Abstract
OBJECTIVE
Assess the state of women veterans' health research.
DESIGN
Systematic review of studies that pertained specifically to or included explicit information about women veterans. A narrative synthesis of studies in 4 domains/topics was conducted: Stress of military life; Health and performance of military/VA women; Health services research/quality of care; and Psychiatric conditions.
MEASUREMENTS AND MAIN RESULTS
We identified 182 studies. Of these, 2 were randomized-controlled trials (RCTs) and the remainder used observational designs. Forty-five percent of studies were VA funded. We identified 77 studies pertaining to the stress of military life, of which 21 reported on sexual harassment or assault. Rates of harassment ranged from 55% to 79% and rates of sexual assault from 4.2% to 7.3% in active duty military women and 11% to 48% among women veterans. Forty-two studies concerned the health and performance of military/VA women, with 21 studies evaluating sexual assault and posttraumatic stress disorder (PTSD) and their effect on health. Fifty-nine studies assessed various aspects of health services research. Eight studies assessed quality of care and 5, patient satisfaction. Twenty-five studies assessed utilization and health care organization, and findings include that women veterans use the VA less than men, that gender-specific reasons for seeking care were common among female military and veteran personnel, that provision of gender-specific care increased women veterans' use of VA, and that virtually all VAs have available on-site basic women's health services. Fifty studies were classified as psychiatric; 31 of these were about the risk, prevalence, and treatment of PTSD.
CONCLUSIONS
Most research on VA women's health is descriptive in nature and has concerned PTSD, sexual harassment and assault, the utilization and organization of care, and various psychiatric conditions. Experimental studies and studies of the quality of care are rare.
Keywords: women, veterans, systematic review
While the Department of Veterans Affairs (VA) has historically been regarded as an agency primarily devoted to the care of male veterans, it is increasingly turning its focus to the health issues of female veterans as well. According to the 2000 U.S. Census, there are nearly 1.6 million women veterans in the United States, and while not all may be eligible for services at the VA, approximately 11.4% use the VA for some or all of their health care. On average, women veterans represent only 5.5% of all VA users at individual facilities, but are among the fastest growing segments of new users. Based on increasing numbers of active duty military women, now comprising 20% of new military recruits, the Department of Veterans Affairs' Office of Policy and Planning projects that veteran women will comprise nearly 10% of the total user population by the year 2010. Veteran women appear to have health needs that can differ from those of veteran men because of many factors including different types of military experiences, the increased prevalence of certain conditions in women, different manifestations of disease in women as compared with men, and gender-specific issues that solely affect women.
Women veterans may also have health issues specific to them that are not as prevalent in or as important to female nonveterans. These issues may relate to exposures that are unique to military personnel including chemical, environmental, and stress exposures, among others. Women who enter the military may also be different because of differing socio-economic factors, life experiences, or baseline health status. For instance, the 2001 National Survey of Veterans (http://www.va.gov/vetdata/SurveyResults/final.htm) found that women veterans are more likely to be members of racial-ethnic minorities than nonveterans.
In order to address these health needs, the VA has focused attention on service delivery for women and on research that enhances VA's understanding of women veteran health issues and ways to optimize their care delivery.
An orderly progression of research on women veterans' health has been hindered by the lack of a systematic evaluation of the literature. Our goal was to evaluate the medical literature related to women veterans in order to summarize the current state of knowledge related to women veterans and their health, identify gaps to help focus future research efforts in this area, and make available a database of women veterans research that could serve as a resource to those involved in health care delivery to or research on women veterans.
METHODS
Literature Search and Selection
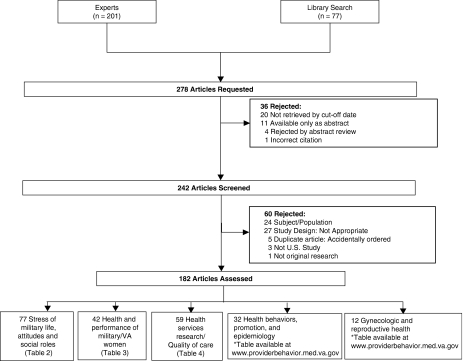
The search for women veterans research studies presented a challenge as “women veterans” is a population that is not indexed in computerized databases. Therefore, we employed 3 main search techniques: computerized searches of Medline (November 17, 2004) and PsychInfo (December 22, 2004) using the text words “woman,”“women,”“female,” and “veteran,*” a snowball sample of experts from whom we requested articles from their personal files, and reference mining of all included studies. Unpublished and gray literature was sought and retrieved. Details of the search and yield of articles are presented in Figure 1.
FIGURE 1.
Literature flow
To be accepted for analysis, articles had to describe original research on veterans' health that either pertained specifically to women veterans, or included explicit information about women veterans or compared men and women veterans.
Extraction of Study-Level Variables and Results
Two reviewers [C.G., T.B.], working individually, extracted data from the same articles and resolved disagreements by consensus. A senior physician [P.S.] resolved any remaining disagreements. Variables assessed were study design, funding, topic, and condition. Both topics and types of conditions were adapted from existing conceptual frameworks, with topics drawn from the Department of Defense Women's Health Research Program (1999) and types of women's health conditions presented by Haseltine and Jacobson.1 Topics included gynecologic and reproductive health; health behaviors, promotion, and epidemiology; health and performance of military/VA women; stress of military life, attitudes and social roles; and health services research/quality of care. Types of conditions included conditions affecting only women, diseases prevalent in women, conditions with different gender manifestation, environmental exposures, and substance abuse. Topics and conditions were not mutually exclusive. In any activity such as this, there are “gray zones” between categories, or areas where content can overlap, making classification of specific articles more challenging. We made certain decisions about how to classify these gray zones, based on our own knowledge and experience as researchers and through our working with VA policy makers. We classified studies about military sexual trauma as “health and performance of military women”; we grouped “quality of care” with “health services research” and considered studies of patient satisfaction to be a domain of quality. There are also somewhat arbitrary decisions about groupings. For example, there were numerous studies concerning posttraumatic stress disorder (PTSD). Rather than add a new PTSD category to the framework of Haseltine and Jacobson, we classified articles concerning PTSD into the relevant categories: those assessing relationships between experiences or exposures during military service and PTSD were placed in the category of “Stress of Military Life”; those dealing with formal measures of health status and PTSD were placed in the “Health Services Research/Quality of Care” category, while those studies dealing with the impact of PTSD on the health and performance of women were classified as “Health and Performance of Military Women.” Articles about PTSD in women that did not fit into any topic area were classified by the condition “Psychiatric” only. Topics and conditions were not mutually exclusive, and articles were classified in as many categories as were relevant.
Data Synthesis
Frequencies of data were tabulated and articles were grouped into clinically similar categories. Because only 2 experimental studies were identified, and because quality measures for observational studies are not universally agreed upon, we did not assess studies for characteristics of quality. Evidence tables were created for each category, and a narrative synthesis was performed.
Role of the Funding Source
The funder had no role in the design, execution, or reporting of the results.
RESULTS
Results of the Literature Search
Our search identified 201 articles from experts' files and an additional 77 from our library search for a total of 278 titles. Figure 1 displays the flow of the literature review. Four articles were rejected at abstract level; 11 articles were available only as abstracts and were rejected; 1 citation was incorrect; and 20 articles were not retrieved by the cutoff date. Two hundred and forty-two articles were screened and 60 were rejected; subject/population not relevant (meaning the study was not about women or about veterans —24 articles); study design not appropriate (meaning, for example, the retrieved article was not research or was not an article, such as a letter to the editor —27 articles); duplicate data (5 articles); nonU.S. population (3 articles); and not original research (1 article). Of the 242 articles screened, 182 articles informed a topic or condition of interest.
Description of Women Veterans Health Studies
The number of articles in each category is presented in Table 1. Of the articles identified and reviewed in detail, by far the greatest number were descriptive studies or observational studies of risk and prognosis. Forty-five percent of studies were reported as being supported by VA. The topics with the greatest number of articles were concentrated in 3 areas: stress of military life; health and performance of military/VA women; and health services research/quality of care. Among conditions, by far the largest number of studies concerned psychiatric conditions and emotional disorders.
Table 1.
