Abstract
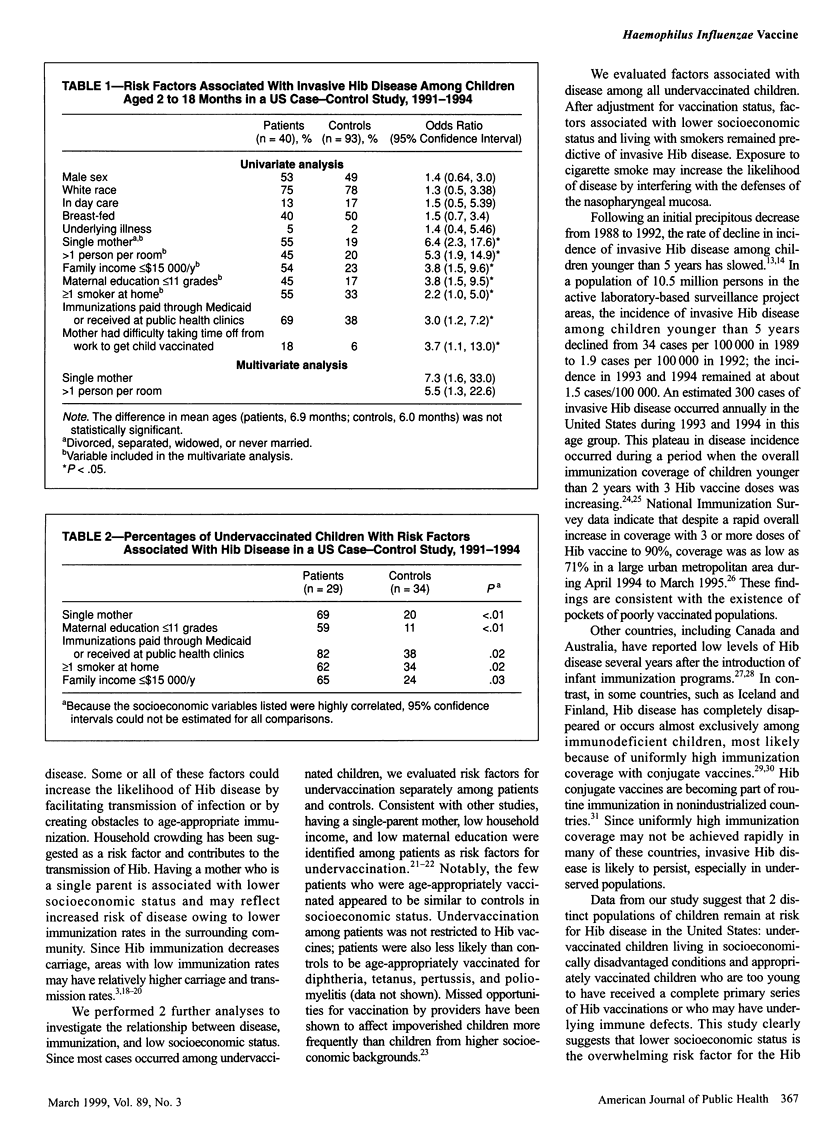
OBJECTIVES: The purpose of this study was to evaluate the effectiveness of Haemophilus influenzae type b (Hib) conjugate vaccines among children aged 2 to 18 months and to determine risk factors for invasive Hib disease during a period of declining incidence (1991-1994). METHODS: A prospective population-based case-control study was conducted in a multistate US population of 15.5 million. A laboratory-based active surveillance system was used for case detection. RESULTS: In a multivariate analysis, having a single-parent mother (odds ratio [OR] = 4.3, 95% confidence interval [CI] = 1.2, 14.8) and household crowding (OR = 3.5, 95% CI = 1.03, 11.7) were risk factors for Hib disease independent of vaccination status. After adjustment for these risk factors, the protective efficacy of 2 or more Hib vaccine doses was 86% (95% CI = 16%, 98%). Among undervaccinated subjects, living with a smoker (P = .02) and several indicators of lower socioeconomic status were risk factors for Hib disease. CONCLUSIONS: Hib disease still occurs at low levels in the United States, predominantly in socioeconomically disadvantaged populations. Low immunization coverage may facilitate continuing transmission of Hib. Special efforts to achieve complete and timely immunization in disadvantaged populations are needed.
