Abstract
Deficiency of the Golgi enzyme UDP-Gal:N-acetylglucosamine β-1,4-galactosyltransferase I (β4GalT I) (E.C.2.4.1.38) causes a new congenital disorder of glycosylation (CDG), designated type IId (CDG-IId), a severe neurologic disease characterized by a hydrocephalus, myopathy, and blood-clotting defects. Analysis of oligosaccharides from serum transferrin by HPLC, mass spectrometry, and lectin binding revealed the loss of sialic acid and galactose residues. In skin fibroblasts and leukocytes, galactosyltransferase activity was reduced to 5% that of controls. In fibroblasts, a truncated polypeptide was detected that was about 12 kDa smaller in size than wild-type β4GalT I and that failed to localize to the Golgi apparatus. Sequencing of the β4GalT I cDNA and gene revealed an insertion of a single nucleotide (1031-1032insC) leading to premature translation stop and loss of the C-terminal 50 amino acids of the enzyme. The patient was homozygous and his parents heterozygous for this mutation. Expression of a corresponding mutant cDNA in COS-7 cells led to the synthesis of a truncated, inactive polypeptide, which localized to the endoplasmic reticulum.
Introduction
The congenital disorders of glycosylation (CDGs) comprise a rapidly growing group of inherited multisystemic disorders that are commonly associated with severe psychomotor and mental retardation. The characteristic biochemical feature of CDGs is the defective glycosylation of glycoproteins due to mutations in genes required for the biosynthesis of N-linked oligosaccharides. Defects of the assembly of lipid-linked oligosaccharides or their transfer onto nascent glycoproteins form type I of CDG, whereas CDG type II comprises all defects of trimming and elongating of N-linked oligosaccharides (1). N-glycosylation defects are routinely detected by isoelectric focusing (IEF) of serum transferrin, which normally carries two sialylated biantennary N-linked oligosaccharides. The hyposialylated transferrin from CDG patients shows a cathodic shift, which in CDG-I is due to the loss of either one or both oligosaccharides and in CDG-II is due to the incomplete processing of protein-bound oligosaccharides. In the past six years the molecular nature of six CDG-I and three CDG-II types has been described (2–16).
Here we present a new type of CDG-II, designated CDG-IId, in which UDP-Gal:N-acetylglucosamine β-1,4-galactosyltransferase I (β4GalT I) is deficient. β4GalT I belongs to a family of at least six related β-1,4-galactosyltransferases. Although the genes for all β-1,4-galactosyltransferases are located at different chromosomal loci, the evolutionary relationship is indicated by a 30–55% amino acid identity. Moreover, they have in common the localization in the Golgi apparatus, the topology of type II membrane proteins, and the transfer of galactose from UDP-galactose onto the C4-hydroxyl group of GlcNAc residues. The enzymes differ in their substrate specificity for glycoproteins and glycolipids and their ability to synthesize lactose in mammals (17). In Chinese hamster ovary cells, which express all six galactosyltransferases, β4GalT I is the main transferase responsible for galactosylation of protein N-linked oligosaccharides (18).
The β4GalT deficiency was identified in a 16-month-old boy with mental retardation, a hydrocephalus due to a Dandy-Walker malformation, blood-clotting problems, and myopathy (19). The deficiency of β4GalT I activity is caused by the insertion of a single nucleotide in the β4GalT I gene, leading to premature translation stop and loss of the C-terminal 50 amino acids of β4GalT I. The mutant enzyme is retained in the endoplasmic reticulum (ER).
Methods
Clinical phenotype.
The now 2.5-year-old boy M.S. is the child of non-consanguineous parents of Turkish origin. He was born in term; however, vacuum extraction was needed due to a macrocephaly. At the day of birth, severe abdominal bleeding due to rupture of the hepatic capsule needed surgical intervention. At the age of 4 months, the insertion of a cystoperitoneal shunt was necessary due to progression of the hydrocephalus caused by a Dandy-Walker malformation. Muscular hypotonia and reduced muscle mass were noted. A myopathy was indicated by the elevated levels of creatine kinase and by electromyography. Further laboratory results showed a consistently prolonged activated partial thromboplastin time and elevated aspartate transaminase values. Determination of the carbohydrate-deficient transferrin fraction (20) showed a severe hyposialylation. This led to further analysis of serum transferrin by IEF and SDS-PAGE. The abnormal glycosylation of transferrin established the diagnosis of CDG. An extensive description of the clinical phenotype of the CDG-IId patient can be found in the case report of the patient (19).
Antibodies.
Rabbit polyclonal antibodies to soluble human-milk β4GalT I were affinity-purified on recombinant GalT1–β-galactosidase fusion protein expressed in Escherichia coli (21, 22) and used at 0.1 mg/ml unless otherwise stated. The mAb’s against the Golgi protein GP130 and the ER protein CLIMP-63 were obtained from H.P. Hauri (Zürich, Switzerland) (23, 24). Secondary antibodies labeled with horseradish peroxidase for Western blot analysis and fluorochrome-conjugated antibodies used for immunofluorescence were obtained from Dianova (Hamburg, Germany).
Analysis of transferrin-linked N-glycans.
Transferrin was purified from control and patient’s serum following the method of Iourin et al. (25), except that dialysis was carried out against 10 mM Tris/HCl, pH 7.4, overnight in a dialysis tube with a cutoff mass of 12–16 kDa. Further purification was carried out by reversed phase–HPLC (RP-HPLC) (SMART HPLC System; Amersham Biosciences, Freiburg, Germany), using an Aquapore butyl column (Perkin Elmer Instruments, Rodgau-Jügesheim, Germany). Gradient conditions were as follows: Solvent A was 0.1% trifluoroacetic acid (TFA) in water, and solvent B was 0.1% TFA, 90% acetonitrile, 9.9% water. Initial conditions were 100% solvent A. The flow rate was kept constant during the whole run at 300 μl/min. These conditions were kept on for the first 5 minutes. After 1 minute, the samples (applied as received from dialysis) were automatically injected. This was followed by a linear gradient of 0–100% of solvent B for 45 minutes, followed by 100–0% solvent B for 6 minutes, followed by 100% solvent A for 5 minutes. The amount of eluting human transferrin (hTf) was determined by integrating the chromatogram.
