Abstract
Here, we describe that microenvironmental IL-1β and, to a lesser extent, IL-1α are required for in vivo angiogenesis and invasiveness of different tumor cells. In IL-1β knockout (KO) mice, local tumor or lung metastases of B16 melanoma cells were not observed compared with WT mice. Angiogenesis was assessed by the recruitment of blood vessel networks into Matrigel plugs containing B16 melanoma cells; vascularization of the plugs was present in WT mice, but was absent in IL-1β KO mice. The addition of exogenous IL-1 into B16-containing Matrigel plugs in IL-1β KO mice partially restored the angiogenic response. Moreover, the incorporation of IL-1 receptor antagonist to B16-containing plugs in WT mice inhibited the ingrowth of blood vessel networks into Matrigel plugs. In IL-1α KO mice, local tumor development and induction of an angiogenic response in Matrigel plugs was less pronounced than in WT mice, but significantly higher than in IL-1β KO mice. These effects of host-derived IL-1α and IL-1β were not restricted to the melanoma model, but were also observed in DA/3 mammary and prostate cancer cell models. In addition to the in vivo findings, IL-1 contributed to the production of vascular endothelial cell growth factor and tumor necrosis factor in cocultures of peritoneal macrophages and tumor cells. Host-derived IL-1 seems to control tumor angiogenesis and invasiveness. Furthermore, the anti-angiogenic effects of IL-1 receptor antagonist, shown here, suggest a possible therapeutic role in cancer, in addition to its current use in rheumatoid arthritis.
The cytokine IL-1 mainly affects inflammatory processes but also possesses various immune, degradative, and growth-promoting properties. There are two IL-1 agonistic proteins, IL-1α and IL-1β, and one antagonistic protein, the IL-1 receptor antagonist (IL-1Ra, reviewed in ref. 1). IL-1Ra binds to the IL-1 receptor type I without transmitting an activation signal and, thus, represents a physiological inhibitor of IL-1 activity. IL-1α and IL-1β bind to the same receptors, and there are no significant differences in the spectrum of activities induced by recombinant IL-1α or IL-1β by using in vitro and in vivo assays, including injection into humans (1). However, processing of IL-1α and IL-1β differ: IL-1β is active only as secreted mature product, whereas IL-1α is active as a precursor or membrane-associated molecule. IL-1α remains cytosolic but IL-1β is abundantly secreted by activated macrophages and blood monocytes. Also, IL-1β is present in the circulation of patients undergoing infectious or inflammatory responses, whereas IL-1α is rarely found in the circulation (1).
Tumor enlargement requires blood vessel growth that originates with the sprouting of new capillaries from preexisting blood vessels; in the absence of access to an adequate vasculature, tumor cells become necrotic and/or apoptotic (reviewed in refs. 2–8). Tumors may exist as microscopic in situ lesions for years in the absence of their own microcirculation. For tumor progression and metastasis, an angiogenic switch permits rapid growth and invasion (2–8). The angiogenic switch is a discrete genetic event that results in a change in the local equilibrium between pro- and anti-angiogenic regulators, which are produced by tumor cells as well as by the surrounding stromal cells and infiltrating leukocytes.
In various experimental models, IL-1 increases tumor invasiveness and metastasis (1, 9–17). For example, IL-1 expression at the site of tumor development enhances the expression of adhesion molecules on endothelial and malignant cells and facilitates the invasion of malignant cells into the circulation and their dissemination to remote tissues (11, 13). Although recombinant IL-1 stimulates the proliferation of endothelial cells, adhesion molecule expression and production of cytokines and small/inflammatory mediator molecules (1, 18, 19), endogenous IL-1 has not been characterized as major cytokine in mediating in vivo tumor angiogenesis. In the present studies, we have assessed the role of IL-1 as a regulator of tumor angiogenesis by using transplantable tumors in IL-1β and IL-1α knockout (KO) mice. We also assessed whether inhibition of IL-1 activity by IL-1Ra can function as an anti-tumor agent by inhibiting angiogenesis.
Materials and Methods
Reagents.
Recombinant human IL-1Ra was obtained from Amgen Biologicals; recombinant mouse IL-1α was obtained from R & D Systems. Matrigel was purchased from Biological Industries, Beit HaEmek, Israel.
Tumor Cells.
B16 melanoma cells (20) and the DA/3 mammary adenocarcinoma (21) were maintained in DMEM (GIBCO/Invitrogen) supplemented with 10% (vol/vol) FCS, 100 units/ml penicillin, 0.1 mg/ml streptomycin, and 2 mM l-glutamine in a humidified 5% CO2 atmosphere at 37°C. All medium ingredients were purchased from Biological Industries.
Mice.
IL-1β and IL-1α KO mice were described (22–24). WT C57BL/6 and BALB/c strains were obtained from The Jackson Laboratory and Harlan, Jerusalem. Animal studies were performed according to the guidelines and approval of the Animal Care Committee of Ben-Gurion University. Female 8- to 10-week-old mice were used in all experiments.
Tumorigenicity Assays.
