Abstract
We used mice deficient in each of the eight types and subtypes of prostanoid receptors and examined the roles of prostanoids in dextran sodium sulfate–induced (DSS-induced) colitis. Among the prostanoid receptor–deficient mice, only EP4-deficient mice and not mice deficient in either DP, EP1, EP2, EP3, FP, IP, or TP developed severe colitis with 3% DSS treatment, which induced only marginal colitis in wild-type mice. This phenotype was mimicked in wild-type mice by administration of an EP4-selective antagonist (AE3-208). The EP4 deficiency impaired mucosal barrier function and induced epithelial loss, crypt damage, and aggregation of neutrophils and lymphocytes in the colon. Conversely, administration of an EP4-selective agonist (AE1-734) to wild-type mice ameliorated severe colitis normally induced with 7% DSS, while that of AE3-208 suppressed recovery from colitis and induced significant proliferation of CD4+ T cells. In vitro AE3-208 enhanced and AE1-734 suppressed the proliferation and Th1 cytokine production of lamina propria mononuclear cells from the colon. DNA microarray analysis revealed elevated expression of genes associated with immune response and reduced expression of genes with mucosal repair and remodeling in the colon of EP4-deficient mice. We conclude that EP4 maintains intestinal homeostasis by keeping mucosal integrity and downregulating immune response.
Introduction
Human inflammatory bowel disease (IBD), including Crohn disease and ulcerative colitis, is a chronic, relapsing, and remitting condition of unknown origin that exhibits various features of immunological inflammation and affects at least 1 in 1,000 people in Western countries (1–3). IBD is characterized by inflammation in the large and/or small intestine associated with diarrhea, hemoccult, abdominal pain, weight loss, anemia, and leukocytosis (1, 2). Studies in humans have implicated impaired mucosal barrier function, pronounced innate immunity, production of proinflammatory and immunoregulatory cytokines, and the activation of CD4+ T cells in the pathogenesis of IBD (1, 2). One of the major risk factors triggering and worsening the disease is the administration of nonsteroidal anti-inflammatory drugs (NSAIDs) (4–6). Because NSAIDs share inhibition of the enzyme cyclooxygenase (COX) as a common mechanism, it is believed that the COX inhibition has adverse effects on IBD. Consistently, genetic disruption of either of the two isoforms of COX, COX-1, or COX-2, in mice exacerbated the extent of colitis in an experimental model (7). COX catalyzes production of prostanoids including prostaglandin D2 (PGD2), PGE2, PGF2α, PGI2, and thromboxane (TX), which act on the respective receptors, the PGD receptor (DP), the PGE receptor (EP), the PGF receptor (FP), the PGI receptor (IP), and the TX receptor (TP) to exert their actions (8, 9). EP has four subtypes, EP1, EP2, EP3, and EP4, which are encoded by different genes. The adverse effect of NSAIDs on IBD, therefore, indicates that during the course of IBD some prostanoids are formed and negatively modulate the extension of the disease. Indeed, in human IBD, a dramatic increase in prostanoid synthesis is found in the intestine and correlates with the disease activity (10–12). However, little is known about how prostanoids modulate IBD and which prostanoid and receptor are responsible for such modulation.
Here we have used dextran sodium sulfate–induced (DSS-induced) colitis as a model of IBD (13) and subjected mice deficient in each type or subtype of prostanoid receptor individually to this treatment. DSS causes acute colitis by damaging epithelial cells and, thereby, stimulating regional inflammation through production of cytokines and other inflammatory mediators (13). The aim of this study is to identify the responsible prostanoid and its receptor in the modulation of IBD and to determine the roles they play in this process.
Methods
Animals.
Mice lacking the EP1, EP2, EP3, EP4, DP, FP, IP, and TP receptors individually (EP1–/–, EP2–/–, EP3–/–, EP4–/–, DP–/–, FP–/–, IP–/–, and TP–/– mice, respectively) were generated as described (14–20). With the exception of EP4–/– and FP–/– mice, each mutant was backcrossed ten times to C57BL/6CrSlc (Japan SLC, Shizuoka, Japan), and females of the F2 progenies of N10 mice were used with C57BL/6 female mice as their control. Most EP4–/– mice die postnatally as a result of patent ductus arteriosus and do not survive at all in the C57BL/6 background (16, 21). Therefore, survivors of the F2 progenies of EP4–/– mice in the mixed genetic background of 129/Ola and C57BL/6 were intercrossed, and the resulting female survivors were used. For FP+/+ and FP–/– mice, the progeny of F2 littermates with a 129/Ola × C57BL/6 mixed background was used. Mice were maintained on a 12-hour light/dark cycle under specific pathogen-free (SPF) conditions. All experimental procedures were approved by the Committee on Animal Research of Kyoto University Faculty of Medicine.
Induction of colitis.
DSS of the average molecular weight of 5,000 (Sigma Chemical Co., St. Louis, Missouri, USA) was administered to 8-week-old mice for 7 days at either 3% (low dose) or 7% (high dose) concentration in the drinking water. The addition of DSS or any drugs mentioned below to the drinking water did not affect water consumption of mice. Indomethacin also was added to the drinking water at a dose of 4 mg/kg/day and administered to the animals during the entire experimental period. This dose of indomethacin was reported to inhibit PGE2 production in rats and mice in vivo (22, 23). An EP4 antagonist, ONO-AE3-208, 4-{4-Cyano-2-[2-(4-fluoronaphthalen-1-yl) propionylamino] phenyl} butyric acid (AE3-208), and an EP4 agonist, ONO-AE1-734, methyl-7-[(1R, 2R, 3R)-3-hydroxy-2-[(E)-(3S)-3-hydroxy-4-(m-methoxymethylphenyl)-1-butenyl]-5-oxocyclopenthl]-5-thiaheptanoate (AE1-734), were kindly provided by Ono Pharmaceutical Co., Osaka, Japan. The Ki values of AE3-208 obtained by competition-binding isotherms to displace the radioligand binding to the respective prostanoid receptor are 1.3, 30, 790, 2,400 nM for EP4, EP3, FP, and TP, respectively, and more than 10,000 nM for the other prostanoid receptors. The Ki values of AE1-734 are 0.7, 56, and 620 nM for EP4, EP3, and EP2, respectively, and more than 10,000 nM for the rest of the prostanoid receptors. AE3-208 was administered (10 mg/kg/day) orally in the drinking water. When this compound was administered orally at 10 mg/kg as a bolus, a peak plasma concentration of 677 ng/ml was attained in 0.25 hours after the administration with 18% of bioavailability. The plasma half-life of this compound measured in an experiment of intravenous injection was 0.2 hours. AE1-734 was administered subcutaneously twice a day (0.1 mg/kg/each) from 1 day before the DSS treatment until the end of experiment. When AE1-734 was injected subcutaneously at this dose, the peak plasma concentration of 100 ng/ml was attained at 10 minutes after the injection with more than 70% for bioavailability. The plasma concentration declined with a half-life of 30 minutes.
To assess the extent of colitis, body weight, stool consistency, and occult blood in the stool were monitored daily (24). Diarrhea was scored as follows: 0, normal; 2, loose stools; 4, watery diarrhea. Hemoccult was scored as follows: 0, normal; 2, hemoccult positive; 4, gross bleeding. On the last day of the experiments, blood was collected from the animals by intracardiac puncture. The colon was removed for histological examination, and the spleen was weighed. Hematocrit (HCT) and the white blood cell (WBC) number were determined using a blood cell counter (Sysmex K4500; Sysmex Co., Long Grove, Illinois, USA).
To evaluate mucosal integrity, the FITC-dextran assay was used (25). Wild-type C57BL/6 mice were administered with either AE3-208 or vehicle in the drinking water. After 1 day, both groups of mice were fed with 3% DSS in the drinking water in the continued presence or absence of AE3-208, and 24 hours later, 200 μl of FITC-dextran (average molecular weight, 4,400; Sigma Chemical Co.) (2 mg/ml in saline) was administered orally. Serum concentration was determined 4 hours after the administration of FITC-dextran. EP4–/– mice and their wild-type control mice were similarly treated with 3% DSS and administered with FITC-dextran. The colon was snap-frozen and cryostat sections of 10-μm thickness were used for fluorescent microscopic analysis.
Histology.