Characteristics of Women Veterans Research Studies
| Design | N | % |
|---|---|---|
| Observational study – assesses the risk of prognosis | 111 | 61 |
| Descriptive study | 22 | 12 |
| Qualitative studies | 7 | 4 |
| Review | 4 | 2 |
| Experimental studies | 2 | 1 |
| Observational study – all other | 36 | 20 |
| VA Funding Source | 82 | 45 |
| Topic | N (Not mutually exclusive) | |
| Gynecologic and reproductive health | 12 | |
| Health behaviors, promotion, and epidemiology | 32 | |
| Health and performance of military/VA women | 42 | |
| Stress of military life, attitudes and social roles | 77 | |
| Health services research/Quality of care | 59 | |
| Other | 2 | |
| Condition | 2 | |
| Only affecting women | 7 | |
| Benign disease of the female reproductive system | 5 | |
| Breast | 2 | |
| Cancers of the reproductive tract | 3 | |
| Disease and conditions of pregnancy | 2 | |
| Disease prevalent in women | 1 | |
| Bone, join, rheumatic | 50 | |
| Endocrinology | 38 | |
| Gastrointestinal | 1 | |
| Psychiatric | 4 | |
| Different gender manifestation | 9 | |
| Emotional disorders | 12 | |
| Environmental exposures | 7 | |
| Estrogen | 1 | |
| Occupational hazards | 17 | |
| Substance abuse | ||
| Alcohol | 9 | |
| Drugs | 12 | |
| Smoking | 7 | |
| Prescription drugs | 1 | |
| Other | 17 | |
Summary of Studies
All research studies were entered into evidence tables, which are available from the authors or at http://www.providerbehavior.med.va.gov and at the JGIM website. In addition, 4 review articles were identified but not included in the evidence tables. One paper reviewed how the stressors of extreme environments, like military environments, may affect the health of military women and underlie potential gender differences in the effects of stress on health.2 Another dealt with a review of VA health services for women, including new initiatives.3 It describes how the VA expanded services for women by creating comprehensive women veterans health centers, positions for full-time women veteran coordinators, and regional stress disorder teams. A third reviewed a variety of studies evaluating the health risks of veterans and exposures while in the military. It specifically focused on studies that evaluated the effects of trauma, mustard gas, ionizing radiation, herbicides, and oil smoke on military personnel.4 The last review paper described the literature regarding the health care needs of women deployed to the Persian Gulf War and found that gynecologic issues accounted for a large proportion of health problems. Other reasons for seeking care were similar to those of men.5
Two experimental studies were identified, 1 dealing with breast cancer6 and the other with a psychiatric therapy.7 The first study evaluated an intervention to improve breast cancer screening rates. Women randomized to receive additional reminders in the form of a personalized follow-up phone call by a nurse were more than 5 times as likely to undergo mammography than women receiving usual care. The second study evaluated the efficacy of dialectical behavior therapy for women veterans with borderline personality disorder and found that women randomized to receive this therapy had greater declines in suicidal ideation, parasuicidal acts, hopelessness, depression, and anger expression than women assigned to usual treatment.
Given the number of other studies identified, an in-depth narrative synthesis of all of them is beyond the limits of a journal article. Faced with a choice between breadth and depth, we chose to present a limited number of topics/conditions and discuss these in moderate depth. We will summarize the topic areas of Stress of Military Life, Health and Performance of Military/VA Women, and Health Services Research/Quality of Care, and articles categorized as pertaining to Psychiatric Conditions. We also present selected findings (Tables 2–4) that were chosen by the project team from our evidence tables for the first 3 topic areas but not from the evidence table for the Psychiatric Conditions because there is considerable overlap between that evidence table and the others. Readers are referred to the full evidence tables available at our website for a complete description of all studies.
Table 2.
Stress of Military Life: General Overview of Published Literature
| Topic (# articles) | Sample Size Ranges* | Study Characteristics | Selected Findings |
|---|---|---|---|
| Sexual harassment, sexual abuse, sexual assault (N=21> | 16–22, 372 | All specific to women Most studies of VA users | High rates of reported military sexual trauma8–24 Sexual harassment and trauma are associated with physical symptoms, medical conditions, depression, alcohol abuse, and eating disorders20, 25, 14, 10–12 |
| Gulf war era (N=21) | 19–4, 888 | Several large cohort studies | In the Ft Devens survey, women were more likely to have or develop PTSD26–32 |
| 7 from the Ft. Devens Operation Desert Storm (ODS) Reunion Survey | Post-deployment, women veterans were more likely to have a mental disorder and poorer health status26, 33, 34 | ||
| Vietnam era (N=17) | 20–9, 900 | 13 relate to PTSD or mental health | Cause-specific mortality rates for female Vietnam veterans similar to those of non-veteran females35 |
| Most smaller sample sizes | War trauma, sexual trauma, and low support at homecoming contributed to PTSD development36 | ||
| Higher PTSD scores are associated with poorer health status37 | |||
| Comparing men and women veterans (N=4) | 28–6, 804 | 7 studies from the National Vietnam Veterans Readjustment Survey (NVVRS) | NVVRS studies evaluate risk factors for PTSD among men and women serving in Vietnam38–44 |
| Men and women are at risk for trauma in the military45, 46 | |||
| Men are more likely to be diagnosed with PTSD47 |
Sample size ranges refer to the number of women included in studies. Studies of men and women may have larger total sample sizes.
Table 4.
Health Services Research: General Overview of Published Literature
| Topic (# articles) | Sample Size Ranges* | Study Characteristics | Selected Findings |
|---|---|---|---|
| Quality of care (N=8) | 66–971 | 4 patient satisfaction studies | Women veterans using women's clinics were more likely to report excellent overall satisfaction55 |
| 3 screening/prevention studies | Women veterans told to have a mammogram and those who were regular VA users were more likely to have a mammogram56 | ||
| Tools (N=7) | 127–393 | 4 trauma/PTSD questionnaires | The PTSD Checklist-Civilian Version was a useful screening instrument in women veterans in primary care57, 58 |
| 2 alcohol screening questionnaires | The AUDIT alcohol screen had good sensitivity and specificity in women veterans; the TWEAK did not59, 60 | ||
| Medical treatment (N=4) | 91–1,722 | 3 studies used national samples | Only 47% of women diagnosed with alcohol dependence in VA in FY 1993 received formal treatment61 |
| Utilization and health care organization (N=25) | 24–283,500 | 5 relate to mental health utilization | VA use by women veterans associated with older age, less private insurance, and poorer physical and mental health; military trauma was associate with former use or never use of VA62 |
| 3 assess organization of care | Female and male Vietnam veterans had equal use of VA mental health services but female veterans had greater non-VA mental health use63 | ||
| 9 national samples | Virtually all VA sites have availability of comprehensive women's health care either on-site or off-site64 | ||
| Health status (N=7) | 31–30,865 | 3 evaluate health status and PTSD | Women with PTSD had poorer physical health status than women with depression or neither diagnosis65 |
| 2 national samples | In women Vietnam veterans, PTSD was associated with increased bed days, poorer physical health, and unemployed status66 | ||
| Preventive care (N=5) | 201–328 | Single VA cohorts | Sexual assault history was associated with more risky behaviors but also increased preventive health care67 |
| Only 1/2 of women with 4 or more risk factors for heart disease worried about it68 |
Sample size ranges refer to the number of women included in studies. Studies of men and women may have larger total sample sizes.
Stress of Military Life
Within the stress of military life section, we identified 77 studies (Table 2). These studies were further categorized as relating to sexual harassment, abuse, or assault; Gulf War Era; Vietnam Era; comparisons between men and women; and, miscellaneous.
Sexual Harassment, Abuse, or Assault
There were 21 articles related to sexual harassment or assault in the military. Most evaluated regional samples of women veterans though 3 studies involved active duty military personnel. Seven studies included national samples of women veterans or active duty military. Rates of sexual harassment were particularly high for both female veterans and active duty military, ranging from 55% to 79%.9, 16, 19 Rates of sexual assault in the military were also significant, ranging from 4.2% to 7.3% in active duty military women,16, 20 and 11% to 48%8–10, 14, 17, 18, 21, 22 for women veteran samples. A number of studies found an association between sexual assault history and poorer health status16, 18, 22–24 and sexual assault history and increased numbers of medical and psychiatric conditions.10–12, 14, 15, 25
Gulf War Era
There were 21 studies classified as relating to the Gulf War Era. These mostly assessed regional samples of Gulf War veterans using surveys or other observational study methods and assessed the prevalence and risk factors for various health problems. A number of studies evaluated risks for developing PTSD or other psychologic disorders and most, though not all, found that women were more likely to develop PTSD or mood disorders than men.27, 29, 30, 33, 32, 48, 69, 70 Three studies evaluating Gulf War Syndrome or similar symptoms did not find differences between men and women.33, 48, 71
Vietnam Era
Seventeen studies related to Vietnam Era veterans. Most utilized regional samples with 3 studies of national samples of veterans. Again, the majority of articles (10 articles) related in some way to PTSD with 2 studies finding that greater PTSD symptomatology was associated with poorer health status in Vietnam era women veterans.37, 72
Fourteen studies in the stress of military life topic area compared men and women and most used surveys. Five studies utilized regional samples of veterans while 9 utilized national samples, 5 of which came from the National Vietnam Veterans Readjustment Survey (NVVRS). Ten studies concerned PTSD and most, but not all, found that many of the predictors of developing PTSD or of the severity of PTSD were similar in men and women.39–43, 45, 73, 74 Finally, 3 studies did not fit into the other sections and were categorized as miscellaneous, and concerned the process of adjusting to military life by female psychiatric patients,75 smoking characteristics,76 and World War II female prisoners of war.77
In summary, articles in the Stress of Military life section indicate that there are high reported rates of sexual victimization among military women, with higher rates among those sampled from VA programs and clinics; military sexual trauma seems to be associated with more physical and mental conditions and with poorer health status; and, among military personnel deployed to the Gulf War, women seem more likely to develop PTSD than men.
Health and Performance of Military/VA Women
Forty-two studies were categorized as dealing with Health and Performance of Military/VA Women (Table 3). We further divided this category into 4 subcategories: sexual assault and PTSD; health needs and utilization; mental health and homelessness; and miscellaneous.
