Abstract
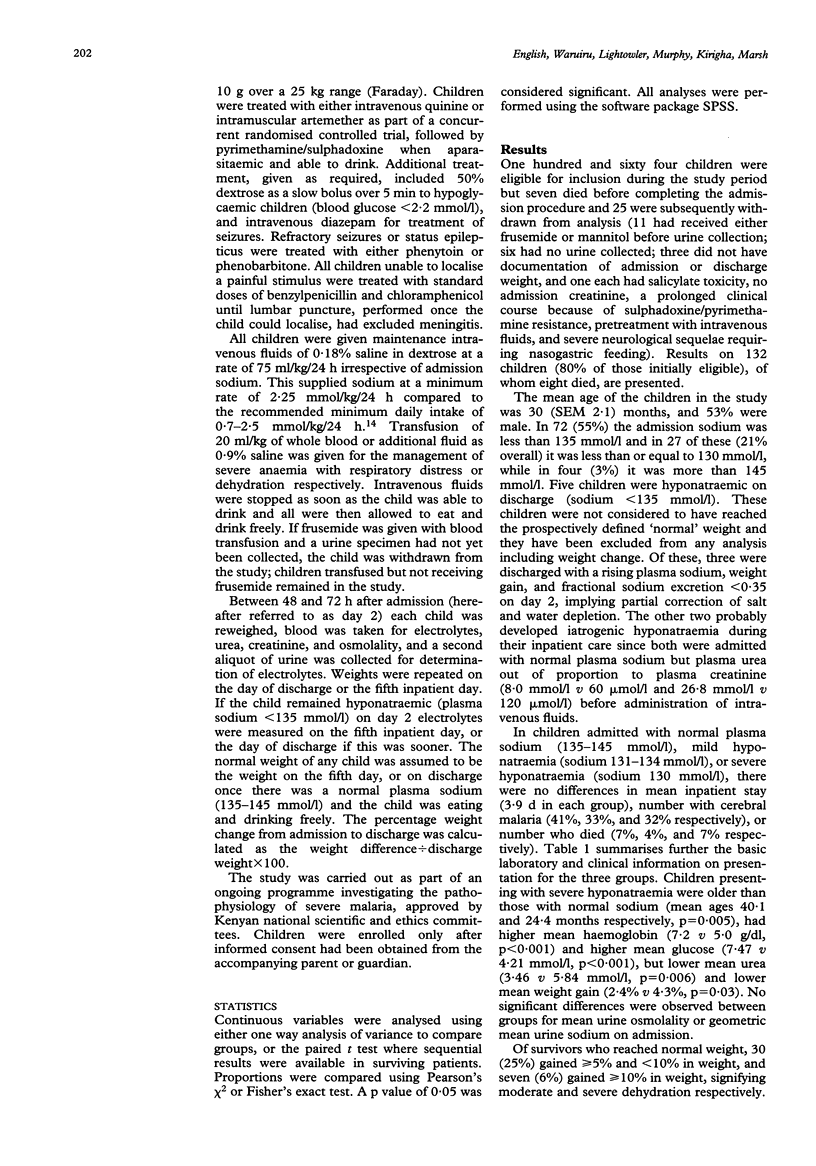
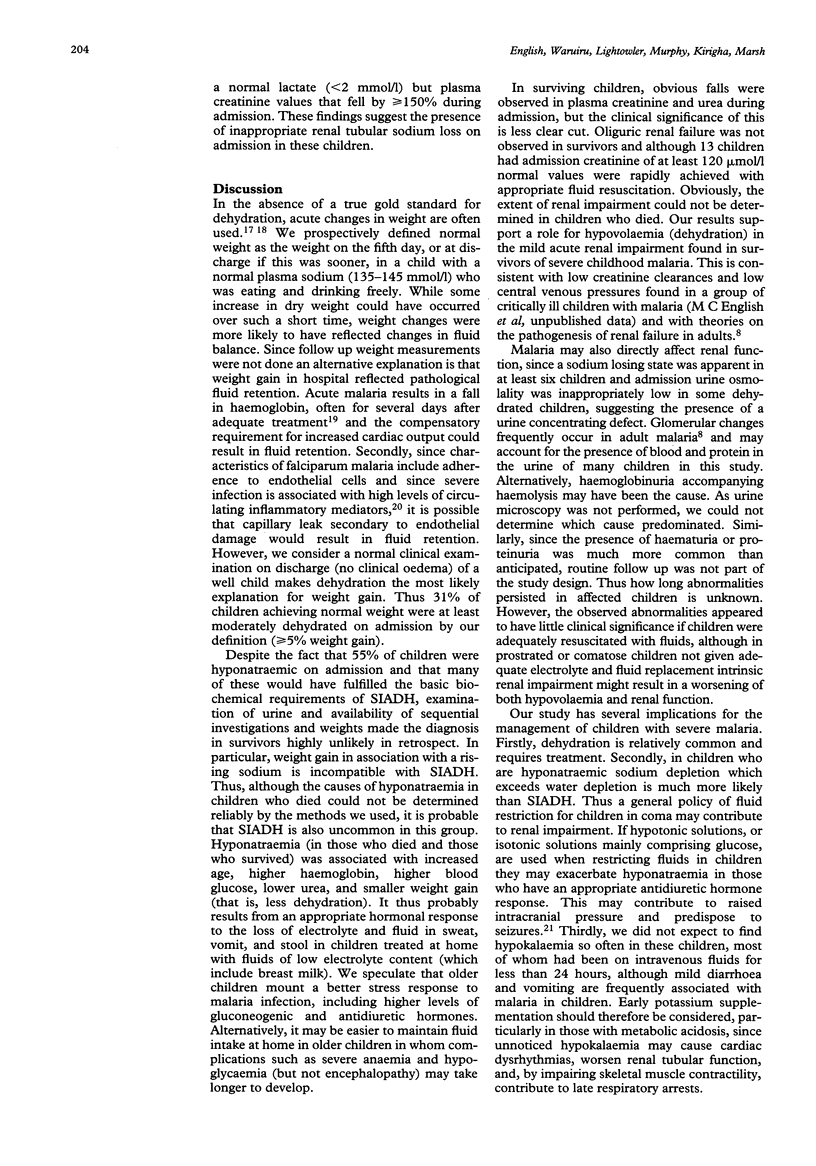
The prevalence and likely cause of hyponatraemia in severe childhood malaria were investigated. One hundred and thirty two children, 47 of whom had cerebral malaria, were prospectively recruited and serial simple indices of fluid and electrolyte balance and renal function monitored during admission. In 55%, hyponatraemia (sodium < 135 mmol/l) was present on admission. Hyponatraemia was pronounced (sodium < or = 130 mmol/l) in 21%, and these children gained less weight during admission (mean weight gain 2.4% v 4.3%) than children with a normal sodium (135-145 mmol/l). Overall, 31% of survivors were at least moderately dehydrated on admission (5% weight gain by discharge). These children had higher plasma urea concentrations on admission (6.1 v 4.5 mmol/l) and were more acidotic (mean base excess -12.1 v -8.0) than children who were not dehydrated. There were changes in simple indices of renal function between admission and discharge in children who survived (creatinine 65.7 v 37.9 mumol/l and urea 5.5 v 1.9 mmol/l). The results suggest that dehydration is common in severe childhood malaria, that it may contribute to mild impairment in renal function, and that hyponatraemic children are less water depleted, showing appropriate rather than inappropriate secretion of antidiuretic hormone.