The colon was divided into the proximal, middle, and distal portions and was fixed in Bouin’s fixative. Sections 5 μm thick were prepared and subjected to staining with hematoxylin and eosin (H&E). The histological examination was performed in a blinded fashion by two coauthors and scored as described (24). Two independent parameters were measured: the extent of inflammation (0, none; 1, slight; 2, moderate; 3, severe) and the extent of crypt damage (0, none; 1, the basal one-third portion damaged; 2, the basal two-thirds portion damaged; 3, the entire crypt damaged but the surface epithelium intact; 4, the entire crypt and epithelium lost). Each score was multiplied by a factor reflecting the percentage of involvement (1: 0–25%; 2: 26–50%; 3: 51–75%; 4: 76–100%) and added. The histological injury score was the sum of the scores obtained in three sections, each taken from the proximal, middle, and distal portions of the colon. The maximal score is 84.
To label S-phase cells, mice were injected intraperitoneally with 120 mg/kg of 5-bromo-2′-deoxyuridine (BrdU) and 12 mg/kg of fluorodeoxyuridine 120 minutes before sacrifice. The colon was excised and fixed as described above. Sections were incubated with a rat anti-BrdU mAb (BU1/75; Oxford Biotechnology, Oxford, United Kingdom), and staining was performed with a Ventana Basic DAB Detection Kit using the Ventana HX system (Ventana, Tucson, Arizona, USA) according to the manufacturer’s protocol. For immunohistochemistry, the colon was snap-frozen in liquid nitrogen and 10-μm thick cryostat sections were transferred on slides and air dried. After fixation for 10 minutes in pure acetone, samples were incubated with either a rat anti-mouse CD4 mAb (RM4-5; PharMingen, San Diego, California, USA), a rat anti-mouse CD8 mAb (53-6.7; PharMingen), a rat anti-mouse B220 mAb (RA3-6B2; PharMingen), or a rabbit anti-mouse IFN-γ polyclonal Ab (PBL Biomedical Laboratories, New Brunswick, New Jersey, USA), and staining was performed with a Ventana Basic DAB Detection Kit.
Isolation and culture of lamina propria mononuclear cells.
Lamina propria mononuclear cells (LPMNCs) were prepared from the colon as described (26). In brief, the colon was digested with collagenase type IV (0.5 mg/ml; Sigma Chemical Co.) in RPMI-1640 medium at 37°C, and the resulting suspension was filtered. The cells were pooled, washed, and layered on the top of discontinuous 40% and 70% Percoll gradient (Amersham Pharmacia Biotech AB, Uppsala, Sweden). After centrifugation for 20 minutes at 600 g, the cells at the interface were collected as LPMNCs.
The isolated LPMNCs were cultured in RPMI-1640 medium with 10% FBS at 37°C in a volume of 200 μl per well in 96-well round-bottom plates at a density of 106 cells/ml. In the proliferation assay, 0.5 μCi of [3H] thymidine was added at 24 hours, and the cells were collected at 72 hours on a cell harvester (Skatron Instruments AS, Lier, Norway). Incorporation of [3H] thymidine was determined using a liquid scintillation counter (Aloka Co., Tokyo, Japan). For measurement of IFN-γ and IL-2, the LPMNCs were incubated with either vehicle, LPS (10 μg/ml) alone, or LPS and concanavalin A (ConA) (2 μg/ml) in combination for 72 hours. The cytokine amounts in the culture supernatants were measured with an ELISA kit (Endogen Inc., Woburn, Massachusetts, USA) as described (26). All experiments were performed in triplicate.
DNA microarray analysis.
The colon was isolated from EP4+/+ and EP4–/– mice treated with or without 3% DSS for 7 days. Polyadenylated RNA was prepared as described (17) and used for the Affymetrix GeneChip Expression Analysis using a MG-U74Av2 chip (Affymetrix Inc., Santa Clara, California, USA) according to the manufacturer’s protocol. Data were analyzed with the Affymetrix GENECHIP Expression Analysis software (version 4.0).
Statistics.
Data are presented as the means plus or minus SEM. Data were analyzed using an unpaired two-tailed t test or one-way ANOVA followed by Dunnett or Tukey multiple comparisons. An associated probability (P value) of less than 0.05 was considered significant.
Results
Exacerbation of colitis by indomethacin in mice treated with low-dose (3%) DSS.
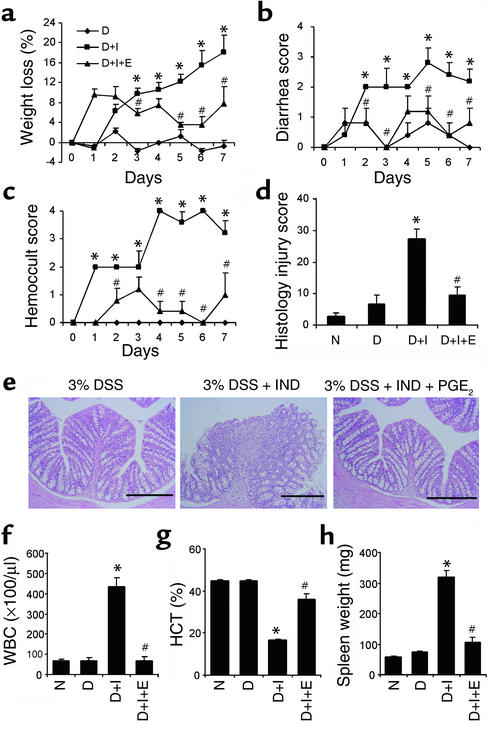
Administration of NSAIDs, the inhibitor of prostanoid synthesis, often triggers or worsens IBD in humans and is regarded as one of the major risk factors of IBD. To confirm the adverse effect of NSAIDs in mice, we added indomethacin to mice treated with low-dose (3%) DSS. Low-dose DSS-treatment of control C57BL/6 mice for 7 days evoked only marginal alterations in stool consistency and slight loss of the body weight, and there was no significant change in the diarrhea and hemoccult scores. Similarly, administration of indomethacin alone in the drinking water (4 mg/kg per day) did not cause significant body weight loss, diarrhea, or hemoccult in the stool (data not shown). When the mice were treated with indomethacin and 3% DSS in combination, however, they gradually lost weight, and their body weight loss was significant compared with the mice treated with 3% DSS alone on day 3 and thereafter (Figure 1a). The mice treated with indomethacin and 3% DSS also showed gradual onset of diarrhea, and the diarrhea score significantly increased compared with the mice treated with 3% DSS alone after day 2 (Figure 1b). Furthermore, the mice treated with indomethacin and 3% DSS developed acute onset of bloody stool. This symptom worsened gradually and, on day 4 and thereafter, most of mice in this group showed gross bleeding, while all of the mice treated with 3% DSS alone did not show hemoccult in the stool at all (Figure 1c). The macroscopic examination of the intestine revealed hemorrhagic redness of the whole large intestine in mice treated with indomethacin and 3% DSS (data not shown). In some cases, the distal portion of the ileum showed redness, while the stomach and jejunum always appeared intact. Upon histological examination, crypt damage, ulceration, and infiltration of inflammatory cells, including neutrophils and lymphocytes, were reproducibly observed in the colon of mice treated with indomethacin and 3% DSS (Figure 1e). The histological injury score was significantly increased in mice treated with indomethacin and 3% DSS when compared with the mice treated with 3% DSS alone (Figure 1d). Treatment with indomethacin and 3% DSS provoked significant leukocytosis and anemia when compared with treatment with 3% DSS alone (Figure 1, f and g). Moreover, splenomegaly was found in mice treated with indomethacin and 3% DSS in combination (Figure 1h). Flow cytometric analysis revealed that most of the splenocytes from mice treated with indomethacin and 3% DSS were TER119-positive cells (data not shown), indicating that extramedullary hematopoiesis occurred in the spleen to compensate for severe anemia.
Figure 1.