Table 3.
Health and Performance of Military and/or VA Women: General Overview of Published Literature
| TOPIC (# articles) | Sample Size Ranges* | Study Characteristics | Selected Findings |
|---|---|---|---|
| Sexual assault and PTSD (N=22) | 52–30, 865 | Subjects from multiple war eras | Compared to non-Gulf war men and women, Gulf War veterans had 3 × the risk of PTSD and 4.8 × the risk of chronic fatigue syndrome48 |
| All survey studies | Alcohol abuse potentiated the effect of sexual trauma on mental illness49 | ||
| Health needs and utilization (N=9) | 41–5, 483 | Most evaluate samples from multiple war eras | Women's health needs during the Gulf War were similar to men's with the exception of gynecologic problems, and 79% sought care for at least 1 gender-specific condition5, 50 |
| More than half of both younger and older female veteran samples reported current health status as good to excellent51 | |||
| Mental health and homelessness (N=6) | 68–3, 480 | All survey studies | Using various community samples, 1.3% to 4.4% of homeless women are veterans52, 53 |
| 2 evaluate homeless populations | Women veterans at a VA women's health center had high rates of depression, anxiety, and trauma exposure54 |
Sample size ranges refer to the number of women included in studies. Studies of men and women may have larger total sample sizes.
Sexual Assault and PTSD
There were 22 studies that we classified as concerning sexual assault and PTSD8, 14, 15, 18, 24, 31, 37, 43, 46, 48, 49, 65, 66, 72, 78–85 (Table 3). Eight of these studied national samples of veterans, the remaining studied local or regional samples. Almost all of the studies assessed either risk factors for PTSD or the effect of PTSD and/or sexual assault on health and performance. A consistent finding was that a diagnosis of PTSD or a history of sexual assault was associated with much poorer health, measured in a variety of ways.15, 18, 24, 31, 37, 43, 66, 72, 78, 81, 82, 83 Relationships between sexual assault and PTSD were also reported.49, 84
Health Needs and Utilization
Nine studies were classified as dealing with health needs and utilization.5, 23, 33, 50, 51, 77, 86–88 One of these reviewed published data on health symptoms and issues of Gulf War veterans and also analyzed registry data maintained by the Department of Defense and by VA.5 The study concluded that the health needs of women were similar to those of men, except for pregnancy. Another study of Gulf War veterans receiving clinical evaluations as part of the Gulf War Comprehensive Clinical Evaluation Program reported that the most frequent diagnoses were musculoskeletal/connective tissue disorders, ill-defined conditions, and mental disorders, with women being more likely to receive the latter.33 A third study reported the prevalence of binge drinking was 25% among 1,243 women at 1 VA.87 Other studies assessed comparisons of health status between men and women, utilization for gender-specific problems, comparison of older to younger women veterans, sexual assault, and World War II prisoners of war.
Mental Health and Homelessness
Six studies concerned mental health and homelessness.52–54, 89–91 All but 1 studied local or regional samples. In the largest study,52 1.6% of homeless veterans were female, and compared with male homeless veterans, women were younger, less likely to be employed, more likely to be diagnosed with a major psychiatric disorder, and less likely to be diagnosed with a substance abuse disorder. Another study estimated that the proportion of veterans among homeless women was greater than the proportion of veterans among domiciled women, and that homelessness was 3.6 times more likely among veterans compared with nonveterans.53 Another study found women veterans in a VA Mental Health clinic were more likely than men to be diagnosed with affective disorders and less likely to have anxiety disorders.89 Two studies using PRIME-MD screening instruments reported in local samples of veterans attending a VA women's health clinic that 37% of patients endorsed symptoms of depression, 56% endorsed symptoms of anxiety, and 45% screened positive for at least 1 mental health disorder.54, 91
Miscellaneous
Lastly, 3 studies did not fit into any of the above categories. They concerned active duty female psychiatric patients,75 evaluations of vulnerability and desire for self-defense training,92 and an examination of sexual function among female veterans with and without chronic fatigue syndrome.93
Summary findings from this section include that lifetime sexual abuse rates are high for women veterans and are associated with PTSD and poorer health; that women Gulf War veterans had a significant need for gender-specific health care, which also accounted for any difference between the health needs of Gulf War men and women; and that women veterans comprise between 1.6% and 4.4% of the homeless female population and are more likely to be homeless than nonveteran women.
Health Services Research/Quality of Care
We divided the category of “health services research/quality of care” (Table 4) into 7 subcategories: utilization and health care organization; health status; preventive care; quality of care; tools and measures; medical treatment; and miscellaneous.
Utilization and Health Care Organization
Twenty-five studies assessed aspects of utilization and health care organization.50, 62–64, 84, 94–113 The majority of these (15 studies) assessed national samples of veterans. Many different aspects of utilization were studied. Findings include that women veterans use the VA less than men veterans,94, 111, 114 that gender-specific reasons for seeking care were common among female military and veteran personnel,50 that provision of gender-specific care increased women veterans' use of VA,102 that virtually all VAs have available on-site basic women's health services,64 and that half of VA sites have women's health clinics.110 Several studies assessed the use of mental health services by women veterans and reported mixed results, with some studies reporting lesser use by women and other studies reporting equivalent use by men and women.
Health Status
In the category of health status, 7 articles were identified.23, 66, 65, 78, 83, 86, 115 Specific health issues were the focus of 6 of these studies: 4 were primarily concerned with PTSD,65, 66, 78, 115 1 was concerned with the effect of military trauma and health status23 and 1 examined the relationship between sexual assault and health status.83 One regional sample of women veterans who completed the SF-36 and other health status instruments were compared with national data on male veterans; women were found to have lower scores, particularly in the areas of mental health functioning.115
Quality of Care
Eight articles were classified as assessing quality of care.55, 56, 116–121 Four assessed national samples and 4 regional or local samples. Five articles concerned satisfaction with care, 1 of which included additional outcome data, and 3 articles concerned preventive care services. Findings included that women tend to be less satisfied with care than men for some domains117, 118 and that women using VA women's clinics are more satisfied than those in general primary care.55 Additional findings included that patients receiving more than 90% of their care from VA obtained more preventive services than patients using primarily non-VA providers,119 that a variety of organizational factors are associated with better performance of breast and cervical cancer screening,116 and that women veterans told to have a mammogram and women who were regular VA users were more likely to get a mammogram than other patients.56
Preventive Care
Five articles were classified as dealing with preventive care67, 68, 122–124 and all assessed regional samples. Two concerned mammography and breast cancer screening,122, 123 1 each concerned coronary artery disease and osteoporosis, and 1 evaluated the impact of sexual assault on health behaviors. Findings included that women generally have difficulty applying risk information, though there is some correlation between the number of risk factors a women has for a condition and her concern about or estimation of her personal risk.68, 122–124
Tools or Measures
Among the other categories, we identified 7 that assessed specific tools or measures. These 7 used regional samples and, with the exception of 2 articles, assessed different tools or combinations of tools: the Trauma Questionnaire,125 the PTSD Checklist—Civilian Version,57, 58 the Gender Awareness Inventory,126 the Women's Wartime Stressor Scale,127 the AUDIT,59 and the TWEAK.60
Medical Treatments and Miscellaneous
Four studies were classified as health services research on various medical treatments: 1 each on hysterectomy,128 breast cancer surgery,129 hormone replacement therapy,130 and alcohol dependence.61 Two other studies could not be classified in any of the other categories and are grouped as “miscellaneous.”53, 131
Summary findings from the Health Services Research section include that women veterans are less likely to use VA outpatient services than men, and women veterans who do use VA outpatient services are poorer and more likely to be service connected but less likely to have private insurance than women who do not use VA; regular use of VA by women veterans is associated with greater receipt of preventive services and women veterans who use women's clinics are more satisfied than those using traditional primary care; and women veterans with PTSD appear to have worse health status and more medical conditions.