After RP-HPLC, hTf was freeze-dried and dissolved in water, and the glycans were released by enzymatic deglycosylation with PNGase F (Roche Diagnostics GmbH, Mannheim, Germany). The samples (5–30 μl) were added to 0.1 M β-mercaptoethanol/0.5% SDS to a total volume of 90 μl and heated 5 minutes at 95°C. Seventy-five microliters 0.5 M Tris/HCl (pH 8.0), 30 μl 0.1 M 1,10-phenanthrolene, 30 μl 10% Triton X-100, and 2.5 μl PNGase F were added and incubated overnight at 37°C. The enzymatic digestion was stopped by heating 5 minutes at 95°C. Desalting of the enzymatically released glycans was performed by using GlycoClean S cleanup cartridges (GLYKO, Bicester, United Kingdom). The GlycoClean S cartridges were washed with 1 ml water, followed by 5 ml 30% acetic acid, followed by 1 ml acetonitrile. Then the glycans were applied to the disc and allowed to adsorb for 15 minutes, followed by addition of 100 μl acetonitrile, which was used to rinse the corresponding vial. Each cartridge was washed with 1 ml acetonitrile, followed by 5× 1 ml 96% acetonitrile/water. The remaining glycans were eluted by washing with 3× 0.5 ml water, followed by freeze drying. The desalted hTf glycans were fluorescently labeled with 2-amino benzamide (2-AB) as described by Bigge et al. (26) and analyzed by HPLC on a GlycoSepN column (GLYKO). Samples were applied in 65% acetonitrile and 35% 250 mM ammonium formate (pH 4.4). Gradient conditions were as follows: Solvent A was acetonitrile, solvent B was 250 mM ammoniumformate (pH 4.4). Initial conditions were 65% solvent A (0.4 ml/min). Subsequent elutions were in the following sequence: linear gradient of 65–47% solvent A (0.4 ml/min) for 72 minutes, linear gradient of 47–0% solvent A (0.4 ml/min) for 3 minutes, 100% solvent B (0.4 ml/min) for 2 minutes, followed by 100% solvent B (1.0 ml/min) for 15 minutes, linear gradient 0–65% solvent A (1.0 ml/min) for 3 minutes, and 65% solvent A (0.4 ml/min) for 5 minutes. The eluting fractions of oligosaccharides were fractionated automatically, freeze-dried, and dissolved in water for further mass analysis.
Mass spectrometric analysis was performed on a Bruker REFLEX III (Bruker Daltonik GmbH, Bremen, Germany). 2,5-Dihydroxybenzoic acid (DHB) (Sigma-Aldrich Chemie GmbH, Taufkirchen, Germany) was used as the matrix. Two different solutions of DHB were made. Ten milligrams of DHB was solved in 500 μl acetone. This was applied to the slide as a thin layer. The glycans were dissolved in water, applied (0.5–1.0 μl) to the target, and dried under a slight airstream. 0.5 μl of the second DHB solution (10 mg DHB dissolved in 333 μl acetonitrile, 167 μl water, 10 μl 5% perfluorinated Nafion [Sigma-Aldrich Chemie GmbH], 0.5 μl TFA) was applied onto the glycans and dried again by a slight airstream.
The effective path length was 145 cm. The samples were ionized with a nitrogen laser at 337.1 nm. Charged oligosaccharides were analyzed by using the linear, negative mode; uncharged oligosaccharides were analyzed by using the linear, positive mode.
Ricinus communis agglutinin I staining of serum glycoproteins.
Lectin blot analysis was performed with 60 μg of control and patient’s serum protein per lane as described previously (27), using biotinylated Ricinus communis agglutinin I (RCA-I) lectin (Vector Laboratories Inc., Burlingame, California, USA).
Cell lines and cell culture.
Fibroblasts from patient M.S. and controls were cultivated at 37°C under 5% CO2 on DMEM (Life Technologies, Karlsruhe, Germany) containing 10% FCS (PAN Biotech GmbH, Aidenbach, Germany).
Determination of β4GalT I activity and UDP-[3H]galactose import.
In order to determine β4GalT I activity, 20 μl buffer A (10 mM Tris/HCl [pH7.7], 250 mM sucrose, 0.5% Triton X-100, 1 mM EDTA) containing 1 μg of cell homogenate was used. Reaction was started by the addition of 30 μl buffer B (5.2 μl 0.5 M Tris/HCl [pH7.4], 5% Triton X-100, 4.4 μl 0.2 M MnCl2, 19.85 μl H2O, 0.35 mg ovalbumin, 0.44 μl 0.2 M ATP, and 0.44 μCi UDP-[3H]galactose [16 Ci/mmol; Amersham Biosciences]). Incubation was carried out for 1 hour at 37°C and then stopped by adding 500 μl of a 10% TCA solution. Precipitation was carried out at 4°C for 1 hour. Samples were centrifuged at 13,600 g for 10 minutes at 4°C, and the supernatants were removed. The pellets were washed another three times with ice-cold 5% TCA. Pellets were resuspended in 200 μl 2.5N NaOH and incubated at 95°C for 10 minutes, followed by the addition of 600 μl H2O and 200 μl 100% acetic acid. Incorporated radioactivity was determined by liquid scintillation counting.
The import of UDP-[3H]galactose into Golgi-enriched vesicles from control and patient’s fibroblasts was assessed as described previously (28).
Mutation analysis.
Total RNA was extracted from control and patient’s fibroblasts using the RNeasy Kit (QIAGEN GmbH, Hilden, Germany). First-strand cDNA was synthesized from 2 μg RNA with Omniscript reverse transcriptase (QIAGEN GmbH) and the primer 3A (5′-GGACCAGCCCAGCAGATTGG-3′). In a first round of PCR, the cDNA was amplified by the primers 3A and 5A (5′-GGAATTCGGGGGCGGCCC-3′) using the HotStar Taq-Polymerase Kit (QIAGEN GmbH), with a preincubation at 95°C for 15 minutes followed by 25 cycles with 1 minute at 94°C, 1 minute at 58°C, and 3 minutes at 72°C. The nested PCR with 35 cycles was carried out with the primers 3B (5′-TCCCTGGCTAATTTCAGTCTC-3′) and 5B (5′-GGCGGCGGGAAGATGAGGC-3′). RT-PCR products were run on a 1% agarose gel. The 1248-bp fragment was extracted from the gel with the QIAquick Gel Extraction Kit (QIAGEN GmbH), subcloned into the pGEM-T Easy vector (Promega GmbH, Mannheim, Germany), and analyzed by dye-determined cycle sequencing with the primers pUC M13 forward and pUC M13 reverse (Stratagene Europe, Amsterdam, The Netherlands) on an Applied Biosystems model 373A automated sequencer.
Genomic DNA was prepared from ten control persons and the patient’s fibroblasts, as well as from peripheral blood leukocytes of the parents, by standard procedures (29). PCR was carried out with Taq DNA Polymerase (QIAGEN GmbH) and the primers Ex5-1 (5′-GCATGATGCTGGGTTGTGGG -3′) and Ex5-4 (5′-GTACTTCCTCCTCCCTCTCC-3′), with a preincubation at 94°C for 1 minute followed by 28 cycles with 1 minute at 94°C, 1 minute at 55°C, and 1.5 minutes at 72°C. The PCR products were run on a 1.5 % agarose gel, and the resulting 361-bp fragments were prepared as described above. Sequencing was carried out with the primer Ex5-2 (5′-GATGGTGGATGGAGCAACAG-3′).