Induction of colitis by indomethacin in mice treated with 3% DSS and suppression of this effect by dm-PGE2. (a–c) Wild-type C57BL/6 mice were treated with either 3% DSS alone (diamonds), 3% DSS and indomethacin (squares), or 3% DSS, indomethacin, and dm-PGE2 (triangles), and monitored for body weight loss (a), diarrhea (b), and hemoccult (c) for 7 days. (d and e) On day 7, the mice were sacrificed. The colon was dissected for histological analysis with H&E staining (e), and the histological injury scores were obtained (d). Blood was collected for measurement of the WBC number (f) and HCT (g). The weights of spleens of the sacrificed animals are shown (h). N, mice treated with vehicle; D, mice treated with 3% DSS alone; D+I, mice treated with 3% DSS and indomethacin; D+I+E, mice treated with 3% DSS, indomethacin, and dm-PGE2. Data in a–d and f–h are means ± SEM from six animals. *P < 0.05 versus D (Dunnett). #P < 0.05 versus D+I (Dunnett multiple comparison test). Scale bars, 200 μm in e.
Suppression by exogenous PGE2 of the indomethacin-induced exacerbation of low-dose (3%) DSS-induced colitis.
Indomethacin inhibited the production of prostanoids by inhibition of both COX-1 and COX-2. Because it was reported that the level of PGE2 was elevated locally in the intestine of IBD patients (10, 11), we wondered whether the exacerbation by indomethacin was due to the inhibition of PGE2 production. To address this point, we administered intraperitoneally a stable PGE2 analogue, dimethyl-PGE2 (dm-PGE2) to the mice treated with indomethacin and 3% DSS. Dm-PGE2 significantly suppressed the weight loss in mice treated with indomethacin and 3% DSS in combination alone (Figure 1a). Dm-PGE2 also prevented clinical symptoms, such as diarrhea and hemoccult, induced by indomethacin and 3% DSS. The diarrhea score was significantly improved on days 2, 3, 5, 6, and 7 (Figure 1b). The hemoccult score was also improved (Figure 1c). Moreover, dm-PGE2 ameliorated the histological findings of the colon induced by the treatment with indomethacin and 3% DSS. There was no epithelial cell loss, crypt damage, or inflammatory cell aggregation in the colon from mice administered with dm-PGE2 (Figure 1e). Consequently, dm-PGE2 significantly suppressed the histological injury score, when compared with the mice treated with indomethacin and 3% DSS (Figure 1d). Hematological evaluation showed that the treatment with dm-PGE2 corrected leukocytosis and anemia found with the treatment with indomethacin and 3% DSS in combination alone (Figure 1, f and g) and resolved the splenomegaly found in the mice treated with indomethacin and 3% DSS in combination alone (Figure 1h). These results suggest that the exacerbation of DSS-induced colitis by indomethacin was mostly, if not solely, due to the inhibition of endogenous PGE2 production.
Induction of severe colitis by 3% DSS in EP4-deficient mice but not in mice deficient in other prostanoid receptors.
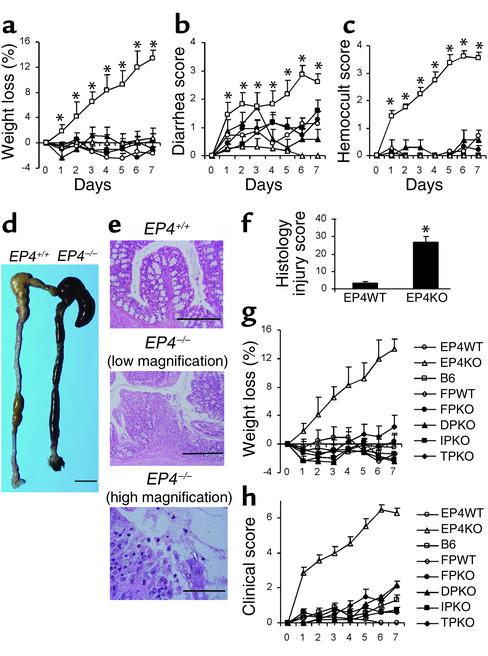
PGE2 elicits its physiological effects by acting on four different subtypes of EP receptors (9). Previously, we generated mice deficient in each EP subtype individually (14–16). To clarify which subtype of the EP receptor mediates the protective action of PGE2 in DSS-induced colitis, we subjected EP1–/–, EP2–/–, EP3–/–, and EP4–/– mice to 3% DSS treatment. C57BL/6 mice were used as controls for EP1–/–, EP2–/–, and EP3–/– mice, and the progeny of wild-type littermates (EP4+/+) in the mixed background of C57BL/6 and 129/Ola were used as controls for EP4–/– mice. These mice neither developed gastrointestinal inflammation spontaneously nor exhibited any clinical manifestations, such as diarrhea, fecal occult blood, or anemia, when they were raised under SPF conditions. When these animals were treated with 3% DSS, only EP4–/– mice developed severe bloody diarrhea and body weight loss, while the body weight loss, diarrhea, and hemoccult of EP1–/–, EP2–/–, and EP3–/– mice were similar to those of control C57BL/6 mice. EP4–/– mice treated with 3% DSS lost their weight progressively during the entire experimental period and significantly as compared with control EP4+/+ mice (Figure 2a). The diarrhea score of EP4–/– mice was significantly high compared with EP4+/+ mice (Figure 2b). These mice showed loose stool already on day 1, and some of them exhibited watery diarrhea after day 6. EP4–/– mice also showed hemoccult already on day 1, and most of them exhibited gross bleeding in the stool after day 6, yielding significantly higher hemoccult scores than the EP4+/+ mice throughout the experimental period (Figure 2c). The macroscopic finding of the intestine of EP4–/– mice treated with 3% DSS and sacrificed on day 7 showed edema and hemorrhagic redness all through the colon and cecum (Figure 2d). These mice also showed splenomegaly (data not shown). While the histological examination of the colon obtained from EP4+/+ mice treated with 3% DSS appeared normal, the histological results from EP4–/– mice treated with 3% DSS showed epithelial loss, crypt damage, partial ulceration, and infiltration of inflammatory cells (Figure 2e, upper and middle). The inflammatory cells included neutrophils, lymphocytes, and eosinophils as found at high magnification (Figure 2e, lower). Consistently, the histological injury score obtained from six EP4–/– mice was significantly higher than that from six control mice (Figure 2f). The time course of weight loss, the character of bloody diarrhea, and histological findings obtained from EP4–/– mice treated with 3% DSS were similar to those obtained from C57BL/6 mice treated with 3% DSS and indomethacin in combination. These findings suggest that the indomethacin-induced exacerbation of colitis was mostly, if not solely, due to its inhibition of the PGE2-EP4 signaling. To confirm this point further and to assess the contribution of prostanoids other than PGE2, we subjected mice deficient in either DP, FP, IP, or TP to the 3% DSS-induced colitis model. As shown in Figure 2, g and h, none of the DP–/–, IP–/–, FP–/–, and TP–/– mice developed body weight loss, diarrhea, or bloody stool to an extent similar to that found in EP4–/– mice. These results suggest that contribution of other prostanoids is, if present, much limited.
Figure 2.
Induction of severe colitis by 3% DSS in EP4-deficient mice and not in mice deficient in other prostanoid receptors. (a–c) Wild-type C57BL/6 (filled circles), EP1–/– (filled triangles), EP2–/– (filled squares), EP3–/– (open circles), EP4+/+ (open triangles), and EP4–/– (open squares) mice were treated with 3% DSS for 7 days and monitored for body weight loss (a), diarrhea (b), and hemoccult (c). The numbers of mice used in this experiment were 25 (C57BL/6), 7 (EP1–/–), 10 (EP2–/–), 14 (EP3–/–), 16 (EP4–/–), and 12 (EP4+/+). (d–f) On day 7, EP4+/+ and EP4–/– mice treated with 3% DSS were sacrificed. The macroscopic examination of the large intestine is shown (d). The colon was dissected for histological analysis with H&E staining (e), and the histological injury scores were obtained (f). (g and h) Body weight loss (g) and clinical scores (h) of mice deficient in DP, FP, IP, and TP in 3% DSS colitis. DP–/–, FP+/+, FP–/–, IP–/–, and TP–/– mice were treated with 3% DSS for 7 days and monitored for body weight, diarrhea, and hemoccult. The body weight loss and clinical scores (diarrhea score plus hemoccult score) of these mice are compared with those of EP4+/+, EP4–/–, and C57BL/6 wild-type mice. The numbers of mice used in this experiment were 12 (EP4+/+), 16 (EP4–/–), 18 (C57BL/6), 11 (DP–/–), 5 (FP+/+), 4 (FP–/–), 8 (IP–/–), and 5 (TP–/–). Data in a–c and f–h are means ± SEM. *P < 0.05 versus EP4+/+ (t test) in a–c. Scale bars, 1 cm in d; 200 μm in upper and middle panel of e; 40 μm in lower panel of e.