Psychiatric Conditions
PTSD
The largest number of studies—31—in the Psychiatric category pertained in some way to PTSD. Six utilized national samples and the remainder regional samples of women. The vast majority were observational studies. Six of the studies evaluated PTSD as it relates to health and functioning in different samples of women veterans, demonstrating that women with PTSD have poorer health status and health functioning,37, 65, 66, 72, 79, 82 more physical health symptoms and medical conditions65, 82 greater bodily pain,81 and more somatization132 than women without PTSD. Seven studies evaluated predictors of the development or severity of PTSD in women. Both war stress and sexual stress or sexual trauma were predictive of PTSD,9, 20, 36, 48, 49, 133 with 1 study indicating that sexual stress is 4 times as influential as war stress.9 Seven studies evaluated a variety of physiologic parameters and brain or neuronal characteristics of women with PTSD,85, 134–139 with some reporting differences in physiologic parameters or MRI findings between women with and without PTSD. Two studies evaluated aspects of treatment for PTSD,80, 113 with 1 demonstrating improved clinical outcomes for PTSD patients enrolled in specialized stress disorder treatment teams and the other finding no improvement related to continuity of care for women in a PTSD treatment program. One study found that Vietnam women with PTSD before the onset of the Gulf War had greater increases in re-experiencing symptoms as a result of the Gulf War140; and 1 study evaluated the validity of the “PTSD Checklist” in screening for PTSD and found that it had good test characteristics.58
Sexual Harassment, Abuse, and Assault
Nine studies assessed psychiatric aspects of sexual harassment, abuse, and assault.11–15, 17, 83, 84, 91 In a national sample of more than 3,000 women veterans using outpatient VA services, 23% reported a history of sexual assault while in the military and in this group the prevalence of depression was 3 times higher than in women without this history.11 Other regional or local samples of women also supported the finding that sexual harassment, abuse, and assault are common and that these experiences are associated with later psychiatric symptoms and diagnoses.12, 15, 14, 83, 84, 91
Prevalence/Characteristics of Psychiatric Conditions
Three studies assessed the prevalence and characteristics of psychiatric conditions in general.54, 141, 142 All 3 assessed local or regional samples. One study reported that the proportion of women attending a women's clinic who screened positive for at least 1 mental health disorder was 45%, and younger women and those with service-connected status were more likely than other women to screen positive for a psychiatric disorder.54 Another study reported an association between substance abuse and psychiatric disorders.142 A third study found that women veterans seen in psychiatric consultation in the emergency room, compared with men veterans, were more likely to be younger, divorced, to complain of anxiety or psychotic symptoms, and to carry diagnoses of depression and borderline personality.141
Services and Use
Three studies assessed services and use. One national sample found that women used less VA services than men because of less use of services by women with mental health disorders.111 Another regional study of veterans found that women used less services than men and that veterans with mental health diagnoses had fewer medical visits than other veterans.105 A survey of 91 Chiefs of Psychology found that the number of female-oriented services offered routinely was related to a variety of factors, including the number of female veterans and the number of psychologists on staff.100
Miscellaneous
Another 3 articles concerned a variety of topics in psychiatry. One was an RCT of dialectical therapy in 20 women meeting criteria for borderline personality, which reported significant improvements in some, but not all, outcome measures7 (described in greater detail previously). Another study evaluated the coping patterns of Vietnam era nurses,90 and a third study assessed the test characteristics of the Women's Wartime Stressor Scale.127
In summary, the majority of the studies in the Psychiatric section relate in some way to PTSD. Women veterans with PTSD seem to be significantly more impaired in multiple domains than women veterans without PTSD and both war stress and sexual stress can result in PTSD in women veterans.
DISCUSSION
The principal findings of our systematic review of women veterans' health literatures are that most studies are descriptive and observational in nature and they cluster in a few areas: the stress of military life, the health and performance of military/VA women, health services research, and psychiatric conditions. The preponderance of these studies relate in some way to the study of PTSD, and often, to the association of sexual trauma with PTSD in military and veteran women. While the derivation of patient samples varies greatly among these studies, most indicate that the prevalence of PTSD and sexual trauma is high and that their impact on women veterans is significant. We identified few papers that evaluated treatment programs or approaches for women patients suffering from PTSD related to sexual trauma; or that described prevention programs. While VA is currently supporting research in this area, it is clear that this represents a current gap in knowledge related to PTSD in military and veteran women.
Other notable gaps in the literature include very limited information on the prevalence of chronic diseases; women veterans' preferences and self-reported care needs; research on utilization patterns within VA and outside of VA; transitions from military to veteran status; and studies of the quality of care delivered to women veterans and how to improve quality.
There are a number of reasons why the women veterans' health research literature may be primarily concentrated in a few areas. The literature may be clustered in certain areas because of the inherent interests of those who have focused on women veteran research. Additionally, when considering the examples of sexual assault and PTSD that are directly related to military experiences, these become special problems for women veterans as compared with nonveterans and thus an important focus of VA researchers. The VA research agenda can, at times, be influenced by the specific interests of Congress and some of the research invariably reflects topics that were explored because of Congressionally mandated studies. Finally, because the literature suggests that women are more likely to utilize VA for mental health issues, this may also have biased the direction of investigations into women veteran health problems.
The primary limitation of this systematic review is the likelihood that there are additional articles about women veterans health that we did not identify. While “missing articles” is a concern for all systematic reviews, it is a greater concern for this review because we lacked sensitive search terms for computerized databases. We solicited input from many leading researchers in the field and believe that it is unlikely that we have missed a large proportion of relevant studies. Nevertheless, one goal in publishing this review is to encourage submission to us of additional articles that we have not identified, so that they may be included in our database and made available to other researchers in the field.
In summary, we identified a substantial body of literature on women veterans' health, but most of it is clustered in only a few areas of importance. In addition to maintaining momentum in the important work on PTSD, new research should be stimulated in other topic areas of recognized importance to women veterans.
Voices of Women Veterans (continued)
VA HEALTH CARE EXPERIENCES
“I did not learn of VA health care until many years after active duty. I wish I had checked into it before. It has made a difference in my health.”
“I was unaware that healthcare was available for women veterans until 10 years ago.”
“In the…VA system, I felt like I was not wanted. The VA rep kept giving me the runaround …a rep helped me overcome my fear of the VA system. From then, I'm cared for better than any civilian doctors I went to.”
“I haven't attempted to get health care at the VA until 3 years ago. My prescriptions went up so much I had to turn to the vets. My experiences are very good. Everyone here is very thorough and compassionate.”
