Abstract
Objective
To compare laparoscopic hernioplasty with two open tension-free hernia repairs.
Summary Background Data
Laparoscopic hernioplasty is associated with a short rehabilitation, but it is a technically difficult procedure. It is unclear if it has advantages over the technically easier open tension-free herniorrhaphy.
Methods
Two hundred ninety-nine men 30 to 75 years old were randomized to undergo laparoscopic totally extraperitoneal hernioplasty (TEP), open operation with mesh-plug and patch, or Lichtenstein’s operation.
Results
Two hundred ninety-four (98%) patients were followed for 19.8 ± 8.6 months. Over 90% of the patients in all groups were operated in day surgery; the rest of the patients were all discharged within 24 hours. Postoperative pain (visual analog score) was lower in the patients undergoing TEP than in those undergoing Lichtenstein and mesh-plug procedures. The median sick-leave period was 5 days in the TEP group, 7 days in the mesh-plug group, and 7 days in the Lichtenstein group. The median time to full recovery was significantly shorter in the TEP group compared to the other two groups. There were no major complications. Two recurrences were found in the TEP group and two in the mesh-plug group.
Conclusions
Laparoscopic hernioplasty is superior to tension-free open herniorrhaphy in terms of postoperative pain and rehabilitation.
Surgery for a groin hernia is the most common operation in general surgery. 1 The recurrence rate in nonspecialized centers is high, 2 and postoperative pain and discomfort are common. 3 With the use of open tension-free hernia surgery with mesh, the recurrence rate has decreased and the rehabilitation period has been reduced compared to sutured repairs. 4 Many different tension-free techniques have been developed, 4–8 and the use of mesh is common and increasing. 9–11 In Sweden and Denmark the most frequently used hernia repair is the Lichtenstein procedure. 12 During the last decade minimally invasive hernioplasties have been developed using either a laparoscopic or an open technique. 6,7,13–16 The learning curve in laparoscopic hernioplasty is long, 17–21 whereas the open operation with a mesh-plug and patch is easier to perform. 7,22 The results from this method have been promising though not yet published in large randomized studies. 23–25
This study was designed to compare three tension-free methods of hernioplasty: laparoscopic totally extraperitoneal hernioplasty (TEP), herniorrhaphy with mesh-plug and patch, and Lichtenstein’s operation. The primary aim was to compare the postoperative rehabilitation variables, with sick leave and time to full recovery as the main variables. The secondary aim was to evaluate if there were any differences in the early recurrence rate or complications.
METHODS
The study was a randomized open trial performed in two hospitals. The patients were randomized to undergo TEP, Perfix mesh-plug and patch, or Lichtenstein’s operation.
Patients
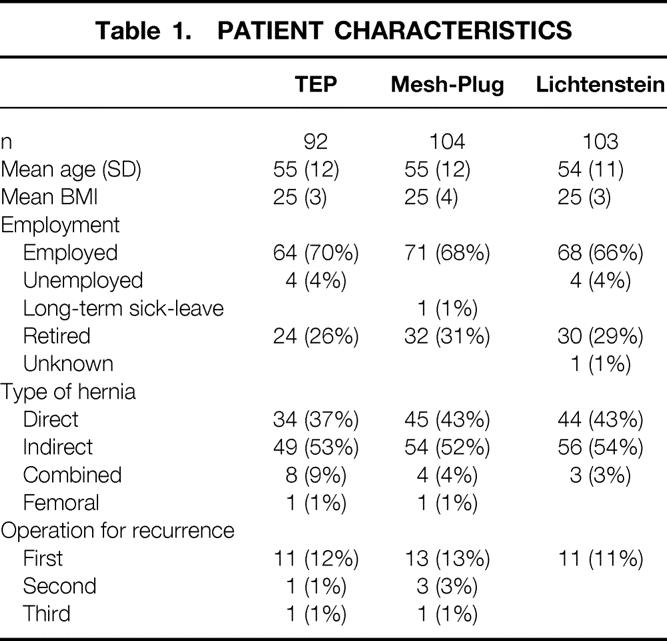
Men aged 30 to 75 years with unilateral inguinal hernia were included in the study. They were determined to be fit for general anesthesia. Patients with a history of major surgery in the lower abdomen other than appendectomy, cancer, or immune deficiency were excluded. Informed consent was obtained from all participants. Two hundred ninety-nine men were randomized between September 1997 and March 2000. The comparative data for the two groups are shown in Table 1. The study was approved by the Ethics Committee of Karolinska Institutet, Stockholm, Sweden.