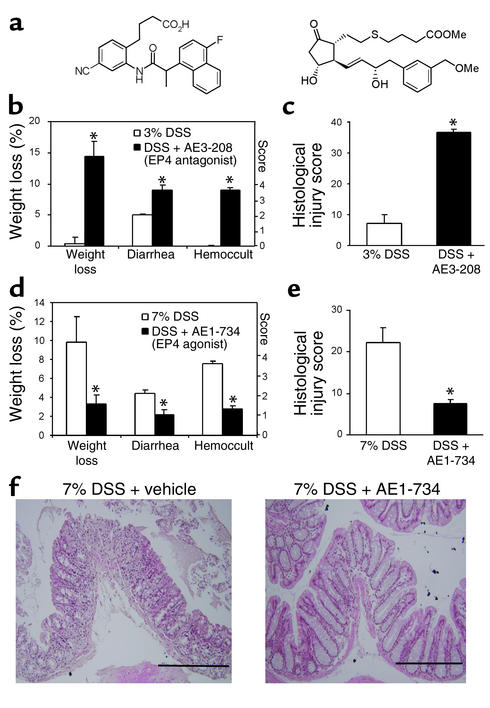
Reproduction of the EP4–/– phenotype in wild-type mice by administration of the EP4 antagonist.
To confirm that the above phenotype of EP4–/– mice is due to the lack of EP4 receptor, we used an EP4-selective antagonist, AE3-208 (Figure 3a, left). AE3-208 was added to 3% DSS in the drinking water and administered to C57BL/6 mice for 7 days. The mice treated with the EP4 antagonist and 3% DSS together showed severe weight loss and bloody diarrhea. Significant differences in the weight loss and the diarrhea and hemoccult scores were found between these mice and mice treated with 3% DSS alone (Figure 3b). Consistently, the histological injury score of mice treated with the EP4 antagonist and 3% DSS in combination was also significantly high compared with those treated with 3% DSS alone (Figure 3c). To verify the specificity of AE3-208 in vivo, we applied this compound to EP4–/– mice together with 3% DSS. AE3-208 did not exacerbate the colitis further in EP4–/– mice; the body weight loss of 10.2% ± 4.2% and 8.7% ± 3.2%, the diarrhea score of 1.3 ± 0.3 and 1.8 ± 0.3, and the hemoccult score of 3.3 ± 0.5 and 3.3 ± 0.5 were observed on day 7 in EP4–/– mice treated with AE3-208 and untreated EP4–/– mice, respectively (n = 5, each).
Figure 3.
Effect of EP4-selective drugs on DSS-induced colitis. (a) Structures of ONO-AE3-208 (left) and ONO-AE1-734 (right). (b and c) Reproduction of the EP4–/– phenotype in wild-type mice by administration of an EP4 antagonist. AE3-208, an EP4 antagonist, was added to 3% DSS in the drinking water and administered to C57BL/6 mice for 7 days. Body weight loss, diarrhea, and hemoccult scores on day 7 of 3% DSS-treated mice administered with vehicle (open bars) or AE3-208 (closed bars) is shown in b, and histological injury scores of the colon are shown in c. (d–f) Amelioration of high-dose (7%) DSS-induced colitis by an EP4 agonist. High-dose (7%) DSS was administered to C57BL/6 mice together with vehicle or AE1-734, an EP4 agonist, for 7 days. Body weight loss, diarrhea, and hemoccult scores on day 7 of 7% DSS-treated mice with vehicle (open bars) or the EP4 agonist (closed bars) are shown in d, and H&E staining of the colon (f) and the histological injury scores (e) are shown. Data are means ± SEM from five to ten mice. *P < 0.05 versus mice treated with 3% or 7% DSS alone (t test). Scale bars, 200 μm in f.
Amelioration of high-dose (7%) DSS-induced colitis by an EP4 agonist.
Because the above study showed that the EP4 antagonist exacerbated low-dose DSS-induced colitis, we wondered whether an EP4 agonist ameliorates severe colitis. To examine this issue, we used the colitis induced by high-dose DSS as a model. Administration of high-dose (7%) DSS in the drinking water to wild-type mice induced fulminant colitis characterized by the bloody diarrhea and loss of body weight; the body weight loss, diarrhea score, and hemoccult score on day 7 were 9.8% ± 2.7%, 2.2 ± 0.1, and 3.8 ± 0.2, respectively (Figure 3d). Upon histological examination, epithelial loss, goblet cell loss, and aggregation of inflammatory cells were observed in the mice treated with 7% DSS (Figure 3f). When we administered an EP4 agonist, AE1-734 (Figure 3a, right), subcutaneously twice a day to 7% DSS-treated mice, we found that the EP4 agonist significantly suppressed the weight loss and bloody diarrhea induced by 7% DSS treatment in C57BL/6 mice. The body weight loss, diarrhea score, and hemoccult score on day 7 were 3.3% ± 1.0% versus 9.8% ± 2.7%, 1.1 ± 0.3 versus 2.2 ± 0.1, and 1.4 ± 0.4 versus 3.8 ± 0.2, respectively (Figure 3d). Upon histological examination, there were neither loss of epithelial and goblet cells nor aggregation of inflammatory cells in the colon of the mice treated with the EP4 agonist in addition to 7% DSS (Figure 3f). Consistently, the EP4 agonist lowered the histological injury score to 7.5 ± 1.1 from 22.3 ± 3.5 found in mice treated with 7% DSS alone (Figure 3e). This preventive action of AE1-734 was most likely due to stimulation of the EP4 receptor, because administration of this compound to EP4–/– mice treated with 7% DSS did not ameliorate any symptoms of the colitis throughout the experi-mental period. The body weight loss, the diarrhea score, and the hemoccult score on day 7 were 23.4% ± 1.4% and 22.0% ± 2.2%, 4.0 ± 0.0 and 4.0 ± 0.0, and 4.0 ± 0.0 and 4.0 ± 0.0 for EP4–/– mice treated with AE1-734 and untreated EP4–/– mice, respectively (n = 5, each).
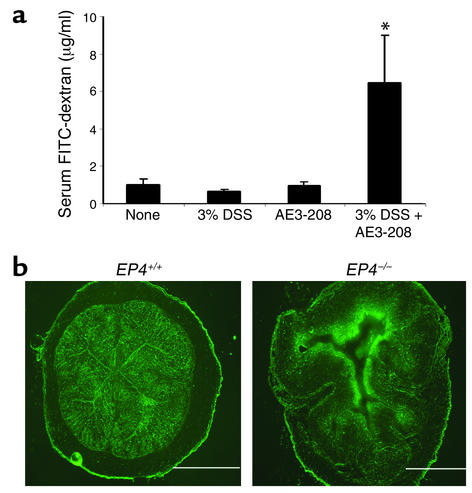
Impaired mucosal integrity in mice with the EP4 deficiency.
The above studies taken together have suggested that the PGE2-EP4 signaling plays a critical role in protection of DSS-induced colitis. To obtain a mechanistic insight into the protective action of the PGE2-EP4 signaling, we first used FITC-dextran assay and evaluated the mucosal barrier function in the induction phase of colitis. The EP4 antagonist (AE3-208) was administered in the drinking water (10 mg/kg/day) to C57BL/6 mice 1 day before and throughout the treatment of 3% DSS. Twenty-four hours after DSS treatment, FITC-dextran was given orally, and 4 hours later blood was drawn. The serum level of FITC-dextran in the mice treated with the EP4 antagonist and DSS was significantly higher than that in nontreated mice, while that in mice treated with 3% DSS alone or AE1-734 alone was not significantly higher than that in nontreated mice (Figure 4a). We also administered FITC-dextran orally to EP4+/+ and EP4–/– mice treated with 3% DSS for 1 day. Four hours after FITC-dextran administration we excised the colon for fluorescent microscopic examination. The colon from EP4–/– mice treated with 3% DSS showed significant infiltration of FITC-dextran into submucosa, while no infiltration was found in that from EP4+/+ mice (Figure 4b).