Overexpression of control and patient’s β4GalT I cDNA in COS-7 cells.
Control and patient β4GalT I cDNA was generated as described above using Pfu-Turbo-Polymerase (Stratagene) instead of Taq-Polymerase. The blunt-ended PCR fragments were A-tailed and ligated into a pGEM-T Easy vector (Promega Corp.). Control and patient cDNAs were controlled by sequencing and subsequently subcloned into the EcoRI site of a pCI-neo vector (Promega GmbH), respectively. Correct insert orientation was determined by control SmaI digestion.
Twelve hours before transfection, 5 × 105 COS-7 cells were plated onto 6-cm dishes and cultured in DMEM (Life Technologies GmbH, Aidenbach, Germany) supplemented with 5% FCS (PAN Biotech GmbH, Aidenbach, Germany) under 5% CO2 atmosphere at 37°C. Transient transfection of COS-7 cells was performed using the QIAGEN Transfection Kit (QIAGEN GmbH) with 1 μg of patient, control, and vector DNA each. Twenty-four hours after transfection, the medium was changed. Cells were incubated for 48 hours. Cell monolayers were washed three times with ice-cold Hanks’ buffer and harvested by scrapping into 1.5 ml of the same buffer. Cells were lysed by sonification. Protein determination was carried out as described (30).
Determination of β4GalT I activity was carried out as described above. Expression of β4GalT I protein in COS-7 cells was shown by separation of 60 μg total cellular protein on a 10% SDS-PAGE gel followed by Western blot analysis using the β4GalT I antiserum as described above.
Immunofluorescence analysis of COS-7 cells and fibroblasts.
Transfected COS-7 cells and fibroblasts were grown on glass coverslips for 2 days. The cells were washed with PBS and fixed with 3% paraformaldehyde for 20 minutes. After blocking free aldehyde groups with 50 mM NH4Cl in PBS for 10 minutes, the cells were permeabilized with 0.5% Triton X-100. Subsequently the cells were incubated with antibodies against GP130, CLIMP-63, or β4GalT I as indicated for 1 hour at 37°C, washed with PBS, and then incubated with 10% goat serum in PBS for 20 minutes. Primary antibodies were detected by secondary antibodies conjugated to the fluorochromes CY2 or CY3. After washing with PBS, the cells were mounted in Fluoromount (DAKO Diagnostika GmbH, Hamburg, Germany) and analyzed using a confocal laser scanning microscope (LSM3; Carl Zeiss Göttingen, Göttingen, Germany).
Preparation of [2-3H]mannose–labeled glycopeptides and analysis by RCA-I lectin binding.
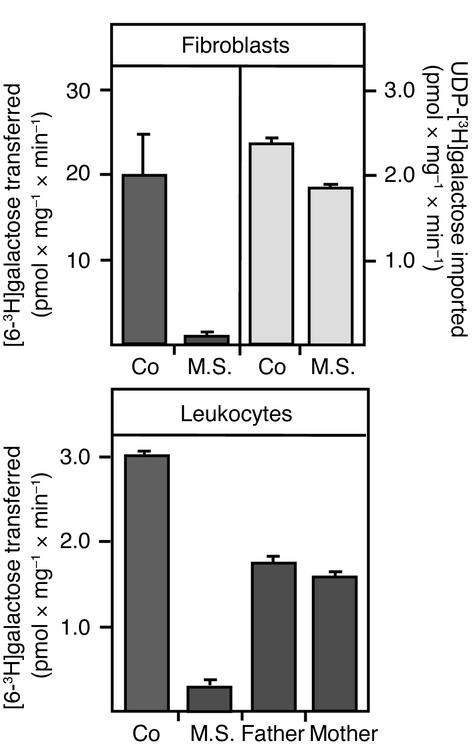
Glycopeptides of control and patient’s fibroblasts were metabolically labeled and prepared as described previously (28). Radiolabeled glycopeptides were subjected to lectin affinity chromatography on a column containing agarose-bound RCA-I lectin (Sigma-Aldrich Chemie GmbH). Elution of bound peptides was carried out with 0.1–10 mM β-lactose as indicated (see Figure 8) in TBS as described previously (31).
Figure 8.
Binding of [2-3H]mannose–labeled glycopeptides from control and CDG-IId patient’s fibroblasts to an RCA-I lectin column. Fibroblasts of a control and the CDG-IId patient were metabolically labeled with [2-3H]mannose, followed by preparation of glycopeptides as described in Methods. Radiolabeled glycopeptides were subjected to lectin affinity chromatography on a column containing agarose-bound RCA-I lectin. After washing, elution of bound peptides was carried out with 0.1–10 mM β-lactose as indicated.
Results
Partial lack of sialic acid and galactose residues in N-glycans linked to serum transferrin.
The diagnosis of CDG in patient M.S. was indicated by IEF of serum transferrin (19). While the bulk of serum transferrin from controls contains four sialic acid residues in two complex-type oligosaccharides, the patient’s transferrin contained mainly forms with no, one, or two sialic acid residues. The IEF pattern is different from that in CDG-I, where part of the transferrin lacks either one or both of its N-glycans and therefore contains two sialic acid residues or none (32), and different from that in CDG-IIa, where transferrin contains two sialic acid residues, each on a monoantennary N-linked oligosaccharide (12). In contrast to serum transferrin from CDG-Ia patients, which migrates faster in SDS-PAGE as transferrin from control persons due to the lack of one or two oligosaccharides, the transferrin from patient M.S. showed a different running profile. It migrated as a mobility intermediate between transferrins carrying one or two oligosaccharides indicating shortened oligosaccharides rather than the loss of either one or two N-glycan side chains (19).
