Abstract
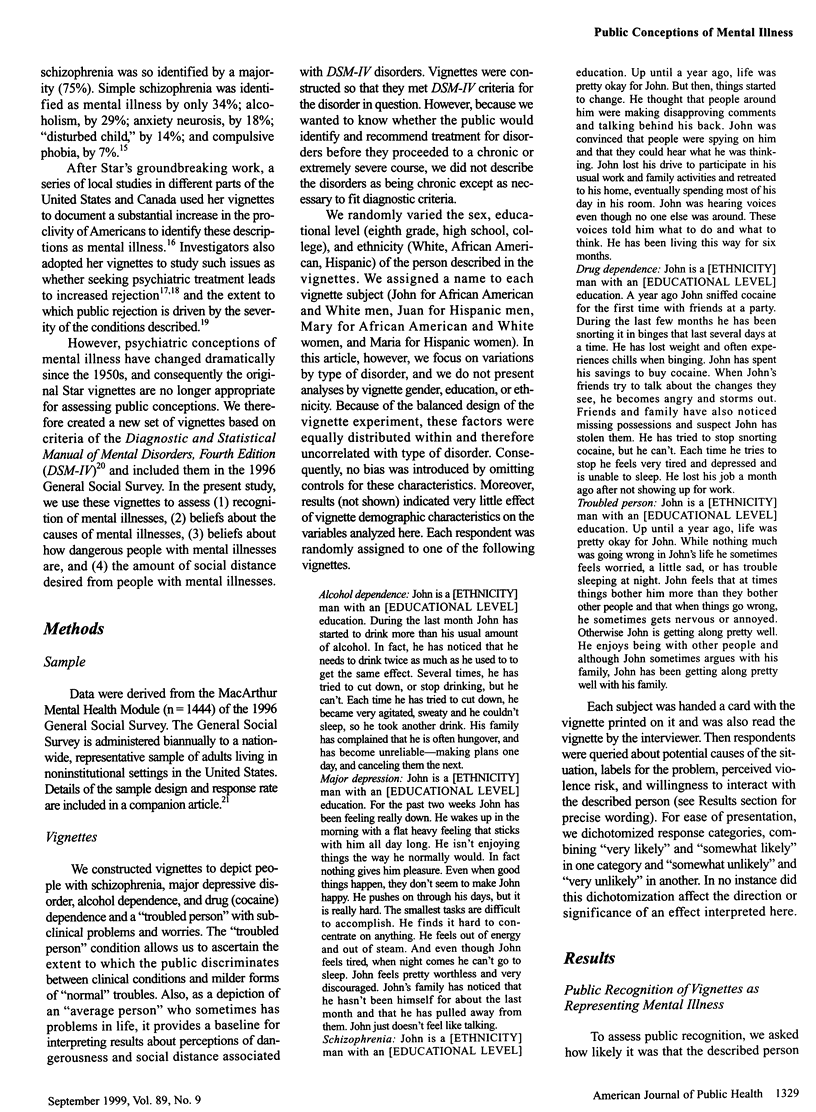
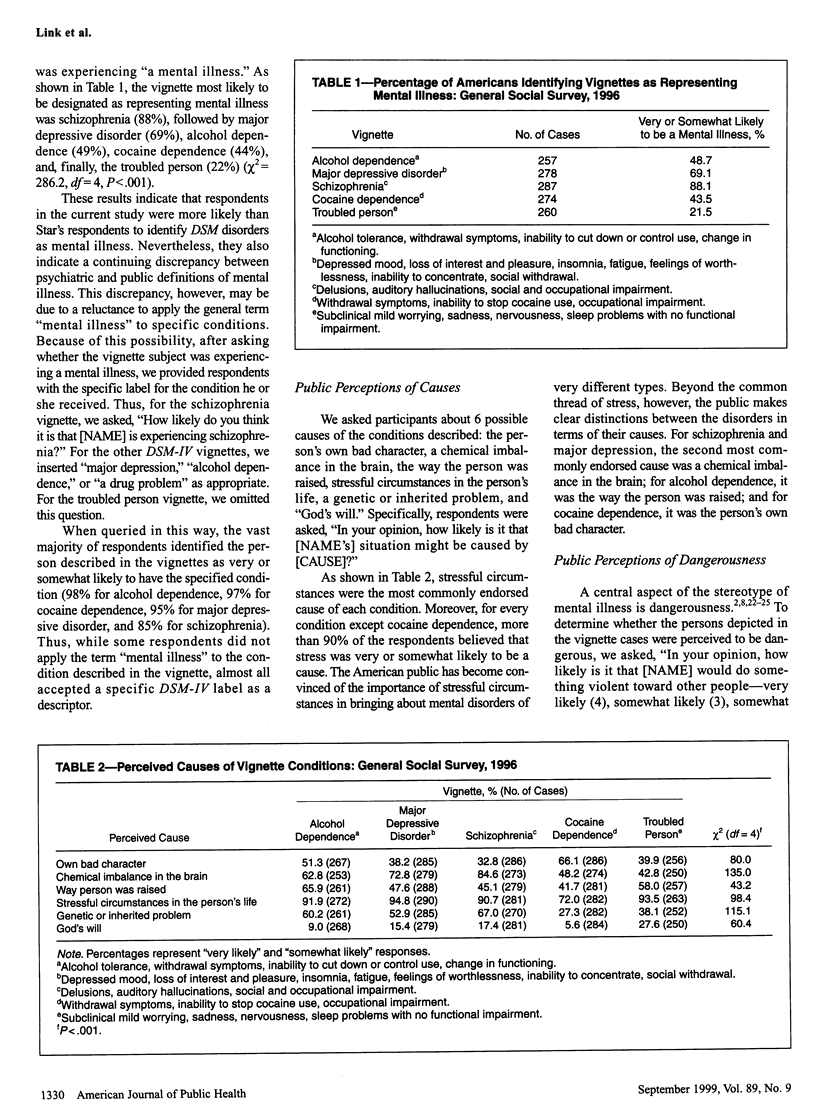
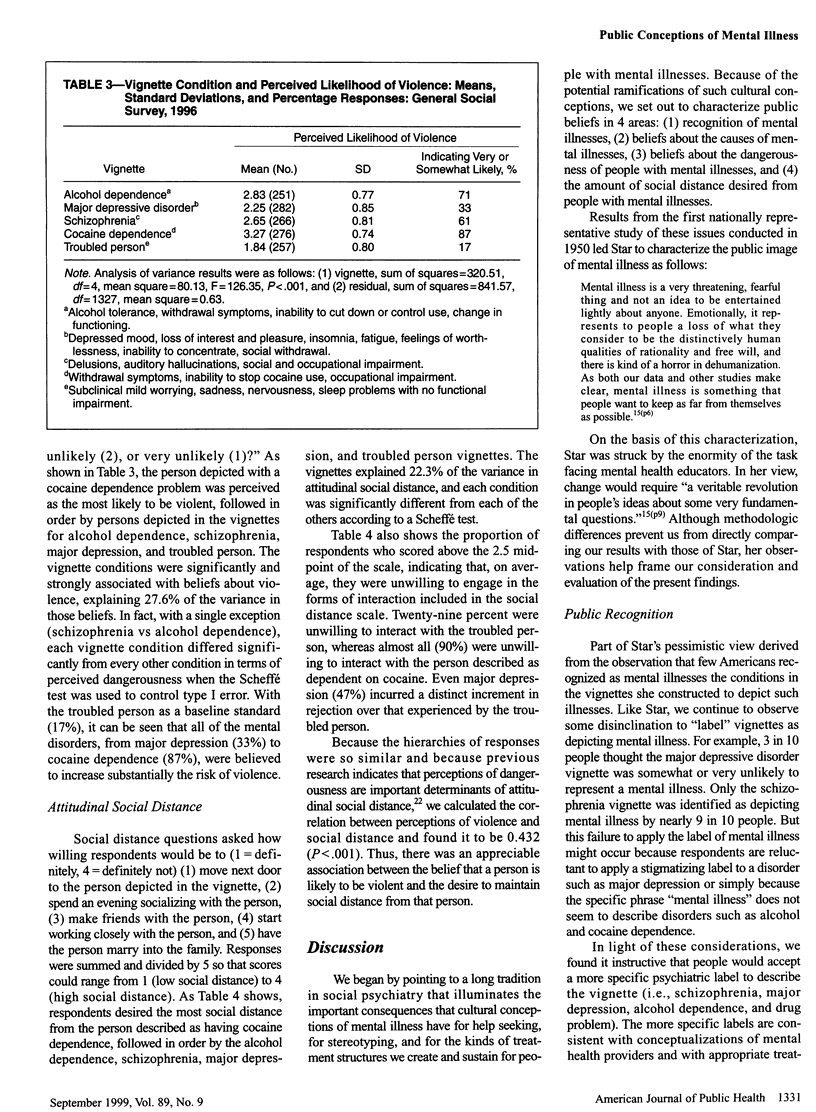
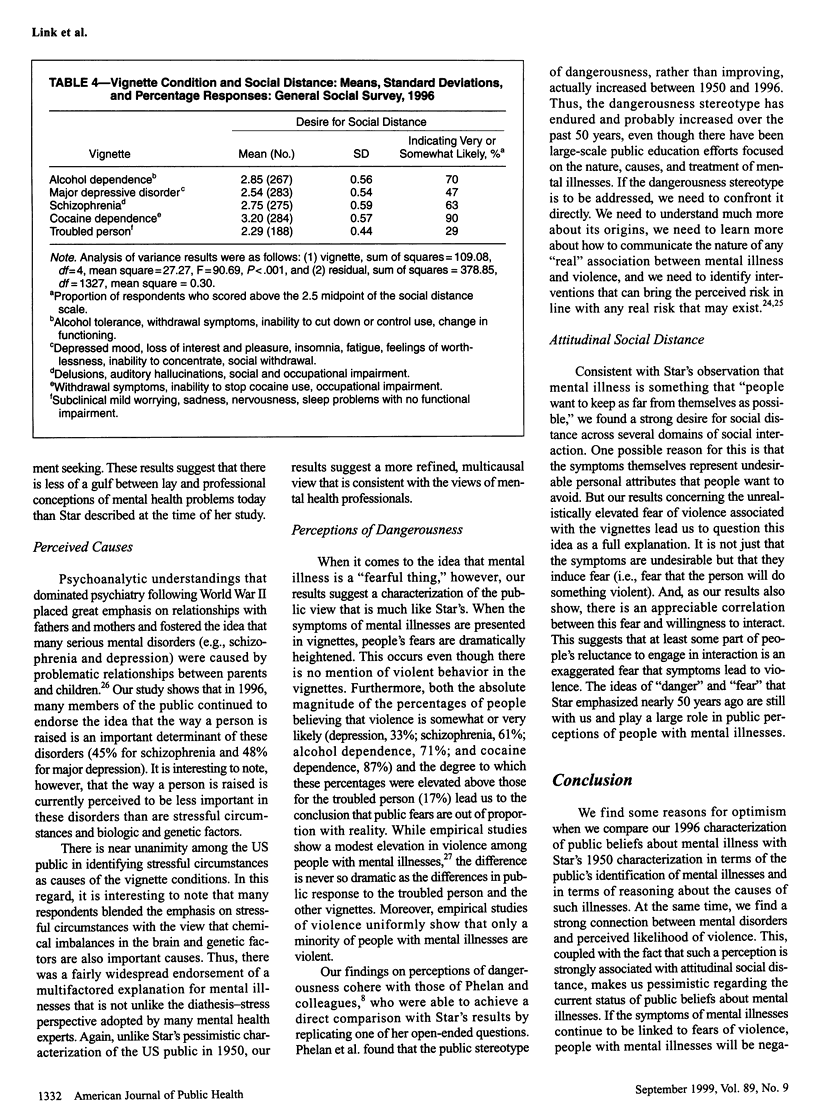
OBJECTIVES: The authors used nationwide survey data to characterize current public conceptions related to recognition of mental illness and perceived causes, dangerousness, and desired social distance. METHODS: Data were derived from a vignette experiment included in the 1996 General Social Survey. Respondents (n = 1444) were randomly assigned to 1 of 5 vignette conditions. Four vignettes described psychiatric disorders meeting diagnostic criteria, and the fifth depicted a "troubled person" with subclinical problems and worries. RESULTS: Results indicate that the majority of the public identifies schizophrenia (88%) and major depression (69%) as mental illnesses and that most report multicausal explanations combining stressful circumstances with biologic and genetic factors. Results also show, however, that smaller proportions associate alcohol (49%) or drug (44%) abuse with mental illness and that symptoms of mental illness remain strongly connected with public fears about potential violence and with a desire for limited social interaction. CONCLUSIONS: While there is reason for optimism in the public's recognition of mental illness and causal attributions, a strong stereotype of dangerousness and desire for social distance persist. These latter conceptions are likely to negatively affect people with mental illness.