WT or IL-1 KO mice were injected intrafootpad (i.f.p.) or intravenously (i.v.) with 2 × 105 B16 melanoma cells to assess local tumor growth or metastasis, respectively. Local tumor development was measured by using a caliper. The endpoint of such experiments was the time at which the tumor's size had reached a diameter of 12 mm. Mice injected i.v. were observed until the first signs of dyspnea and then killed. Lung metastases were evaluated histologically in formalin-fixed paraffin sections stained with hematoxylin/eosin. BALB/c or IL-1 KO mice from the same background were injected i.f.p. with 5 × 105 DA/3 mammary adenocarcinoma cells, and the development of the tumor growth was scored as above.
Angiogenesis in Matrigel Plugs.
Angiogenesis was assessed in Matrigel plugs (25). Mice were inoculated s.c. in the interscapular area with 0.4 ml of Matrigel alone or with Matrigel mixed with 2 × 105 tumor cells. Matrigel is liquid at 4°C but solid at room temperature. In some experiments, recombinant IL-1α or IL-1Ra was added to the mixture of Matrigel and B16 melanoma cells at 4°C just before injection into mice. Saline was mixed with Matrigel to compensate for the volume of IL-1Ra or IL-1α. Matrigel plugs were surgically removed on day 7. Part of each plug was fixed with 10% (vol/vol) formaldehyde, embedded in paraffin, sectioned, and either stained with hematoxylin/eosin or immunostained with antibodies for Von Willebrand's factor, a marker for endothelial cells (26).
Quantification of Microvessel Density (MVD).
Microvessels in Matrigel plugs were visualized by using rat antibodies to human Von Willebrand's factor (DAKO), which crossreact with murine Von Willebrand's factor. MVD was determined by first screening areas of highest vascularity under low magnification (×100; ref. 27). The MVD was calculated by counting six highly vascularized fields in each section at a magnification of ×200. MVD calculations were performed by the same pathologist in a blinded manner.
Culture of Peritoneal Macrophages.
Peritoneal exudate cells (PEC) were obtained from mice as described (28). Briefly, mice were injected i.p. with thioglycollate (Hy-Labs, Kiryat Weizmann, Rehovot, Israel). After 4 days, PEC were collected from peritoneal lavage and plated (5 × 105 cells per ml) in 24-well plates (Greiner, Frickenhausen, Germany) for 18 h to allow for adherence. Cells were washed, and adherent cell monolayers were activated with B16 melanoma cells (melanoma/macrophage ratio, 1:5). Levels of vascular endothelial cell growth factor (VEGF) and tumor necrosis factor α (TNFα) in 48-h supernatants were measured by specific ELISA kits (DuoSet, R & D Systems).
Results
Tumorigenicity of B16 Melanoma Cells in IL-1β KO Mice.
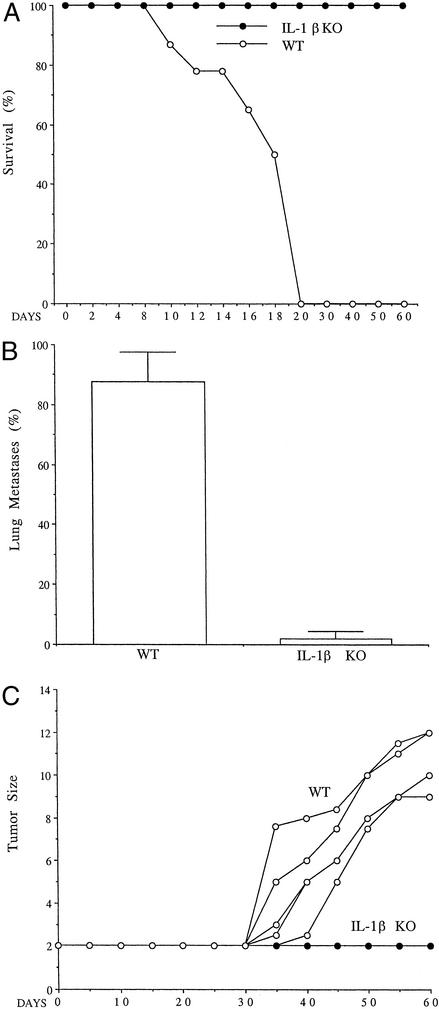
Tumor growth was assessed in C57BL/6 WT mice and in IL-1β KO mice from the same background. Because B16 melanoma cells metastasize to the lungs, the development of experimental lung metastasis after i.v. inoculation of the malignant cells and mortality was recorded. Consistently, as shown in Fig. 1A, all WT C57BL/6 mice died within 20 days, whereas all IL-1β KO mice injected with the B16 cells remained alive throughout the experiment. Mice died from lung metastasis (Fig. 1B), as evidenced in histological sections from moribund mice suffering from dyspnea. To evaluate the kinetics of local tumor development in IL-1β KO, B16 melanoma cells were injected i.f.p., and the diameter of the tumors was measured every 5 days. As shown in Fig. 1C, no tumor development was observed when B16 melanoma cells were injected into IL-1β KO mice, whereas progressive tumor growth was observed in WT mice. In F1 (WT × IL-1β KO) of C57BL/6 origin tumors developed as in WT mice (data not shown).
Figure 1.
