. and A. G. Cowles Memorial Trust.
We thank Richard Kinney for use of the D2/IC-30P-A infectious clone, Philip Armstrong for help with statistical analyses, and Luis Giavedoni and April Hopstetter for review of the manuscript.
REFERENCES
- 1.Anderson, R., S. Wang, C. Osiowy, and A. C. Issekutz. 1997. Activation of endothelial cells via antibody-enhanced dengue virus infection of peripheral blood monocytes. J. Virol. 71:4226-4232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Armstrong, P. M., and R. Rico-Hesse. 2001. Differential susceptibility of Aedes aegypti to infection by the American and Southeast Asian genotypes of dengue type 2 virus. Vector-Borne Zoon. Dis. 1:159-168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bosch, I., K. Xhaja, L. Estevez, G. Raines, H. Melichar, R. V. Warke, M. V. Fournier, F. A. Ennis, and A. L. Rothman. 2002. Increased production of interleukin-8 in primary human monocytes and in human epithelial and endothelial cell lines after dengue virus challenge. J. Virol. 76:5588-5597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Brandt, W. E., J. M. McCown, M. K. Gentry, and P. K. Russell. 1982. Infection enhancement of dengue type 2 virus in the U-937 human monocyte cell line by antibodies to flavivirus cross-reactive determinants. Infect. Immun. 36:1036-1041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Burke, D. S., A. Nisalak, D. E. Johnson, and R. M. Scott. 1988. A prospective study of dengue infections in Bangkok. Am. J. Trop. Med. Hyg. 38:172-180. [DOI] [PubMed] [Google Scholar]
- 6.Butrapet, S., C. Y. Huang, D. J. Pierro, N. Bhamarapravati, D. J. Gubler, and R. M. Kinney. 2000. Attenuation markers of a candidate dengue type 2 vaccine virus, strain 16681 (PDK-53), are defined by mutations in the 5′ noncoding region and nonstructural proteins 1 and 3. J. Virol. 74:3011-3019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cahour, A., A. Pletnev, M. Vazielle-Falcoz, L. Rosen, and C. J. Lai. 1995. Growth-restricted dengue virus mutants containing deletions in the 5′ noncoding region of the RNA genome. Virology 207:68-76. [DOI] [PubMed] [Google Scholar]
- 8.Chambers, T. J., C. S. Hahn, R. Galler, and C. M. Rice. 1990. Flavivirus genome organization, expression, and replication. Annu. Rev. Microbiol. 44:649-688. [DOI] [PubMed] [Google Scholar]
- 9.Chen, Y. C., and S. Y. Wang. 2002. Activation of terminally differentiated human monocytes/macrophages by dengue virus: productive infection, hierarchical production of innate cytokines and chemokines, and the synergistic effect of lipopolysaccharide. J. Virol. 76:9877-9887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Diamond, M. S., D. Edgil, T. G. Roberts, B. Lu, and E. Harris. 2000. Infection of human cells by dengue virus is modulated by different cell types and viral strains. J. Virol. 74:7814-7823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Doms, R. W., R. A. Lamb, J. K. Rose, and A. Helenius. 1993. Folding and assembly of viral membrane proteins. Virology 193:545-562. [DOI] [PubMed] [Google Scholar]
- 12.Dunn, O. J. 1964. Multiple contrasts using rank sums. Technometrics 6:241-252. [Google Scholar]
