Abstract
BACKGROUND
Male veterans receiving Veterans Health Administration (VA) care have worse health than men in the general population. Less is known about health status in women veteran VA patients, a rapidly growing population.
OBJECTIVE
To characterize health status of women (vs men) veteran VA patients across age cohorts, and assess gender differences in the effect of social support upon health status.
DESIGN AND PATIENTS
Data came from the national 1999 Large Health Survey of Veteran Enrollees (response rate 63%) and included 28,048 women and 651,811 men who used VA in the prior 3 years.
MEASUREMENTS
Dimensions of health status from validated Veterans Short Form-36 instrument; social support (married, living arrangement, have someone to take patient to the doctor).
RESULTS
In each age stratum (18 to 44, 45 to 64, and ≥65 years), Physical Component Summary (PCS) and Mental Component Summary (MCS) scores were clinically comparable by gender, except that for those aged ≥65, mean MCS was better for women than men (49.3 vs 45.9, P<.001). Patient gender had a clinically insignificant effect upon PCS and MCS after adjusting for age, race/ethnicity, and education. Women had lower levels of social support than men; in patients aged <65, being married or living with someone benefited MCS more in men than in women.
CONCLUSIONS
Women veteran VA patients have as heavy a burden of physical and mental illness as do men in VA, and are expected to require comparable intensity of health care services. Their ill health occurs in the context of poor social support, and varies by age.
Keywords: women's health, veterans, health status, quality of life, social support
Robust empiric data and decades of clinical experience have established that male veterans receiving care in the Veterans Health Administration (VA) have worse health status than do men in the general population.1–4 However, much less is known about the health status of women veterans in the VA health care system.
This group deserves attention: there were 1.6 million women veterans in the United States as of 2000,5 and their ranks will continue to expand as women have an increasing presence in the military. With this ongoing demographic shift, VA clinicians and policy makers need to understand various health care issues unique to this population, including, at the most fundamental level, their overall health status.
Some known characteristics of women veteran VA patients would be expected to be associated with more favorable health status, others with less favorable health status. For example, women veterans are on average younger than their male counterparts,6 and younger patients tend to be in better health. Similarly, women are less likely than men to have seen combat,7 a potential source of physical injury, emotional trauma, and disability. Conversely, prior work has shown that the rate of military sexual trauma is substantially higher in women veterans than in male veterans8–10; sexual trauma is associated with decrements in health.11–13 War zone exposure likewise correlates with poor physical health in women.14 There is little available information about the net effect of these and other characteristics of women veterans upon health status.15
Contextual factors mediate the impact of illness upon functional health status. Social support is a particularly powerful contextual factor, affecting a range of health outcomes,16–20 sometimes differently in woman than in men.21 The typical woman veteran makes a nontraditional career choice in early adulthood; that decision could have a lifelong series of repercussions upon higher education, marriage, childbearing, employment, and connectedness to social networks.22 Social ramifications of military service may be less pronounced for men. Thus, the health status of women veterans must be understood against the backdrop of their social support structures.
Therefore, we used existing national survey data to examine the health status of women veterans in VA, benchmarking them against male veterans, whose health issues are much better understood. Our specific questions were:
Does the health status of women veterans differ from that of male veterans, across age strata?
What is the contribution of female gender to physical and mental health status after accounting for age, race/ethnicity, and education?
Does social support influence health status differently in women veterans than in men veterans?
METHODS
Data Source
Data came from the 1999 Large Health Survey of Veteran Enrollees, a cross-sectional, mailed survey assessing health and functional status in a national sample of VA enrollees. A random sample of 1.5 million veterans enrolled in VA as of March 1999 (from a sampling frame of 3.4 million) received a mailed questionnaire between July 1999 and January 2000, using a modified Dillman Approach with 4 carefully spaced mailings over 12 weeks.23
Patient Sample
From the 887,775 respondents (63% of the 1,406,049 surveyed who were living and had valid names/addresses),24 we excluded patients for whom gender or age (ranging from 18 to 98 years) could not be ascertained (N=39,296, 4.4%), or who reported in the survey that they had received no VA care in the prior 3 years (N=168,620, 19.0%). Six hundred seventy-nine thousand eight hundred and fifty-nine patients (28,048 women and 651,811 men) constituted the analytic cohort for this study. This secondary data analysis was approved by the human studies committee at Edith Nourse Rogers Memorial Veterans Hospital.
Variables
Patient gender and age were available from VA administrative data. Because patients could select as many race/ethnicity categories as applied, we used a hierarchy to assign race/ethnicity so as to maximize identification of minority subgroups. Specifically, if a patient selected more than one race/ethnicity category (true for 4% of patients), she/he was assigned to the lowest prevalence race/ethnicity group selected. As “white” was the highest prevalence group, a patient was “white” only if she/he selected the category “white” and no other categories. Education and employment status likewise came from self-report.