Table 1.PATIENT CHARACTERISTICS
Randomization and Stratification
The patients were randomized at each hospital by consecutive opening of sealed envelopes. Stratification was made for primary and recurrent hernias. The patients were informed of their treatment assignment directly after the randomization.
Surgical Technique
Ten surgeons, experienced in the Lichtenstein and mesh-plug techniques, participated in the study performing mesh-plug and Lichtenstein operations. Five of these surgeons were also experienced in TEP and performed the laparoscopic operations. Seven TEP, seven mesh-plug, and nine Lichtenstein operations were performed by surgeons in training, assisted by one of the experienced surgeons.
All laparoscopic operations and the majority of the open operations were performed under general anesthesia. Six (6%) patients in the mesh-plug group and three (3%) in the Lichtenstein group had spinal or epidural anesthesia.
TEP
TEP was performed with reusable trocars and instruments. 18 An infraumbilical incision was made and the ipsilateral anterior rectus sheath was opened. A blunt digital dissection was made in the preperitoneal space through the ipsilateral anterior rectus sheath. A blunt trocar with CO2 insufflation and a 30° laparoscope were introduced in the preperitoneal space, and the dissection was continued by using the laparoscope under direct vision. Two trocars were then introduced infraumbilically into the preperitoneal space. Dissection of the preperitoneal space was performed medially across the midline and laterally cranial to the anterior-superior iliac spine. The hernia sac was reduced and the peritoneum was retracted cranially. A 10 × 15-cm polypropylene mesh (Prolene, Ethicon GmbH) was introduced into the preperitoneal space, covering the inguinal floor. The CO2 was exsufflated and the anterior rectus sheath was closed with 2-0 polyglactin (Vicryl, Ethicon GmbH). The skin was closed with 3-0 polyglactin (Vicryl Rapid, Ethicon GmbH).
Mesh-Plug
The mesh-plug operation was performed as described by Robbins and Rutkow 23 using a large Bard Perfix plug-and-patch (C. R. Bard, Inc., Cranston, RI) We used interrupted sutures with 2-0 polypropylene (Prolene) to secure the plug, but the patch was not fixed with sutures. After closure of the external oblique and Scarpa’s fascia, the skin was closed with a running 3-0 polyglactin (Vicryl Rapid).
Lichtenstein
The Lichtenstein operation was performed as described by Amid et al. 5 using 2-0 polypropylene (Prolene) to secure the mesh. We used a 7.5 × 15-cm polypropylene mesh (Bard Mesh) that was trimmed to match the size of the inguinal floor if necessary. After closure of the external oblique and Scarpa’s fascia, the skin was closed with a running 3-0 polyglactin (Vicryl Rapid).
Postoperative Care
All patients received bupivacaine in the wound edges at the end of the procedure. Postoperative pain was controlled with standard oral medication: paracetamol 1 g qid and tramadol 50 mg three times daily on the day of surgery and the first postoperative day. Extra analgesia was recorded in the protocol.
Perioperative Parameters
Pain was recorded using a visual analog scale (VAS, 0–10) in the hospital at 2 and 4 hours after the operation. Day surgery patients were called by a nurse, who recorded the VAS score on the first postoperative morning. Inpatients had the VAS score recorded in the hospital. All patients received the same postoperative instructions and were encouraged to return to work and normal activities as soon as possible.
Follow-Up
Questionnaires were given to the patients at hospital discharge; the questionnaires were to be returned within 3 months. Questions about the period of sick leave and time to full recovery (when the patient subjectively felt fully recovered) were included.