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Angermeyer M. C., Link B. G., Majcher-Angermeyer A. Stigma perceived by patients attending modern treatment settings. Some unanticipated effects of community psychiatry reforms. J Nerv Ment Dis. 1987 Jan;175(1):4–11. doi: 10.1097/00005053-198701000-00002. [DOI] [PubMed] [Google Scholar]
- Angermeyer M. C., Matschinger H. The effect of violent attacks by schizophrenic persons on the attitude of the public towards the mentally ill. Soc Sci Med. 1996 Dec;43(12):1721–1728. doi: 10.1016/s0277-9536(96)00065-2. [DOI] [PubMed] [Google Scholar]
- Arens D. A. What do the neighbors think now? Community residences on Long Island, New York. Community Ment Health J. 1993 Jun;29(3):235–245. doi: 10.1007/BF00778809. [DOI] [PubMed] [Google Scholar]
- D'Arcy C., Brockman J. Changing public recognition of psychiatric symptoms? Blackfoot revisited. J Health Soc Behav. 1976 Sep;17(3):302–310. [PubMed] [Google Scholar]
- Greenley J. R., Mechanic D., Cleary P. D. Seeking help for psychologic problems. A replication and extension. Med Care. 1987 Dec;25(12):1113–1128. doi: 10.1097/00005650-198712000-00001. [DOI] [PubMed] [Google Scholar]
- Kessler R. C., McGonagle K. A., Zhao S., Nelson C. B., Hughes M., Eshleman S., Wittchen H. U., Kendler K. S. Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States. Results from the National Comorbidity Survey. Arch Gen Psychiatry. 1994 Jan;51(1):8–19. doi: 10.1001/archpsyc.1994.03950010008002. [DOI] [PubMed] [Google Scholar]
- Link B. G., Cullen F. T. Reconsidering the social rejection of ex-mental patients: levels of attitudinal response. Am J Community Psychol. 1983 Jun;11(3):261–273. doi: 10.1007/BF00893367. [DOI] [PubMed] [Google Scholar]
- Link B. G., Struening E. L., Rahav M., Phelan J. C., Nuttbrock L. On stigma and its consequences: evidence from a longitudinal study of men with dual diagnoses of mental illness and substance abuse. J Health Soc Behav. 1997 Jun;38(2):177–190. [PubMed] [Google Scholar]
- Markowitz F. E. The effects of stigma on the psychological well-being and life satisfaction of persons with mental illness. J Health Soc Behav. 1998 Dec;39(4):335–347. [PubMed] [Google Scholar]
- Penn D. L., Guynan K., Daily T., Spaulding W. D., Garbin C. P., Sullivan M. Dispelling the stigma of schizophrenia: what sort of information is best? Schizophr Bull. 1994;20(3):567–578. doi: 10.1093/schbul/20.3.567. [DOI] [PubMed] [Google Scholar]
- Pescosolido B. A., Gardner C. B., Lubell K. M. How people get into mental health services: stories of choice, coercion and "muddling through" from "first-timers". Soc Sci Med. 1998 Jan;46(2):275–286. doi: 10.1016/s0277-9536(97)00160-3. [DOI] [PubMed] [Google Scholar]
- Pescosolido B. A., Monahan J., Link B. G., Stueve A., Kikuzawa S. The public's view of the competence, dangerousness, and need for legal coercion of persons with mental health problems. Am J Public Health. 1999 Sep;89(9):1339–1345. doi: 10.2105/ajph.89.9.1339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shapiro S., Skinner E. A., Kessler L. G., Von Korff M., German P. S., Tischler G. L., Leaf P. J., Benham L., Cottler L., Regier D. A. Utilization of health and mental health services. Three Epidemiologic Catchment Area sites. Arch Gen Psychiatry. 1984 Oct;41(10):971–978. doi: 10.1001/archpsyc.1984.01790210053007. [DOI] [PubMed] [Google Scholar]
- Swanson J. W., Holzer C. E., 3rd, Ganju V. K., Jono R. T. Violence and psychiatric disorder in the community: evidence from the Epidemiologic Catchment Area surveys. Hosp Community Psychiatry. 1990 Jul;41(7):761–770. doi: 10.1176/ps.41.7.761. [DOI] [PubMed] [Google Scholar]