The 1999 Large Health Survey of Veteran Enrollees included 3 indicators of social support, originally developed for the Veterans Health Study from established constructs of social support25: whether the patient was currently married, whether the patient was living alone, and whether the patient had someone who could take him/her to the doctor if needed. The items were completed by 96%, 92%, and 99% of subjects, respectively. These indicators of social support have important health correlates, and can influence health outcomes differently.16, 26–30 Survey items were also used to determine whether VA was the patient's exclusive source of care in the past year and in the past 3 years.
To assess health status, we used scales from the Veterans SF-36 health survey instrument, a version of the Short Form 36 (SF-36) modified for use in veteran populations. The SF-36 has been used in diverse patient populations, and has well-established validity and reliability.31–34 The SF-36 examines 8 domains of health: physical functioning (PF), role limitations because of physical problems (RP), bodily pain (BP), general health (GH), role limitations because of emotional problems (RE), mental health (MH), energy/vitality (VT), and social function (SF), each scored from 0 to 100 where 100 denotes best health. The Physical Component Summary (PCS) and Mental Component Summary (MCS) are weighted summaries of physical and mental health status, respectively, using weights derived from a national probability sample of the U.S. population (weighted to a U.S. population mean of 50 and standard deviation of 10).35 The Veterans SF-36 includes modifications to the role physical and role emotional scales, with improvements to the reliability and validity of the original version.25, 36, 37, 38 Among our subjects, 93% completed the Veterans SF-36 items in usable format.
Analyses
The characteristics of veterans using VA care vary by war era.3, 39 Therefore, to better understand the characteristics of various cohorts, we stratified the women and men in our cohort by age: <35, 35 to 44, 45 to 54, 55 to 64, 65 to 74, and ≥75 years. Then, in age-stratified analyses, we compared socio-demographic characteristics, source of care (VA only or VA plus non-VA), and levels of social support for women versus men.
We used t tests to compare mean Veterans SF-36 scores (8 domains and 2 summary scores) by age, but for parsimony we collapsed age strata into 3 groups (<45, 45 to 64, and ≥65 years). Based on prior work,1 we considered a small effect of at least 20% of 1 standard deviation for the 8 Veterans SF-36 scales and the PCS and MCS scores to be clinically significant. In a sensitivity analysis we used least squares means to adjust for age as a continuous variable within age strata, to account for differences in average age by gender. Next, in a multiple regression model we assessed the independent effect of patient gender upon PCS and MCS scores after controlling for age, race/ethnicity, and education.
Finally, we calculated mean PCS and MCS scores, stratified by gender and age, for patients with versus without indicators of social support (married, live with someone, have someone who could take patient to the doctor). We then used t tests to compare those means.
RESULTS
Among veterans using VA care, women tended to be younger than men (Table 1). Across age strata, women were more highly educated than men, and in the youngest cohort, a greater proportion of women than men were nonwhite. Among patients less than 65 years old, women were more likely than men to report that some of their care was provided outside of VA.
Table 1.
Sociodemographic, Utilization, and Social Support Characteristics of Female Veterans, Benchmarked Against Male Veterans, by Age Cohort*
| Age Cohort | 18 to 34 | 35 to 44 | 45 to 54 | 55 to 64 | 65 to 75 | 75+ | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| F | M | F | M | F | M | F | M | F | M | F | M | |
| N | 4,033 | 14,926 | 6,956 | 38,107 | 6,641 | 126,252 | 3,010 | 116,881 | 2,574 | 197,983 | 4,834 | 157,662 |
| % | 14.4 | 2.3 | 24.8 | 5.9 | 23.7 | 19.4 | 10.7 | 17.9 | 9.2 | 30.4 | 17.2 | 24.2 |
| Sociodemographics | ||||||||||||
| White (%) | 59.6 | 64.5 | 58.9 | 58.8 | 66.2 | 67.8 | 79.8 | 74.8 | 84.6 | 80.0 | 91.9 | 83.8 |
| Black (%) | 26.1 | 18.1 | 27.6 | 25.4 | 20.7 | 17.5 | 9.9 | 12.8 | 7.5 | 10.0 | 3.2 | 8.0 |
| Hispanic (%) | 7.0 | 10.1 | 5.7 | 8.4 | 4.3 | 6.8 | 2.3 | 5.6 | 2.4 | 5.4 | 1.4 | 4.2 |
| Other (%) | 7.3 | 7.3 | 7.8 | 7.4 | 8.8 | 7.8 | 8.0 | 6.7 | 5.5 | 4.6 | 3.5 | 4.0 |
| College grad (%) | 17.7 | 13.2 | 25.1 | 12.4 | 32.2 | 14.8 | 25.1 | 15.0 | 19.9 | 12.3 | 19.4 | 11.3 |
| Employed (%) | 62.5 | 73.7 | 58.8 | 60.5 | 51.8 | 48.0 | 36.7 | 36.0 | 12.1 | 13.6 | 4.4 | 6.0 |
| Source of health care | ||||||||||||
| VA only past 3 y (%) | 25.8 | 36.2 | 33.7 | 42.7 | 41.1 | 48.2 | 48.3 | 50.2 | 45.4 | 44.3 | 38.9 | 38.5 |
| VA only past 1 y (%) | 31.6 | 36.9 | 39.6 | 44.7 | 47.1 | 51.8 | 55.3 | 55.7 | 49.1 | 48.7 | 42.6 | 41.6 |
| Social support indicators | ||||||||||||
| Not married (%) | 60.3 | 54.6 | 60.2 | 51.6 | 61.8 | 47.6 | 66.0 | 41.1 | 70.8 | 32.2 | 71.4 | 30.9 |
| Live alone (%) | 16.3 | 18.1 | 20.0 | 22.5 | 28.1 | 25.2 | 38.8 | 25.4 | 48.1 | 22.3 | 52.5 | 22.1 |
| No one to take to doctor (%) | 14.4 | 10.9 | 19.6 | 16.5 | 21.9 | 16.5 | 20.6 | 13.9 | 18.5 | 10.6 | 15.1 | 9.6 |
This table is descriptive, so tests of statistical significance are not presented; F refers to females, M to males; VA is Veterans Health Administration.