Figure 4.
Impaired mucosal integrity caused by the EP4-deficiency. (a) Effect of the EP4 antagonist. C57BL/6 mice were treated with either vehicle (None), 3% DSS alone, AE3-208 (EP4 antagonist) alone, or 3% DSS and AE3-208 in combination for 1 day. FITC-dextran was administered by mouth, and the serum level was measured 4 hours later. Data are means ± SEM from six mice per group. *P < 0.05 versus the vehicle-treated mice (t test). (b) DSS-induced submucosal infiltration of FITC-dextran in EP4-deficient mice. FITC-dextran was administered by mouth to EP4+/+ and EP4–/– mice pretreated with 3% DSS for 1 day. Four hours later the colon was excised and subjected to fluorescent microscopic examination. Scale bars, 1 mm.
Impaired epithelial regeneration and enhanced CD4+ T cell activation in mice treated with an EP4 antagonist during the recovery period after high-dose DSS-induced colitis.
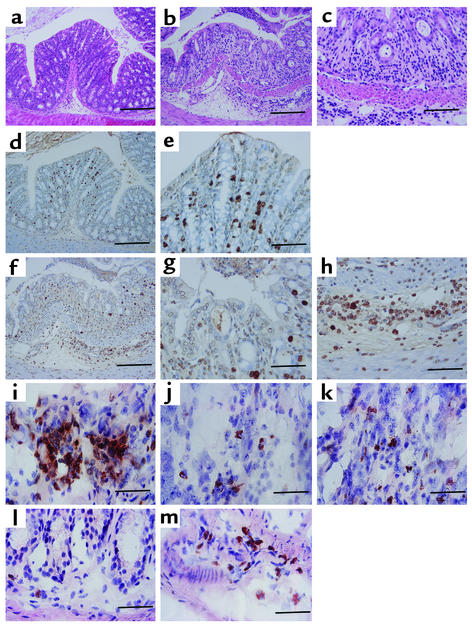
The results above revealed that the PGE2-EP4 signaling is important in the maintenance of the mucosal barrier in induction of colitis. This impairment of the mucosal barrier would lead to the exposure of submucosa to luminal antigens. We next examined whether EP4 plays a role in prevention of the disease progression and/or in repair of epithelial damage. Since EP4 was reported to be expressed on epithelial cells in the large intestine (27), we hypothesized that the intestinal epithelial growth after injury was modulated by the PGE2-EP4 signaling. To clarify this point, we used the BrdU incorporation assay. After high-dose (7%) DSS treatment for 7 days, mice were treated with or without the EP4 antagonist (AE3-208) in the absence of DSS treatment for 3 days and sacrificed. BrdU was added intraperitoneally 2 hours before sacrifice. While the vehicle-treated mice quickly recovered from the weight loss and bloody diarrhea, the EP4 antagonist–treated mice continued to exhibit severe colitis (data not shown). The histological results from the H&E-stained colon from the vehicle-treated mice appeared normal, while those from the EP4 antagonist–treated mice showed that epithelial and crypt loss remained as that seen in the colon from mice treated with 7% DSS for 7 days (Figure 5, a and b). Moreover, in the mice treated with the EP4 antagonist, infiltration of inflammatory cells, including lymphocytes and neutrophils in submucosa, became more pronounced (Figure 5c). As for BrdU staining, a number of positive cells were found in the crypt epithelium of the colon from the vehicle-treated mice, suggesting that repair from epithelial damage was occurring (Figure 5, d and e). On the other hand, in mice treated with the EP4 antagonist after DSS treatment, BrdU-positive epithelial cells were barely detected, indicating that the PGE2-EP4 signal blockade suppressed epithelial regeneration (Figure 5, f and g). On the other hand, there existed a large number of BrdU-positive mononuclear cells in the submucosal area of the EP4 antagonist–treated mice (Figure 5, f and h). Immunohistochemistry showed that CD4+ T cells comprised the majority of these inflammatory cells (Figure 5i). This pronounced infiltration of CD4+ T cells was not seen in the colons from mice treated with 7% DSS for 7 days (data not shown). CD8- or B220-positive cells were also seen, but they did not make clusters as did CD4+ cells but were scattered all over the lamina propria (Figure 5, j and k). Neutrophils and macrophages were also detected (data not shown). Most of the infiltrated cells were also stained positive with anti–IFN-γ Ab, while IFN-γ–positive cells were found only occasionally in the submucosa from the vehicle-treated mice (Figure 5, l and m). These results suggest that the activation of T cells occurred upon prolonged PGE2-EP4 signal blockade.
Figure 5.
Impaired epithelial proliferation and enhanced CD4+ T cell proliferation in mice treated with an EP4 antagonist. Mice pretreated with 7% DSS for 7 days were then administered with either vehicle (a, d, e, and l) or the EP4 antagonist (AE3-208) (b, c, f–k, and m) for 3 days without DSS and sacrificed. BrdU was added intraperitoneally 2 hours before sacrifice. The colon was dissected for histological examination with H&E staining (a–c) and immunohistochemical analysis for BrdU (d–h), CD4 (i), CD8 (j), B220 (k), and IFN-γ (l and m). (e and g) Enlarged figures of d and f, respectively, showing the epithelial area; (h) an enlarged figure of f showing the submucosal area. (i–m) The submucosal area. Scale bars, 200 μm in a, b, d, f; 100 μm in c, e, g, h; 40 μm in i–m.
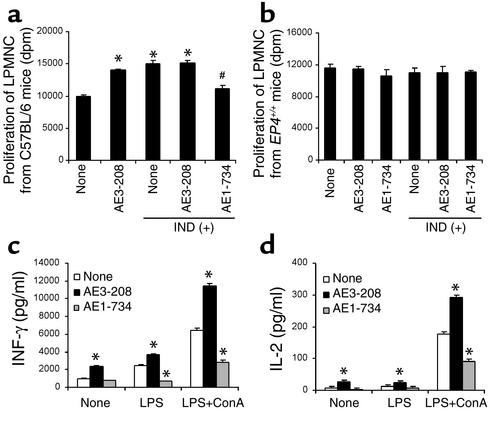
Downregulation of LPMNC proliferation and Th1 cytokine production by the PGE2-EP4 signaling.
The results above showed that the enhanced proliferation of CD4+ T cells in the lamina propria occurred with prolonged inhibition of the EP4 signaling in colitis. EP4 was reported to be present on CD4+ T cells in the submucosa of the large intestine (27). These findings taken together suggest that EP4 activation may downregulate the proliferation of CD4+ T cells to modulate immunological response in the lamina propria. To examine this issue, we isolated LPMNCs from C57BL/6 mice and examined the effect of the EP4 agonist and antagonist on their proliferative response by measuring [3H] thymidine incorporation. LPMNCs treated with the EP4 antagonist (AE3-208) or indomethacin exerted a significant increase in the proliferative response compared with those treated with vehicle (Figure 6a). There was no additive effect of the EP4 antagonist and indomethacin in combination compared with the EP4 antagonist alone or indomethacin alone. The addition of the EP4 agonist suppressed the increase in the proliferative response by indomethacin (Figure 6a), while it did not suppress the proliferation of LPMNCs without indomethacin treatment (data not shown). Control experiments using LPMNCs from EP4–/– mice showed that the EP4 agonist and antagonist, as well as indomethacin, did not affect the proliferative response (Figure 6b). These results suggest that stimulation of the proliferative response of wild-type LPMNCs by the EP4 antagonist or indomethacin was due to the inhibition of the action of endogenous PGE2 on the EP4 receptor of these cells. This experiment thus clearly corroborates the immunosuppressive action of EP4 on LPMNCs and suggests that the enhanced proliferation of CD4+ T cells seen in the colitis of the animals treated with the EP4 antagonist AE3-208 was caused by prolonged inhibition of the EP4 signaling in T cells. We next examined the effect of the EP4 signaling on cytokine production. We either incubated LPMNCs for 72 hours without stimulation or stimulated them for 72 hours with LPS or LPS and ConA in combination and examined the effects of the EP4 agonist or antagonist on the levels of Th1 cytokines produced under these conditions. In all cases, the levels of IFN-γ significantly increased with the treatment of the EP4 antagonist and decreased with the EP4 agonist (AE1-734) treatment (Figure 6c). Similarly, the levels of IL-2 in the culture medium significantly increased with the EP4 antagonist treatment and decreased with the EP4 agonist treatment (Figure 6d). These results suggest that the PGE2-EP4 signaling regulates the proliferation and Th1 cytokine production of LPMNCs.