Increased survival rate and decreased tumor growth in IL-1β KO mice. (A) Survival after i.v. injection of B16 melanoma into IL-1β KO (n = 10) compared with WT mice (n = 10). (B) Frequency of lung micrometastases as detected in histological sections on day 14 after tumor cell injection (n = 10). (C) Tumor size of B16 melanoma after i.f.p. injection (2 × 105 cells per mouse; n = 5 per group). Results shown are from one experiment of six performed.
Reduced in Vivo Angiogenesis of B16 Melanoma Tumors in IL-1β KO Mice.
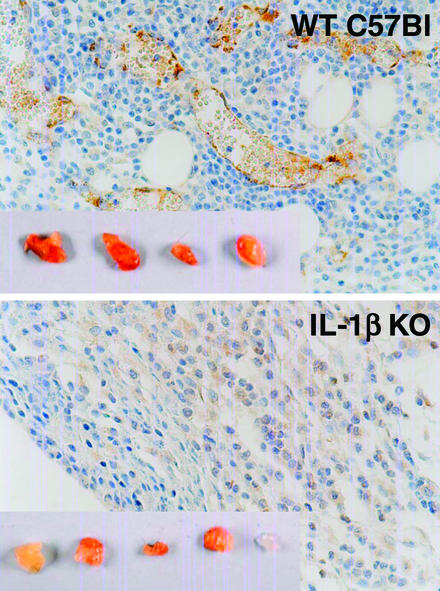
Next, we examined the in vivo recruitment of the angiogenic network into Matrigel plugs embedded with B16 melanoma cells. Tumor cells were mixed with Matrigel and injected s.c. into WT and IL-1β KO mice. As shown in Fig. 2 Upper Inset, active angiogenesis could be observed macroscopically in plugs recovered from WT mice: the plugs are more red compared with B16 melanoma cell-containing plugs from IL-1β KO mice (Fig. 2 Lower Inset). To directly view angiogenesis in the plugs, histological sections were stained with antibodies against Von Willebrand's factor. As shown in Fig. 2, B16 melanoma cells embedded in Matrigel plugs in WT mice induced a potent angiogenic response (Upper), whereas the angiogenic response developing in malignant cells containing plugs from IL-1β KO mice exhibited a background response.
Figure 2.
Blood vessel growth in B16 cells embedded in Matrigel plugs. (Upper) Section through a B16-embedded Matrigel plug injected s.c. in WT mice and removed on day 7 (×400). (Inset) Gross morphology of Matrigel plugs. (Lower) Similarly stained sections through Matrigel plugs injected into IL-1β KO mice. Results shown are from one of four experiments performed.
IL-1 Controls Tumor Angiogenesis.
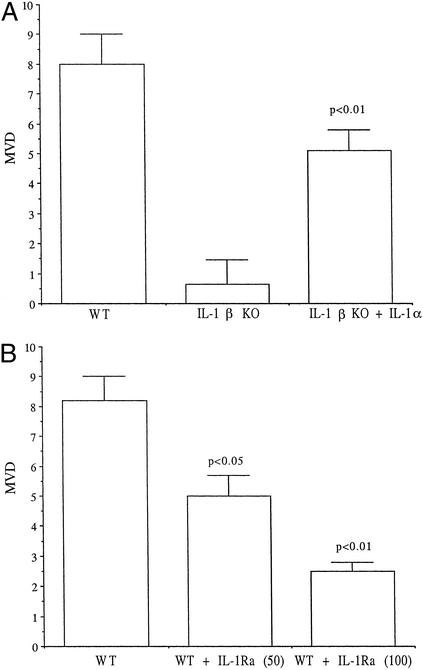
To study whether IL-1 is indeed the factor responsible for this tumor-induced angiogenic response, Matrigel plugs injected into IL-1β KO mice were supplemented with IL-1, in this case, recombinant murine IL-1α. As depicted in Fig. 3A, recombinant IL-1α embedded into Matrigel plugs together with B16 melanoma cells before gelation largely restored the missing angiogenic response observed in IL-1β KO mice.
Figure 3.
MVD in B16 melanoma embedded in Matrigel plugs. (A) MVD ± SEM in B16 melanoma-embedded Matrigel plugs in WT or IL-1β KO mice on day 7. IL-1β KO mice were also implanted with Matrigel plugs embedded with a mixture of B16 cells and 100 ng of murine IL-1α per 0.4 ml of Matrigel (n = 5 in each group). (B) Day 7 MVD of Matrigel plugs embedded into WT mice containing a mixture of B16 melanoma cells plus saline, 50 or 100 μg of recombinant human IL-1Ra per 0.4 ml of Matrigel (n = 5 in each group).
Next, increasing concentrations of IL-1Ra were incorporated into B16 melanoma-containing Matrigel plugs and injected into WT mice. This procedure resulted in a dose-dependent reduction in MVD in the plugs (Fig. 3B). Together, these results demonstrate that microenvironmental IL-1β is required for tumor invasiveness, possibly through induction of an angiogenic response.