Full text
PDF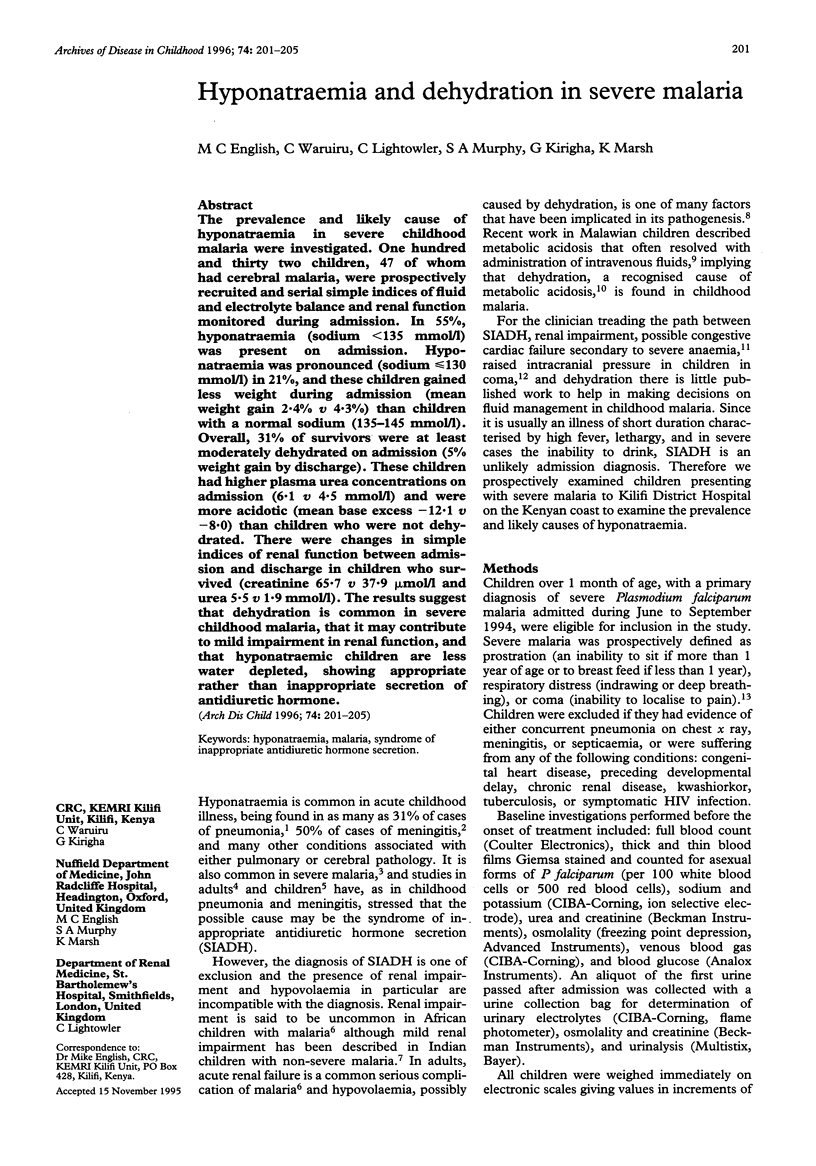


Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Abdalla S., Weatherall D. J., Wickramasinghe S. N., Hughes M. The anaemia of P. falciparum malaria. Br J Haematol. 1980 Oct;46(2):171–183. doi: 10.1111/j.1365-2141.1980.tb05956.x. [DOI] [PubMed] [Google Scholar]
- Ahmad S. H., Danish T., Faridi M. M., Ahmad A. J., Fakhir S., Khan A. S. Renal function in acute malaria in children. J Trop Pediatr. 1989 Dec;35(6):291–294. doi: 10.1093/tropej/35.6.291. [DOI] [PubMed] [Google Scholar]
- Andrew R. D. Seizure and acute osmotic change: clinical and neurophysiological aspects. J Neurol Sci. 1991 Jan;101(1):7–18. doi: 10.1016/0022-510x(91)90013-w. [DOI] [PubMed] [Google Scholar]
- Bartter F. C., Schwartz W. B. The syndrome of inappropriate secretion of antidiuretic hormone. Am J Med. 1967 May;42(5):790–806. doi: 10.1016/0002-9343(67)90096-4. [DOI] [PubMed] [Google Scholar]
- Boonpucknavig V., Sitprija V. Renal disease in acute Plasmodium falciparum infection in man. Kidney Int. 1979 Jul;16(1):44–52. doi: 10.1038/ki.1979.101. [DOI] [PubMed] [Google Scholar]
- Dhawan A., Narang A., Singhi S. Hyponatraemia and the inappropriate ADH syndrome in pneumonia. Ann Trop Paediatr. 1992;12(4):455–462. doi: 10.1080/02724936.1992.11747614. [DOI] [PubMed] [Google Scholar]
- Gennari F. J. Current concepts. Serum osmolality. Uses and limitations. N Engl J Med. 1984 Jan 12;310(2):102–105. doi: 10.1056/NEJM198401123100207. [DOI] [PubMed] [Google Scholar]
- Holst F. G., Hemmer C. J., Kern P., Dietrich M. Inappropriate secretion of antidiuretic hormone and hyponatremia in severe falciparum malaria. Am J Trop Med Hyg. 1994 May;50(5):602–607. doi: 10.4269/ajtmh.1994.50.602. [DOI] [PubMed] [Google Scholar]
- KILDEBERG P. METABOLIC ACIDOSIS IN INFANTILE GASTROENTERITIS. PHYSIOLOGIC AND THERAPEUTIC ASPECTS. Acta Paediatr Scand. 1965 Mar;54:155–167. doi: 10.1111/j.1651-2227.1965.tb06357.x. [DOI] [PubMed] [Google Scholar]
- Kovacs L., Robertson G. L. Syndrome of inappropriate antidiuresis. Endocrinol Metab Clin North Am. 1992 Dec;21(4):859–875. [PubMed] [Google Scholar]