Levels of social support were almost universally lower in women than in men, across age strata (Table 1). Women were more likely to be unmarried and to have no one to take them to the doctor if unwell, and women over age 45 years were progressively more likely than men to live alone. For example, among patients 75 years and older, 71.4% of women (vs 30.9% of men) were not married, 52.5% of women (vs 22.1% of men) lived alone, and 15.1% of women (vs 9.6% of men) had no one to take them to the doctor.
In each age stratum (18 to 44, 45 to 64, 65 or higher), PCS and MCS scores were clinically comparable in women and men, except that for those aged ≥65 years, mean MCS score was better for women (49.3) than for men (45.9) (Table 2). For the 8 dimensions of the Veterans SF-36, scores of women tended to be comparable to or—in a few instances, for older women—better than those of men.
Table 2.
Mean SF-36 Scores for Physical and Mental Health Status of Women Versus Men Across Age Groups
| Age 18–44 | Age 45–64 | Age 65–98 | |||||||
|---|---|---|---|---|---|---|---|---|---|
| N | Women 10,989 | Men 53,033 | Delta* | Women 9,651 | Men 243,133 | Delta* | Women 7,408 | Men 355,645 | Delta* |
| Physical | |||||||||
| PF | 66.8 | 66.0 | 0.8† | 56.4 | 53.2 | 3.2‡ | 45.5 | 46.2 | −0.7‡ |
| RP | 53.3 | 50.7 | 2.5‡ | 43.4 | 35.5 | 7.9‡ | 33.0 | 27.5 | 5.5‡ |
| BP | 50.8 | 50.3 | 0.6 | 46.7 | 45.0 | 1.7‡ | 49.6 | 47.8 | 1.8‡ |
| GH | 53.7 | 51.6 | 2.1‡ | 51.2 | 43.8 | 7.4‡ | 53.7 | 45.2 | 8.5‡ |
| Emotional/social | |||||||||
| RE | 62.2 | 61.6 | 0.6 | 58.9 | 50.2 | 8.8‡ | 60.3 | 49.0 | 11.3‡ |
| MH | 61.8 | 61.6 | 0.2 | 62.2 | 58.9 | 3.4‡ | 72.0 | 66.9 | 5.2‡ |
| VT | 41.5 | 45.5 | −4.0‡ | 40.3 | 39.8 | 0.5 | 45.3 | 41.8 | 3.5‡ |
| SF | 58.9 | 59.1 | −0.2 | 57.7 | 54.4 | 3.2‡ | 64.0 | 59.9 | 4.1‡ |
| Summary scores | |||||||||
| PCS (physical) | 40.7 | 40.2 | 0.6‡ | 37.1 | 35.5 | 1.6‡ | 33.6 | 33.0 | 0.5‡ |
| MCS (mental) | 42.8 | 43.4 | −0.6‡ | 43.8 | 42.1 | 1.8‡ | 49.3 | 45.9 | 3.4‡ |
Delta: Mean score for women minus mean score for men; differences in bold are of clinically meaningful magnitude (i.e., >20% of 1 standard deviation)
P<.05 (Note: exact P-values are presented in online Appendix 1).
P<.001.
PF, Physical Function; RP, Role Functioning, Physical; BP, Bodily Pain; GH, General Health Perception; RE, Role Functioning, Emotional; MH, Mental Health Index; VT, Energy and Vitality; SF, Social Function; PCS, Physical Component Summary; MCS, Mental Component Summary.
In a sensitivity analysis (data not shown in Tables; online Appendix 2), we modeled scores for the 8 dimensions and 2 summary scales of the Veterans SF-36 as a function of patient gender and patient age within age strata. The magnitude of difference in scores for women versus men was generally comparable to that shown in Table 2.
Next, we examined PCS and MCS scores as a function of patient gender, age category, race/ethnicity, and education, stratified based on whether or not the patient had received any non-VA care in the prior 3 years (Table 3). Findings were generally similar for patients receiving care in VA only and in those receiving both VA and non-VA care. Patient gender had a clinically insignificant (but positive) effect upon PCS and MCS scores when these other factors were taken into account, certainly much less pronounced than the effect of age or education.
Table 3.