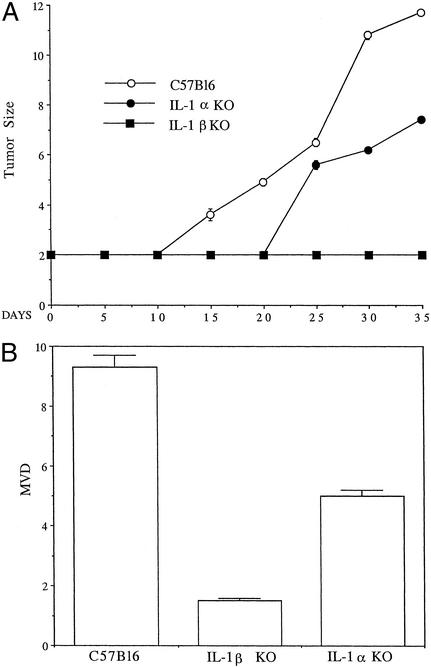
Because recombinant IL-1α substituted the angiogenic response missing in IL-1β KO mice, it was of interest to assess directly the effects of microenvironmental IL-1α on tumor invasiveness and blood vessel formation. B16 melanoma cells were injected i.f.p. into WT, IL-1α, or IL-1β KO C57BL/6 mice, and the growth of local tumors was determined. Again, in IL-1β KO mice, no tumor development was observed, whereas in WT mice, B16 melanoma induced progressive tumors. In IL-1α KO mice, tumorigenicity patterns of B16 cells were reduced compared with the WT mice, as evidenced by the late appearance and slower growth rate of the tumors (Fig. 4A). Next, the angiogenic response in B16 melanoma-containing Matrigel plugs from WT, IL-1α, and IL-1β KO mice was compared. As shown by MVD in Fig. 4B, in IL-1β KO mice, the angiogenic response is nearly absent, whereas in IL-1α KO mice, the response is reduced by ≈50%, compared with that in WT mice.
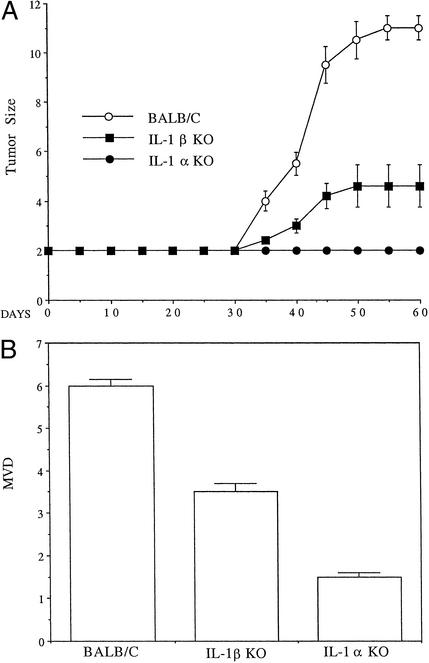
Figure 4.
Growth and MVD of B16 melanoma cells in WT, IL-1α, and IL-1β KO mice. (A) Tumor growth in mice injected i.f.p. with B16 cells, as indicated in legend to Fig. 1C. The results represent one of three experiments. Mean ± SEM for each (n = 8 per group) are shown. (B) MVD ± SEM in B16 melanoma-embedded Matrigel plugs (2 × 105) in WT, IL-1β, or IL-1α KO mice (n = 5 in each group).
Effects of IL-1 on Tumor Invasiveness and Angiogenesis in DA/3 Mammary Adenocarcinoma Tumors.
It was necessary to determine whether host-derived IL-1 also affects the in vivo growth patterns of other experimental tumors. The mammary cancer tumor DA/3 in BALB/c mice was used. As shown in Fig. 5A, in IL-1α KO mice, no tumor development was observed, whereas in IL-1β KO mice, tumors developed slower and were smaller compared with tumors in WT BALB/c mice. This hierarchy was also observed when MVD was determined on sections from Matrigel plugs containing embedded DA/3 cells in control, IL-1α KO, and IL-1β KO BALB/c mice (Fig. 5B). It seems that host-derived IL-1 is important for the growth of both B16 melanoma and DA/3 breast cancer cells. For B16 cells, IL-1β plays a dominant role in tumor development; for the invasiveness of DA/3 cells, IL-1α plays a more dominant role.
Figure 5.
Growth and MVD of DA/3 mammary cancer cells in WT BALB/c, IL-1α, or IL-1β KO mice. (A) Mice were injected i.f.p. with DA/3 cells (5 × 105 cells per mouse). The results represent one of three experiments. Mean ± SEM from each group (n = 8 per group) are shown. (B) MVD ± SEM in DA/3-embedded Matrigel plugs (2 × 105) in WT, IL-1β, or IL-1α KO mice (n = 5 in each group).
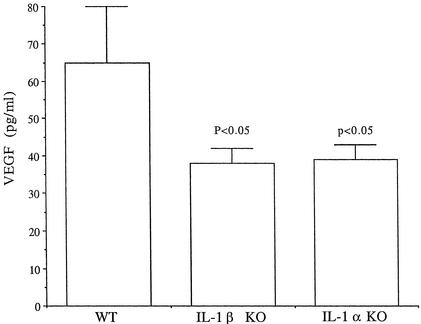
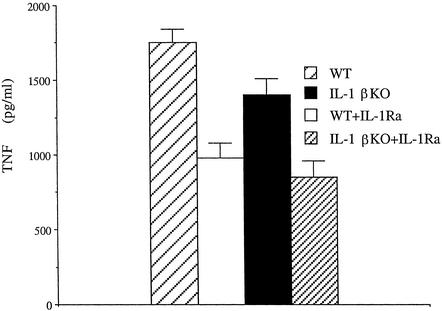
Role of IL-1 in the Production of VEGF and TNFα from PEC.