Full text
PDF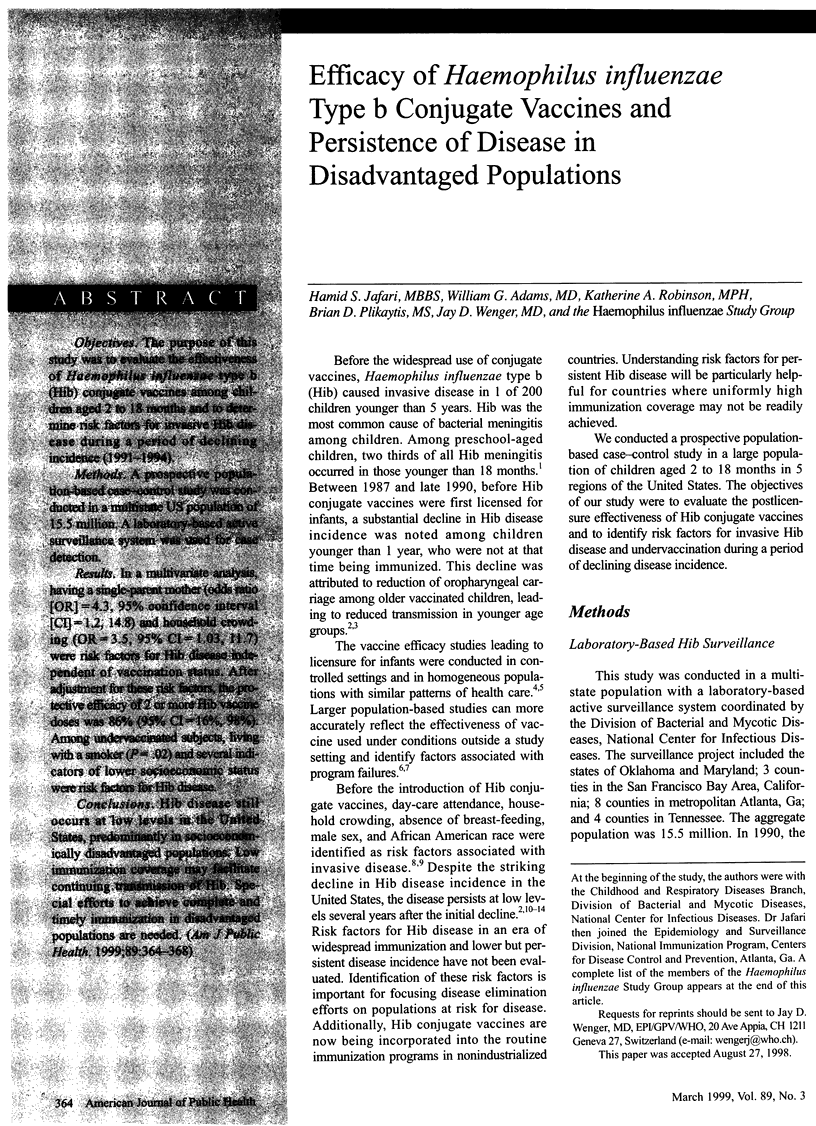



Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Adams W. G., Deaver K. A., Cochi S. L., Plikaytis B. D., Zell E. R., Broome C. V., Wenger J. D. Decline of childhood Haemophilus influenzae type b (Hib) disease in the Hib vaccine era. JAMA. 1993 Jan 13;269(2):221–226. [PubMed] [Google Scholar]
- Barbour M. L., Mayon-White R. T., Coles C., Crook D. W., Moxon E. R. The impact of conjugate vaccine on carriage of Haemophilus influenzae type b. J Infect Dis. 1995 Jan;171(1):93–98. doi: 10.1093/infdis/171.1.93. [DOI] [PubMed] [Google Scholar]
- Bates A. S., Fitzgerald J. F., Dittus R. S., Wolinsky F. D. Risk factors for underimmunization in poor urban infants. JAMA. 1994 Oct 12;272(14):1105–1110. [PubMed] [Google Scholar]
- Bisgard K. M., Kao A., Leake J., Strebel P. M., Perkins B. A., Wharton M. Haemophilus influenzae invasive disease in the United States, 1994-1995: near disappearance of a vaccine-preventable childhood disease. Emerg Infect Dis. 1998 Apr-Jun;4(2):229–237. doi: 10.3201/eid0402.980210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Black S. B., Shinefield H. R., Fireman B., Hiatt R., Polen M., Vittinghoff E. Efficacy in infancy of oligosaccharide conjugate Haemophilus influenzae type b (HbOC) vaccine in a United States population of 61,080 children. The Northern California Kaiser Permanente Vaccine Study Center Pediatrics Group. Pediatr Infect Dis J. 1991 Feb;10(2):97–104. doi: 10.1097/00006454-199102000-00004. [DOI] [PubMed] [Google Scholar]
- Black S. B., Shinefield H. R. Immunization with oligosaccharide conjugate Haemophilus influenzae type b (HbOC) vaccine on a large health maintenance organization population: extended follow-up and impact on Haemophilus influenzae disease epidemiology. The Kaiser Permanente Pediatric Vaccine Study Group. Pediatr Infect Dis J. 1992 Aug;11(8):610–613. [PubMed] [Google Scholar]
- Bobo J. K., Gale J. L., Thapa P. B., Wassilak S. G. Risk factors for delayed immunization in a random sample of 1163 children from Oregon and Washington. Pediatrics. 1993 Feb;91(2):308–314. [PubMed] [Google Scholar]
- Broadhurst L. E., Erickson R. L., Kelley P. W. Decreases in invasive Haemophilus influenzae diseases in US Army children, 1984 through 1991. JAMA. 1993 Jan 13;269(2):227–231. [PubMed] [Google Scholar]
- Cochi S. L., Broome C. V., Hightower A. W. Immunization of US children with Hemophilus influenzae type b polysaccharide vaccine. A cost-effectiveness model of strategy assessment. JAMA. 1985 Jan 25;253(4):521–529. [PubMed] [Google Scholar]
- Cochi S. L., Fleming D. W., Hightower A. W., Limpakarnjanarat K., Facklam R. R., Smith J. D., Sikes R. K., Broome C. V. Primary invasive Haemophilus influenzae type b disease: a population-based assessment of risk factors. J Pediatr. 1986 Jun;108(6):887–896. doi: 10.1016/s0022-3476(86)80922-2. [DOI] [PubMed] [Google Scholar]
- Hueston W. J., Mainous A. G., 3rd, Palmer C. Delays in childhood immunizations in public and private settings. Arch Pediatr Adolesc Med. 1994 May;148(5):470–473. doi: 10.1001/archpedi.1994.02170050028005. [DOI] [PubMed] [Google Scholar]