Parameter Estimates From Regression Models on Physical Component Summary (PCS) and Mental Component Summary (MCS) Scores in Veterans Who Used Veterans Health Administration (VA) Services Only or VA Plus non-VA Services During the Past 3 Years*
| Used VA Care Only in Past 3 y N=300,261 | P | Used VA+non-VA Care in Past 3 y N=379,598 | P | |
|---|---|---|---|---|
| PCS | ||||
| Intercept | 40.3 | † | 39.1 | † |
| Female | 0.5 | † | 0.6 | † |
| Age 65+ | −7.7 | † | −6.7 | † |
| Age 45 to 64 | −5.1 | † | −4.4 | † |
| African American | 1.1 | † | 0.0 | .64 |
| Hispanic | 1.2 | † | 0.2 | .014 |
| Other race | −1.0 | † | −1.6 | † |
| College graduate | 4.0 | † | 4.5 | † |
| MCS | ||||
| Intercept | 42.5 | † | 43.4 | † |
| Female | 1.0 | † | 0.6 | † |
| Age 65+ | 2.7 | † | 2.6 | † |
| Age 45 to 64 | −0.8 | † | −1.4 | † |
| African American | 0.2 | .03 | −0.4 | † |
| Hispanic | −2.6 | † | −3.5 | † |
| Other race | −1.8 | † | −1.9 | † |
| College graduate | 3.7 | † | 4.4 | † |
The intercept represents the mean PCS (or MCS) score for a white male age <45 years who did not graduate from college. Estimates for other groups can be calculated from these scores. For example, the mean PCS score for a white woman age 65+who graduated from college in the “VA only” group would be: 40.3+(0.5)+(−7.7)+(4.0)=37.1.
P<.001.
Finally, as Table 4 shows, indicators of social support had a complex effect upon health status. Being married had a paradoxical adverse effect on PCS score in men under age 45; the effect of social support upon PCS was not clinically significant in other groups. Being married or living with someone had a beneficial effect on MCS in men (but not women) under age 65. For example, among patients <45 years old, men living with someone had a 3.4 point better MCS score than did men living alone, whereas women living with someone had only a 1.1 point better MCS score than did women living alone; this difference in women did not reach the threshold for clinical significance. Having someone who could take the patient to the doctor when needed had a large beneficial effect on MCS in all gender-age groups and especially in patients less than 65 years old.
Table 4.
Difference in Mean Physical Component Summary (PCS) and Mental Component Summary (MCS) Health Status Scores in Patients With Versus Without Indicators of Social Support, by Gender and Age
| Domain of Social Support | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Married | Live With Someone | Someone Could Take to Doctor | ||||||||||
| Female | P | Male | P | Female | P | Male | P | Female | P | Male | P | |
| PCS | ||||||||||||
| Age 18 to 44 | −1.9 | * | −2.9 | * | −1.4 | * | −1.6 | * | 1.8 | * | 1.0 | * |
| Age 45 to 64 | 0.1 | .85 | −1.2 | * | 0.0 | .95 | −0.8 | * | 2.0 | * | 0.1 | .14 |
| Age 65 to 98 | 2.0 | * | −0.8 | * | 0.0 | .85 | −1.1 | * | 0.9 | .02 | 0.0 | .86 |
| MCS | ||||||||||||
| Age 18 to 44 | 1.8 | * | 3.2 | * | 1.1 | .005 | 3.4 | * | 6.2 | * | 6.6 | * |
| Age 45 to 64 | 2.1 | * | 3.0 | * | 1.6 | * | 3.0 | * | 5.7 | * | 5.4 | * |
| Age 65 to 98 | 0.6 | .06 | 1.1 | * | −0.2 | .54 | 1.1 | * | 3.2 | * | 3.8 | * |
Difference significant at P<.001; a positive difference means that patients with more social support have better health status than patients with less social support. Note: Differences in bold face are of clinically meaningful magnitude (i.e., >20% of 1 standard deviation).
PCS, physical component summary; MCS, mental component summary.
DISCUSSION
Among veterans using VA care, physical and mental health status are comparable across genders in each age stratum, except that mental health status is better for elderly women than for elderly men. Health status is also comparable across genders after controlling for age, race/ethnicity, and education. The association between indicators of social support and health status is complex; being married or living with someone benefits mental health status in men but not in women (among patients less than 65 years old), whereas having instrumental support benefits mental health status in both men and women.
Overall, the health status of women veterans is comparable to the health status of male veterans, who represent the bulk of VA clinicians' practices, and who are well known to be much sicker, on average, than the general population.1–4 Our findings are generally similar to prior VA work by Skinner et al.15 except that in that study, women veterans had even lower mental health function than did a comparison group of men; however, unlike our national study, theirs was conducted at a single tertiary care VA facility which was a referral center for women with posttraumatic stress disorder. Therefore, our findings extend this line of inquiry by being nationally representative.