Upon interaction with malignant cells, macrophages present in the tumor's microenvironment likely secrete factors that may affect the malignant process, including tumor angiogenesis. Thus, we assessed the production of VEGF in macrophages from control and IL-1 KO mice that were cocultured with B16 melanoma cells. Adherent PEC were incubated with melanoma cells for 48 h, and the supernatants were assessed for VEGF and TNFα. Cultured alone, PEC did not release VEGF or TNFα. In contrast, melanoma cells cultured alone released 20 pg/ml VEGF but not TNFα after 48 h (not shown). In cocultures of peritoneal macrophages from WT mice plus B16 cells (as shown in Fig. 6), a further increase in VEGF secretion was observed; however, this increase was reduced by ≈50% when macrophages were obtained from IL-1β KO or IL-1α KO mice. In macrophage-B16 cocultures, TNFα (Fig. 7) and IL-6 (not shown), were also induced; their generation was largely inhibited by IL-1Ra. As can be seen in Fig. 7, less TNFα was observed in supernatants of cocultures consisting of macrophages from IL-1β KO mice, and in both cases TNFα release was inhibited by IL-1Ra.
Figure 6.
VEGF secretion in cocultures of B16 melanoma cells and macrophages from WT, IL-1α, or IL-1β KO mice. PEC were obtained and cocultured with B16 melanoma cells, as indicated in Materials and Methods. Mean ± SEM VEGF levels in 48-h supernatants were measured (n = 5 experiments).
Figure 7.
TNFα secretion in cocultures of B16 melanoma cells and macrophages from WT and IL-1β KO mice. PEC were obtained and stimulated with melanoma cells in the presence or absence of IL-1Ra (10 μg/ml). Mean ± SEM TNFα levels in 48-h supernatants are shown (n = 5 experiments).
Discussion
The present study demonstrates the role of endogenous IL-1 in promoting the invasiveness of malignant cells and emphasizes the dependency of tumor angiogenesis on this cytokine. To our knowledge, this is the first report that shows that mostly IL-1β accounts for the ability of tumor cells to initiate and complete the processes of angiogenesis, as manifested by the inability of tumor cells embedded in Matrigel plugs to recruit a vasculature network. Mice solely deficient in IL-1α or IL-1β exhibit dramatically impaired tumor development and blood vessel growth. These findings seem to represent a general phenomenon, because they were observed in different experimental tumor models: B16 melanoma, DA/3 mammary adenocarcinoma in BALB/e mice, and prostate cancer cell lines injected i.f.p. into C57Bl6 mice (data not shown). It seems that for B16 melanoma and prostate cancer, IL-1β is essential for invasiveness, but for others (DA/3 mammary cancer), IL-1α plays a greater role than IL-1β.
B16 melanoma cells injected into the footpad of IL-1β-deficient mice failed to develop into local tumors, compared with WT mice. In IL-1α-deficient mice, the reduction was less dramatic. This failure to proliferate and progress into an expansive tumor is likely caused by an inability to initiate angiogenesis. On histological examination, B16 cells injected into IL-1β-deficient mice remained pigmented at the site of inoculation, similar to their appearance in culture, and thus possibly representing dormant tumor cells. This result was in sharp contrast to control WT mice, where invading B16 melanoma cells seemed to be de-differentiated and to lose melanin (data not shown). Moreover, when injected i.v., B16 cells produce micrometastases in the lungs, resulting in death after 14–16 days, whereas in IL-1β-deficient mice, micrometastases were not observed, and mice were long survivors, at least 6 months after tumor-cell injection.
We also examined the effect of specific blockade of IL-1 receptor in WT mice by using the IL-1Ra. IL-1Ra incorporated into B16 cell-containing Matrigel plugs implanted into WT mice significantly reduced the outgrowth of tumors and the recruitment of an angiogenic network into the plugs. Furthermore, the addition of 100 ng of recombinant IL-1 into Matrigel plugs with B16 cells in IL-1β KO mice resulted in restoration of the angiogenic response. Thus, the use of IL-1Ra itself, as well as other methods to reduce IL-1 activity, may have clinical utility in both inflammatory as well as neoplastic diseases where angiogenesis is a contributing factor.
Both IL-1α and IL-1β were shown to contribute to tumor angiogenesis and invasiveness, but the role of IL-1β is more evident in these processes. This may be due to IL-1β being secreted into the microenvironment, thus activating cells in the tumor's stroma, including the malignant cells. In contrast, the effects of IL-1α are more limited, as this cytokine is largely cell-associated. The present findings agree with our previous observations that tumor cells engineered to secrete IL-1β result in a more severe and invasive pattern compared with that of mock-transfected cells (15). In contrast, in that study, IL-1α-expressing transfectants did not produce tumors, likely because of IL-1α-induced immune responses, which eradicated the malignant cells (15, 28–30).
