Abstract
Background
To report a 45 year old lady presenting with proximal jejunal gangrene due to invasive Aspergillosis. The patient was undergoing adjuvant chemotherapy for advance carcinoma of breast (Stage IV).
Methods
The patient was referred to our surgical emergency for acute abdominal symptoms for 6 hours. Histopathology revealed bowel wall necrosis and vascular invasion by Aspergillus Fumigatus. Postoperative recovery was uneventful and the patient received Amphotericin-B (1 mg/kg/day) for invasive aspergillosis. Invasive pulmonary aspergillosis was confirmed by isolating Aspergillus Fumigatus from bronchoalveolar lavage and by a positive circulating galactomannan test (ELISA Assay).
Results
Detailed history revealed dry cough and two episodes of haemoptesis for 2 weeks. Haemogram and counts revealed anemia and neutropenia. Plain X – ray of the abdomen showed multiple air fluid levels and ultrasound of the abdomen revealed distended bowel loops. On exploration small bowel was found to be gangrenous. The patient was successfully managed by supportive treatment and conventional intravenous Amphotericin-B for 2 weeks. The lady was discharged one week after completion of antifungal therapy and one month later she underwent toilet mastectomy. The lady came to follow up for 1 year and she is currently under hormone therapy.
Conclusion
With the emergence of new and powerful immunosuppressive, anticancer drugs and potent antibiotics the survival of transplant and critically ill patients has remarkably increased but it has shown a significant rise in the incidence of invasive opportunistic fungal infections. We conclude hat the diagnosis of invasive gastrointestinal aspergillosis may be considered in a neutropenic patient with acute abdominal symptoms.
Background
Despite the use of new and effective drugs, the disseminated invasive aspergillosis often remains lethal in neutropenic patients [1]. There is a great need to create high index of clinical investigation and develop better diagnostic tools to detect invasive aspergillosis before it causes irreversible damage. In the present study we report a 45 year old lady with severe neutropenia (400/cumm) presenting with acute abdomen. Invasive gastrointestinal aspergillosis leading to widespread proximal bowel infarction was found on exploration. The diagnosis was established by isolating Aspergillus fumigatus from bronchoalveolar lavage and by a positive circulating galactomannan test (ELISA). The patient received conventional intravenous amphotericin-B for 2 weeks.
Methods
A 45 year old lady admitted in intensive care unit was referred to our surgical emergency unit for severe acute pain and distention of the abdomen for 6 hours. She was undergoing chemotherapy in clinical oncology department for locally advance carcinoma (Stage IV) of breast and four days back she was shifted to the intensive care unit when she developed severe neutropenia after fourth cycle CAF regimen (Cyclophosphamide 500 mg/m2, Adriamycin 50 mg/m2 and 5-FU 500 mg/m2). There was no metastasis. Detailed history revealed that the patient had developed dry cough and fever 7 days back. The patient had absolute constipation. On examination the abdomen was distended and there was guarding and rebound tenderness. Hematocrit and counts revealed anemia (Hb 7 gm%) and neutropenia (400/cumm).
Plain radiograph of chest showed patchy infiltrates in both the lung fields suggestive of pneumonitis and X-ray abdomen showed distended bowel loops and multiple air fluid levels. There was no gas under the diaphragm. Ultrasound of the abdomen could not add much to the findings of plain X-ray and showed distended bowel loops and minimal interbowel fluid. Emergency exploratory laprotomy was performed under general anesthesia. About 30 cm of proximal jejunum 15 cm distal to duodeno-jejunal junction was found to be gangrenous. Primary resection and anastomosis was done and the specimen (resected bowel segment with adjoining mesentery) was sent for histopathology. After surgery the patient was shifted to postoperative ICU where she developed fever which was not responding to any antibiotic.