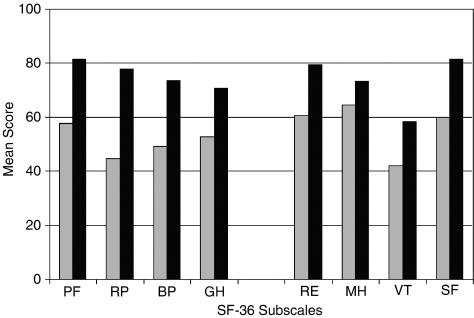
Comparing mean SF-36 subscale scores of the women veterans in our cohort (who had a mean age of 52 years) to those of women in the general population31 (who had a mean age of 46 years40), women veterans have consistently and markedly worse scores in every domain of physical and mental health (see Fig. 1). Likewise, comparing mean SF-36 subscale scores of the women veterans in our cohort to care-seeking private sector patients in the Medical Outcomes Study (who were 53% female and had a mean age of 55 years),32 scores in the general population of women veteran VA patients were comparable to or worse than scores of the subset of private sector patients who had “serious chronic medical conditions” (symptomatic congestive heart failure patients, myocardial infarction survivors with recurring angina and/or severe congestive heart failure symptoms, hypertension patients with severe congestive heart failure symptoms and/or history of stroke, and diabetes patients with severe complications). Differences were particularly marked for Bodily Pain (mean score 49.1 vs 65.1 in women veteran VA patients vs care-seeking private sector patients with serious medical conditions, respectively), Role Emotional (60.6 vs 76.2, respectively) and Social Function (59.8 vs 80.0, respectively).32 Thus, like male veteran patients, women veterans in VA have particularly poor health status.
FIGURE 1.
Mean Short Form 36 subscale scores (unadjusted) in women veterans in the current study (gray bars) compared with Medical Outcomes Study data31 for women in the general population (black bars). PF, Physical Function; RP, Role Functioning, Physical; BP, Bodily Pain; GH, General Health Perception; RE, Role Functioning, Emotional; MH, Mental Health Index; VT, Energy and Vitality; SF, Social Function.
The reasons for the ill health of women veterans in VA are unknown; indeed, the finding is somewhat surprising given that good health is a prerequisite to entering the military. It could be that exposures during military service (such as physical injuries, toxic exposures, combat exposure, or military sexual trauma) distinguish women veterans from non-veteran women, adversely affecting their health.8–10, 41–43 High-risk behaviors, such as smoking or substance use, could begin during military service and persist after discharge from the armed services.44, 45 The vast majority of the 1.6 million women veterans in the United States do not receive VA care. It could be that women who elect to use VA services are sicker than other women veterans, perhaps related in part to economic disadvantage.46
Another possibility is that the markedly low levels of indicators of social support that we documented among women veterans—which is consistent with prior VA work (where gender comparisons were not available)22—contribute to their ill health. While our cross-sectional study could not test this directly, it is well established that low levels of social support are associated with adverse health outcomes.16–20 Even when married, women tend to bear a heavier burden of care giving and may receive less support themselves than do men.47, 48 This is consistent with our finding that being married or living with someone appears to benefit mental health status in men but not women. In contrast, instrumental support (having someone who could take the patient to the doctor when needed) does benefit mental health status in women. Therefore, VA's efforts to outreach to vulnerable populations—e.g., with in-home care, transportation benefits, and satellite primary care centers—may prove of particular value to women.
Gender differences varied across age cohorts. In particular, while health status summary scores were mostly comparable in women and men, an exception was that women over age 65 years had better mental health summary scores than did men. In this group the effect of social support upon mental health status was also less pronounced. Therefore, it is possible that women in this cohort had access to some types of social support (e.g., networks of friends or qualitatively different types of relationships) less available to men. Alternatively, the women in this oldest group (who represent mostly World War II and Korean era veterans) may have acquired some specific patterns of coping which distinguish them from men of their era.
With ongoing growth of women's representation in the armed services, the health care needs of VA's youngest female enrollees (who may receive VA care for the remainder of their lives) also require special scrutiny. Like their older female counterparts, young women tend to be more highly educated than men in VA, yet are less likely than men to be employed or married or to use VA as their exclusive source of care. VA needs to take possible economic hardship into account when planning care for this emerging population, given the established connections between poverty and ill health.49, 50 Clinicians will also need to monitor the degree to which their care is coordinated across health care systems. Women veterans in the youngest age group did not exceed men in dimensions of the Veterans SF-36 (unlike older women). Therefore, the possibility that, as they age, the newest cohort's health care needs will prove to be greater than those of current cohorts of older women veterans deserves exploration.
Our study must be interpreted subject to several considerations. While the response rate was high for a large national survey, the characteristics of VA patients who responded to the survey could differ from those of veterans who did not. It is also important to recognize that women veterans who use VA services may be different from women veterans who do not use VA; our findings cannot necessarily be extrapolated to the latter population. Finally, because of the cross-sectional nature of our data, causal conclusions about the association between social support and health status cannot be drawn.
Despite these limitations, there are major strengths of our study. We sampled a large proportion of the women veterans who use VA services, maximizing our ability to represent the health status of this special population. To do so, we used a well-validated measure of health status known to correlate with objective outcomes such as severity of medical conditions and mortality.32, 51 We also had the opportunity to assess indicators of social support, a strong but often neglected predictor of health.