Figure 6.
Modulation of the LPMNC proliferation and Th1 cytokine production by EP4 signaling. (a and b) LPMNCs were prepared from C57BL/6 mice (a) or from EP4–/– mice (b), cultured with either vehicle (None), the EP4 antagonist (AE3-208), the EP4 agonist (AE1-734), or indomethacin (IND) either alone or in indicated combination, and examined for the proliferation by measuring [3H] thymidine uptake. Data are means ± SEM (n = 3). *P < 0.05 versus None (Tukey multiple comparison test). #P < 0.05 versus IND (Tukey multiple comparison test). (c and d) LPMNCs were stimulated for 72 hours with vehicle, LPS, or LPS and ConA in combination in the presence of vehicle (None), the EP4 antagonist (AE3-208), or the EP4 agonist (AE1-734), and the levels of IFN-γ (c) and IL-2 (d) in the culture medium were measured with an ELISA kit. Data are means ± SEM (n = 3). *P < 0.05 versus None (Dunnett multiple comparison test).
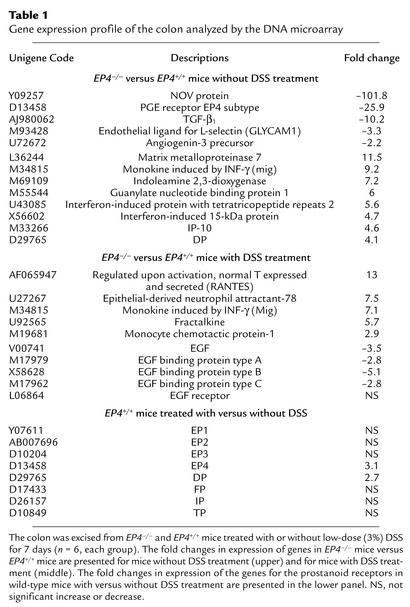
Elevated expression of genes associated with immune response and reduced expression of genes with mucosal repair and remodeling in the colon of EP4-deficient mice.
To evaluate the functions of the EP4 signaling in more detail at the molecular level, we employed the DNA microarray analysis and compared the gene expression profiles of the colon between EP4–/– mice and EP4+/+ mice treated either with vehicle or low-dose (3%) DSS for 7 days. We tested about 10,000 genetic loci as identified UNIGENE clusters. After exclusion of expressed sequence tags (ESTs), we detected 30 genes that showed more than twofold increase and 53 genes that showed more than twofold decrease of expression in the vehicle-treated EP4–/– mice as compared with the vehicle-treated EP4+/+ mice. Representative genes are shown in the upper panel of Table 1. Gene expression profiles revealed that EP4–/– mice had reduced expression of genes involved in tissue defense, remodeling, and immunosuppression, such as NOV protein, angiogenin-3 precursor, intelectin, and TGF-β, and had increased expression of genes involved in tissue destruction, such as matrix metalloproteinase, and genes induced by IFN-γ, such as mig, guanylate nucleotide–binding protein, and indoleamine 2,3-dioxygenase. These results suggest that although EP4–/– mice appeared normal, both clinically and histologically without overt insults, they already have signs of intestinal injury or infection. To explore the possibility that other prostanoid receptors may be upregulated in compensation for the EP4 absence, we also examined expression of other prostanoid receptor genes. Among the seven other receptors, only the DP receptor showed a significant increase in expression (Table 1, upper panel). We next compared the gene expression profiles of the colon from EP4–/– and EP4+/+ mice treated with 3% DSS. After exclusion of ESTs, we detected 388 genes that showed more than threefold increase and 79 genes that showed more than threefold decrease of expression in EP4–/– mice as compared with EP4+/+ mice. Since the histological results of 3% DSS-treated EP4–/– mice showed epithelial loss and inflammatory cell aggregation, we focused on genes related to epithelial repair and chemokine families. EP4–/– mice treated with 3% DSS showed decreased expression of genes of epidermal growth factor (EGF) and EGF-binding proteins and increased expression of genes of chemokine families, such as ENA78, fractalkine, MCP-1, and RANTES (Table 1, the middle panel). Moreover, we examined whether the DSS treatment affected expression of genes of the prostanoid receptors and found that the expression of the gene for EP4 as well as that for DP significantly increased with DSS treatment in wild-type mice (Table 1, the lower panel).
Table 1.
Gene expression profile of the colon analyzed by the DNA microarray
Discussion
In the present study we have analyzed the roles and functions of prostanoids in modulation of IBD using DSS-induced colitis as a model. Two doses of DSS have been used, low-dose (3%) DSS to evaluate the susceptibility of experimental animals to IBD and high-dose (7%) DSS to evaluate the protective effect of exogenously applied prostanoids and to analyze the functions of endogenous prostanoids in the recovery phase after fulminant colitis. First, we found that indomethacin exacerbated the marginal colitis induced by the low-dose DSS and that this exacerbation was almost completely counteracted by exogenous administration of PGE2. PGE2 was reported previously to attenuate other forms of experimental colitis in rats (28, 29). Our study has, therefore, not only confirmed this effect in DSS-induced colitis in mice, but also has strongly suggested that endogenous PGE2 is the mediator of mucosal protection. We then compared the susceptibilities of mice deficient in each of the prostanoid receptors to low-dose DSS. Disruption of the EP4 gene alone caused severe colitis under this condition, but disruption of none of the other receptor genes alone caused significant change. These results thus strongly indicate that the PGE2-EP4 system is the major PG system to prevent mucosal intestinal inflammation caused by DSS, although we do not exclude the contribution by the other prostanoids and receptors under different conditions. The role of the PGE2-EP4 has then been confirmed by the use of the EP4-selective agonists and antagonist. The DNA microarray analysis revealed that EP4–/– mice, even without DSS treatment, have reduced expression of genes in-volved in tissue defense, remodeling, and immunosuppression, and increased expression of genes induced by IFN-γ and that the expression of the EP4 gene is significantly induced in association with DSS treatment. The latter finding is consistent with the previous finding that the expression of the EP4 gene in the colon was elevated during inflammation in patients with ulcerative colitis (27). These results taken together suggest that the PGE2-EP4 signaling plays a protective role in the colon even under physiological conditions and that once the epithelium is exposed to intestinal injury, this system is amplified by upregulation of the EP4 receptor. The expression level of EP4 therefore might also influence the susceptibility to IBD in humans. The microarray analysis also revealed that the expression of the DP gene increased in the colon of EP4–/– mice and was induced in that of wild-type mice treated with DSS, suggesting that DP might have some role in intestinal inflammation. Our previous study on allergic asthma (17) showed that DP is induced upon allergen challenge in the airway epithelial cells of sensitized mice and mediates allergic inflammation of the lung. Whether DP in the colon also works in a proinflammatory pathway or antagonizes inflammation with EP4 remains to be examined.
How then does the PGE2-EP4 signaling attenuate intestinal inflammation? Studies in humans have implicated the impaired mucosal barrier function, pronounced innate immunity, altered production of Th1 and Th2 cytokines, and the activation of CD4+ T cells in the pathogenesis of IBD (1, 2). To examine the function of EP4 in the mucosal barrier integrity, we have used two assays, i.e., the FITC-dextran infiltration assay and the BrdU-incorporation assay. COX-1, COX-2, and EP4 are known to be present in the intestinal epithelium (27, 30, 31). The FITC-dextran assay has revealed that the mucosal integrity is impaired without the EP4 signaling in the induction phase of colitis, suggesting that the PGE2-EP4 signaling is important in the maintenance of the mucosal barrier against the injurious stimulus of DSS. The BrdU-incorporation assay has revealed that the inhibition of EP4 signaling suppresses epithelial regeneration after epithelial damage. This result is consistent with the previous finding that exogenous PGE2 promoted epithelial proliferation after mucosal injury (30). Consistently, the DNA microarray analysis revealed that colons from EP4–/– mice treated with DSS showed decreased gene expression of EGF families. Taken together, these studies have revealed that the PGE2–EP4 signaling serves to keep mucosal integrity and suggest that one mechanism to promote the epithelial regeneration by EP4 is the production of the EGF family proteins.