“Initially, VA was a nightmare. I stayed away for years. No idea of women's issues. Very pleased with current experience past 2 months.”
“I have severe PTSD. It causes isolation, withdrawal from people. I cannot have relationships, do not get along well with people. Health care through the VA was impossible for decades. The VA said they didn't take women. Years later…I asked again. They said my [monthly] income…was too much. Some male veterans at the vet center encouraged me to persist. They already knew I had PTSD. I didn't. It was delayed PTSD. It was a stressful process.”
Supplementary Material
The following supplementary material is available for this article online at http://www.blackwell-synergy.com:
Evidence Tables of Stress of Military Life Studies
Evidence Tables of Health and Performance
Evidence Tables of Health Services Research/Quality of Care
Psychiatric Evidence Tables
Evidence Tables of Different Gender Manifestations of Emotional Disorders
Evidence Tables of Health Behaviors, Prevention and Epidemiology
Evidence Tables of Clinical Conditions
Evidence Tables of Gynecological Conditions
REFERENCES
- 1.Haseltine FP, Jacobson BG. Women's Health Research: A Medical and Policy Primer. Washington DC: Health Press International; 1997. [Google Scholar]
- 2.Norwood AE, Ursano RJ, Gabbay FH. Health effects of the stressors of extreme environments on military women. Mil Med. 1997;162:643–8. [PubMed] [Google Scholar]
- 3.Weiss TW. Improvements in VA health services for women veterans. Women Health. 1995;23:1–12. doi: 10.1300/J013v23n02_01. [DOI] [PubMed] [Google Scholar]
- 4.Bullman TA, Kang HK. The effects of mustard gas, ionizing radiation, herbicides, trauma, and oil smoke on US military personnel: the results of veteran studies. Annu Rev Public Health. 1994;15:69–90. doi: 10.1146/annurev.pu.15.050194.000441. [DOI] [PubMed] [Google Scholar]
- 5.Murphy F, Browne D, Mather S, Scheele H, Hyams KC. Women in the Persian Gulf War: health care implications for active duty troops and veterans. Mil Med. 1997;162:656–60. [PubMed] [Google Scholar]
- 6.Dalessandri KM, Cooper M, Rucker T. Effect of mammography outreach in women veterans. West J Med. 1998;169:150–2. [PMC free article] [PubMed] [Google Scholar]
- 7.Koons CR, Robins CJ, Tweed JL, et al. Efficacy of dialectical behavior therapy in women veterans with borderline personality disorder. Behav Ther. 2001;32:371–90. [Google Scholar]
- 8.Coyle BS, Wolan DL, Van Horn AS. The prevalence of physical and sexual abuse in women veterans seeking care at a Veterans Affairs Medical Center. Mil Med. 1996;161:588–93. [PubMed] [Google Scholar]
- 9.Fontana A, Rosenheck R. Duty-related and sexual stress in the etiology of PTSD among women veterans who seek treatment. Psychiatr Serv. 1998;49:658–62. doi: 10.1176/ps.49.5.658. [DOI] [PubMed] [Google Scholar]
- 10.Frayne SM, Skinner KM, Sullivan LM, et al. Medical profile of women Veterans Administration outpatients who report a history of sexual assault occurring while in the military. J Womens Health Gend Based Med. 1999;8:835–45. doi: 10.1089/152460999319156. [DOI] [PubMed] [Google Scholar]
- 11.Hankin CS, Skinner KM, Sullivan LM, Miller DR, Frayne S, Tripp TJ. Prevalence of depressive and alcohol abuse symptoms among women VA outpatients who report experiencing sexual assault while in the military. J Trauma Stress. 1999;12:601–12. doi: 10.1023/A:1024760900213. [DOI] [PubMed] [Google Scholar]
- 12.Butterfield MI, McIntyre LM, Stechuchak KM, Nanda K, Bastian LA. Mental disorder symptoms in veteran women: impact of physical and sexual assault. J Am Women's Med Assoc. 1998;53:198–200. [Google Scholar]
- 13.Davis TM, Wood PS. Substance abuse and sexual trauma in a female veteran population. J Subst Abuse Treat. 1999;16:123–7. doi: 10.1016/s0740-5472(98)00014-2. [DOI] [PubMed] [Google Scholar]
- 14.Read JP, Stern AL, Wolfe J, Ouimette PC. Use of a screening instrument in women's health care: detecting relationships among victimization history, psychological distress, and medical complaints. Women Health. 1997;25:1–17. doi: 10.1300/J013v25n03_01. [DOI] [PubMed] [Google Scholar]
- 15.DeRoma VM, Root LP, Smith BS., Jr Socioenvironmental context of sexual trauma and well-being of women veterans. Mil Med. 2003;168:399–403. [PubMed] [Google Scholar]
- 16.Harned MS, Ormerod AJ, Palmieri PA, Collinsworth LL, Reed M. Sexual assault and other types of sexual harassment by workplace personnel: a comparison of antecedents and consequences. J Occup Health Psychol. 2002;7:174–88. doi: 10.1037//1076-8998.7.2.174. [DOI] [PubMed] [Google Scholar]
- 17.Chang BH, Skinner KM, Boehmer U. Religion and mental health among women veterans with sexual assault experience. Int J Psychiatry Med. 2001;31:77–95. doi: 10.2190/0NQA-YAJ9-W0AM-YB3P. [DOI] [PubMed] [Google Scholar]
- 18.Sadler AG, Booth BM, Nielson D, Doebbeling BN. Health-related consequences of physical and sexual violence: women in the military. Obstet Gynecol. 2000;96:473–80. doi: 10.1016/s0029-7844(00)00919-4. [DOI] [PubMed] [Google Scholar]
- 19.Sadler AG, Booth BM, Cook BL, Torner JC, Doebbeling BN. The military environment: risk factors for women's non-fatal assaults. J Occup Environ Med. 2001;43:325–34. doi: 10.1097/00043764-200104000-00007. [DOI] [PubMed] [Google Scholar]
- 20.Wolfe J, Sharkansky E, Read J, Dawson R, Martin J, Ouimette PC. Sexual harassment and assault as predictors of PTSD symptomatology among US female Persian Gulf War military personnel. J Interpers Violence. 1998;13:40–7. [Google Scholar]
- 21.Sadler AG, Booth BM, Cook BL, Doebbeling BN. Factors associated with women's risk of rape in the military environment. Am J Ind Med. 2003;43:262–73. doi: 10.1002/ajim.10202. [DOI] [PubMed] [Google Scholar]
- 22.Baker DG, Boat BW, Grinvalsky HT, Geracioti TD., Jr Interpersonal trauma and animal-related experiences in female and male military veterans: implications for program development. Mil Med. 1998;163:20–5. [PubMed] [Google Scholar]
- 23.Sadler AG, Booth BM, Mengeling MA, Doebbeling BN. Life span and repeated violence against women during military service: effects on health status and outpatient utilization. J Womens Health (Larchmt) 2004;13:799–811. doi: 10.1089/jwh.2004.13.799. [DOI] [PubMed] [Google Scholar]
- 24.Skinner KM, Kressin N, Frayne S, et al. The prevalence of military sexual assault among female Veterans Administration outpatients. J Interpers Violence. 2000;15:291–310. [Google Scholar]
- 25.Harned MS, Fitzgerald LF. Understanding a link between sexual harassment and eating disorder symptoms: a mediational analysis. J Consult Clin Psychol. 2002;70:1170–81. doi: 10.1037//0022-006x.70.5.1170. [DOI] [PubMed] [Google Scholar]
- 26.Wolfe J, Proctor SP, Davis JD, Borgos MS, Friedman MJ. Health symptoms reported by Persian Gulf War veterans two years after return. Am J Ind Med. 1998;33:104–13. doi: 10.1002/(sici)1097-0274(199802)33:2<104::aid-ajim2>3.0.co;2-y. [DOI] [PubMed] [Google Scholar]
- 27.Erickson DJ, Wolfe J, King DW, King LA, Sharkansky EJ. Posttraumatic stress disorder and depression symptomatology in a sample of Gulf War veterans: a prospective analysis. J Consult Clin Psychol. 2001;69:41–9. doi: 10.1037//0022-006x.69.1.41. [DOI] [PubMed] [Google Scholar]
- 28.King DW, King LA, Erickson DJ, Huang MT, Sharkansky EJ, Wolfe J. Posttraumatic stress disorder and retrospectively reported stressor exposure: a longitudinal prediction model. J Abnorm Psychol. 2000;109:624–33. doi: 10.1037//0021-843x.109.4.624. [DOI] [PubMed] [Google Scholar]
- 29.Wolfe J, Erickson DJ, Sharkansky EJ, King DW, King LA. Course and predictors of posttraumatic stress disorder among Gulf War veterans: a prospective analysis. J Consult Clin Psychol. 1999;67:520–8. doi: 10.1037//0022-006x.67.4.520. [DOI] [PubMed] [Google Scholar]
- 30.Sharkansky EJ, King DW, King LA, Wolfe J, Erickson DJ, Stokes LR. Coping with Gulf War combat stress: mediating and moderating effects. J Abnorm Psychol. 2000;109:188–97. [PubMed] [Google Scholar]
- 31.Wagner AW, Wolfe J, Rotnitsky A, Proctor SP, Erickson DJ. An investigation of the impact of posttraumatic stress disorder on physical health. J Trauma Stress. 2000;13:41–55. doi: 10.1023/A:1007716813407. [DOI] [PubMed] [Google Scholar]
- 32.Wolfe J, Brown P, Kelley JM. Reassessing war stress: exposure and the Persian Gulf War. J Soc Issues. 1993;49:15–31. [Google Scholar]
- 33.Stuart JA, Murray KM, Ursano RJ, Wright KM. The Department of Defense's Persian Gulf War registry year 2000: an examination of veterans' health status. Mil Med. 2002;167:121–8. [PubMed] [Google Scholar]