- 13.Gardner, J. P., I. Frolov, S. Perri, Y. Ji, M. L. MacKichan, J. zur Megede, M. Chen, B. A. Belli, D. A. Driver, S. Sherrill, C. E. Greer, G. R. Otten, S. W. Barnett, M. A. Liu, T. W. Dubensky, and J. M. Polo. 2000. Infection of human dendritic cells by a Sindbis virus replicon vector is determined by a single amino acid substitution in the E2 glycoprotein. J. Virol. 74:11849-11857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gubler, D. J. 1998. Dengue and dengue hemorrhagic fever. Clin. Microbiol. Rev. 11:480-496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Halstead, S. B. 1970. Observations related to pathogensis of dengue hemorrhagic fever. VI. Hypotheses and discussion. Yale J. Biol. Med. 42:350-362. [PMC free article] [PubMed] [Google Scholar]
- 16.Halstead, S. B., S. Nimmannitya, and S. N. Cohen. 1970. Observations related to pathogenesis of dengue hemorrhagic fever. IV. Relation of disease severity to antibody response and virus recovered. Yale J. Biol. Med. 42:311-328. [PMC free article] [PubMed] [Google Scholar]
- 17.Halstead, S. B., H. Shotwell, and J. Casals. 1973. Studies on the pathogenesis of dengue infection in monkeys. II. Clinical laboratory responses to heterologous infection. J. Infect. Dis. 128:15-22. [DOI] [PubMed] [Google Scholar]
- 18.Halstead, S. B., N. J. Marchette, J. S. Sung Chow, and S. Lolekha. 1976. Dengue virus replication enhancement in peripheral blood leukocytes from immune human beings. Proc. Soc. Exp. Biol. Med. 151:136-139. [DOI] [PubMed] [Google Scholar]
- 19.Halstead, S. B., and E. J. O'Rourke. 1977. Dengue viruses and mononuclear phagocytes. I. Infection enhancement by non-neutralizing antibody. J. Exp. Med. 146:201-217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Halstead, S. B., and E. J. O'Rourke. 1977. Antibody-enhanced dengue virus infection in primate leukocytes. Nature 265:739-741. [DOI] [PubMed] [Google Scholar]
- 21.Halstead, S. B. 1979. In vivo enhancement of dengue virus infection in rhesus monkeys by passively transferred antibody. J. Infect. Dis. 140:527-533. [DOI] [PubMed] [Google Scholar]
- 22.Halstead, S. B., C. N. Venkateshan, M. K. Gentry, and L. K. Larsen. 1984. Heterogeneity of infection enhancement of dengue 2 strains by monoclonal antibodies. J. Immunol. 132:1529-1532. [PubMed] [Google Scholar]
- 23.Halstead, S. B., T. G. Streit, J. G. Lafontant, R. Putvatana, K. Russell, W. Sun, N. Kanesa-Thasan, C. G. Hayes, and D. M. Watts. 2001. Haiti: absence of dengue hemorrhagic fever despite hyperendemic dengue virus transmission. Am. J. Trop. Med. Hyg. 65:180-183. [DOI] [PubMed] [Google Scholar]
- 24.Harris, E., E. Videa, L. Perez, E. Sandoval, Y. Tellez, M. L. Perez, R. Cuadra, J. Rocha, W. Idiaquez, R. E. Alonso, M. A. Delgado, L. A. Campo, F. Acevedo, A. Gonzalez, J. J. Amador, and A. Balmaseda. 2000. Clinical, epidemiologic, and virologic features of dengue in the 1998 epidemic in Nicaragua. Am. J. Trop. Med. Hyg. 63:5-11. [DOI] [PubMed] [Google Scholar]
- 25.Ho, L. J., J. J. Wang, M. F. Shaio, C. L. Kao, D. M. Chang, S. W. Han, and J. H. Lai. 2001. Infection of human dendritic cells by dengue virus causes cell maturation and cytokine production. J. Immunol. 166:1499-1506. [DOI] [PubMed] [Google Scholar]
- 26.Hober, D., L. Poli, B. Roblin, P. Gestas, E. Chungue, G. Granic, P. Imbert, J. L. Pecarere, R. Vergez-Pascal, P. Wattre, et al. 1993. Serum levels of tumor necrosis factor-alpha (TNF-α), interleukin-6 (IL-6), and interleukin-1β (IL-1β) in dengue-infected patients. Am. J. Trop. Med. Hyg. 48:324-331. [DOI] [PubMed] [Google Scholar]