On the basis of preoperative X-ray chest, neutropenia and high index of clinical suspicion broncho-alveolar lavage was performed which revealed pulmonary aspergillosis. Serum galactomannan test (ELISA) was also positive for Aspergillus. The diagnosis of invasive pulmonary aspergillosis was made and the patient was put on conventional intravenous Amphotericin B (1 mg/kg/day) for 2 weeks. Histopathology of the specimen was available on fourth postoperative day and revealed transmural ischemic necrosis of the bowel and widespread invasion and blockade of arterioles due to Aspergillus fungal forms (Fig. 1). The diagnosis of invasive gastrointestinal aspergillosis secondary to pulmonary Aspergillosis was made and antifungal treatment was continued. The patient responded to intravenous antifungal treatment and was discharged after 2 week of antifungal treatment. The lady underwent toilet mastectomy and was under follow up for 1 year. Postoperative chemotherapy was also given after improvements in the counts and presently she is under hormone therapy.
Figure 1.
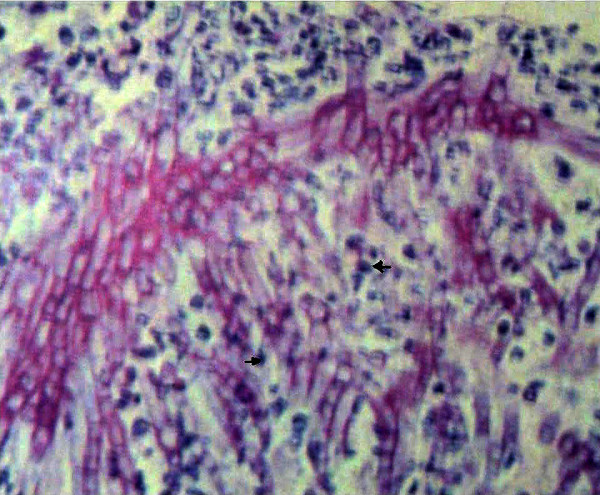
Histopathology analysis demonstrates vascular invasion by disseminated aspergillosis. (Arrows showing fungal forms).
Results and discussion
In our patient the diagnosis was made by exclusion and the decision for bronchi-alveolar lavage was taken which came out positive for aspergillosis. This evidence along with positive galactomannan test was enough to support the diagnosis of invasive Aspergillosis and intravenous Amphotericin B was started. The patient showed dramatic response and fever subsided on the next day. After recovery patient underwent modified radical mastectomy and postoperative chemotherapy and hormone therapy were also given. The patient was alive and well at the end of 1 year follow up.
Invasive gastrointestinal aspergillosis is an opportunistic infection that characteristically affects the immunocompromised host, resulting in high degree of morbidity and mortality [2]. The incidence of invasive aspergillosis has risen considerably during the past decade due to more intensive chemotherapy, organ transplantation, intensive care, and aggressive surgical interventions [3]. Extrapulmonary aspergillosis is rare but can involve gastrointestinal tract, heart, kidney, central nervous system, liver and pancreas etc [4]. Almost one-quarter of those with invasive pulmonary aspergillosis develop disseminated infection with Aspergillus sp. via hematogenous spread [2,5]. Among these patients the reported incidence of gastrointestinal involvement has been 41 – 47% [2,5,6].
Patients with bowel involvement are rarely diagnosed prior to autopsy because the typical symptoms of abdominal pain, obstruction and gastrointestinal bleeding are usually overshadowed by the septic manifestation of systemic infection. Wingrad et al [7] documented a case of aspergillosis as an unusual cause of perforated appendicitis in 1982. In our patient gastrointestinal invasion was secondary to hematogenous spread of fungal forms leading to ischemic necrosis of bowel. The diagnosis was made on the basis of high clinical suspicion followed by bronchoalveolar lavage and positive serum galactomannan test. This diagnosis should be considered when a neutropenic patients presents with abdominal pain and distention with fever.
There has been an increased understanding of the immunology of Aspergillus infection, paving the way to novel immune augmentation strategies in animal models that merit evaluation in phase I clinical trials [8]. Chest CT scan [8] and new techniques like PCR assays based on real time technologies that are able to quantify Aspergillus DNA are promising [9]. Considerable progress has been made in understanding the genetics of Aspergillus Fumigates and molecular techniques for manipulation of the fungus have been developed but still invasive Aspergillus's is associated with a high mortality rate ranging from 30% to 90% [10].
Repeated serum assays to detect Aspergillus antigenemia and meticulous search for other aspergillosis localizations like pulmonary, should continue until the diagnosis allows administration of early antifungal therapy. Though in our patient we used conventional antifungal treatment, combined antifungal therapy or treatment with amphotericin-B at high doses significantly reduces mortality as compared with the conventional treatment [11].
