Abstract
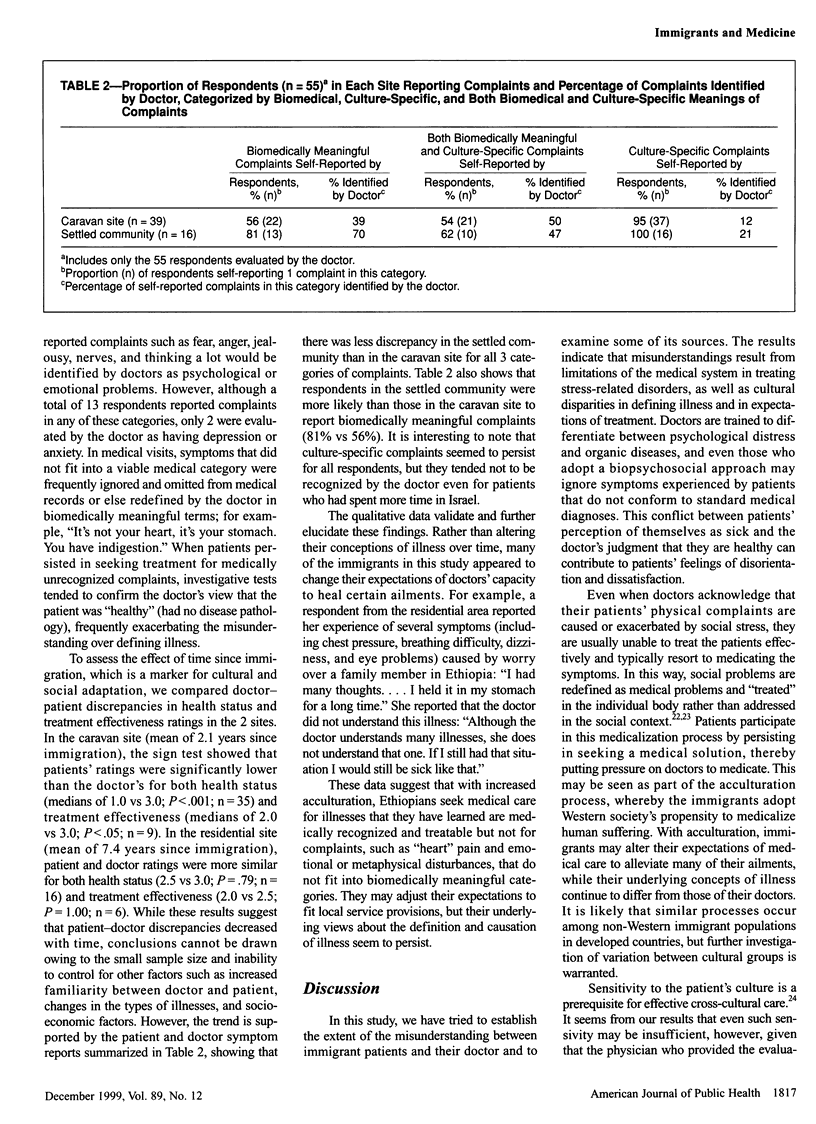
OBJECTIVES: Patient-provider misunderstandings arising from disparate medical and cultural concepts can impede health care among immigrant populations. This study assessed the extent of disagreement and identified the salient problems of communication between Israeli doctors and Ethiopian immigrant patients. METHODS: Semistructured interviews were conducted with 59 Ethiopian immigrants. Self-reports of health status and effectiveness of treatment were compared with evaluations by the primary care physician and supplemented by qualitative data from descriptions of illness, observations of medical visits, informant interviews, and participant observations conducted by the anthropologist. RESULTS: Health status and effectiveness of treatment were rated significantly higher by the doctor than by the patients. Low doctor-patient agreement occurred mainly for illnesses with stress-related or culture-specific associations. Qualitative data suggested that more long-term immigrants may alter their expectations of treatment but continue to experience symptoms that are culturally, but not biomedically, meaningful. CONCLUSIONS: Misunderstandings between immigrant patients and their doctors emerge from the biomedical system's limitations in addressing stress-related illnesses and from culture-based discrepancies in concepts of illness and healing. Including trained translators in medical teams can reduce medical misunderstandings and increase patient satisfaction among immigrant populations.