Long-term follow-up was carried out by validated questionnaires 26 that were mailed to the patients. An independent surgeon in the hospital saw patients with any complaints, such as pain or a lump in the groin. Recurrence was defined as a bulge or weakness in the operative area exacerbated by a Valsalva maneuver and necessitating further operation or use of a truss. 27
Data Handling
Data were collected according to standardized preprinted pro-formas at each hospital. They were collected by the study coordinating center, where the transfer to computer data files and statistical analysis were performed.
Statistical Analysis
With a two-sided test with a power of 80% and an alpha level of less than 0.05 ± 0.93, 80 patients were needed in each group to detect a 2-day difference in sick leave. Approximately 80% of the patients were employed. The sample size was thus calculated to be 100 patients in each group.
All data were analyzed using Statistica version 5.5 A (StatSoft Inc., Tulsa, OK) software. All patients, including those who were lost to follow-up or declined postoperative examination, were included in the data analysis. The Kruskal-Wallis analysis of variance was used to analyze the continuous variables and visual analog scale scores, with multiple comparisons according to Siegel-Castellan to distinguish between the variables if a level of significance was found. The chi-square test, exact chi-square test, and Fisher exact test were used to assess the differences between categorical data. P < .05 was considered statistically significant.
RESULTS
In the TEP group 90 patients (97%), in the mesh-plug group 97 patients (93%), and in the Lichtenstein group 95 patients (92%) were operated on in day surgery; the rest were all discharged within 24 hours. Two hundred ninety-four patients (98%) were followed up for 19.8 ± 8.6 months; 291 answered the questionnaire and 3 were interviewed by telephone. One patient in the TEP group and one in the Lichtenstein group died during the study period; neither death was related to the hernioplasty. One patient in each group was lost to follow-up. Sixty-nine patients were seen by an independent surgeon. Another five patients were supposed to be seen by a surgeon in accordance with the questionnaire but declined postoperative examination.
Perioperative Data
Mean operative time was significantly shorter in the mesh-plug group at 36 minutes (range 19–88) compared to 50 minutes (range 25–150) in the TEP group and 45 minutes (range 24–100) in the Lichtenstein group (P < .0001). There were no perioperative complications and no conversions to another method in any group.
Postoperative Data