Once the mucosal barrier is impaired, the submucosa is exposed to various luminal antigens, including foods and bacteria, and the cells involved in innate immunity are activated. How much then does the PGE2-EP4 signaling affect innate immunity? Both COX-1 and COX-2 are reported to be present in LPMNCs (30–34), and, when mice are treated with DSS, PGE2 is produced in a COX-2–dependent manner (7). Newberry et al. (32, 33) reported that lamina propria stroma cells in the small intestine produce PGE2 spontaneously and continuously at a high level not seen in other immune organs and it was suggested that PGE2 thus produced induces oral tolerance to specific antigen in the small intestine (35). It has also been reported repeatedly that prostanoids, particularly, PGE2 and PGI2, modulate function of cells in innate immunity. For example, PGE2 downregulates the production and release of proinflammatory cytokines such as TNF-α by macrophages and neutrophils in vitro (36, 37). In the present study, we have found that neutrophils and mononuclear cells accumulated in the absence of the EP4 signaling in the colon of mice treated with low DSS for 7 days. The DNA microarray analysis has revealed that the colon of EP4–/– mice subjected to such treatment showed increased expression of genes of chemokine families (38). These findings support the idea that the PGE2 produced in the submucosa works to suppress innate immune response to luminal antigen through the EP4 signaling.
Using DSS-induced colitis, we have further investigated the roles of the PGE2-EP4 signaling in the protracting phase of IBD. DSS-induced colitis is originally viewed as a T cell–independent model because it occurs even in T cell–deficient SCID mice (39, 40). However, this view is based on the findings of the disease initiation and does not take into a consideration the prolongation mechanisms of the disease that involves cellular immune response. Indeed, it was reported recently that DSS treatment induces both Th1 and Th2 cytokines as well as other inflammatory mediators (41). We have found that when we suppressed the EP4 signaling by administration of the EP4 antagonist after 7% DSS treatment, the recovery from the colitis was severely affected and the disease became prolonged. Under these conditions, pronounced accumulation of BrdU-positive mononuclear cells was noted in the submucosa of the colon. The majority of these cells were CD4+ T cells, and most of them were also stained positive with anti–IFN-γ Ab. These results indicate that CD4+ T cells are activated by inhibition of the EP4 signaling in the recovery phase from severe colitis. Our in vitro experiments have demonstrated that activation of the EP4 signaling induces suppression of proliferation and Th1 cytokine production of isolated LPMNCs (Figure 6). These results suggest that the enhanced activation of CD4+ T cells in vivo as discussed above are due to direct inhibition of their PGE2-EP4 signaling. Our study thus suggests the possibility that once the PGE2-EP4 signaling is blocked, unrestrained activation of CD4+ T cells is induced. Unrestrained activation of CD4+ T cells (42) and an excessive production of IFN-γ produced by Th1 cells (43, 44) have been suggested as the factors in protraction of IBD.
In summary, we have clarified the roles of the PGE2-EP4 signaling in maintenance of intestinal homeostasis. EP4 works to keep mucosal integrity, to suppress the innate immunity, and to downregulate the proliferation and activation of CD4+ T cells. These findings have not only elucidated the mechanism of exacerbation of IBD by NSAIDs, but also indicated the therapeutic potential of EP4-selectve agonists in prevention and treatment of IBD.
Acknowledgments
We are grateful to T. Dohi of the International Medical Center of Japan; S. Fukuyama, M-N. Kweon, and H. Kiyono of Osaka University for helpful discussions; S. Kitajima of Saga Medical School for advice on the FITC-dextran assay; C Hamada of Kyoto University for advice on statistical analysis; K. Deguchi for animal care and breeding; and T. Arai for secretarial assistance. This work was supported in part by a Grant-in-Aid for Scientific Research from the Ministry of Education, Science, Sports and Culture of Japan and by a grant from the Organization for Pharmaceutical Safety and Research.
References
- 1.Fiocchi C. Inflammatory bowel disease: etiology and pathogenesis. Gastroenterology. 1998;115:182–205. doi: 10.1016/s0016-5085(98)70381-6. [DOI] [PubMed] [Google Scholar]
- 2.Blumberg RS, Saubermann LJ, Strober W. Animal models of mucosal inflammation and their relation to human inflammatory bowel disease. Curr Opin Immunol. 1999;11:648–656. doi: 10.1016/s0952-7915(99)00032-1. [DOI] [PubMed] [Google Scholar]
- 3.Logan RF. Inflammatory bowel disease incidence: up, down or unchanged? Gut. 1998;42:309–311. doi: 10.1136/gut.42.3.309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bjarnason I, Hayllar J, MacPherson AJ, Russell AS. Side effects of nonsteroidal anti-inflammatory drugs on the small and large intestine in humans. Gastroenterology. 1993;104:1832–1847. doi: 10.1016/0016-5085(93)90667-2. [DOI] [PubMed] [Google Scholar]
- 5.Kaufmann HJ, Taubin HL. Nonsteroidal anti-inflammatory drugs activate quiescent inflammatory bowel disease. Ann Intern Med. 1987;107:513–516. doi: 10.7326/0003-4819-107-4-513. [DOI] [PubMed] [Google Scholar]
- 6.Felder JB, et al. Effects of nonsteroidal anti-inflammatory drugs on inflammatory bowel disease: a case-control study. Am J Gastroenterol. 2000;95:1949–1954. doi: 10.1111/j.1572-0241.2000.02262.x. [DOI] [PubMed] [Google Scholar]
- 7.Morteau O, et al. Impaired mucosal defense to acute colonic injury in mice lacking cyclooxygenase-1 or cyclooxygenase-2. J Clin Invest. 2000;105:469–478. doi: 10.1172/JCI6899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Krause W, DuBois RN. Eicosanoids and the large intestine. Prostaglandins Other Lipid Mediat. 2000;61:145–161. doi: 10.1016/s0090-6980(00)00069-1. [DOI] [PubMed] [Google Scholar]
- 9.Narumiya S, Sugimoto Y, Ushikubi F. Prostanoid receptors: structures, properties, and functions. Physiol Rev. 1999;79:1193–1226. doi: 10.1152/physrev.1999.79.4.1193. [DOI] [PubMed] [Google Scholar]
- 10.Sharon P, Ligumsky M, Rachmilewitz D, Zor U. Role of prostaglandins in ulcerative colitis. Enhanced production during active disease and inhibition by sulfasalazine. Gastroenterology. 1978;75:638–640. [PubMed] [Google Scholar]
- 11.Wiercinska-Drapalo A, Flisiak R, Prokopowicz D. Effects of ulcerative colitis activity on plasma and mucosal prostaglandin E2concentration. Prostaglandins Other Lipid Mediat. 1999;58:159–165. doi: 10.1016/s0090-6980(99)00032-5. [DOI] [PubMed] [Google Scholar]
- 12.Carty E, De Brabander M, Feakins RM, Rampton DS. Measurement of in vivo rectal mucosal cytokine and eicosanoid production in ulcerative colitis using filter paper. Gut. 2000;46:487–492. doi: 10.1136/gut.46.4.487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Elson CO, Sartor RB, Tennyson GS, Riddell RH. Experimental models of inflammatory bowel disease. Gastroenterology. 1995;109:1344–1367. doi: 10.1016/0016-5085(95)90599-5. [DOI] [PubMed] [Google Scholar]
- 14.Ushikubi F, et al. Impaired febrile response in mice lacking the prostaglandin E receptor subtype 3. Nature. 1998;395:281–284. doi: 10.1038/26233. [DOI] [PubMed] [Google Scholar]