Full text
PDF



Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Anderson J. M. Immigrant women speak of chronic illness: the social construction of the devalued self. J Adv Nurs. 1991 Jun;16(6):710–717. doi: 10.1111/j.1365-2648.1991.tb01729.x. [DOI] [PubMed] [Google Scholar]
- Beiser M., Edwards R. G. Mental health of immigrants and refugees. New Dir Ment Health Serv. 1994 Spring;(61):73–86. doi: 10.1002/yd.23319946110. [DOI] [PubMed] [Google Scholar]
- Budman C. L., Lipson J. G., Meleis A. I. The cultural consultant in mental health care: the case of an Arab adolescent. Am J Orthopsychiatry. 1992 Jul;62(3):359–370. doi: 10.1037/h0079347. [DOI] [PubMed] [Google Scholar]
- Cave A., Maharaj U., Gibson N., Jackson E. Physicians and immigrant patients. Cross-cultural communication. Can Fam Physician. 1995 Oct;41:1685–1690. [PMC free article] [PubMed] [Google Scholar]
- Ferron M. La symptomatologie transculturelle. Son expression en médecine familiale. Can Fam Physician. 1995 Oct;41:1718–1725. [PMC free article] [PubMed] [Google Scholar]
- Garrity T. F., Somes G. W., Marx M. B. Factors influencing self-assessment of health. Soc Sci Med. 1978 Mar;12(2A):77–81. [PubMed] [Google Scholar]
- Greenfield S. F., Borkan J., Yodfat Y. Health beliefs and hypertension: a case-control study in a Moroccan Jewish community in Israel. Cult Med Psychiatry. 1987 Mar;11(1):79–95. doi: 10.1007/BF00055010. [DOI] [PubMed] [Google Scholar]
- Hodes R. M., Teferedegne B. Traditional beliefs and disease practices of Ethiopian Jews. Isr J Med Sci. 1996 Jul;32(7):561–567. [PubMed] [Google Scholar]
- Hull D. Migration, adaptation, and illness: a review. Soc Sci Med Med Psychol Med Sociol. 1979 Jan;13A(1):25–36. doi: 10.1016/0160-7979(79)90005-5. [DOI] [PubMed] [Google Scholar]
- Kaplan G. A., Camacho T. Perceived health and mortality: a nine-year follow-up of the human population laboratory cohort. Am J Epidemiol. 1983 Mar;117(3):292–304. doi: 10.1093/oxfordjournals.aje.a113541. [DOI] [PubMed] [Google Scholar]
- Kaufert J. M., Koolage W. W. Role conflict among 'culture brokers': the experience of native Canadian medical interpreters. Soc Sci Med. 1984;18(3):283–286. doi: 10.1016/0277-9536(84)90092-3. [DOI] [PubMed] [Google Scholar]
- Meleis A. I. Between two cultures: identity, roles, and health. Health Care Women Int. 1991 Oct-Dec;12(4):365–377. doi: 10.1080/07399339109515961. [DOI] [PubMed] [Google Scholar]
- Mossey J. M., Shapiro E. Self-rated health: a predictor of mortality among the elderly. Am J Public Health. 1982 Aug;72(8):800–808. doi: 10.2105/ajph.72.8.800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phelan M., Parkman S. How to work with an interpreter. BMJ. 1995 Aug 26;311(7004):555–557. doi: 10.1136/bmj.311.7004.555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singer E., Garfinkel R., Cohen S. M., Srole L. Mortality and mental health: evidence from the Midtown Manhattan Restudy. Soc Sci Med. 1976 Nov-Dec;10(11-12):517–525. doi: 10.1016/0037-7856(76)90019-6. [DOI] [PubMed] [Google Scholar]
- Taussig M. T. Reification and the consciousness of the patient. Soc Sci Med Med Anthropol. 1980 Feb;14B(1):3–13. doi: 10.1016/0160-7987(80)90035-6. [DOI] [PubMed] [Google Scholar]
- Vasquez C., Javier R. A. The problem with interpreters: communicating with Spanish-speaking patients. Hosp Community Psychiatry. 1991 Feb;42(2):163–165. doi: 10.1176/ps.42.2.163. [DOI] [PubMed] [Google Scholar]
- Ware J. E., Jr, Brook R. H., Davies A. R., Lohr K. N. Choosing measures of health status for individuals in general populations. Am J Public Health. 1981 Jun;71(6):620–625. doi: 10.2105/ajph.71.6.620. [DOI] [PMC free article] [PubMed] [Google Scholar]