- Istre G. R., Conner J. S., Broome C. V., Hightower A., Hopkins R. S. Risk factors for primary invasive Haemophilus influenzae disease: increased risk from day care attendance and school-aged household members. J Pediatr. 1985 Feb;106(2):190–195. doi: 10.1016/s0022-3476(85)80285-7. [DOI] [PubMed] [Google Scholar]
- Mohle-Boetani J. C., Ajello G., Breneman E., Deaver K. A., Harvey C., Plikaytis B. D., Farley M. M., Stephens D. S., Wenger J. D. Carriage of Haemophilus influenzae type b in children after widespread vaccination with conjugate Haemophilus influenzae type b vaccines. Pediatr Infect Dis J. 1993 Jul;12(7):589–593. doi: 10.1097/00006454-199307000-00009. [DOI] [PubMed] [Google Scholar]
- Murphy T. V., Pastor P., Medley F., Osterholm M. T., Granoff D. M. Decreased Haemophilus colonization in children vaccinated with Haemophilus influenzae type b conjugate vaccine. J Pediatr. 1993 Apr;122(4):517–523. doi: 10.1016/s0022-3476(05)83529-2. [DOI] [PubMed] [Google Scholar]
- Murphy T. V., White K. E., Pastor P., Gabriel L., Medley F., Granoff D. M., Osterholm M. T. Declining incidence of Haemophilus influenzae type b disease since introduction of vaccination. JAMA. 1993 Jan 13;269(2):246–248. [PubMed] [Google Scholar]
- Peltola H., Kilpi T., Anttila M. Rapid disappearance of Haemophilus influenzae type b meningitis after routine childhood immunisation with conjugate vaccines. Lancet. 1992 Sep 5;340(8819):592–594. doi: 10.1016/0140-6736(92)92117-x. [DOI] [PubMed] [Google Scholar]
- Santosham M., Wolff M., Reid R., Hohenboken M., Bateman M., Goepp J., Cortese M., Sack D., Hill J., Newcomer W. The efficacy in Navajo infants of a conjugate vaccine consisting of Haemophilus influenzae type b polysaccharide and Neisseria meningitidis outer-membrane protein complex. N Engl J Med. 1991 Jun 20;324(25):1767–1772. doi: 10.1056/NEJM199106203242503. [DOI] [PubMed] [Google Scholar]
- Scheifele D., Gold R., Marchessault V., Duclos P. Failures after immunization with Haemophilus influenzae type b vaccines--1991-1995. Can Commun Dis Rep. 1996 Feb 1;22(3):17-20, 23. [PubMed] [Google Scholar]
- Takala A. K., Eskola J., Leinonen M., Käyhty H., Nissinen A., Pekkanen E., Mäkelä P. H. Reduction of oropharyngeal carriage of Haemophilus influenzae type b (Hib) in children immunized with an Hib conjugate vaccine. J Infect Dis. 1991 Nov;164(5):982–986. doi: 10.1093/infdis/164.5.982. [DOI] [PubMed] [Google Scholar]
- Vadheim C. M., Greenberg D. P., Eriksen E., Hemenway L., Christenson P., Ward B., Mascola L., Ward J. I. Protection provided by Haemophilus influenzae type b conjugate vaccines in Los Angeles County: a case-control study. Pediatr Infect Dis J. 1994 Apr;13(4):274–280. doi: 10.1097/00006454-199404000-00006. [DOI] [PubMed] [Google Scholar]
- Wenger J. D., Pierce R., Deaver K. A., Plikaytis B. D., Facklam R. R., Broome C. V. Efficacy of Haemophilus influenzae type b polysaccharide-diphtheria toxoid conjugate vaccine in US children aged 18-59 months. Haemophilus Influenzae Vaccine Efficacy Study Group. Lancet. 1991 Aug 17;338(8764):395–398. [PubMed] [Google Scholar]