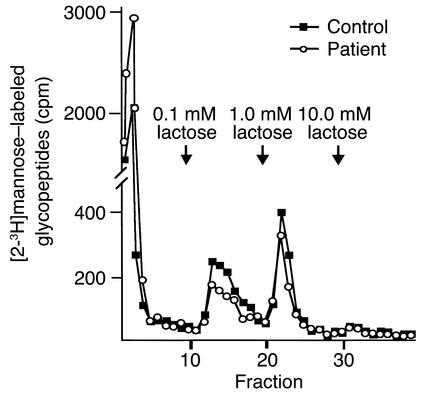
To analyze the oligosaccharide structure, transferrin was purified from control and patient’s serum. The oligosaccharides were released with peptide-N-glycosidase F and reductively aminated with the fluorophore 2-AB. Fractionation by HPLC showed that oligosaccharides from the patient eluted earlier (main peaks at 33 and 46 minutes; Figure 1, middle) than oligosaccharides from control transferrin (main peak at 57 minutes; Figure 1, top). This suggested that oligosaccharides of the patient are smaller in size. In fact the main glycan peak of the control coeluted with a 2-AB-GlcNAc2Man3GlcNAc2Gal2Neu(N)Ac2 standard oligosaccharide (Figure 1, lower panel). The main oligosaccharide fraction from the patient coeluted with a 2-AB-GlcNAc2Man3GlcNAc2 standard (Figure 1, middle panel). Matrix-assisted laser desorption/ionization–time of flight (MALDI-TOF) analysis revealed for the major oligosaccharide from control transferrin a mass of 2344.4 Da, which corresponds to 2-AB-GlcNAc2Man3GlcNAc2Gal2Neu(N)Ac2, and for the major oligosaccharide from the patient’s transferrin a mass of 1438.2 Da. The loss of two sialic acid residues and two galactose residues accounts for the difference between 2344.4 and 1438.2 Da. The second oligosaccharide had a mass of 1892.2 Da, indicating the loss of one sialic acid residue and one galactose residue. The third oligosaccharide, coeluting with the 2-AB-GlcNAc2Man3GlcNAc2Gal2Neu(N)Ac2 standard had the expected mass of 2342.5 Da. This indicates that most of the N-linked oligosaccharides in transferrin have a complete or partial loss of galactose and neuraminic acid residues. However, a minor fraction of full-length N-linked oligosaccharides is also present.
Figure 1.
HPLC and mass spectrometric analysis of transferrin-linked oligosaccharides. Transferrin was purified from the serum of a control and the CDG-IId patient. Oligosaccharides were released by PNGase F digestion and subsequently analyzed by HPLC. The peak fractions were further investigated by mass spectrometry. The values over the HPLC peaks indicate the detected masses. Squares, N-acetylglucosamine; circles, mannose; hexagons, galactose; triangles, neuraminic acid.
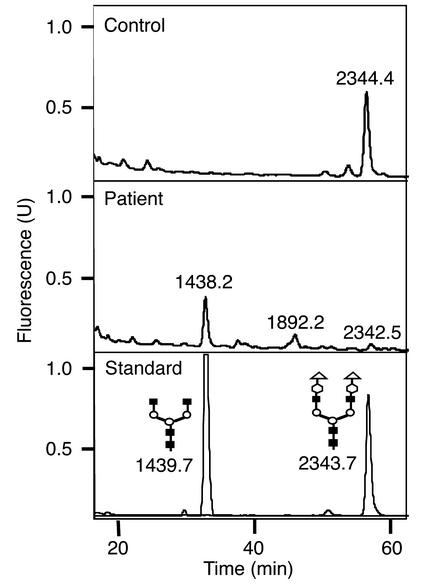
Deficiency of β-1,4–linked galactose residues in other serum glycoproteins was analyzed by lectin blotting. Following SDS-PAGE, proteins were either stained by Coomassie brilliant blue (Figure 2, left) or blotted onto nitrocellulose. To enhance binding of a β-1,4-galactose–specific lectin, nitrocellulose-bound glycoproteins were desialylated with sialidase from Arthrobacter ureafaciens. Subsequently, the nitrocellulose was incubated with biotinylated RCA-I and streptavidin-coupled horseradish peroxidase (Figure 2, right). RCA-I recognizes terminal galactose residues β-1,4–linked to N-acetylglucosamine (33). The lectin staining of the patient’s sample showed a reduced binding of RCA-I, indicating a reduction of terminal β-1,4-GlcNAc–linked galactose residues in serum glycoproteins.
Figure 2.
RCA-I lectin blot analysis of serum glycoproteins. Sixty micrograms of serum proteins from a control (Co) and the CDG-IId patient were separated by SDS-PAGE and subsequently either stained by Coomassie brilliant blue (left) or transferred to nitrocellulose by Western blotting. The nitrocellulose membrane was pretreated with neuraminidase from Arthrobacter ureafaciens. Terminal galactose residues were stained by biotinylated RCA-I lectin.
Deficiency of β4GalT I activity.
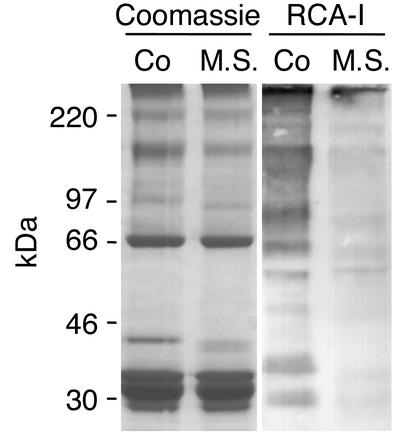
The analysis of the transferrin oligosaccharides as well as the RCA-I staining of serum glycoproteins indicated shortening of N-glycans due to a total or a partial loss of galactosylation. This could be due to a lack of the donor of galactose, UDP-galactose, as has been reported for galactosemia (34); to a decreased import of UDP-galactose into the Golgi apparatus; or to a defective transfer of galactose by galactosyltransferase. Galactosemia seemed unlikely as judged from the clinical phenotype as well as from the IEF pattern (35). Therefore we determined the import of UDP-galactose and the activity of β-galactosyltransferase I in control and patient-derived fibroblasts (Figure 3, upper panel). The import of UDP-[6-3H]galactose into Golgi-enriched vesicles from the patient’s fibroblasts was only slightly but repeatedly reduced compared with control fibroblasts, which might be explained by a secondary effect due to hypoglycosylation of the UDP-galactose transporter. For determination of β-1,4-galactosyltransferase activity, lysates from control and patient’s fibroblasts were incubated with UDP-[6-3H]galactose as the donor and ovalbumin as acceptor substrate. Activity of β-1,4-galactosyltransferase in the fibroblasts from the patient was reduced to 5% of control. Determination of β-1,4-galactosyltransferase activity in leukocyte lysates showed a residual activity of 9% in the patient and a residual activity of 58% and 52% in the father and the mother, respectively (Figure 3, lower panel). These results suggested a deficiency of β4GalT I, the major galactosyltransferase for β-1,4-galactosylation of N-linked oligosaccharides in glycoproteins (18), as cause for the galactosylation defect in the patient.
Figure 3.
Determination of UDP-[3H]galactose import and β4GalT I activity. The import of UDP-[3H]galactose was investigated in Golgi-enriched vesicle preparations from control and patient’s fibroblasts (upper panel, right lanes). β4GalT I activity was determined in lysates from control and patient’s fibroblasts (upper panel, left lanes) or leukocytes from control, the patient, and his parents (lower panel) with UDP-[3H]galactose as donor and ovalbumin as acceptor substrate. In all cases the mean and the SD of three independent experiments are given.
Identification of an insertion mutation in the β4GalT I gene.