Seventeen patients (18%) in the TEP group, 26 (25%) in the mesh-plug group, and 20 (19%) in the Lichtenstein group required extra analgesia during the 4 hours immediately after surgery. The VAS score was lower in the TEP patients than the Lichtenstein patients after 2 hours (P = .009) and 4 hours (P = .015) and lower compared to the Lichtenstein and mesh-plug patients the next morning (P < .0001) (Fig. 1).
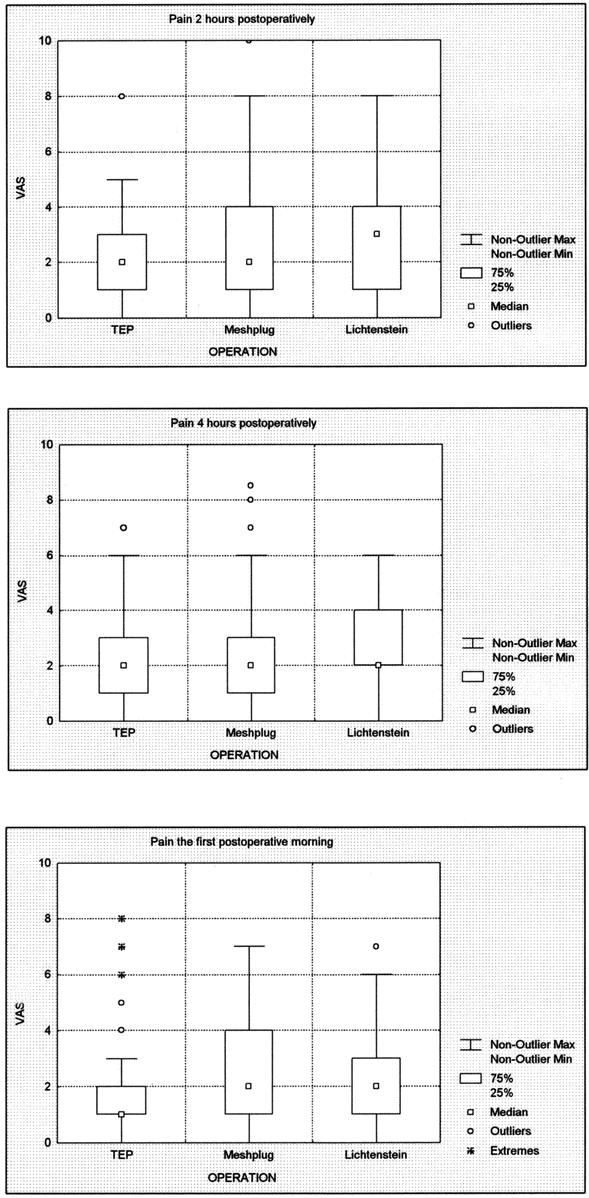
Figure 1. Pain 2 and 4 hours after surgery and the morning after surgery. VAS, visual analog scale.
The median sick-leave period was 5 days (range 0–30) in the TEP group, 7 days (range 0–150) in the mesh-plug group, and 7 days (range 0–70) in the Lichtenstein group. The difference between the TEP and Lichtenstein groups was statistically significant (P = .02).
Eighty-four patients (91%) in the TEP group, 94 (90%) in the mesh-plug group, and 86 (83%) in the Lichtenstein group assessed their time to full recovery in the questionnaire. The median time to full recovery was significantly shorter in the TEP group at 14 days (range 0–80) compared to the mesh-plug group (24.5 days, range 0–122) and the Lichtenstein group (28.5 days, range 1–365) (P < .0001).
There were no major complications. The postoperative complications (<30 days) recorded are shown in Table 2. There were no significant differences between the groups. None of the hematomas needed evacuation. One seroma in the mesh-plug group was reoperated acutely with an open exploration because the surgeon who was on call suspected an acute recurrence. All infections healed without surgical intervention. One patient had a dyspneic attack after TEP; nothing abnormal was found, and the patient was discharged a few hours later. The patients with prolonged pain had recovered completely before follow-up.
Table 2.EARLY COMPLICATIONS
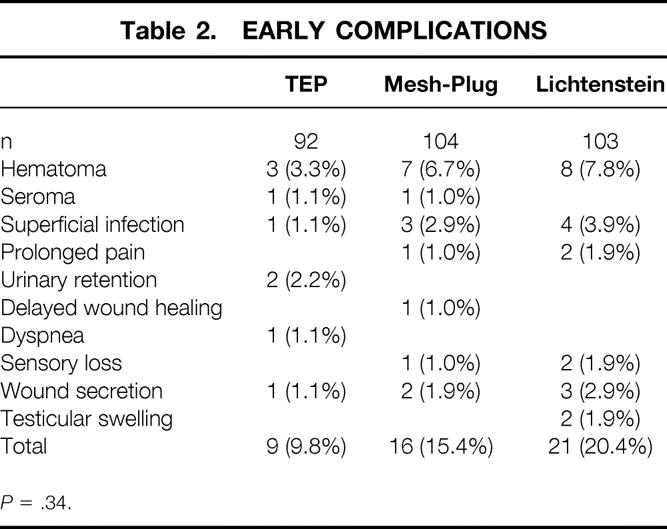
P = .34.
Long-term complications, including recurrences, are shown in Table 3. There were no significant differences between the groups. None of the patients with pain or mesh-related problems were permanently disabled or needed a reoperation. No patient has chronic pain. One patient in the TEP group (recurrent, indirect hernia) was operated on after 21 months because of a hydrocele of the cord. No recurrent hernia was found. There was one early recurrence in the TEP group 5 months after a repair of a primary direct hernia and one recurrence after follow-up (a repair of a primary combined hernia; 2.2%). In the mesh-plug group there were two recurrences, both after repair of primary indirect hernias (1.9%). In the Lichtenstein group there were no recurrences.