Our study has important implications for policy makers, researchers, and health care providers. Strong age cohort effects are seen, suggesting that approaches to providing care for older women veterans may not apply to recent military discharges. Caring for the large subgroup of women with low levels of social support will require interventions sensitive to social context; to compensate for gender role differences in our society, the nature of such interventions may need to be different in women than in men. It is well known that male VHA patients have worse health status than men in the general population; our work demonstrates that female VHA patients are not substantially better off, suggesting they will require comparable intensity of services.
Supplementary material
The following supplementary material is available for this article online at http://www.blackwell-synergy.com
Standard Deviations and P-values for Mean SF-36 Scores Presented in Table S2.
Mean SF-36 scores in Women and Men by Age Strata, Adjusting for Age as a Continuous Variable Using Least Square Means (Sensitivity Analyses).
Acknowledgments
Financial Support: Work for this article was financially supported by the Veterans Health Administration through the Office of Public Health and Environmental Hazards (Project XVA-65003), by Department of Veterans Affairs Health Services Research & Development grant RCD 98-312, and by Department of Veterans Affairs' Office of Research & Development Project CSF 04-376. Data used in this manuscript were originally collected as part of the 1999 Large Health Survey of Veteran Enrollees, funded by the Department of Veterans Affairs Office for Quality and Performance. The SF-36 is a registered trademark of the Medical Outcomes Trust. The views expressed in this article are those of the authors and do not necessarily represent the views of the Department of Veterans Affairs.
The authors gratefully acknowledge the VA Office of Public Health and Environmental Hazards, and in particular Susan Mather, MD, MPH, Carole Turner, RN, MN, CNAA, and the National Women Veterans Health Strategic Work Group, for their support for this project. They also appreciate contributions of Rudolf Moos, PhD, to portions of an earlier version of the manuscript. Ms. Ann Walsh provided invaluable technical expertise.
REFERENCES
- 1.Kazis LE, Miller DR, Clark J, et al. Health-related quality of life in patients served by the Department of Veterans Affairs: results from the Veterans Health Study. Arch Intern Med. 1998;158:626–32. doi: 10.1001/archinte.158.6.626. [DOI] [PubMed] [Google Scholar]
- 2.Hankin CS, Spiro A, III, Miller DR, Kazis L. Mental disorders and mental health treatment among U.S. Department of Veterans Affairs outpatients: the Veterans Health Study. Am J Psychiatry. 1999;156:1924–30. doi: 10.1176/ajp.156.12.1924. [DOI] [PubMed] [Google Scholar]
- 3.Rosenheck R, Massari L. Wartime military service and utilization of VA health care services. Mil Med. 1993;158:223–8. [PubMed] [Google Scholar]
- 4.Randall M, Kilpatrick KE, Pendergast JF, Jones KR, Vogel WB. Differences in patient characteristics between Veterans Administration and community hospitals. Implications for VA planning. Med Care. 1987;25:1099–104. doi: 10.1097/00005650-198711000-00008. [DOI] [PubMed] [Google Scholar]
- 5.Richardson C, Waldrop J. (U. S. Census Bureau, U.S. Department of Commerce). Veterans, 2000, May 2003.
- 6.Skinner K, Christiansen C, Frayne S, et al. 2002. (VA Women Veterans Health Program and National Women Veterans Health Strategic Work Group, Office of Public Health and Environmental Hazards). Final Report: Project #XVA 65–003: Status of VA Women Veterans Health Program: Perceptions of Women Veterans Coordinators, Results of a National Survey. [Google Scholar]
- 7.Friedman MJ, Schnurr PP, McDonagh-Coyle A. Post-traumatic stress disorder in the military veteran. Psychiatr Clin North Am. 1994;17:265–77. [PubMed] [Google Scholar]
- 8.Skinner K, Kressin N, Frayne S, et al. The prevalence of military sexual assault among female Veterans Administration outpatients. J Interpers Violence. 2000;15:289–309. [Google Scholar]
- 9.Murdoch M, Nichol KL. Women veterans' experiences with domestic violence and with sexual harassment while in the military. Arch Fam Med. 1995;4:411–8. doi: 10.1001/archfami.4.5.411. [DOI] [PubMed] [Google Scholar]
- 10.Turner C, Frayne S, editors. Veterans Health Initiative: Military Sexual Trauma. Washington, DC: Department of Veterans Affairs Employee Education System and the Center for Women's Health; 2004. Available at: http://www.va.gov/VHI/ [Google Scholar]