We emphasize the role of host-derived IL-1 as an important factor for tumor angiogenesis and tumor growth. Previous studies have focused on the invasion-promoting features of IL-1 (9–12, 14, 17). IL-1 induces adhesion molecule expression on both malignant and endothelial cells (11), enabling access of malignant cells into the circulation and their invasiveness. Vidal-Vanaclocha and coworkers (10, 13, 14, 17) have demonstrated the role of hepatic sinusoidal endothelial cell-derived IL-1 in promoting hepatic metastasis of B16 melanoma cells. In that model, reduction of metastases and increased survival rates were observed using systemic administration of IL-1Ra (10). Hepatic metastasis was also significantly reduced in IL-1β-deficient mice and almost completely absent in mice deficient in the IL-1β-converting enzyme, which processes the precursors of IL-1β as well as IL-18 (17). In vitro, increased binding of the melanoma cells to hepatic sinusoidal endothelial cells was observed and shown to be caused by the up-regulation of expression of vascular cell adhesion molecule-1 and possibly other adhesion molecules on endothelial cells (10, 13, 14). Supernatants of melanoma cells stimulated endothelial cells to secrete IL-1β, TNFα, and IL-18, each of which up-regulate adhesion molecule expression.
Multiple cytokines may affect tumor growth by stimulating angiogenic factor production (2–8). The role of IL-1 in inducing VEGF production has been described (31). Moreover, IL-1β selectively induces the expression of hypoxia inducible factor-1α, a dominant transcription factor for VEGF (32–35). Here, we show that endogenous IL-1 is involved in the production of VEGF in cocultures of macrophages and B16 melanoma cells: by using macrophages from IL-1β and IL-1α KO mice, there was reduced VEGF secretion. Nozaki et al. (36) have shown that VEGF production by breast cancer cells, which constitutively secrete IL-1α, is not inhibited by anti-IL-1 antibodies, whereas IL-6 and IL-8 are inhibited by these antibodies, suggesting that the effects of IL-1 on VEGF production are indirect. However, IL-1 is directly involved in production of IL-6 and TNFα in cocultures of macrophages and B16 melanoma cells where production of TNFα and IL-6 is lower in macrophages from IL-1β KO mice, and, in each case, inhibited by IL-1Ra.
Intervention in tumor vascularity in experimental tumors has been reported using inhibitors of the VEGF loop (37–39) and anti-angiogenic factors, i.e., angiostatin, endostatin (4–6, 40, 41), and IFN-α or -β (42). In addition, antiproteolytic agents, which target metalloproteinases (43, 44) and heparanase (45), inhibit extra cellular matrix degradation and possess anti-tumor activity. Anti-inflammatory agents, such as cyclooxygenase inhibitors (46) and inhibitors of NF-κΒ (47, 48), have also been effective in reducing angiogenesis. Because IL-1 is a major inducer of inflammation and particularly of cyclooxygenase-2 (1), other angiogenic and small mediator molecules may represent a downstream event of an IL-1-initiated signal. As such, IL-1 may serve as a master cytokine upon which different angiogenic stimuli converge. Thus, blockade of a single molecule, i.e., IL-1, may inhibit the cascade of downstream (effector) angiogenic factors. In VEGF-impregnated nylon discs implanted into rat corneal stromata, systemic treatment with IL-1Ra reduced the numbers of new blood vessels growing from the corneal limbus toward the implant by 75% (49). Thus, the use of IL-1Ra, which blocks cell activation by either IL-1β or IL-1α and is approved for reducing inflammation in patients with rheumatoid arthritis, may be an appropriate therapeutic strategy for inhibiting tumor angiogenesis. The use of IL-1Ra as an adjunct therapy in combination with tumor resection and chemotherapy is supported by our preclinical studies.
Acknowledgments
We thank Rosalyn M. White and Parvin Zarin for skillful technical help and Philip Bufler for advice. R.N.A. is supported by the Israel Ministry of Science jointly with the Deutsches Krebsforschungszentrum (Heidelberg), the United States–Israel Binational Science Foundation, the Israel Science Foundation founded by the Israel Academy of Sciences and Humanities, the Israel Cancer Association, and the Association for International Cancer Research. E.V. is supported by the Concern Foundation, the Israel Cancer Association, and the Israeli Ministry of Health. C.A.D. is supported by National Institutes of Health Grant AI-15614.
Abbreviations
- IL-1Ra
IL-1 receptor antagonist
- i.f.p.