Table 3.LONG-TERM COMPLICATIONS
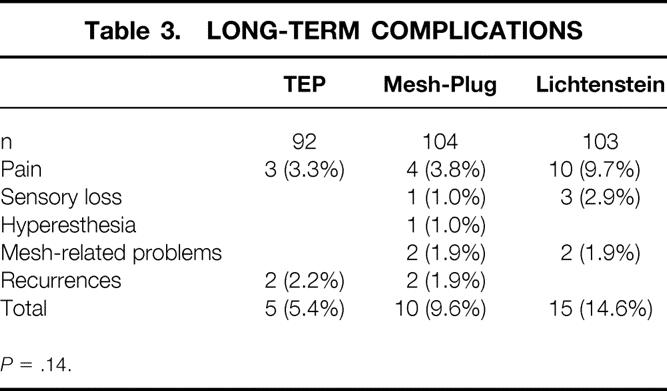
P = .14.
DISCUSSION
Laparoscopic hernia repair has been criticized for technical difficulties, cost, and a long learning curve. 17–21 The indications for laparoscopic hernia repair have been debated. 28–30 Many of the publications that have been the foundation for the debate have been studies using the transabdominal preperitoneal (TAPP) technique in a randomized design compared with a conventional open repair with or without mesh. 16 In TAPP the abdominal cavity is entered, leading to the possibility of injury to the intraperitoneal contents. 31–33 In the present study, we chose to use TEP since it does not involve entering the abdominal cavity.
In laparoscopic hernioplasty it has been common to use disposable instruments, which may increase the direct cost (the cost for the hospital). However, in our study we used only reusable instruments, including trocars. Thus, the only cost for disposable material differing between the methods is the cost of the mesh. During the study period this was $30 in the TEP group, $90 in the mesh-plug group, and $42 in the Lichtenstein group. No other economic calculations were performed.
In our study, the laparoscopic repair took longer than the mesh-plug repair but not longer than the Lichtenstein repair. We do not consider the shorter operative time in the mesh-plug group to have any clinical relevance. The economic impact of a shorter operative time differs between healthcare systems and between countries. In our healthcare system the relatively small difference in operative time between the groups does not have much economic impact.
In this study we showed that there was less postoperative pain and shorter time to full recovery in TEP compared to both open methods. This is consistent with a recent meta-analysis showing that laparoscopic repair had a shorter rehabilitation than open repair. 16 In this meta-analysis the laparoscopic repair took a longer time to perform.
In other studies, laparoscopic repair has had shorter sick-leave periods, but some of these studies have been comparisons with sutured repairs, which might influence the outcome. 16 In the present study, the sick leave was short in all groups, but it was significantly shorter in the TEP group than in the Lichtenstein group.
One of the problems in inguinal hernia research is that the patients must be followed for a significant period to evaluate the recurrence rate and the rate of late postoperative morbidity. Having all the patients return to the hospital for a physical examination is time-consuming and requires economic resources both for the patients and the healthcare system. Using a questionnaire for follow-up has been validated in two previous studies to be a good alternative to clinical visits. 26,34
There was no statistically significant difference between the groups in terms of overall late complications. However, there was a tendency toward a higher incidence of pain and sensory loss in the Lichtenstein group than in the other groups. This may be an important finding, but it needs further investigation. One hypothesis is that the dissection and fixation in the Lichtenstein method is more extensive than the other two, which could increase the risk of nerve injuries leading to pain and/or sensory loss. We found no significant differences in the recurrence rates, but the number of patients in this study did not allow an assessment of the methods regarding recurrence rates.
In conclusion, our results indicate that laparoscopic hernioplasty is superior to tension-free open herniorrhaphy with mesh-plug and patch or Lichtenstein’s operation in terms of postoperative pain and rehabilitation.