- 34.Stuart JA, Ursano RJ, Fullerton CS, Norwood AE, Murray K. Belief in exposure to terrorist agents: reported exposure to nerve or mustard gas by Gulf War veterans. J Nerv Ment Dis. 2003;191:431–6. doi: 10.1097/01.NMD.0000081634.28356.6B. [DOI] [PubMed] [Google Scholar]
- 35.Thomas TL, Kang HK, Dalager NA. Mortality among women Vietnam veterans, 1973–1987. Am J Epidemiol. 1991;134:973–80. doi: 10.1093/oxfordjournals.aje.a116182. [DOI] [PubMed] [Google Scholar]
- 36.Fontana A, Schwartz LS, Rosenheck R. Posttraumatic stress disorder among female Vietnam veterans: a causal model of etiology. Am J Public Health. 1997;87:169–75. doi: 10.2105/ajph.87.2.169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wolfe J, Schnurr PP, Brown PJ, Furey J. Posttraumatic stress disorder and war-zone exposure as correlates of perceived health in female Vietnam War veterans. J Consult Clin Psychol. 1994;62:1235–40. doi: 10.1037//0022-006x.62.6.1235. [DOI] [PubMed] [Google Scholar]
- 38.King DW, King LA, Foy DW, Gudanowski DM. Prewar factors in combat-related posttraumatic stress disorder: structural equation modeling with a national sample of female and male Vietnam veterans. J Consult Clin Psychol. 1996;64:520–31. doi: 10.1037//0022-006x.64.3.520. [DOI] [PubMed] [Google Scholar]
- 39.Schnurr PP, Lunney CA, Sengupta A. Risk factors for the development versus maintenance of posttraumatic stress disorder. J Trauma Stress. 2004;17:85–95. doi: 10.1023/B:JOTS.0000022614.21794.f4. [DOI] [PubMed] [Google Scholar]
- 40.King LA, King DW, Fairbank JA, Keane TM, Adams GA. Resilience-recovery factors in post-traumatic stress disorder among female and male Vietnam veterans: hardiness, postwar social support, and additional stressful life events. J Pers Soc Psychol. 1998;74:420–34. doi: 10.1037//0022-3514.74.2.420. [DOI] [PubMed] [Google Scholar]
- 41.King DW, King LA, Foy DW, Keane TM, Fairbank JA. Posttraumatic stress disorder in a national sample of female and male Vietnam veterans: risk factors, war-zone stressors, and resilience-recovery variables. J Abnorm Psychol. 1999;108:164–70. doi: 10.1037//0021-843x.108.1.164. [DOI] [PubMed] [Google Scholar]
- 42.King DW, King LA, Gudanowski DM, Vreven DL. Alternative representations of war zone stressors: relationships to posttraumatic stress disorder in male and female Vietnam veterans. J Abnorm Psychol. 1995;104:184–95. doi: 10.1037//0021-843x.104.1.184. [DOI] [PubMed] [Google Scholar]
- 43.Taft CT, Stern AS, King LA, King DW. Modeling physical health and functional health status: the role of combat exposure, posttraumatic stress disorder, and personal resource attributes. J Trauma Stress. 1999;12:3–23. doi: 10.1023/A:1024786030358. [DOI] [PubMed] [Google Scholar]
- 44.Jordan BK, Schlenger WE, Hough R, et al. Lifetime and current prevalence of specific psychiatric disorders among Vietnam veterans and controls. Arch Gen Psychiatry. 1991;48:207–15. doi: 10.1001/archpsyc.1991.01810270019002. [DOI] [PubMed] [Google Scholar]
- 45.Baker DG, Boat BW, Grinvalsky HT, Geracioti TD., Jr Interpersonal trauma and animal-related experiences in female and male military veterans: implications for program development. Mil Med. 1998;163:20–5. [PubMed] [Google Scholar]
- 46.Hourani LL, Yuan H, Bray RM. Psychosocial and health correlates of types of traumatic event exposures among U.S. military personnel. Mil Med. 2003;168:736–43. [PubMed] [Google Scholar]
- 47.Pereira A. Combat trauma and the diagnosis of post-traumatic stress disorder in female and male veterans. Mil Med. 2002;167:23–7. [PubMed] [Google Scholar]
- 48.Kang HK, Natelson BH, Mahan CM, Lee KY, Murphy FM. Post-traumatic stress disorder and chronic fatigue syndrome-like illness among Gulf War veterans: a population-based survey of 30,000 veterans. Am J Epidemiol. 2003;157:141–8. doi: 10.1093/aje/kwf187. [DOI] [PubMed] [Google Scholar]
- 49.Ouimette PC, Wolfe J, Chrestman KR. Characteristics of posttraumatic stress disorder-alcohol abuse comorbidity in women. J Subst Abuse. 1996;8:335–46. doi: 10.1016/s0899-3289(96)90188-1. [DOI] [PubMed] [Google Scholar]
- 50.Pierce PF, Antonakos C, Deroba BA. Health care utilization and satisfaction concerning gender-specific health problems among military women. Mil Med. 1999;164:98–102. [PubMed] [Google Scholar]
- 51.Stern A, Wolfe J, Daley J, Zaslavsky A, Roper SF, Wilson K. Changing demographic characteristics of women veterans: results from a national sample. Mil Med. 2000;165:773–80. [PubMed] [Google Scholar]
- 52.Leda C, Rosenheck R, Gallup P. Mental illness among homeless female veterans. Hosp Community Psychiatry. 1992;43:1026–8. doi: 10.1176/ps.43.10.1026. [DOI] [PubMed] [Google Scholar]
- 53.Gamache G, Rosenheck R, Tessler R. Overrepresentation of women veterans among homeless women. Am J Public Health. 2003;93:1132–6. doi: 10.2105/ajph.93.7.1132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Bader G, Ragsdale KG, Franchina JJ. Screening for mental illness in a Veterans Affairs women's health clinic. Psychiatr Serv. 2001;52:1521–2. doi: 10.1176/appi.ps.52.11.1521. [DOI] [PubMed] [Google Scholar]
- 55.Bean-Mayberry BA, Chang CC, McNeil MA, Whittle J, Hayes PM, Scholle SH. Patient satisfaction in women's clinics versus traditional primary care clinics in the Veterans Administration. J Gen Intern Med. 2003;18:175–81. doi: 10.1046/j.1525-1497.2003.20512.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Hynes DM, Bastian LA, Rimer BK, Sloane R, Feussner JR. Predictors of mammography use among women veterans. J Womens Health. 1998;7:239–47. doi: 10.1089/jwh.1998.7.239. [DOI] [PubMed] [Google Scholar]
- 57.Lang AJ, Laffaye C, Satz LE, Dresselhaus TR, Stein MB. Sensitivity and specificity of the PTSD checklist in detecting PTSD in female veterans in primary care. J Trauma Stress. 2003;16:257–64. doi: 10.1023/A:1023796007788. [DOI] [PubMed] [Google Scholar]
- 58.Dobie DJ, Kivlahan DR, Maynard C, et al. Screening for post-traumatic stress disorder in female Veteran's Affairs patients: validation of the PTSD checklist. Gen Hosp Psychiatry. 2002;24:367–74. doi: 10.1016/s0163-8343(02)00207-4. [DOI] [PubMed] [Google Scholar]
- 59.Bradley KA, Bush KR, Epler AJ, et al. Two brief alcohol-screening tests from the alcohol use disorders identification test (AUDIT): validation in a female Veterans Affairs patient population. Arch Intern Med. 2003;163:821–9. doi: 10.1001/archinte.163.7.821. [DOI] [PubMed] [Google Scholar]
- 60.Bush KR, Kivlahan DR, Davis TM, et al. The TWEAK is weak for alcohol screening among female Veterans Affairs outpatients. Alcohol Clin Exp Res. 2003;27:1971–8. doi: 10.1097/01.ALC.0000099262.50094.98. [DOI] [PubMed] [Google Scholar]
- 61.Ross R, Fortney J, Lancaster B, Booth BM. Age, ethnicity, and comorbidity in a national sample of hospitalized alcohol-dependent women veterans. Psychiatr Serv. 1998;49:663–8. doi: 10.1176/ps.49.5.663. [DOI] [PubMed] [Google Scholar]
- 62.Ouimette P, Wolfe J, Daley J, Gima K. Use of VA health care services by women veterans: findings from a national sample. Women Health. 2003;38:77–91. doi: 10.1300/J013v38n02_06. [DOI] [PubMed] [Google Scholar]
- 63.Hoff RA, Rosenheck RA. The use of VA and non-VA mental health services by female veterans. Med Care. 1998;36:1524–33. doi: 10.1097/00005650-199811000-00002. [DOI] [PubMed] [Google Scholar]
- 64.Washington DL, Caffrey C, Goldzweig C, Simon B, Yano EM. Availability of comprehensive women's health care through Department of Veterans Affairs Medical Center. Womens Health Issues. 2003;13:50–4. doi: 10.1016/s1049-3867(02)00195-0. [DOI] [PubMed] [Google Scholar]
- 65.Frayne SM, Seaver MR, Loveland S, et al. Burden of medical illness in women with depression and posttraumatic stress disorder. Arch Intern Med. 2004;164:1306–12. doi: 10.1001/archinte.164.12.1306. [DOI] [PubMed] [Google Scholar]
- 66.Zatzick DF, Weiss DS, Marmar CR, et al. Post-traumatic stress disorder and functioning and quality of life outcomes in female Vietnam veterans. Mil Med. 1997;162:661–5. [PubMed] [Google Scholar]
- 67.Lang AJ, Rodgers CS, Laffaye C, Satz LE, Dresselhaus TR, Stein MB. Sexual trauma, posttraumatic stress disorder, and health behavior. Behav Med. 2003;28:150–8. doi: 10.1080/08964280309596053. [DOI] [PubMed] [Google Scholar]
- 68.Biswas MS, Calhoun PS, Bosworth HB, Bastian LA. Are women worrying about heart disease? Womens Health Issues. 2002;12:204–11. doi: 10.1016/s1049-3867(02)00136-6. [DOI] [PubMed] [Google Scholar]
- 69.Pierce PF. Physical and emotional health of Gulf War veteran women. Aviat Space Environ Med. 1997;68:317–21. [PubMed] [Google Scholar]