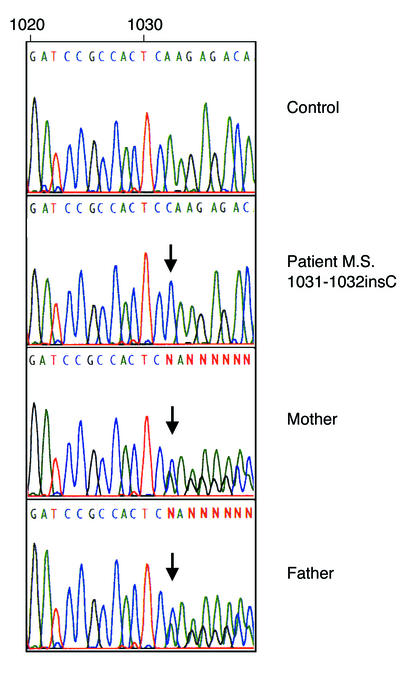
The human β4GalT I cDNA sequence (GenBank accession no. M22921) was used to generate primers for RT-PCR from total RNA prepared from control and CDG-IId patient’s fibroblasts. Sequencing of β4GalT I cDNA revealed the insertion of a single nucleotide (1031-1032insC) in the patient, compared with cDNAs of six control persons and the corrected sequence of β4GalT I cDNA (GenBank accession no. XM_036232). The 1031-1032insC mutation is predicted to cause premature translation stop with loss of the C-terminal 50 amino acids of β4GalT I. Sequencing of genomic DNA showed that the patient was homozygous for the 1031-1032insC mutation, whereas the parents were heterozygous (Figure 4).
Figure 4.
Identification of a 1031-1032insC mutation leading to premature translation stop and loss of the C-terminal 50 amino acids of the patient’s β4GalT I. Sequence alignment of the PCR-amplified genomic DNA fragment from a control, patient M.S. homozygous for the mutation, and heterozygous parents. Arrows indicate localization of the 1031-1032insC mutation.
1031-1032insC β4GalT I encodes a truncated, catalytically inactive polypeptide retained in the endoplasmic reticulum.
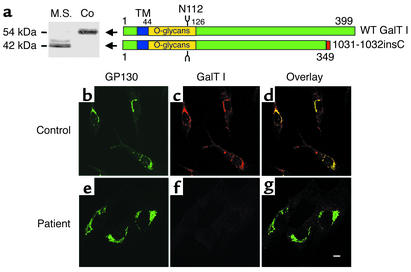
To determine whether the 1031-1032insC β4GalT I allele encodes a stable polypeptide, we performed a Western blot analysis of control and patient’s fibroblast extracts using an antiserum raised against soluble human milk β4GalT I (see Methods). The major form of β4GalT I in control fibroblasts has an apparent size of 54 kDa, which is comparable to that of β4GalT I in HeLa cells (36, 37). In the patient, a major form of a 42-kDa polypeptide accompanied by some minor 45- to 46-kDa forms was observed (Figure 5a). The loss of the C-terminal 50 amino acid residues is expected to account for a reduction of size by about 5 kDa. The additional reduction in size is ascribed to defective glycosylation (see above).
Figure 5.
Localization of the Golgi resident protein GP130 and the β4GalT I in control (Co) and patient’s (M.S.) fibroblasts. (a) Western blot analysis of the wild-type (WT) β4GalT I and the 1031-1032insC mutant (left). The bars represent wild-type and mutant β4GalT I. TM denotes the transmembrane domain. The region carrying the O-glycans (E.G. Berger, unpublished data) is indicated in yellow. N112 indicates the single N-glycosylation site of β4GalT I. In the case of the patient, the five new C-terminal residues caused by the frame shift in the 1031-1032insC mutant are indicated in red (right). (b–g) Immunofluorescence double labeling of fibroblasts for GP130 (green, b and e) or β4GalT I (red, c and f) and an overlay of both (d and g). Increasing the concentration of the β4GalT I antibody tenfold above the standard concentration failed to detect β4GalT I in the patient’s fibroblasts. Bar in g: 10 μm.
Intracellular localization of β4GalT I in fibroblasts was determined by indirect immunofluorescence (Figure 5, b–g). Control fibroblasts (Figure 5, b–d) showed a colocalization of β4GalT I with the Golgi marker GP130 (23). In patient-derived fibroblasts, GP130 was localized in the Golgi apparatus (Figure 5e) whereas no signal for β4GalT I was detectable (Figure 5, f and g). This shows that the polypeptide encoded by the 1031-1032insC allele fails to localize to the Golgi apparatus. The absence of a signal in indirect immunofluorescence even at antibody concentrations 30-fold higher than that giving a strong signal for wild-type β4GalT I in the Golgi apparatus of control cells appears to conflict with detection of a truncated β4GalT I by Western blot (Figure 5a), but it would be compatible with a retention and dilution of the truncated polypeptide in the ER (see Discussion).
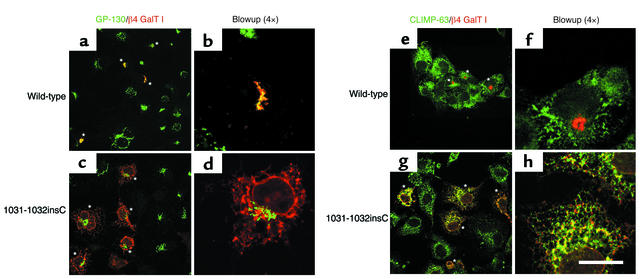
Further investigations of the properties of β4GalT I were carried out in COS-7 cells overexpressing wild-type or 1031-1032insC β4GalT I (Figure 6). Indirect immunofluorescence of COS-7 cells showed a normal Golgi staining for GP130, but no signal for β4GalT I, indicating that the antiserum against human β4GalT I does not cross-react with the endogenous β4GalT I of COS-7 cells. COS-7 cells expressing the human wild-type β4GalT I showed a colocalization of β4GalT I and GP130 in the Golgi apparatus (Figure 6, a and b). COS-7 cells expressing the 1031-1032insC β4GalT I showed a reticular staining pattern including the nuclear envelope suggestive of an ER localization of the mutant β4GalT I, while GP130 was localized in the Golgi apparatus (Figure 6, c and d). This was confirmed by colocalization of 1031-1032insC β4GalT I with CLIMP-63, an established ER-marker protein (24) (Figure 6, g and h).
Figure 6.
Localization of wild-type and 1031-1032insC β4GalT I overexpressed in COS-7 cells. The left panels show immunofluorescence double labeling for the Golgi resident protein GP130 (green in a–d) or the ER marker CLIMP-63 (green in e–h), and the expression of wild-type (red in a, b, e, and f) and mutant β4GalT I (red in c, d, g, and h). The right panels show one of the β4GalT-expressing cells at a fourfold higher magnification. The asterisks indicate COS-7 cells overexpressing β4GalT I. Bar: 20 μm.