- 11.Frayne SM, Skinner KM, Sullivan LM, et al. Medical profile of women Veterans Administration outpatients who report a history of sexual assault occurring while in the military. J Womens Health Gender Based Med. 1999;8:835–45. doi: 10.1089/152460999319156. [DOI] [PubMed] [Google Scholar]
- 12.Hankin CS, Skinner KM, Sullivan LM, Miller DR, Frayne S, Tripp TJ. Prevalence of depressive and alcohol abuse symptoms among women VA outpatients who report experiencing sexual assault while in the military. J Trauma Stress. 1999;12:601–12. doi: 10.1023/A:1024760900213. [DOI] [PubMed] [Google Scholar]
- 13.Kimerling R, Clum GA, Wolfe J. Relationships among trauma exposure, chronic posttraumatic stress disorder symptoms, and self-reported health in women: replication and extension. J Trauma Stress. 2000;13:115–28. doi: 10.1023/A:1007729116133. [DOI] [PubMed] [Google Scholar]
- 14.Wolfe J, Schnurr PP, Brown PJ, Furey J. Posttraumatic stress disorder and war-zone exposure as correlates of perceived health in female Vietnam War veterans. J Consulting Clin Psych. 1994;62:1235–40. doi: 10.1037//0022-006x.62.6.1235. [DOI] [PubMed] [Google Scholar]
- 15.Skinner K, Sullivan LM, Tripp TJ, et al. Comparing the health status of male and female veterans who use VA health care: results from the VA Women's Health Project. Women Health. 1999;29:17–33. doi: 10.1300/J013v29n04_02. [DOI] [PubMed] [Google Scholar]
- 16.Ren XS, Skinner K, Lee A, Kazis L. Social support, social selection and self-assessed health status: results from the Veterans Health Study in the United States. Soc Sci Med. 1999;48:1721–34. doi: 10.1016/s0277-9536(99)00069-6. [DOI] [PubMed] [Google Scholar]
- 17.Williams RB, Barefoot JC, Califf RM, et al. Prognostic importance of social and economic resources among medically treated patients with angiographically documented coronary artery disease. JAMA. 1992;267:520–4. [PubMed] [Google Scholar]
- 18.Cohen S, Doyle WJ, Skoner DP, Rabin BS, Gwaltney JM., Jr Social ties and susceptibility to the common cold. JAMA. 1997;277:1940–4. [PubMed] [Google Scholar]
- 19.Case RB, Moss AJ, Case N, McDermott M, Eberly S. Living alone after myocardial infarction. Impact on prognosis. JAMA. 1992;267:515–9. [PubMed] [Google Scholar]
- 20.Sherbourne CD, Hays RD, Wells KB. Personal and psychosocial risk factors for physical and mental health outcomes and course of depression among depressed patients. J Consult Clin Psychol. 1995;63:345–55. doi: 10.1037//0022-006x.63.3.345. [DOI] [PubMed] [Google Scholar]
- 21.Berkman LF, Syme SL. Social networks, host resistance, and mortality: a nine-year follow-up study of Alameda County residents. Am J Epidemiol. 1979;109:186–204. doi: 10.1093/oxfordjournals.aje.a112674. [DOI] [PubMed] [Google Scholar]
- 22.Cotten SR, Skinner KM, Sullivan LM. Social support among women veterans. J Women Aging. 2000;12:39–62. doi: 10.1300/J074v12n01_04. [DOI] [PubMed] [Google Scholar]
- 23.Dillman D. Mail and Telephone Surveys: The Total Design Method. New York: John Wiley and Sons; 1978. [Google Scholar]
- 24.Perlin J, Kazis L, Skinner K, et al. (Department of Veterans Affairs). Health status and outcomes of veterans: Physical and mental component summary scores, Veterans SF36 1999 Large Health Survey of Veteran Enrollees Executive Report. May 2000.
- 25.Kazis LE, Miller DR, Skinner KM, et al. Patient-reported measures of health: the Veterans Health Study. J Ambul Care Manage. 2004;27:70–83. doi: 10.1097/00004479-200401000-00012. [DOI] [PubMed] [Google Scholar]
- 26.Sherbourne CD, Hays RD. Marital status, social support, and health transitions in chronic disease patients. J Health Soc Behav. 1990;31:328–43. [PubMed] [Google Scholar]
- 27.Berkman LF, Leo-Summers L, Horwitz RI. Emotional support and survival after myocardial infarction. A prospective, population-based study of the elderly. Ann Intern Med. 1992;117:1003–9. doi: 10.7326/0003-4819-117-12-1003. [DOI] [PubMed] [Google Scholar]
- 28.Gove WR, Hughes M, Style CB. Does marriage have positive effects on the psychological well-being of the individual? J Health Soc Behav. 1983;24:122–31. [PubMed] [Google Scholar]
- 29.Blazer DG. Social support and mortality in an elderly community population. Am J Epidemiol. 1982;115:684–94. doi: 10.1093/oxfordjournals.aje.a113351. [DOI] [PubMed] [Google Scholar]
- 30.Thompson MG, Heller K. Facets of support related to well-being: quantitative social isolation and perceived family support in a sample of elderly women. Psychol Aging. 1990;5:535–44. doi: 10.1037//0882-7974.5.4.535. [DOI] [PubMed] [Google Scholar]
- 31.Ware JE. SF-36 Health Survey: Manual and Interpretation Guide. Boston, MA: The Health Institute, New England Medical Center; 1993. [Google Scholar]