intrafootpad
- MVD
mean vessel density
- PEC
peritoneal exudate cells
- VEGF
vascular endothelial growth factor
- KO
knockout
- TNFα
tumor necrosis factor α
References
- 1.Dinarello C A. Blood. 1996;87:2095–2147. [PubMed] [Google Scholar]
- 2.Folkman J. N Engl J Med. 1971;285:404–405. doi: 10.1056/NEJM197108122850711. [DOI] [PubMed] [Google Scholar]
- 3.Folkman J. Cancer Metastasis Rev. 1990;9:171–174. doi: 10.1007/BF00046358. [DOI] [PubMed] [Google Scholar]
- 4.Holmgren L, O'Reilly M S, Folkman J. Nat Med. 1995;1:149–153. doi: 10.1038/nm0295-149. [DOI] [PubMed] [Google Scholar]
- 5.Folkman J, D'Amore P A. Cell. 1996;87:1153–1155. doi: 10.1016/s0092-8674(00)81810-3. [DOI] [PubMed] [Google Scholar]
- 6.Hanahan D, Folkman J. Cell. 1996;86:353–364. doi: 10.1016/s0092-8674(00)80108-7. [DOI] [PubMed] [Google Scholar]
- 7.Carmeliet P, Jain R K. Nature. 2000;407:249–257. doi: 10.1038/35025220. [DOI] [PubMed] [Google Scholar]
- 8.Liotta L A, Kohn E C. Nature. 2001;411:375–379. doi: 10.1038/35077241. [DOI] [PubMed] [Google Scholar]
- 9.Chirivi R G, Garofalo A, Padura I M, Mantovani A, Giavazzi R. Cancer Res. 1993;53:5051–5054. [PubMed] [Google Scholar]
- 10.Vidal-Vanaclocha F, Amezaga C, Asumendi A, Kaplanski G, Dinarello C A. Cancer Res. 1994;54:2667–2672. [PubMed] [Google Scholar]
- 11.Chirivi R G, Chiodoni C, Musiani P, Garofalo A, Bernasconi S, Colombo M P, Giavazzi R. Int J Cancer. 1996;67:856–863. doi: 10.1002/(SICI)1097-0215(19960917)67:6<856::AID-IJC16>3.0.CO;2-#. [DOI] [PubMed] [Google Scholar]
- 12.McKenzie R C, Oran A, Dinarello C A, Sauder D N. Anticancer Res. 1996;16:437–441. [PubMed] [Google Scholar]
- 13.Vidal-Vanaclocha F, Alvarez A, Asumendi A, Urcelay B, Tonino P, Dinarello C A. J Natl Cancer Inst. 1996;88:198–205. doi: 10.1093/jnci/88.3-4.198. [DOI] [PubMed] [Google Scholar]
- 14.Anasagasti M J, Alvarez A, Martin J J, Mendoza L, Vidal-Vanaclocha F. Hepatology. 1997;25:840–846. doi: 10.1002/hep.510250410. [DOI] [PubMed] [Google Scholar]
- 15.Apte R N, Dvorkin T, Song X, Fima E, Krelin Y, Yulevitch A, Gurfinkel R, Werman A, White R M, Argov S, et al. Adv Exp Med Biol. 2000;479:277–288. [PubMed] [Google Scholar]
- 16.Apte R N, Voronov E. Semin Cancer Biol. 2002;12:277–290. doi: 10.1016/s1044-579x(02)00014-7. [DOI] [PubMed] [Google Scholar]
- 17.Vidal-Vanaclocha F, Fantuzzi G, Mendoza L, Fuentes A M, Anasagasti M J, Martin J, Carrascal T, Walsh P, Reznikov L L, Kim S H, et al. Proc Natl Acad Sci USA. 2000;97:734–739. doi: 10.1073/pnas.97.2.734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mantovani A, Dejana E. Immunol Today. 1989;10:370–375. doi: 10.1016/0167-5699(89)90270-3. [DOI] [PubMed] [Google Scholar]
- 19.Meager A. J Immunol Methods. 1999;227:197–198. doi: 10.1016/s0022-1759(99)00081-2. [DOI] [PubMed] [Google Scholar]
- 20.Porgador A, Tzehoval E, Katz A, Vadai E, Revel M, Feldman M, Eisenbach L. Cancer Res. 1992;52:3679–3686. [PubMed] [Google Scholar]
- 21.Fu Y X, Watson G, Jimenez J J, Wang Y, Lopez D M. Cancer Res. 1990;50:227–234. [PubMed] [Google Scholar]
- 22.Zheng H, Fletcher D, Kozak W, Jiang M, Hofmann K J, Conn C A, Soszynski D, Grabiec C, Trumbauer M E, Shaw A, et al. Immunity. 1995;3:9–19. doi: 10.1016/1074-7613(95)90154-x. [DOI] [PubMed] [Google Scholar]
- 23.Fantuzzi G, Zheng H, Faggioni R, Benigni F, Ghezzi P, Sipe J D, Shaw A R, Dinarello C A. J Immunol. 1996;157:291–296. [PubMed] [Google Scholar]
- 24.Horai R, Asano M, Sudo K, Kanuka H, Suzuki M, Nishihara M, Takahashi M, Iwakura Y. J Exp Med. 1998;187:1463–1475. doi: 10.1084/jem.187.9.1463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Fridman R, Kibbey M C, Royce L S, Zain M, Sweeney M, Jicha D L, Yannelli J R, Martin G R, Kleinman H K. J Natl Cancer Inst. 1991;83:769–774. doi: 10.1093/jnci/83.11.769. [DOI] [PubMed] [Google Scholar]