Conclusion
Even with more effective and safer therapies, substantial progress in quelling aspergillosis may not occur until the early diagnostic tools are developed and incorporated into strategies to start earlier treatment. We suggest that a very high index of suspicion of invasive gastrointestinal aspergillosis may be maintained in immunocompromised patients presenting with acute abdominal symptoms.
Acknowledgments
Acknowledgements
We thank to the Department of Surgery, King George Medical University, India and Children's Memorial Research Center, The Feinberg School of Medicine, Chicago, USA for supporting the present investigation.
Contributor Information
Amit Chaudhary, Email: amitwtc@yahoo.co.in.
Vinod Jain, Email: vinodjainkgmu@yahoo.co.in.
Rama S Dwivedi, Email: ramaa@northwestern.edu.
Samir Misra, Email: drsamirkgmc@yahoo.com.
References
- Tresallet C, Nguyen-Thanh Q, Aubriot-Lorton MH, Akakpo JP, Al Jijakli A, Cardot V, Chigot JP, Menegaux F. Small-bowel infarction from disseminated aspergillosis. Dis Colon Rectum. 2004;47:1515–8. doi: 10.1007/s10350-004-0625-9. [DOI] [PubMed] [Google Scholar]
- Shah SS, Birnbaum BA, Jacobs JE. Disseminated aspergillosis inciting intestinal ischemia and obstruction. Brit J Radiol. 2001;74:1145–1147. doi: 10.1259/bjr.74.888.741145. [DOI] [PubMed] [Google Scholar]
- Kulberg BJ, Oude Lashif AM. Epidemology of oppurtunistic invasive mycoses. European J Med Res. 2002;31:183–191. [PubMed] [Google Scholar]
- Hori A, Kami M, Kishi Y, Machida U, Matsumura T, Kashima T. Clinical significance of extra-pulmonary involvement of invasive aspergillosis: a retrospective autopsy-based study of 107 patients. J Hosp Infect. 2002;50:175–182. doi: 10.1053/jhin.2001.1170. [DOI] [PubMed] [Google Scholar]
- Young RC, Bennett JE, Vogel CL, Carbone , De Vita VT. Aspergillosis: The spectrum of disease in 98 patients. Medicine. 1970;49:147–173. doi: 10.1097/00005792-197003000-00002. [DOI] [PubMed] [Google Scholar]
- Prescott RJ, Harris M, Banerjee SS. Fungal infection of small and large intestine. J Clinical Pathology. 1992;45:806–811. doi: 10.1136/jcp.45.9.806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weingrad DN, Knapper WH, Gold J. Aspergillus peritonitis complicating perforated appendicitis in adult acute leukemia. J Surgical oncology. 1982;19:5–8. doi: 10.1002/jso.2930190103. [DOI] [PubMed] [Google Scholar]
- Segal BH, Walsh TJ. Current approaches to the diagnosis and treatment of invasive Aspergillosis. Am J Respir Crit Care Med. 2006;173:707–17. doi: 10.1164/rccm.200505-727SO. [DOI] [PubMed] [Google Scholar]
- Ferns RB. Evaluation of the role of real time PCR in the diagnosis of invasive aspergillosis. Leuk Lymphoma. 2006;47:15–20. doi: 10.1080/10428190500244233. [DOI] [PubMed] [Google Scholar]
- Brakhage AA. Systemic fungal infections caused by Aspergillus species: epidemiology, infection process and virulence determinants. Curr Drug Targets. 2005;6:875–886. doi: 10.2174/138945005774912717. [DOI] [PubMed] [Google Scholar]
- Trullas JC, Cervera C, Benito N, Puig de la Bellacasa J, Agusti C, Rovira M, Mas A, Navasa M, Cofan F, Ricart MJ, Perez-Villa F, Moreno A. Invasive pulmonary aspergillosis in solid organ and bone marrow transplant recipients. Transplant Proc. 2005;37:4091–4093. doi: 10.1016/j.transproceed.2005.09.182. [DOI] [PubMed] [Google Scholar]