- 32.McHorney CA, Ware JE, Jr, Raczek AE. The MOS 36-Item Short-Form Health Survey (SF-36): II. Psychometric and clinical tests of validity in measuring physical and mental health constructs. Med Care. 1993;31:247–63. doi: 10.1097/00005650-199303000-00006. [DOI] [PubMed] [Google Scholar]
- 33.Ware JE, Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Medical Care. 1992;30:473–83. [PubMed] [Google Scholar]
- 34.Ware JE, Jr, Kosinski M, Bayliss MS, McHorney CA, Rogers WH, Raczek A. Comparison of methods for the scoring and statistical analysis of SF-36 health profile and summary measures: summary of results from the Medical Outcomes Study. Med Care. 1995;33(4 suppl):264–79. [PubMed] [Google Scholar]
- 35.Ware J, Kosinski M, Keller S. SF-36 Physical and Mental Health Summary Scales: A Users Manual. Boston, MA: The Health Institute, New England Medical Center; 1994. [Google Scholar]
- 36.Kazis LE, Miller DR, Clark JA, et al. Improving the response choices on the veterans SF-36 health survey role functioning scales: results from the Veterans Health Study. J Ambul Care Manage. 2004;27:263–80. doi: 10.1097/00004479-200407000-00010. [DOI] [PubMed] [Google Scholar]
- 37.Kazis L, Lee A, Spiro A, III, et al. Measurement comparisons of the medical outcomes study and the Veterans SF-36® Health Survey. Health Care Financ Rev. 2004;25:43–58. [PMC free article] [PubMed] [Google Scholar]
- 38.Jones D, Kazis L, Lee A, et al. Health status assessments using the Veterans SF-12 and SF-36: methods for evaluating outcomes in the Veterans Health Administration. J Ambul Care Manage. 2001;24:68–86. doi: 10.1097/00004479-200107000-00011. [DOI] [PubMed] [Google Scholar]
- 39.Villa VM, Harada ND, Washington D, Damron-Rodriguez J. Health and functioning among four war eras of US veterans: examining the impact of war cohort membership, socioeconomic status, mental health, and disease prevalence. Mil Med. 2002;167:783–9. [PubMed] [Google Scholar]
- 40.McHorney C, Kosinsky M, Ware J. Comparisons of the costs and quality of norms for the SF-36 Health Survey collected by mail versus telephone interview: results from a national survey. Medical Care. 1994;32:551–67. doi: 10.1097/00005650-199406000-00002. [DOI] [PubMed] [Google Scholar]
- 41.Bullman TA, Kang HK. The effects of mustard gas, ionizing radiation, herbicides, trauma, and oil smoke on US military personnel: the results of veteran studies. Annu Rev Public Health. 1994;15:69–90. doi: 10.1146/annurev.pu.15.050194.000441. [DOI] [PubMed] [Google Scholar]
- 42.Coyle B, Wolan D. The prevalence of physical and sexual abuse in women veterans seeking care at a Veterans Affairs Medical Center. Mil Med. 1996;161:588–93. [PubMed] [Google Scholar]
- 43.Proctor SP, Harley R, Wolfe J, Heeren T, White RF. Health-related quality of life in Persian Gulf War Veterans. Mil Med. 2001;166:510–9. [PubMed] [Google Scholar]
- 44.Klevens RM, Giovino GA, Peddicord JP, Nelson DE, Mowery P, Grummer-Strawn L. The association between veteran status and cigarette-smoking behaviors. Am J Prev Med. 1995;11:245–50. [PubMed] [Google Scholar]
- 45.Bradley KA, Bush KR, Davis TM, et al. Binge drinking among female Veterans Affairs patients: prevalence and associated risks. Psychol Addict Behav. 2001;15:297–305. doi: 10.1037//0893-164x.15.4.297. [DOI] [PubMed] [Google Scholar]
- 46.Wilson NJ, Kizer KW. The VA health care system: an unrecognized national safety net. Health Aff (Millwood) 1997;16:200–4. doi: 10.1377/hlthaff.16.4.200. [DOI] [PubMed] [Google Scholar]
- 47.Wilkins K. Social support and mortality in seniors. Health Rep. 2003;14:21–34. [PubMed] [Google Scholar]
- 48.Allen SM. Gender differences in spousal caregiving and unmet need for care. J Gerontol. 1994;49:S187–95. doi: 10.1093/geronj/49.4.s187. [DOI] [PubMed] [Google Scholar]
- 49.Epstein AM, Stern RS, Weissman JS. Do the poor cost more? A multihospital study of patients' socioeconomic status and use of hospital resources. New Engl J Med. 1990;322:1122–8. doi: 10.1056/NEJM199004193221606. [DOI] [PubMed] [Google Scholar]
- 50.Haan M, Kaplan GA, Camacho T. Poverty and health. Prospective evidence from the Alameda County Study. Am J Epidemiol. 1987;125:989–98. doi: 10.1093/oxfordjournals.aje.a114637. [DOI] [PubMed] [Google Scholar]
- 51.Idler EL, Benyamini Y. Self-rated health and mortality: a review of twenty-seven community studies. J Health and Soc Behav. 1997;38:21–37. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Standard Deviations and P-values for Mean SF-36 Scores Presented in Table S2.
Mean SF-36 scores in Women and Men by Age Strata, Adjusting for Age as a Continuous Variable Using Least Square Means (Sensitivity Analyses).