Footnotes
Correspondence: Dr Sven Bringman, MD, MISS (Minimally Invasive Surgery Stockholm), Center for Surgical Sciences, K53, Karolinska Institutet at Huddinge University Hospital, SE-141 86 Stockholm, Sweden.
E-mail: sven.bringman@cfss.ky.se
Accepted for publication May 10, 2002.
References
- 1.Rutkow IM. Surgical operations in the United States. Then (1983) and now (1994). Arch Surg 1997; 132: 983–990. [DOI] [PubMed] [Google Scholar]
- 2.Nilsson E, Kald A, Anderberg B, et al. Hernia surgery in a defined population: a prospective three-year audit. Eur J Surg 1997; 163: 823–829. [PubMed] [Google Scholar]
- 3.Bay-Nielsen M, Perkins FM, Kehlet H. Pain and functional impairment 1 year after inguinal herniorrhaphy: a nationwide questionnaire study. Ann Surg 2001; 233: 1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Collaboration EH. Mesh compared with non-mesh methods of open groin hernia repair: systematic review of randomized controlled trials. Br J Surg 2000; 87: 854–859. [DOI] [PubMed] [Google Scholar]
- 5.Amid PK, Shulman AG, Lichtenstein IL. Open. “tension-free” repair of inguinal hernias: the Lichtenstein technique. Eur J Surg 1996; 162: 447–453. [PubMed] [Google Scholar]
- 6.Kugel RD. Minimally invasive, nonlaparoscopic, preperitoneal, and sutureless, inguinal herniorrhaphy. Am J Surg 1999; 178: 298–302. [DOI] [PubMed] [Google Scholar]
- 7.Rutkow IM, Robbins AW. “Tension-free” inguinal herniorrhaphy: a preliminary report on the “mesh plug” technique. Surgery 1993; 114: 3–8. [PubMed] [Google Scholar]
- 8.Stoppa R, Petit J, Abourachid H, et al. [Original procedure of groin hernia repair: interposition without fixation of Dacron tulle prosthesis by subperitoneal median approach]. Chirurgie 1973; 99: 119–123. [PubMed] [Google Scholar]
- 9.[The Danish hernia database–the first year]. Ugeskr Laeger 2000; 162:1552–1555. [PubMed]
- 10.Hair A, Duffy K, McLean J, et al. Groin hernia repair in Scotland. Br J Surg 2000; 87: 1722–1726. [DOI] [PubMed] [Google Scholar]
- 11.Nilsson E, Haapaniemi S, Gruber G, et al. Methods of repair and risk for reoperation in Swedish hernia surgery from 1992 to 1996. Br J Surg 1998; 85: 1686–1691. [DOI] [PubMed] [Google Scholar]
- 12.Bay-Nielsen M, Nordin P, Nilsson E, et al. Operative findings in recurrent hernia after a Lichtenstein procedure. Am J Surg 2001; 182: 134–136. [DOI] [PubMed] [Google Scholar]
- 13.Darzi A, Nduka CC. Endoscopically guided percutaneous repair of inguinal hernia through a 2-cm incision. Minihernia repair. Surg Endosc 1997; 11: 782–784. [DOI] [PubMed] [Google Scholar]
- 14.Geis WP, Crafton WB, Novak MJ, et al. Laparoscopic herniorrhaphy: results and technical aspects in 450 consecutive procedures. Surgery 1993; 114: 765–774. [PubMed] [Google Scholar]
- 15.Go PM. Overview of randomized trials in laparoscopic inguinal hernia repair. Semin Laparosc Surg 1998; 5: 238–241. [DOI] [PubMed] [Google Scholar]
- 16.Collaboration EH. Laparoscopic compared with open methods of groin hernia repair: systematic review of randomized controlled trials. Br J Surg 2000; 87: 860–867. [DOI] [PubMed] [Google Scholar]