- 27.Jirakanjanakit, N., M. M. Khin, S. Yoksan, and N. Bhamarapravati. 1999. Dynamics of susceptibility and transmissibility of the live, attenuated, candidate vaccines dengue-1 PDK13, dengue-3 PGMK30F3, and dengue-4 PDK48 after oral infection in Aedes aegypti. Am. J. Trop. Med. Hyg. 61:672-676. [DOI] [PubMed] [Google Scholar]
- 28.Kalayanarooj, S., D. W. Vaughn, S. Nimmannitya, S. Green, S. Suntayakorn, N. Kunentrasai, W. Viramitrachai, S. Ratanachu-eke, S. Kiatpolpoj, B. L. Innis, A. L. Rothman, A. Nisalak, and F. A. Ennis. 1997. Early clinical and laboratory indicators of acute dengue illness. J. Infect. Dis. 176:313-321. [DOI] [PubMed] [Google Scholar]
- 29.Khin, M. M., N. Jirakanjanakit, S. Yoksan, and N. Bhamarapravati. 1994. Infection, dissemination, transmission, and biological attributes of dengue-2 PDK53 candidate vaccine virus after oral infection in Aedes aegypti. Am. J. Trop. Med. Hyg. 51:864-869. [DOI] [PubMed] [Google Scholar]
- 30.Kinney, R. M., S. Butrapet, G. J. Chang, K. R. Tsuchiya, J. T. Roehrig, N. Bhamarapravati, and D. J. Gubler. 1997. Construction of infectious cDNA clones for dengue 2 virus: strain 16681 and its attenuated vaccine derivative, strain PDK-53. Virology 230:300-308. [DOI] [PubMed] [Google Scholar]
- 31.Kliks, S. C., A. Nisalak, W. E. Brandt, L. Wahl, and D. S. Burke. 1989. Antibody-dependent enhancement of dengue virus growth in human monocytes as a risk factor for dengue hemorrhagic fever. Am. J. Trop. Med. Hyg. 40:444-451. [DOI] [PubMed] [Google Scholar]
- 32.Kontny, U., I. Kurane, and F. A. Ennis. 1988. Gamma interferon augments Fc gamma receptor-mediated dengue virus infection of human monocytic cells. J. Virol. 62:3928-3933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kruskal, W. H., and W. A. Wallis. 1952. Use of ranks in one-criterion analysis of variance. J. Am. Statist. Assoc. 47:583-621. [Google Scholar]
- 34.Kurane, I., and F. A. Ennis. 1987. Induction of interferon alpha from human lymphocytes by autologous, dengue virus-infected monocytes. J. Exp. Med. 166:999-1010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kurane, I., U. Kontny, J. Janus, and F. A. Ennis. 1990. Dengue-2 virus infection of human mononuclear cell lines and establishment of persistent infections. Arch. Virol. 110:91-101. [DOI] [PubMed] [Google Scholar]
- 36.Lee, D. H., S. S. Tam, S. Benyoucef, D. De Groote, V. Deubel, and P. Wattre. 1996. Enhanced TNF alpha production by monocytic-like cells exposed to dengue virus antigens. Immunol. Lett. 53:115-120. [DOI] [PubMed] [Google Scholar]
- 37.Leitmeyer, K. C., D. W. Vaughn, D. M. Watts, R. Salas, I. C. de Villalobos, C. Ramos, and R. Rico-Hesse. 1999. Dengue virus structural differences that correlate with pathogenesis. J. Virol. 73:4738-4747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Libraty, D. H., S. Pichyangkul, C. Ajariyakhajorn, T. P. Endy, and F. A. Ennis. 2001. Human dendritic cells are activated by dengue virus infection: enhancement by gamma interferon and implications for disease pathogenesis. J. Virol. 75:3501-3508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Libraty, D. H., T. P. Endy, H. S. Houng, S. Green, S. Kalayanarooj, S. Suntayakorn, W. Chansiriwongs, D. W. Vaughn, A. Nisalak, F. A. Ennis, and A. L. Rothman. 2002. Differing influences of virus burden and immune activation on disease severity in secondary dengue-3 virus infections. J. Infect. Dis. 185:1213-1221. [DOI] [PubMed] [Google Scholar]