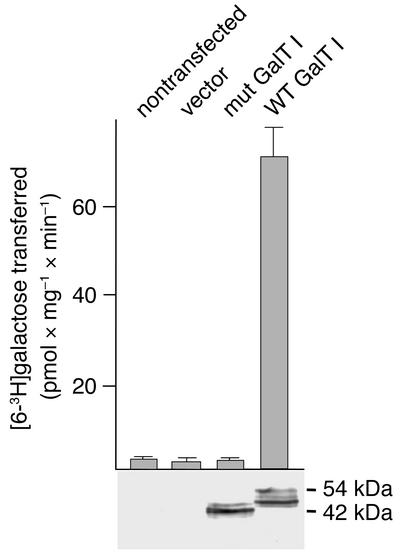
To determine the catalytic activity of the 1031-1032insC β4GalT I, lysates of nontransfected COS-7 cells and COS-7 cells transfected with the expression vector alone or containing the cDNA insert of wild-type or mutant β4GalT I were analyzed for galactosyltransferase activity. β4GalT I protein levels were determined by Western blot (Figure 7, bottom). An increase of galactosyltransferase activity above the basal level of COS-7 cells was detectable only in the COS-7 transfected with the wild-type β4GalT I cDNA (Figure 7, graph). The protein expression levels of COS-7 cells transfected with the wild-type or the 1031-1032insC β4GalT I cDNA were comparable. The size of 1031-1032insC β4GalT I forms was similar to that observed in patient-derived fibroblasts (Figure 5a). The wild-type β4GalT I polypeptide showed, in addition to the 54-kDa form, several smaller forms, which are supposed to represent incompletely glycosylated β4GalT I polypeptides.
Figure 7.
Galactosyltransferase activity in COS-7 cells overexpressing wild-type β4GalT I and the 1031-1032insC mutation. β4GalT I activity was determined in lysates of nontransfected COS-7 cells and of cells transfected with either the vector alone (vector) or vector containing the wild-type or the 1031-1032insC β4GalT I cDNA (mut). The graph shows the mean and the SD of four independent determinations. Below, the Western blot analysis of the lysates with a polyclonal β4GalT I antiserum is shown.
Galactosylation of glycoproteins is only slightly reduced in patient-derived fibroblasts.
In order to determine whether, in fibroblasts, the β4GalT I deficiency results in a hypoglycosylation of glycoproteins comparable to that of serum glycoproteins, fibroblasts were metabolically labeled with [2-3H]mannose. The cell lysates were digested with pronase. The 3H-glycopeptides were desialylated with neuraminidase from A. ureafaciens and passed over an RCA-I agarose column. Bound material was eluted with 0.1 mM, 1 mM, and 10 mM lactose (Figure 8). While of the 3H-glycopeptides from control fibroblasts 14% were eluted with 0.1 mM lactose and 10.6% with 1 mM lactose, 6.5% of the 3H-glycopeptides from the patient were eluted with 0.1 mM lactose and 7.3% with 1 mM lactose. The removal of terminal galactose residues by treatment with β-galactosidase from Streptococcus pneumoniae abolished the binding (data not shown), indicating that the binding to the RCA-I lectin depended on galactose residues. These data show a high residual galactosylation of glycoproteins synthesized in the fibroblasts of the patient. In line with this, lectin staining with RCA-I of cell lysates from control and patient’s fibroblasts separated by SDS-PAGE and blotted onto nitrocellulose was comparable (data not shown).
Discussion
The present study shows that deficiency of β4GalT I, the main enzyme responsible for the transfer of galactose residues from UDP-galactose onto terminal N-acetylglucosamine residues of complex-type oligosaccharides in newly synthesized glycoproteins in the Golgi apparatus, is the cause of a new type of CDG-II, designated CDG-IId. The β4GalT I deficiency results in brain malformation, mental retardation, myopathy, and blood clotting defects. Serum glycoproteins including transferrin lack the majority of galactose residues and the sialic acid residues linked to galactose. Galactosylation is not completely abolished, as shown for transferrin and total serum glycoproteins. Since no activity of the mutant β4GalT I was detectable in overexpressing COS-7 cells, we assume that the residual galactosylation of serum glycoproteins, the bulk of which originates from hepatocytes and plasma cells, and the residual galactosyltransferase activity that is detectable by the in vitro assay, are due to the activity of other galactosyltransferases. However, we cannot exclude a residual activity of the mutant β4GalT I.
The 1031-1032insC β4GalT I allele, for which the patient is homozygous, encodes a stable polypeptide. It is catalytically inactive, is C-terminally truncated, and is not transported to the Golgi apparatus but retained in the ER. The latter could be demonstrated directly in COS-7 cells overexpressing the 1031-1032insC β4GalT I. For the patients’ fibroblasts, evidence for retention in the ER is only indirect. It is suggested by the failure to detect an immunofluorescence signal in the Golgi apparatus or another compartment, although the protein level of the truncated β4GalT I polypeptide is comparable to that of β4GalT I in control fibroblasts. One of several tentative explanations is that β4GalT I polypeptides are concentrated in the Golgi apparatus, while retention in the ER may lower their concentration below the threshold critical for detection by immunofluorescence. Also in line with an accumulation in the ER is the apparent size of the truncated β4GalT I polypeptides, which was heterogenous and smaller than expected from the loss of the C-terminal 50 amino acids. Since β4GalT I carries a heterogenous group of O-glycans (38) and a single N-glycan side chain (39) in the luminal stem region (amino acids 44–126; E.G. Berger, unpublished data), the size reduction points to an incomplete O- and N-glycosylation due to retention in the ER.
Galactosylation of glycoproteins synthesized in the patient’s fibroblasts was almost normal. We ascribe this to the compensatory activity of other β-1,4-galactosyltransferases rather than to a residual activity of the truncated β4GalT I. The β-1,4-galactosyltransferase(s) substituting for the loss of β4GalT I in fibroblasts remains to be determined. It is interesting, however, to note that tissue-specific expression of galactosyltransferases can compensate for the loss of β4GalT I in some cell types, such as fibroblasts, but not in others, such as hepatocytes.
A possible animal model for this enzyme defect is β4GalT I knockout mice (27, 40). In these mice, glycoproteins from serum are severely hypogalactosylated, whereas glycoproteins from the salivary glands are fully galactosylated. The residual galactosyltransferase activity in various tissues was about 5%, as in the fibroblasts and leukocytes of our patient (27). The phenotype of the β4GalT I knockout mice presents with growth retardation, enhanced proliferation of the skin and the small intestine, and an abnormal differentiation of intestinal villi. Male and female β4GalT I–deficient mice were fertile, indicating that neither the enzyme nor galactosylated structures are essential for fertilization and embryonic development as has been proposed earlier (41). Furthermore, 50% of the mice die within 4 weeks after birth. At present it is difficult to assess to what extent β4GalT I deficiency in β4GalT I–null mice mimics the defects in humans. To date, only a single patient with β4GalT I deficiency is known, and only a few of the parameters that could be studied in mice have been analyzed in the patient. Interestingly, both in humans and mice a tissue-specific expression of the galactosylation defect was observed.