- 17.Edwards CC, 2nd, Bailey RW. Laparoscopic hernia repair: the learning curve. Surg Laparosc Endosc Percut Techn 2000; 10: 149–153. [DOI] [PubMed] [Google Scholar]
- 18.Bringman S, Ek A, Haglind E, et al. Is a dissection balloon beneficial in totally extraperitoneal endoscopic hernioplasty (TEP)? A randomized prospective multicenter study. Surg Endosc 2001; 15: 266–270. [DOI] [PubMed] [Google Scholar]
- 19.Voitk AJ. The learning curve in laparoscopic inguinal hernia repair for the community general surgeon. Can J Surg 1998; 41: 446–450. [PMC free article] [PubMed] [Google Scholar]
- 20.Wright D, O’Dwyer PJ. The learning curve for laparoscopic hernia repair. Semin Laparosc Surg 1998; 5: 227–232. [DOI] [PubMed] [Google Scholar]
- 21.Liem MS, van Steensel CJ, Boelhouwer RU, et al. The learning curve for totally extraperitoneal laparoscopic inguinal hernia repair. Am J Surg 1996; 171: 281–285. [DOI] [PubMed] [Google Scholar]
- 22.Bringman S, Ramel S, Nyberg B, et al. Introduction of herniorrhaphy with mesh plug and patch. Eur J Surg 2000; 166: 310–312. [DOI] [PubMed] [Google Scholar]
- 23.Robbins AW, Rutkow IM. Mesh plug repair and groin hernia surgery. Surg Clin North Am 1998; 78: 1007–1023. [DOI] [PubMed] [Google Scholar]
- 24.Khoury N. A randomized prospective controlled trial of laparoscopic extraperitoneal hernia repair and mesh-plug hernioplasty: a study of 315 cases. J Laparoendosc Adv Surg Tech A 1998; 8: 367–372. [DOI] [PubMed] [Google Scholar]
- 25.Kingsnorth AN, Porter CS, Bennett DH, et al. Lichtenstein patch or Perfix plug-and-patch in inguinal hernia: a prospective double-blind randomized controlled trial of short-term outcome. Surgery 2000; 127: 276–283. [DOI] [PubMed] [Google Scholar]
- 26.Kald A, Nilsson E. Quality assessment in hernia surgery. Qual Assur Health Care 1991; 3: 205–210. [DOI] [PubMed] [Google Scholar]
- 27.Marsden A. Inguinal hernia: A three-year review of two thousand cases. Br J Surg 1962; 49: 384–394. [DOI] [PubMed] [Google Scholar]
- 28.Beattie DK, Foley RJ, Callam MJ. Future of laparoscopic inguinal hernia surgery. Br J Surg 2000; 87: 1727–1728. [DOI] [PubMed] [Google Scholar]
- 29.Arvidsson D, Smedberg S. Laparoscopic compared with open hernia surgery: complications, recurrences and current trends. Eur J Surg 2000; Suppl: ( 585) 40–47. [DOI] [PubMed] [Google Scholar]
- 30.Meakins JL, Barkun JS. Old and new ways to repair inguinal hernias. N Engl J Med 1997; 336: 1596–1597. [DOI] [PubMed] [Google Scholar]
- 31.Felix EL, Michas CA, Gonzalez MH, Jr. Laparoscopic hernioplasty. TAPP vs. TEP. Surg Endosc 1995; 9: 984–989. [DOI] [PubMed] [Google Scholar]
- 32.Laparoscopic versus open repair of groin hernia: a randomised comparison. The MRC Laparoscopic Groin Hernia Trial Group. Lancet 1999; 354(9174):185–190. [PubMed]
- 33.Ramshaw BJ, Tucker JG, Conner T, et al. A comparison of the approaches to laparoscopic herniorrhaphy. Surg Endosc 1996; 10: 29–32. [DOI] [PubMed] [Google Scholar]
- 34.Haapaniemi S, Nilsson E. Recurrence and pain three years after groin hernia repair: Validation of postal questionnaire and selective physical examination as a method of follow-up. Eur J Surg 2002; 168: 22–28. [DOI] [PubMed] [Google Scholar]