- 40.Libraty, D. H., P. R. Young, D. Pickering, T. P. Endy, S. Kalayanarooj, S. Green, D. W. Vaughn, A. Nisalak, F. A. Ennis, and A. L. Rothman. 2002. High circulating levels of the dengue virus nonstructural protein NS1 early in dengue illness correlate with the development of dengue hemorrhagic fever. J. Infect. Dis. 186:1165-1168. [DOI] [PubMed] [Google Scholar]
- 41.Littaua, R., I. Kurane, and F. A. Ennis. 1990. Human IgG Fc receptor II mediates antibody-dependent enhancement of dengue virus infection. J. Immunol. 144:3183-3186. [PubMed] [Google Scholar]
- 42.Mady, B. J., D. V. Erbe, I. Kurane, M. W. Fanger, and F. A. Ennis. 1991. Antibody-dependent enhancement of dengue virus infection mediated by bispecific antibodies against cell surface molecules other than Fc gamma receptors. J. Immunol. 147:3139-3144. [PubMed] [Google Scholar]
- 43.Mangada, M. N., and A. Igarashi. 1998. Molecular and in vitro analysis of eight dengue type 2 viruses isolated from patients exhibiting different disease severities. Virology 244:458-466. [DOI] [PubMed] [Google Scholar]
- 44.Men, R., M. Bray, D. Clark, R. M. Chanock, and C. J. Lai. 1996. Dengue type 4 virus mutants containing deletions in the 3′ noncoding region of the RNA genome: analysis of growth restriction in cell culture and altered viremia pattern and immunogenicity in rhesus monkeys. J. Virol. 70:3930-3937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Murgue, B., C. Roche, E. Chungue, and X. Deparis. 2000. Prospective study of the duration and magnitude of viraemia in children hospitalized during the 1996-1997 dengue-2 outbreak in French Polynesia. J. Med. Virol. 60:432-438. [DOI] [PubMed] [Google Scholar]
- 46.Murgue, B., O. Cassar, and X. Deparis. 2001. Plasma concentrations of sVCAM-1 and severity of dengue infections. J. Med. Virol. 65:97-104. [PubMed] [Google Scholar]
- 47.O'Sullivan, M. A., and H. M. Killen. 1994. The differentiation state of monocytic cells affects their susceptibility to infection and the effects of infection by dengue virus. J. Gen. Virol. 75:2387-2392. [DOI] [PubMed] [Google Scholar]
- 48.Pryor, M. J., J. M. Carr, H. Hocking, A. D. Davidson, P. Li, and P. J. Wright. 2001. Replication of dengue virus type 2 in human monocyte-derived macrophages: comparisons of isolates and recombinant viruses with substitutions at amino acid 390 in the envelope glycoprotein. Am. J. Trop. Med. Hyg. 65:427-434. [DOI] [PubMed] [Google Scholar]
- 49.Raftery, M. J., A. A. Kraus, R. Ulrich, D. H. Kruger, and G. Schonrich. 2002. Hantavirus infection of dendritic cells. J. Virol. 76:10724-10733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Raghupathy, R., U. C. Chaturvedi, H. Al-Sayer, E. A. Elbishbishi, R. Agarwal, R. Nagar, S. Kapoor, A. Misra, A. Mathur, H. Nusrat, F. Azizieh, M. A. Khan, and A. S. Mustafa. 1998. Elevated levels of IL-8 in dengue hemorrhagic fever. J. Med. Virol. 56:280-285. [DOI] [PubMed] [Google Scholar]
- 51.Rico-Hesse, R. 1990. Molecular evolution and distribution of dengue viruses type 1 and 2 in nature. Virology 174:479-493. [DOI] [PubMed] [Google Scholar]
- 52.Rico-Hesse, R., L. M. Harrison, R. A. Salas, D. Tovar, A. Nisalak, C. Ramos, J. Boshell, M. T. de Mesa, R. M. Nogueira, and A. T. da Rosa. 1997. Origins of dengue type 2 viruses associated with increased pathogenicity in the Americas. Virology 230:244-251. [DOI] [PubMed] [Google Scholar]
- 53.Sangkawibha, N., S. Rojanasuphot, S. Ahandrik, S. Viriyapongse, S. Jatanasen, V. Salitul, B. Phanthumachinda, and S. B. Halstead. 1984. Risk factors in dengue shock syndrome: a prospective epidemiologic study in Rayong, Thailand. I. The 1980 outbreak. Am. J. Epidemiol. 120:653-669. [DOI] [PubMed] [Google Scholar]