- 70.Engel CC, Jr, Ursano R, Magruder C, et al. Psychological conditions diagnosed among veterans seeking Department of Defense Care for Gulf War-related health concerns. J Occup Environ Med. 1999;41:384–92. doi: 10.1097/00043764-199905000-00006. [DOI] [PubMed] [Google Scholar]
- 71.Gray GC, Reed RJ, Kaiser KS, Smith TC, Gastanaga VM. Self-reported symptoms and medical conditions among 11,868 Gulf War-era veterans: the Seabee Health Study. Am J Epidemiol. 2002;155:1033–44. doi: 10.1093/aje/155.11.1033. [DOI] [PubMed] [Google Scholar]
- 72.Kimerling R, Clum GA, Wolfe J. Relationships among trauma exposure, chronic posttraumatic stress disorder symptoms, and self-reported health in women: replication and extension. J Trauma Stress. 2000;13:115–28. doi: 10.1023/A:1007729116133. [DOI] [PubMed] [Google Scholar]
- 73.Fontana A, Litz B, Rosenheck R. Impact of combat and sexual harassment on the severity of posttraumatic stress disorder among men and women peacekeepers in Somalia. J Nerv Ment Dis. 2000;188:163–9. doi: 10.1097/00005053-200003000-00006. [DOI] [PubMed] [Google Scholar]
- 74.Litz BT, Orsillo SM, Friedman M, Ehlich P, Batres A. Posttraumatic stress disorder associated with peacekeeping duty in Somalia for U.S. military personnel. Am J Psychiatry. 1997;154:178–84. doi: 10.1176/ajp.154.2.178. [DOI] [PubMed] [Google Scholar]
- 75.Kirstein L. Female soldiers' social adjustment. Mil Med. 1978;143:695–7. [PubMed] [Google Scholar]
- 76.Whitlock EP, Ferry LH, Burchette RJ, Abbey D. Smoking characteristics of female veterans. Addict Behav. 1995;20:409–26. doi: 10.1016/0306-4603(95)00011-z. [DOI] [PubMed] [Google Scholar]
- 77.Skelton WP, III, Skelton NK. Women as prisoners of war. Mil Med. 1995;160:558–60. [PubMed] [Google Scholar]
- 78.Ouimette P, Cronkite R, Henson BR, Prins A, Gima K, Moos RH. Posttraumatic stress disorder and health status among female and male medical patients. J Trauma Stress. 2004;17:1–9. doi: 10.1023/B:JOTS.0000014670.68240.38. [DOI] [PubMed] [Google Scholar]
- 79.Butterfield MI, Forneris CA, Feldman ME, Beckham JC. Hostility and functional health status in women veterans with and without posttraumatic stress disorder: a preliminary study. J Trauma Stress. 2000;13:735–41. doi: 10.1023/A:1007874620024. [DOI] [PubMed] [Google Scholar]
- 80.Fontana A, Rosenheck R. Women under stress II: evaluation of the clinical performance of the Department of Veterans Affairs women's stress disorder treatment teams. National Center for PTSD. 2002 [Google Scholar]
- 81.Asmundson GJ, Wright KD, Stein MB. Pain and PTSD symptoms in female veterans. Eur J Pain. 2004;8:345–50. doi: 10.1016/j.ejpain.2003.10.008. [DOI] [PubMed] [Google Scholar]
- 82.Dobie DJ, Kivlahan DR, Maynard C, Bush KR, Davis TM, Bradley KA. Posttraumatic stress disorder in female veterans: association with self-reported health problems and functional impairment. Arch Intern Med. 2004;164:394–400. doi: 10.1001/archinte.164.4.394. [DOI] [PubMed] [Google Scholar]
- 83.Stein MB, Lang AJ, Laffaye C, Satz LE, Lenox RJ, Dresselhaus TR. Relationship of sexual assault history to somatic symptoms and health anxiety in women. Gen Hosp Psychiatry. 2004;26:178–83. doi: 10.1016/j.genhosppsych.2003.11.003. [DOI] [PubMed] [Google Scholar]
- 84.Suris A, Lind L, Kashner TM, Borman PD, Petty F. Sexual assault in women veterans: an examination of PTSD risk, health care utilization, and cost of care. Psychosom Med. 2004;66:749–56. doi: 10.1097/01.psy.0000138117.58559.7b. [DOI] [PubMed] [Google Scholar]
- 85.Forneris CA, Butterfield MI, Bosworth HB. Physiological arousal among women veterans with and without posttraumatic stress disorder. Mil Med. 2004;169:307–12. doi: 10.7205/milmed.169.4.307. [DOI] [PubMed] [Google Scholar]
- 86.Skinner K, Sullivan LM, Tripp TJ, et al. Comparing the health status of male and female veterans who use VA health care: results from the VA Women's Health Project. Women Health. 1999;29:17–33. doi: 10.1300/J013v29n04_02. [DOI] [PubMed] [Google Scholar]
- 87.Bradley KA, Bush KR, Davis TM, et al. Binge drinking among female Veterans Affairs patients: prevalence and associated risks. Psychol Addict Behav. 2001;15:297–305. doi: 10.1037//0893-164x.15.4.297. [DOI] [PubMed] [Google Scholar]
- 88.Carney CP, Sampson TR, Voelker M, Woolson R, Thorne P, Doebbeling BN. Women in the Gulf War: combat experience, exposures, and subsequent health care use. Mil Med. 2003;168:654–61. [PubMed] [Google Scholar]
- 89.Willer JK, Grossman LS. Mental health care needs of female veterans. Psychiatr Serv. 1995;46:938–40. doi: 10.1176/ps.46.9.938. [DOI] [PubMed] [Google Scholar]
- 90.Leon G, Ben-Porath Y, Hjemboe S. Coping patterns and current functioning in a group of Vietnam and Vietnam-Era nurses. J Soc Clin Psychol. 1990;9:334–53. [Google Scholar]
- 91.Butterfield M, Bastian L, McIntyre L, Kroons C, Vollmer M, Burns B. Screening for mental disorders and history of sexual trauma and battering among women using primary health care services. JCOM. 1996;3 [Google Scholar]
- 92.David WS, Cotton AJ, Simpson TL, Weitlauf JC. Making a case for personal safety: perceptions of vulnerability and desire for self-defense training among female veterans. J Interpers Violence. 2004;19:991–1001. doi: 10.1177/0886260504268001. [DOI] [PubMed] [Google Scholar]
- 93.Gilhooly PE, Ottenweller JE, Lange G, Tiersky L, Natelson BH. Chronic fatigue and sexual dysfunction in female Gulf War veterans. J Sex Marital Ther. 2001;27:483–7. doi: 10.1080/713846825. [DOI] [PubMed] [Google Scholar]
- 94.Ashton CM, Petersen NJ, Wray NP, Yu HJ. The Veterans Affairs medical care system: hospital and clinic utilization statistics for 1994. Med Care. 1998;36:793–803. doi: 10.1097/00005650-199806000-00003. [DOI] [PubMed] [Google Scholar]
- 95.Guihan M, Weaver FM, Cowper DC, Nydam T, Miskevics S. Using Department of Veterans Affairs Administrative databases to examine long-term care utilization for men and women veterans. J Med Syst. 1999;23:201–18. doi: 10.1023/a:1020571504693. [DOI] [PubMed] [Google Scholar]
- 96.Hoff RA, Rosenheck RA. Utilization of mental health services by women in a male-dominated environment: the VA experience. Psychiatr Serv. 1997;48:1408–14. doi: 10.1176/ps.48.11.1408. [DOI] [PubMed] [Google Scholar]
- 97.Romeis JC, Gillespie KN, Thorman KE. Female veterans' use of health care services. Med Care. 1988;26:589–95. doi: 10.1097/00005650-198806000-00007. [DOI] [PubMed] [Google Scholar]
- 98.Romeis JC, Gillespie KN, Virgo KS, Thorman KE. Female veterans' and nonveterans' use of health care services. Med Care. 1991;29:932–6. doi: 10.1097/00005650-199109000-00013. [DOI] [PubMed] [Google Scholar]
- 99.Sajatovic M, Vernon L, Semple W. Clinical characteristics and health resource use of men and women veterans with serious mental illness. Psychiatr Serv. 1997;48:1461–3. doi: 10.1176/ps.48.11.1461. [DOI] [PubMed] [Google Scholar]
- 100.Schuler MP, Barclay A, Harrison B, Larson P. Psychological services offered to female veterans. J Clin Psychol. 1986;42:668–75. doi: 10.1002/1097-4679(198607)42:4<668::aid-jclp2270420424>3.0.co;2-i. [DOI] [PubMed] [Google Scholar]
- 101.Weiss TW, Ashton CM. Access of women veterans to Veterans Affairs hospitals. Women Health. 1994;21:23–38. doi: 10.1300/J013v21n02_02. [DOI] [PubMed] [Google Scholar]
- 102.Bean-Mayberry B, Chang C, McNeil M, Hayes P, Hudson Scholle S. Comprehensive care for women veterans: indicators of dual use of VA and non-VA providers. J Am Women's Med Assoc. 2004;59:192–7. [PubMed] [Google Scholar]
- 103.Murdoch M, Hodges J, Cowper D, Fortier L, van Ryn M. Racial disparities in VA service connection for posttraumatic stress disorder disability. Med Care. 2003;41:536–49. doi: 10.1097/01.MLR.0000053232.67079.A5. [DOI] [PubMed] [Google Scholar]
- 104.Westermeyer J, Canive J, Thuras P, Chesness D, Thompson J. Perceived barriers to VA mental health care among Upper Midwest American Indian veterans: description and associations. Med Care. 2002;40:I62–71. doi: 10.1097/00005650-200201001-00008. [DOI] [PubMed] [Google Scholar]
- 105.Cradock-O'Leary J, Young AS, Yano EM, Wang M, Lee ML. Use of general medical services by VA patients with psychiatric disorders. Psychiatr Serv. 2002;53:874–8. doi: 10.1176/appi.ps.53.7.874. [DOI] [PubMed] [Google Scholar]
- 106.Murdoch M, Nelson DB, Fortier L. Time, gender, and regional trends in the application for service-related post-traumatic stress disorder disability benefits, 1980–1998. Mil Med. 2003;168:662–70. [PubMed] [Google Scholar]