β4GalT I deficiency falls by definition into the group II CDGs (1). So far this group comprises three defects, that of N-acetylglucosaminyltransferase II in CDG-IIa (12), that of α-glucosidase I in CDG-IIb (14), and that of the GDP-fucose transporter in CDG-IIc/leukocyte adhesion deficiency II (15, 16). β4GalT I deficiency therefore defines CDG type IId. Previously it has been shown that mutations in a β-1,4-galactosyltransferase (β4GalT 7), which catalyzes the formation of Galβ1-4Xylβ-R in the linkage region of proteoglycans, can impair the synthesis of proteoglycans and cause a progeroidal disease with symptoms resembling the Ehlers-Danlos syndrome (42, 43). Disorders linked to mutations in the remaining β-1,4-galactosyltransferases β4GalT 2–6 (17) are so far unknown.
Acknowledgments
The mAb’s αGP130 and αCLIMP-63 were kindly provided by H.P. Hauri. This work was supported by the European Commission, contract no. QLG1-CT2000-00047 (Euroglycan); the Deutsche Forschungsgemeinschaft; the Graduiertenkolleg 60; the Fonds der Chemischen Industrie; and grant 31-61355.00 of the Schweizerischer Nationalfond to E.G. Berger.
Footnotes
Bengt Hanßke and Christian Thiel contributed equally to this work.
References
- 1.Aebi M, et al. Carbohydrate-deficient glycoprotein syndromes become congenital disorders of glycosylation: an updated nomenclature for CDG. Glycoconj J. 1999;10:669–671. doi: 10.1023/a:1017249723165. [DOI] [PubMed] [Google Scholar]
- 2.van Schaftingen E, Jaeken J. Phosphomannomutase deficiency is a cause of carbohydrate deficient glycoprotein syndrome type I. FEBS Lett. 1995;377:318–320. doi: 10.1016/0014-5793(95)01357-1. [DOI] [PubMed] [Google Scholar]
- 3.Matthijs G, et al. Mutations in PMM2, a phosphomannomutase gene on chromosome16p13, in carbohydrate-deficient glycoprotein type I syndrome (Jaeken syndrome) Nat Genet. 1997;16:88–92. doi: 10.1038/ng0597-88. [DOI] [PubMed] [Google Scholar]
- 4.Niehues R, et al. Carbohydrate deficient glycoprotein syndrome type Ib: phosphomannose isomerase deficiency and mannose therapy. J Clin Invest. 1998;101:1414–1420. doi: 10.1172/JCI2350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Körner C, et al. Carbohydrate deficient glycoprotein syndrome type V: deficiency of dolichyl-P-Glc:Man9GlcNAc2-PP-dolichyl glucosyltransferase. Proc Natl Acad Sci USA. 1998;95:13200–13205. doi: 10.1073/pnas.95.22.13200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Imbach T, et al. A mutation in the human ortholog of the Saccharomyces cerevisiaeALG6 gene causes carbohydrate-deficient glycoprotein syndrome type-Ic. Proc Natl Acad Sci USA. 1999;96:6982–6987. doi: 10.1073/pnas.96.12.6982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Körner C, et al. Carbohydrate deficient glycoprotein syndrome type IV: deficiency of dolichyl-P-Man:Man5GlcNAc2-PP-dolichyl mannosyltransferase. EMBO J. 1999;18:6818–6822. doi: 10.1093/emboj/18.23.6816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Imbach T, et al. Deficiency of dolichol-phosphate-mannose synthase-1 causes congenital disorder of glycosylation type Ie. J Clin Invest. 2000;105:233–239. doi: 10.1172/JCI8691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kim S, et al. Dolichol phosphate mannose synthase (DPM1) mutations define congenital disorder of glycosylation Ie (CDG-Ie) J Clin Invest. 2000;105:191–198. doi: 10.1172/JCI7302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Schenk B, et al. MPDU1mutations underlie a novel human congenital disorder of glycosylation, designated type If. J Clin Invest. 2001;108:1687–1695. DOI:10.1172/JCI200113419. doi: 10.1172/JCI13419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kranz C, et al. A mutation in the human MPDU1gene causes congenital disorder of glycosylation type If (CDG-If) J Clin Invest. 2001;108:1613–1619. DOI:10.1172/JCI200113635. doi: 10.1172/JCI13635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jaeken J, et al. Carbohydrate deficient glycoprotein syndrome type II: a deficiency in Golgi localised N-acetyl-glucosaminyltransferase II. Arch Dis Child. 1994;71:123–127. doi: 10.1136/adc.71.2.123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tan J, Dunn J, Jaeken J, Schachter H. Mutations in the MGAT2 gene controlling complex N-glycan synthesis cause carbohydrate-deficient glycoprotein syndrome type II, an autosomal recessive disease with defective brain development. Am J Hum Genet. 1996;59:810–817. [PMC free article] [PubMed] [Google Scholar]
- 14.de Praeter C, et al. A novel disorder caused by defective biosynthesis of N-linked oligosaccharides due to glucosidase I deficiency. Am J Hum Genet. 2000;66:1744–1756. doi: 10.1086/302948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lübke T, Marquardt T, Etzioni A, Hartmann E, von Figura K, Körner C. Complementation cloning identifies CDG-IIc (LAD II), a new type of congenital disorders of glycosylation, as a GDP-fucose transporter deficiency. Nat Genet. 2001;28:73–76. doi: 10.1038/ng0501-73. [DOI] [PubMed] [Google Scholar]
- 16.Lühn K, Wild M, Eckhardt M, Gerardy-Schahn R, Vestweber D. The defective gene in leukocyte adhesion deficiency II codes for a putative GDP-fucose transporter. Nat Genet. 2001;28:69–72. doi: 10.1038/ng0501-69. [DOI] [PubMed] [Google Scholar]
- 17.Amado M, Almeida R, Schwientek T, Clausen H. Identification and characterization of large galactosyltransferase gene families: galactosylation for all functions. Biochim Biophys Acta. 1999;1473:35–53. doi: 10.1016/s0304-4165(99)00168-3. [DOI] [PubMed] [Google Scholar]
- 18.Lee J, Sundaram S, Shaper N, Raju T, Stanley P. Chinese hamster ovary (CHO) cells may express six β4-galactosyltransferases (β4GalTs) J Biol Chem. 2001;276:13924–13934. doi: 10.1074/jbc.M010046200. [DOI] [PubMed] [Google Scholar]