- 26.Sehested M, Hou-Jensen K. Virchows Arch A Pathol Anat Histol. 1981;391:217–225. doi: 10.1007/BF00437598. [DOI] [PubMed] [Google Scholar]
- 27.Weidner N, Semple J P, Welch W R, Folkman J. N Engl J Med. 1991;324:1–8. doi: 10.1056/NEJM199101033240101. [DOI] [PubMed] [Google Scholar]
- 28.Voronov E, Weinstein Y, Benharroch D, Cagnano E, Ofir R, Dobkin M, White R M, Zoller M, Barak V, Segal S, Apte R N. Cancer Res. 1999;59:1029–1035. [PubMed] [Google Scholar]
- 29.Douvdevani A, Huleihel M, Zoller M, Segal S, Apte R N. Int J Cancer. 1992;51:822–830. doi: 10.1002/ijc.2910510526. [DOI] [PubMed] [Google Scholar]
- 30.Apte R N, Douvdevani A, Zoller M, White R M, Dvorkin T, Shimoni N, Fima E, Hacham M, Huleihel M, Benharroch D, et al. Immunol Lett. 1993;39:45–52. doi: 10.1016/0165-2478(93)90163-v. [DOI] [PubMed] [Google Scholar]
- 31.Saijo Y, Tanaka M, Miki M, Usui K, Suzuki T, Maemondo M, Hong X, Tazawa R, Kikuchi T, Matsushima K, Nukiwa T. J Immunol. 2002;169:469–475. doi: 10.4049/jimmunol.169.1.469. [DOI] [PubMed] [Google Scholar]
- 32.Carmeliet P, Dor Y, Herbert J M, Fukumura D, Brusselmans K, Dewerchin M, Neeman M, Bono F, Abramovitch R, Maxwell P, et al. Nature. 1998;394:485–490. doi: 10.1038/28867. [DOI] [PubMed] [Google Scholar]
- 33.Keshet E, Ben-Sasson S A. J Clin Invest. 1999;104:1497–1501. doi: 10.1172/JCI8849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Thornton R D, Lane P, Borghaei R C, Pease E A, Caro J, Mochan E. Biochem J. 2000;350, Part 1:307–312. [PMC free article] [PubMed] [Google Scholar]
- 35.Haddad J J. Eur Cytokine Network. 2002;13:250–260. [PubMed] [Google Scholar]
- 36.Nozaki S, Sledge G W, Jr, Nakshatri H. Biochem Biophys Res Commun. 2000;275:60–62. doi: 10.1006/bbrc.2000.3241. [DOI] [PubMed] [Google Scholar]
- 37.Neufeld G, Kessler O, Vadasz Z, Gluzman-Poltorak Z. Surg Oncol Clin North Am. 2001;10:339–56. , ix. [PubMed] [Google Scholar]
- 38.Dor Y, Djonov V, Abramovitch R, Itin A, Fishman G I, Carmeliet P, Goelman G, Keshet E. EMBO J. 2002;21:1939–1947. doi: 10.1093/emboj/21.8.1939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Harris A L. Nat Rev Cancer. 2002;2:38–47. doi: 10.1038/nrc704. [DOI] [PubMed] [Google Scholar]
- 40.O'Reilly M S, Holmgren L, Shing Y, Chen C, Rosenthal R A, Moses M, Lane W S, Cao Y, Sage E H, Folkman J. Cell. 1994;79:315–328. doi: 10.1016/0092-8674(94)90200-3. [DOI] [PubMed] [Google Scholar]
- 41.O'Reilly M S, Boehm T, Shing Y, Fukai N, Vasios G, Lane W S, Flynn E, Birkhead J R, Olsen B R, Folkman J. Cell. 1997;88:277–285. doi: 10.1016/s0092-8674(00)81848-6. [DOI] [PubMed] [Google Scholar]
- 42.Slaton J W, Perrotte P, Inoue K, Dinney C P, Fidler I J. Clin Cancer Res. 1999;5:2726–2734. [PubMed] [Google Scholar]
- 43.Kleiner D E, Stetler-Stevenson W G. Cancer Chemother Pharmacol. 1999;43,Suppl.:S42–S51. doi: 10.1007/s002800051097. [DOI] [PubMed] [Google Scholar]
- 44.Zucker S, Cao J, Chen W T. Oncogene. 2000;19:6642–6650. doi: 10.1038/sj.onc.1204097. [DOI] [PubMed] [Google Scholar]
- 45.Vlodavsky I, Friedmann Y. J Clin Invest. 2001;108:341–347. doi: 10.1172/JCI13662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Thun M J, Henley S J, Patrono C. J Natl Cancer Inst. 2002;94:252–266. doi: 10.1093/jnci/94.4.252. [DOI] [PubMed] [Google Scholar]
- 47.Scatena M, Giachelli C. Trends Cardiovasc Med. 2002;12:83–88. doi: 10.1016/s1050-1738(01)00151-7. [DOI] [PubMed] [Google Scholar]
- 48.Huang S, Pettaway C A, Uehara H, Bucana C D, Fidler I J. Oncogene. 2001;20:4188–4197. doi: 10.1038/sj.onc.1204535. [DOI] [PubMed] [Google Scholar]
- 49.Coxon A, Bolon B, Estrada J, Kaufman S, Scully S, Rattan A, Duryea D, Hu Y L, Rex K, Pacheco E, et al. Arthritis Rheum. 2002;46:2604–2612. doi: 10.1002/art.10546. [DOI] [PubMed] [Google Scholar]