- 15.Hizaki H, et al. Abortive expansion of the cumulus and impaired fertility in mice lacking the prostaglandin E receptor subtype EP2. Proc Natl Acad Sci USA. 1999;96:10501–10506. doi: 10.1073/pnas.96.18.10501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Segi E, et al. Patent ductus arteriosus and neonatal death in prostaglandin receptor EP4-deficient mice. Biochem Biophys Res Commun. 1998;246:7–12. doi: 10.1006/bbrc.1998.8461. [DOI] [PubMed] [Google Scholar]
- 17.Matsuoka T, et al. Prostaglandin D2as a mediator of allergic asthma. Science. 2000;287:2013–2017. doi: 10.1126/science.287.5460.2013. [DOI] [PubMed] [Google Scholar]
- 18.Sugimoto Y, et al. Failure of parturition in mice lacking the prostaglandin F receptor. Science. 1997;277:681–683. doi: 10.1126/science.277.5326.681. [DOI] [PubMed] [Google Scholar]
- 19.Murata T, et al. Altered pain perception and inflammatory response in mice lacking prostacyclin receptor. Nature. 1997;388:678–682. doi: 10.1038/41780. [DOI] [PubMed] [Google Scholar]
- 20.Okada Y, et al. Characterization of prostanoid receptors mediating contraction of the gastric fundus and ileum: studies using mice deficient in prostanoid receptors. Br J Pharmacol. 2000;131:745–755. doi: 10.1038/sj.bjp.0703627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Nguyen M, et al. The prostaglandin receptor EP4 triggers remodelling of the cardiovascular system at birth. Nature. 1997;390:78–81. doi: 10.1038/36342. [DOI] [PubMed] [Google Scholar]
- 22.Masferrer JL, et al. Selective inhibition of inducible cyclooxygenase 2 in vivo is anti-inflammatory and nonulcerogenic. Proc Natl Acad Sci USA. 1994;91:3228–3232. doi: 10.1073/pnas.91.8.3228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cohn SM, Schloemann S, Tessner T, Seibert K, Stenson WF. Crypt stem cell survival in the mouse intestinal epithelium is regulated by prostaglandins synthesized through cyclooxygenase-1. J Clin Invest. 1997;99:1327–1379. doi: 10.1172/JCI119296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cooper HS, Murthy SNS, Shah RS, Sedergran DJ. Clinicopathologic study of dextran sulfate sodium experimental murine colitis. Lab Invest. 1993;69:238–249. [PubMed] [Google Scholar]
- 25.Westrom BR, Svendsen J, Ohlsson BG, Tagesson C, Karlsson BW. Intestinal transmission of macromolecules (BSA and FITC-labelled dextrans) in the neonatal pig. Influence of age of piglet and molecular weight of markers. Biol Neonate. 1984;46:20–26. doi: 10.1159/000242028. [DOI] [PubMed] [Google Scholar]
- 26.Kweon MN, Yamamoto M, Kajiki M, Takahashi I, Kiyono H. Systemically derived large intestinal CD4+ Th2 cells play a central role in STAT6-mediated allergic diarrhea. J Clin Invest. 2000;106:199–206. doi: 10.1172/JCI8490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cosme R, Lublin D, Takafuji V, Lynch K, Roche JK. Prostanoids in human colonic mucosa: effects of inflammation on PGE2receptor expression. Hum Immunol. 2000;61:684–696. doi: 10.1016/s0198-8859(00)00131-2. [DOI] [PubMed] [Google Scholar]
- 28.Fedorak RN, Empey LR, MacArthur C, Jewell LD. Misoprostol provides a colonic mucosal protective effect during acetic acid-induced colitis in rats. Gastroenterology. 1990;98:615–625. doi: 10.1016/0016-5085(90)90280-e. [DOI] [PubMed] [Google Scholar]
- 29.Allgayer H, Deschryver K, Stenson WF. Treatment with 16,16′-deimethyl PGE2before and after induction of colitis with trinitrobenzene sulfonic acid in rats decreases inflammation. Gastroenterology. 1989;96:1290–1300. doi: 10.1016/s0016-5085(89)80016-2. [DOI] [PubMed] [Google Scholar]
- 30.Tessner T, Cohn S, Schloemann S, Stenson WF. Prostaglandins prevent decreased the epithelial proliferation associated with dextran sodium sulfate injury in mice. Gastroenterology. 1998;115:874–882. doi: 10.1016/s0016-5085(98)70259-8. [DOI] [PubMed] [Google Scholar]
- 31.Singer II, et al. Cyclooxygenase 2 is induced in colonic epithelial cells in inflammatory bowel disease. Gastroenterology. 1998;115:297–306. doi: 10.1016/s0016-5085(98)70196-9. [DOI] [PubMed] [Google Scholar]
- 32.Newberry RD, Stenson WF, Lorenz RG. Cyclooxygenase-2-dependent arachidonic acid metabolites are essential modulators of the intestinal immune response to dietary antigen. Nat Med. 1999;5:900–906. doi: 10.1038/11341. [DOI] [PubMed] [Google Scholar]
- 33.Newberry RD, McDonough JS, Stenson WF, Lorenz RG. Spontaneous and continuous cyclooxygenase-2-dependent prostaglandin E2production by stromal cells in the murine small intestine lamina propria: directing the tone of the intestinal immune response. J Immunol. 2001;166:4465–4472. doi: 10.4049/jimmunol.166.7.4465. [DOI] [PubMed] [Google Scholar]
- 34.Reuter BK, Asfaha S, Buret A, Sharkey KA, Wallace JL. Exacerbation of inflammation-associated colonic injury in rat through inhibition of cyclooxygenase-2. J Clin Invest. 1996;98:2076–2085. doi: 10.1172/JCI119013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Morteau O. COX-2: promoting tolerance. Nat Med. 1999;5:867–868. doi: 10.1038/11301. [DOI] [PubMed] [Google Scholar]
- 36.Shinomiya S, et al. Regulation of TNF alpha and interleukin-10 production by prostaglandins I(2) and E(2): studies with prostaglandin receptor-deficient mice and prostaglandin E-receptor subtype-selective synthetic agonists. Biochem Pharmacol. 2001;61:1153–1160. doi: 10.1016/s0006-2952(01)00586-x. [DOI] [PubMed] [Google Scholar]
- 37.Yamane H, Sugimoto Y, Tanaka S, Ichikawa A. Prostaglandin E(2) receptors, EP2 and EP4, differentially modulate TNF-alpha and IL-6 production induced by lipopolysaccharide in mouse peritoneal neutrophils. Biochem Biophys Res Commun. 2000;27:224–228. doi: 10.1006/bbrc.2000.3779. [DOI] [PubMed] [Google Scholar]
- 38.Rossi D, Zlotnik A. The biology of chemokines and their receptors. Annu Rev Immunol. 2000;18:217–242. doi: 10.1146/annurev.immunol.18.1.217. [DOI] [PubMed] [Google Scholar]
- 39.Axelsson LG, Landstrom E, Goldschmidt TJ, Gronberg A, Bylund-Fellenius AC. Dextran sulfate sodium (DSS) induced experimental colitis in immunodeficient mice: effects in CD4(+)-cell depleted, athymic and NK cell depleted SCID mice. Inflamm Res. 1996;45:181–191. doi: 10.1007/BF02285159. [DOI] [PubMed] [Google Scholar]
- 40.Dieleman LA, et al. Dextran sulfate sodium-induced colitis occurs in severe combined immunodeficient mice. Gastroenterology. 1994;107:1643–1652. doi: 10.1016/0016-5085(94)90803-6. [DOI] [PubMed] [Google Scholar]
- 41.Dieleman LA, et al. Chronic experimental colitis induced by dextran sulphate sodium (DSS) is characterized by Th1 and Th2 cytokines. Clin Exp Immunol. 1998;114:385–391. doi: 10.1046/j.1365-2249.1998.00728.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Emmrich F, Thole J, van Embden J, Kaufmann SH. A recombinant 64 kilodalton protein of Mycobacterium bovisbacillus Calmette-Guerin specifically stimulates human T4 clones reactive to mycobacterial antigens. J Exp Med. 1986;163:1024–1029. doi: 10.1084/jem.163.4.1024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Powrie F, et al. Inhibition of Th1 responses prevents inflammatory bowel disease in SCID mice reconstituted with CD45RBhi CD4+T cells. Immunity. 1994;1:553–562. doi: 10.1016/1074-7613(94)90045-0. [DOI] [PubMed] [Google Scholar]
- 44.Berg DJ, Davidson N. Enterocolitis and colon cancer in interleukin-10-deficient mice are associated with aberrant cytokine production and CD4(+) Th1-like responses. J Clin Invest. 1996;98:1010–1020. doi: 10.1172/JCI118861. [DOI] [PMC free article] [PubMed] [Google Scholar]