- 107.Murdoch M, Hodges J, Hunt C, Cowper D, Kressin N, O'Brien N. Gender differences in service connection for PTSD. Med Care. 2003;41:950–61. doi: 10.1097/00005650-200308000-00008. [DOI] [PubMed] [Google Scholar]
- 108.Huynh-Hohnbaum A, Damron-Rodriguez J, Washington D, Villa V, Harada N. Exploring the diversity of women veterans' Identity to improve the delivery of veterans' health services. AFFILIA. 2003;18:165–76. [Google Scholar]
- 109.Bosworth HB, Butterfield MI, Stechuchak KM, Bastian LA. The relationship between self-rated health and health care service use among women veterans in a primary care clinic. Womens Health Issues. 2000;10:278–85. doi: 10.1016/s1049-3867(00)00056-6. [DOI] [PubMed] [Google Scholar]
- 110.Yano EM, Washington DL, Goldzweig C, Caffrey C, Turner C. The organization and delivery of women's health care in Department of Veterans Affairs Medical Center. Womens Health Issues. 2003;13:55–61. doi: 10.1016/s1049-3867(02)00198-6. [DOI] [PubMed] [Google Scholar]
- 111.Hoff RA, Rosenheck RA. Female veterans' use of Department of Veterans Affairs health care services. Med Care. 1998;36:1114–9. doi: 10.1097/00005650-199807000-00017. [DOI] [PubMed] [Google Scholar]
- 112.Forneris CA, Bosworth HB, Butterfield MI. Outpatient care use among female veterans: differences between mental health and non-mental health users. Mil Med. 2002;167:10–3. [PubMed] [Google Scholar]
- 113.Greenberg GA, Fontana A, Rosenheck RA. Continuity and intensity of care among women receiving outpatient care for PTSD. Psychiatr Q. 2004;75:165–81. doi: 10.1023/b:psaq.0000019757.85605.fd. [DOI] [PubMed] [Google Scholar]
- 114.Sunshine JH, Witkin MJ, Atay JE, Manderscheid RW. Mental health services of the Veterans Administration, United States, 1986. Ment Health Stat Note. 1991;197:1–17. doi: 10.1037/e477942004-001. [DOI] [PubMed] [Google Scholar]
- 115.Grossman LS, Willer JK, Stovall JG, McRae SG, Maxwell S, Nelson R. Underdiagnosis of PTSD and substance use disorders in hospitalized female veterans. Psychiatr Serv. 1997;48:393–5. doi: 10.1176/ps.48.3.393. [DOI] [PubMed] [Google Scholar]
- 116.Goldzweig CL, Parkerton PH, Washington DL, Lanto AB, Yano EM. Primary care practice and facility quality orientation: influence on breast and cervical cancer screening rates. Am J Manag Care. 2004;10:265–72. [PubMed] [Google Scholar]
- 117.Hoff RA, Rosenheck RA, Materko M, Wilson NJ. The quality of VA mental health services. Adm Policy Ment Health. 1998;26:45–56. doi: 10.1023/a:1021217420121. [DOI] [PubMed] [Google Scholar]
- 118.Kressin NR, Skinner K, Sullivan L, et al. Patient satisfaction with Department of Veterans Affairs health care: do women differ from men. Mil Med. 1999;164:283–8. [PubMed] [Google Scholar]
- 119.Rabiner DJ, Branch LG, Sullivan RJ. The receipt of prevention services by veterans using VA versus non-VA facilities. Prev Med. 1998;27:690–6. doi: 10.1006/pmed.1998.0345. [DOI] [PubMed] [Google Scholar]
- 120.Turpin RS, Darcy LA, Weaver FM, Kruse K. Assessing health care delivery to male versus female veterans. Women Health. 1992;18:81–95. doi: 10.1300/J013v18n01_04. [DOI] [PubMed] [Google Scholar]
- 121.Rothman GH. Needs of female patients in a veterans psychiatric hospital. Soc Work. 1984;29:380–5. doi: 10.1093/sw/29.4.380. [DOI] [PubMed] [Google Scholar]
- 122.Schwartz LM, Woloshin S, Black WC, Welch HG. The role of numeracy in understanding the benefit of screening mammography. Ann Intern Med. 1997;127:966–72. doi: 10.7326/0003-4819-127-11-199712010-00003. [DOI] [PubMed] [Google Scholar]
- 123.Woloshin S, Schwartz LM, Black WC, Welch HG. Women's perceptions of breast cancer risk: how you ask matters. Med Decis Making. 1999;19:221–9. doi: 10.1177/0272989X9901900301. [DOI] [PubMed] [Google Scholar]
- 124.Osborn B, Couchman GM, Seigler IC, Bastian LA. Osteoporosis risk factors: association with use of HRT and with worry about osteoporosis. Women's Health Issues. 1999;9:278–85. [Google Scholar]
- 125.McIntyre LM, Butterfield MI, Nanda K, et al. Validation of a trauma questionnaire in veteran women. J Gen Intern Med. 1999;14:186–9. doi: 10.1046/j.1525-1497.1999.00311.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Salgado DM, Vogt DS, King LA, King DW. Gender Awareness Inventory-VA: a measure of ideology, sensitivity, and knowlege related to women veterans' health care. Sex Roles. 2002;46:247–62. [Google Scholar]
- 127.Wolfe J, Brown P, Furey J, Levin K. Development of a wartime stressor scale for women. Psychological Assessment. 1993;5:330–335. [Google Scholar]
- 128.Weaver F, Hynes D, Goldberg JM, Khuri S, Daley J, Henderson W. Hysterectomy in Veterans Affairs medical centers. Obstet Gynecol. 2001;97:880–4. doi: 10.1016/s0029-7844(01)01350-3. [DOI] [PubMed] [Google Scholar]
- 129.Hynes DM, Weaver F, Morrow M, et al. Breast cancer surgery trends and outcomes: results from a National Department of Veterans Affairs study. J Am Coll Surg. 2004;198:707–16. doi: 10.1016/j.jamcollsurg.2004.01.027. [DOI] [PubMed] [Google Scholar]
- 130.Roumie CL, Grogan EL, Falbe W, et al. A three-part intervention to change the use of hormone replacement therapy in response to new evidence. Ann Intern Med. 2004;141:118–25. doi: 10.7326/0003-4819-141-2-200407200-00010. [DOI] [PubMed] [Google Scholar]
- 131.Schumm W, Jurich A, Bollman S, Sanders D, Castelo C, Webb F. Understanding mail survey response rates among female reserve component veterans serving during the persian gulf war. Psychol Rep. 1999;85:653–64. doi: 10.2466/pr0.2000.87.3.859. [DOI] [PubMed] [Google Scholar]
- 132.Escalona R, Achilles G, Waitzkin H, Yager J. PTSD and somatization in women treated at a VA primary care clinic. Psychosomatics. J Consultation Liaison Psychiatry. 2004;45:291–96. doi: 10.1176/appi.psy.45.4.291. [DOI] [PubMed] [Google Scholar]
- 133.Norman EM. Post-traumatic stress disorder in military nurses who served in Vietnam during the war years 1965–1973. Mil Med. 1988;153:238–42. [PubMed] [Google Scholar]
- 134.Mohanakrishnan Menon P, Nasrallah HA, Lyons JA, Scott MF, Liberto V. Single-voxel proton MR spectroscopy of right versus left hippocampi in PTSD. Psychiatry Res. 2003;123:101–8. doi: 10.1016/s0925-4927(03)00044-1. [DOI] [PubMed] [Google Scholar]
- 135.Metzger LJ, Carson MA, Paulus LA, et al. Event-related potentials to auditory stimuli in female Vietnam nurse veterans with posttraumatic stress disorder. Psychophysiology. 2002;39:49–63. doi: 10.1017/S0048577202001002. [DOI] [PubMed] [Google Scholar]
- 136.Carson MA, Paulus LA, Lasko NB, et al. Psychophysiologic assessment of posttraumatic stress disorder in Vietnam nurse veterans who witnessed injury or death. J Consult Clin Psychol. 2000;68:890–7. [PubMed] [Google Scholar]
- 137.Wolfe J, Chrestman KR, Ouimette PC, Kaloupek D, Harley RM, Bucsela M. Trauma-related psychophysiological reactivity in women exposed to war-zone stress. J Clin Psychol. 2000;56:1371–9. doi: 10.1002/1097-4679(200010)56:10<1371::AID-JCLP8>3.0.CO;2-X. [DOI] [PubMed] [Google Scholar]
- 138.Gurvits TV, Carson MA, Metzger L, et al. Absence of selected neurological soft signs in Vietnam nurse veterans with post-traumatic stress disorder. Psychiatry Res. 2002;110:81–5. doi: 10.1016/s0165-1781(02)00026-4. [DOI] [PubMed] [Google Scholar]
- 139.Rauch SL, Shin LM, Segal E, et al. Selectively reduced regional cortical volumes in post-traumatic stress disorder. Neuroreport. 2003;14:913–6. doi: 10.1097/01.wnr.0000071767.24455.10. [DOI] [PubMed] [Google Scholar]
- 140.Wolfe J, Brown PJ, Bucsela ML. Symptom responses of female Vietnam veterans to Operation Desert Storm. Am J Psychiatry. 1992;149:676–9. doi: 10.1176/ajp.149.5.676. [DOI] [PubMed] [Google Scholar]
- 141.Levitte SS, Hoffman WF. Characteristics of male and female veterans who use VA psychiatric emergency services. Psychiatr Serv. 1995;46:281–2. doi: 10.1176/ps.46.3.281. [DOI] [PubMed] [Google Scholar]
- 142.Davis TM, Bush KR, Kivlahan DR, Dobie DJ, Bradley KA. Screening for substance abuse and psychiatric disorders among women patients in a VA Health Care System. Psychiatr Serv. 2003;54:214–8. doi: 10.1176/appi.ps.54.2.214. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Evidence Tables of Stress of Military Life Studies
Evidence Tables of Health and Performance
Evidence Tables of Health Services Research/Quality of Care
Psychiatric Evidence Tables
Evidence Tables of Different Gender Manifestations of Emotional Disorders
Evidence Tables of Health Behaviors, Prevention and Epidemiology
Evidence Tables of Clinical Conditions
Evidence Tables of Gynecological Conditions