- Kwiatkowski D., Hill A. V., Sambou I., Twumasi P., Castracane J., Manogue K. R., Cerami A., Brewster D. R., Greenwood B. M. TNF concentration in fatal cerebral, non-fatal cerebral, and uncomplicated Plasmodium falciparum malaria. Lancet. 1990 Nov 17;336(8725):1201–1204. doi: 10.1016/0140-6736(90)92827-5. [DOI] [PubMed] [Google Scholar]
- Mackenzie A., Barnes G., Shann F. Clinical signs of dehydration in children. Lancet. 1989 Sep 9;2(8663):605–607. doi: 10.1016/s0140-6736(89)90723-x. [DOI] [PubMed] [Google Scholar]
- Marsh K., Forster D., Waruiru C., Mwangi I., Winstanley M., Marsh V., Newton C., Winstanley P., Warn P., Peshu N. Indicators of life-threatening malaria in African children. N Engl J Med. 1995 May 25;332(21):1399–1404. doi: 10.1056/NEJM199505253322102. [DOI] [PubMed] [Google Scholar]
- Miller L. H., Makaranond P., Sitprija V., Suebsanguan C., Canfield C. J. Hyponatraemia in malaria. Ann Trop Med Parasitol. 1967 Sep;61(3):265–279. doi: 10.1080/00034983.1967.11686487. [DOI] [PubMed] [Google Scholar]
- Newton C. R., Kirkham F. J., Winstanley P. A., Pasvol G., Peshu N., Warrell D. A., Marsh K. Intracranial pressure in African children with cerebral malaria. Lancet. 1991 Mar 9;337(8741):573–576. doi: 10.1016/0140-6736(91)91638-b. [DOI] [PubMed] [Google Scholar]
- Ogunye O., Gbadebo A. O. Syndrome of inappropriate antidiuretic hormone (SIADH) in measles and malaria infections. Trop Geogr Med. 1981 Jun;33(2):165–168. [PubMed] [Google Scholar]
- Powell K. R., Sugarman L. I., Eskenazi A. E., Woodin K. A., Kays M. A., McCormick K. L., Miller M. E., Sladek C. D. Normalization of plasma arginine vasopressin concentrations when children with meningitis are given maintenance plus replacement fluid therapy. J Pediatr. 1990 Oct;117(4):515–522. doi: 10.1016/s0022-3476(05)80682-1. [DOI] [PubMed] [Google Scholar]
- Shann F., Germer S. Hyponatraemia associated with pneumonia or bacterial meningitis. Arch Dis Child. 1985 Oct;60(10):963–966. doi: 10.1136/adc.60.10.963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor T. E., Borgstein A., Molyneux M. E. Acid-base status in paediatric Plasmodium falciparum malaria. Q J Med. 1993 Feb;86(2):99–109. [PubMed] [Google Scholar]