- 19.Peters V, et al. Congenital disorder of glycosylation IId (CDG-IId) — A new entity: clinical presentation with Dandy-Walker malformation and myopathy. Neuropediatrics. 2002;33:1–6. doi: 10.1055/s-2002-23597. [DOI] [PubMed] [Google Scholar]
- 20.Stibler H, Jaeken J, Kristiansson B. Biochemical characteristics and diagnosis of the carbohydrate-deficient glycoprotein syndrome. Acta Paediatr Scand Suppl. 1991;375:21–31. [PubMed] [Google Scholar]
- 21.Watzele G, Bachofner R, Berger EG. Immunocytochemical localization of the Golgi apparatus using protein-specific antibodies to galactosyltransferase. Eur J Cell Biol. 1991;56:451–458. [PubMed] [Google Scholar]
- 22.Berger EG, Berger B, Hochli M, Dinter A. Colocalization of β-1,4galactosyltransferase with mannose 6-phosphate receptor in monensin-induced TGN-derived structures. Histochem Cell Biol. 2001;115:157–168. doi: 10.1007/s004180000231. [DOI] [PubMed] [Google Scholar]
- 23.Linstedt A, Mehta A, Suhan J, Reggio H, Hauri H-P. Sequence and overexpression of GPP130/GIMPc: evidence for saturable pH-sensitive targeting of a type II early Golgi membrane protein. Mol Biol Cell. 1997;8:1073–1087. doi: 10.1091/mbc.8.6.1073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Klopfenstein D, et al. Subdomain-specific localisation of CLIMP-63 (p63) in the endoplasmic reticulum is mediated by its luminal α-helical segment. J Cell Biol. 2001;153:1287–1299. doi: 10.1083/jcb.153.6.1287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Iourin O, et al. The identification of abnormal glycoforms of serum transferrin in carbohydrate deficient glycoprotein syndrome type I by capillary zone electrophoresis. Glycoconj J. 1996;13:1031–1042. doi: 10.1007/BF01053199. [DOI] [PubMed] [Google Scholar]
- 26.Bigge JC, et al. Nonselective and efficient fluorescent labeling of glycans using 2-amino benzamide and anthranilic acid. Anal Biochem. 1995;230:229–238. doi: 10.1006/abio.1995.1468. [DOI] [PubMed] [Google Scholar]
- 27.Asano M, et al. Growth retardation and early death of β-1,4-galactosyltransferase knockout mice with augmented proliferation and abnormal differentiation of epithelial cells. EMBO J. 1997;16:1850–1857. doi: 10.1093/emboj/16.8.1850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lübke T, Marquardt T, von Figura K, Körner C. A new type of carbohydrate deficient glycoprotein syndrome due to a decreased import of GDP-fucose into the Golgi. J Biol Chem. 1999;274:25986–25989. doi: 10.1074/jbc.274.37.25986. [DOI] [PubMed] [Google Scholar]
- 29.Sambrook, J., Fritsch, E.F., and Maniatis, T. 1989. Molecular cloning: a laboratory manual. 2nd edition. Cold Spring Harbor Laboratory Press. Cold Spring Harbor, New York, USA. 14–19.
- 30.Lowry O, Rosebrough N, Farr A, Randall R. Protein determination by a modified Folin-phenol method. J Biol Chem. 1951;193:265–275. [PubMed] [Google Scholar]
- 31.Cummings, R.D. 1994. Glycobiology: a practical approach. M. Fukuda and A. Kobata, editors. IRL Press. Oxford, United Kingdom. 262–263.
- 32.Yamashita K, et al. Sugar chains of serum transferrin from patients with carbohydrate deficient glycoprotein syndrome. J Biol Chem. 1993;268:5783–5789. [PubMed] [Google Scholar]
- 33.Baenzinger JU, Fiete D. Structure of the complex oligosaccharides of fetuin. J Biol Chem. 1979;254:9795–9804. [PubMed] [Google Scholar]
- 34.Petry K, Reichhardt J. The fundamental importance of human galactose metabolism: lessons from genetics and biochemistry. Trends Genet. 1998;14:98–102. doi: 10.1016/s0168-9525(97)01379-6. [DOI] [PubMed] [Google Scholar]
- 35.Charlwood J, Clayton P, Keir G, Mian N, Winchester B. Defective galactosylation of serum transferrin in galactosemia. Glycobiology. 1998;8:351–357. doi: 10.1093/glycob/8.4.351. [DOI] [PubMed] [Google Scholar]
- 36.Berger EG, Mandel T, Schilt U. Immunohistochemical localization of galactosyltransferase in human fibroblasts and HeLa cells. J Histochem Cytochem. 1981;29:364–370. doi: 10.1177/29.3.6787115. [DOI] [PubMed] [Google Scholar]
- 37.Strouss G, Berger EG. Biosynthesis, intracellular transport and release of the Golgi enzyme galactosyltransferase (lactose synthase A protein) in HeLa cells. J Biol Chem. 1982;257:7623–7628. [PubMed] [Google Scholar]
- 38.Amano J, et al. Structures of mucin-type sugar chains of the galactosyltransferase purified from human milk. J Biol Chem. 1991;266:11461–11477. [PubMed] [Google Scholar]
- 39.Endo T, Amano J, Berger EG, Kobata A. Structure identification of the complex type, asparagine-linked sugar chains of D-galactosyltransferase purified from human milk. Carbohydr Res. 1986;150:241–264. doi: 10.1016/0008-6215(86)80020-9. [DOI] [PubMed] [Google Scholar]
- 40.Lu Q, Hasty P, Shur BD. Targeted mutation in β1,4-galactosyltransferase leads to pituitary insufficiency and neonatal lethality. Dev Biol. 1997;181:257–267. doi: 10.1006/dbio.1996.8444. [DOI] [PubMed] [Google Scholar]
- 41.Shur BD, Evans S, Lu QX. Cell surface galactosyltransferase: current issues. Glycoconj J. 1998;15:537–548. doi: 10.1023/a:1006951407168. [DOI] [PubMed] [Google Scholar]
- 42.Quentin E, Gladen A, Roden L, Kresse H. A genetic defect in the biosynthesis of dermatan sulfate proteoglycan: galactosyltransferase I deficiency in fibroblasts from a patient with a progeroid syndrome. Proc Natl Acad Sci USA. 1990;87:1342–1346. doi: 10.1073/pnas.87.4.1342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Almeida R, et al. Cloning and expression of a proteoglycan UDP-galactose:β-xylose β1,4-galactosyltransferase I. J Biol Chem. 1999;274:26165–26171. doi: 10.1074/jbc.274.37.26165. [DOI] [PubMed] [Google Scholar]