- 54.Sardelis, M. R., R. Edelman, T. A. Klein, B. L. Innis, J. R. Putnak, J. W. Jones, and M. J. Turell. 2000. Limited potential for transmission of live dengue virus vaccine candidates by Aedes aegypti and Aedes albopictus. Am. J. Trop. Med. Hyg. 62:698-701. [DOI] [PubMed] [Google Scholar]
- 55.Tesh, R. B. 1979. A method for the isolation and identification of dengue viruses, using mosquito cell cultures. Am. J. Trop. Med. Hyg. 28:1053-1059. [DOI] [PubMed] [Google Scholar]
- 56.Thein, S., M. M. Aung, T. N. Shwe, M. Aye, A. Zaw, K. Aye, K. M. Aye, and J. Aaskov. 1997. Risk factors in dengue shock syndrome. Am. J. Trop. Med. Hyg. 56:566-572. [DOI] [PubMed] [Google Scholar]
- 57.Troyer, J. M., K. A. Hanley, S. S. Whitehead, D. Strickman, R. A. Karron, A. P. Durbin, and B. R. Murphy. 2001. A live attenuated recombinant dengue-4 virus vaccine candidate with restricted capacity for dissemination in mosquitoes and lack of transmission from vaccinees to mosquitoes. Am. J. Trop. Med. Hyg. 65:414-419. [DOI] [PubMed] [Google Scholar]
- 58.Vaughn, D. W., S. Green, S. Kalayanarooj, B. L. Innis, S. Nimmannitya, S. Suntayakorn, T. P. Endy, B. Raengsakulrach, A. L. Rothman, F. A. Ennis, and A. Nisalak. 2000. Dengue viremia titer, antibody response pattern, and virus serotype correlate with disease severity. J. Infect. Dis. 181:2-9. [DOI] [PubMed] [Google Scholar]
- 59.Watts, D. M., K. R. Porter, P. Putvatana, B. Vasquez, C. Calampa, C. G. Hayes, and S. B. Halstead. 1999. Failure of secondary infection with American genotype dengue 2 to cause dengue haemorrhagic fever. Lancet 354:1431-1434. [DOI] [PubMed] [Google Scholar]
- 60.Wills, B. A., E. E. Oragui, A. C. Stephens, O. A. Daramola, N. M. Dung, H. T. Loan, N. V. Chau, M. Chambers, K. Stepniewska, J. J. Farrar, and M. Levin. 2002. Coagulation abnormalities in dengue hemorrhagic fever: serial investigations in 167 Vietnamese children with dengue shock syndrome. Clin. Infect. Dis. 35:277-285. [DOI] [PubMed] [Google Scholar]
- 61.World Health Organization. 2002. Dengue and dengue hemorrhagic fever. Fact sheet no. 117. World Health Organization, Geneva, Switzerland.
- 62.Wu, S. J., G. Grouard-Vogel, W. Sun, J. R. Mascola, E. Brachtel, R. Putvatana, M. K. Louder, L. Filgueira, M. A. Marovich, H. K. Wong, A. Blauvelt, G. S. Murphy, M. L. Robb, B. L. Innes, D. L. Birx, C. G. Hayes, and S. S. Frankel. 2000. Human skin Langerhans cells are targets of dengue virus infection. Nat. Med. 6:816-820. [DOI] [PubMed] [Google Scholar]
- 63.You, S., and R. Padmanabhan. 1999. A novel in vitro replication system for dengue virus: initiation of RNA synthesis at the 3′-end of exogenous viral RNA templates requires 5′- and 3′-terminal complementary sequence motifs of the viral RNA. J. Biol. Chem. 274:33714-33722. [DOI] [PubMed] [Google Scholar]
- 64.You, S., B. Falgout, L. Markoff, and R. Padmanabhan. 2001. In vitro RNA synthesis from exogenous dengue viral RNA templates requires long range interactions between 5′- and 3′-terminal regions that influence RNA structure. J. Biol. Chem. 276:15581-15591. [DOI] [PubMed] [Google Scholar]
- 65.Zeng, L., B. Falgout, and L. Markoff. 1998. Identification of specific nucleotide sequences within the conserved 3′-SL in the dengue type 2 virus genome required for replication. J. Virol. 72:7510-7522. [DOI] [PMC free article] [PubMed] [Google Scholar]