Abstract
Five Listeria monocytogenes isolates (CLIP 21369, CLIP 73298, CLIP 74811, CLIP 75679, and CLIP 79372) were found to be resistant to fluoroquinolones during the screening for antibiotic resistance of 488 L. monocytogenes isolates from human cases of listeriosis in France. On the basis of a fourfold or greater decrease in the ciprofloxacin MIC in the presence of reserpine, fluoroquinolone resistance was attributed to active efflux of the drugs. The lde gene (Listeria drug efflux; formerly lmo2741) encodes a 12-transmembrane-segment putative efflux pump belonging to the major facilitator superfamily of secondary transporters that displayed 44% identity with PmrA from Streptococcus pneumoniae. Insertional inactivation of the lde gene in CLIP 21369 indicated that the corresponding protein was responsible for fluoroquinolone resistance and was involved in the level of susceptibility to dyes such as ethidium bromide and acridine orange.
Listeria monocytogenes is widely distributed in the environment and can cause serious human infections, such as bacteremia and central nervous system infections, primarily in neonates and immunocompromised adults, and abortions (22). Food-borne transmission is recognized as the main route of acquisition of the infection during epidemic and sporadic listerioses (3, 18). Listeriosis differs from most food-borne diseases by its high fatality rate (20 to 30% of cases), despite the administration of appropriate antibiotics (3, 9). L. monocytogenes is generally susceptible to a wide range of antibiotics but is not susceptible to cephalosporins and fosfomycin (8). However, during the last few years, increasing numbers of strains resistant to one or more antibiotics have been reported (1, 2, 8, 11, 19, 20).
Although indications for the use of fluoroquinolones do not include listeriosis, they can, due to their increasing use for other pathologies such as respiratory tract infections, select resistant Listeria. In gram-positive bacteria, resistance usually results from mutational alterations in the so-called quinolone resistance-determining regions (QRDRs) of the intracellular targets of fluoroquinolones, the type II DNA topoisomerases gyrase and topoisomerase IV, or active export of the drugs via efflux pumps (12). We have detected ciprofloxacin-resistant L. monocytogenes clinical isolates and characterized the efflux pump involved in resistance.
(An initial report of this work was presented at the 41st Interscience Conference on Antimicrobial Agents and Chemotherapy [S. Godreuil, M. Galimand, G. Gerbaud, and P. Courvalin, Abstr. 41st Intersci. Conf. Antimicrob. Agents Chemother., abstr. UL-11, 2001].)
MATERIALS AND METHODS
Strains, plasmids, and growth conditions.
Screening of 488 L. monocytogenes isolates responsible for human listeriosis in France for resistance to fluoroquinolones was carried out on brain heart infusion agar (Difco Laboratories, Detroit, Mich.) containing 4 μg of ciprofloxacin per ml. Strains that were found to be resistant and susceptible L. monocytogenes EGD were studied (Table 1). The strains were serotyped with antibodies made in the Laboratoire des Listeria and by the agglutination technique, as described elsewhere (23). Escherichia coli TOP10 plasmid PCR2 (Invitrogen, Paisley, United Kingdom), which is a vector used for cloning of PCR products, and plasmid pKSV7, which is thermosensitive for replication (24), were used. The E. coli strains were grown at 37°C, and the L. monocytogenes strains were grown at 30, 37, or 43°C. The strains were grown in brain heart infusion broth and agar supplemented with ampicillin at 100 μg/ml and kanamycin at 20 μg/ml for E. coli and chloramphenicol at 8 μg/ml for L. monocytogenes.
TABLE 1.
Properties of the strains tested
| L. monocytogenes | Serovar | Yr of isolation | MIC (μg/ml)a
|
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Ciprofloxacin
|
Norfloxacin
|
Sparfloxacin
|
Moxifloxacin
|
Ethidium bromide
|
Acridine orange
|
|||||||||
| − | + | − | + | − | + | − | + | − | + | − | + | |||
| EGDe | 1/2a | 1964 | 0.5-1 | 0.50-0.75 | 2-3 | 2-3 | 1-1.5 | 0.75-1 | 0.25-0.38 | 0.19-0.25 | 10 | 10 | 20 | 20 |
| CLIP 21369 | 1/2b | 1992 | 8-16 | 0.75-1 | 48-64 | 3-4 | 1-1.5 | 0.75-1 | 0.25-0.38 | 0.19-0.25 | 200 | 100 | 80 | 40 |
| CLIP 73298 | 1/2a | 1997 | 8-16 | 0.75-1 | 48-64 | 3-4 | 1-1.5 | 0.50-0.75 | 0.25-0.38 | 0.19-0.25 | 200 | 100 | 80 | 40 |
| CLIP 74811 | 4b | 1997 | 6-8 | 0.50-0.75 | 32-64 | 2-4 | 1-1.5 | 0.50-0.75 | 0.25-0.38 | 0.19-0.25 | 200 | 100 | 80 | 40 |
| CLIP 75679 | SNDb | 1997 | 6-8 | 0.50-0.75 | 32-48 | 2-3 | 1-1.5 | 0.50-0.75 | 0.25-0.38 | 0.19-0.25 | 200 | 100 | 80 | 40 |
| CLIP 79372 | 1/2b | 1999 | 6-8 | 0.50-0.75 | 16-24 | 2-4 | 1-1.5 | 0.75-1 | 0.25-0.38 | 0.19-0.25 | 200 | 100 | 80 | 40 |
| BM4497 | SND | NAc | 0.5-1 | 0.50-0.75 | 2-4 | 2-3 | 1-1.5 | 0.50-0.75 | 0.25-0.38 | 0.19-0.25 | 100 | 100 | 40 | 40 |
Values are ranges from three independent determinations; consistent values were obtained for dyes. −, without reserpine; +, with 10 μg of reserpine per ml.
SND, serovar not designated.
NA, not applicable.
Susceptibility testing.
The isolates were tested for their antibiotic susceptibilities by disk diffusion on Mueller-Hinton agar (Bio-Rad, Marnes-la-Coquette, France). A minimum of three independent determinations of the MICs of the antimicrobial agents and dyes were determined on Mueller-Hinton agar by the E-test (AB Biodisk France, Combourg, France) or by agar dilution with or without reserpine (10 μg/ml) with 104 CFU per spot after 24 h of incubation at 37 or 43°C (25).
DNA preparation and transformation.
Purification of plasmid DNA was performed by using the Wizard minipreps DNA kit (Promega, Madison, Wis.). Total DNA of L. monocytogenes was prepared as described previously (20). Restriction with endonucleases was according to the recommendations of the supplier. Extraction of DNA fragments separated by agarose gel electrophoresis was carried out with a Sephaglas BandPrep kit (Amersham-Pharmacia Biotech, Saint Quentin en Yvelines, France). L. monocytogenes DNA in plugs was digested with AscI or ApaI, and large restriction fragments were separated by electrophoresis in a CHEF-DRIII system (Bio-Rad Laboratories, Richmond, Calif.) by using an electric field of 6 V/cm and an angle of 120°. The initial and final pulse times were 4 and 40 s, respectively. Migration of the DNA fragments was performed in a 1% agarose gel in 0.5× Tris-borate-EDTA at 14°C (6).
Amplification of DNA was performed in a 2400 thermal cycler (Perkin-Elmer Cetus, Norwalk, Conn.), with Pfu DNA polymerase (Stratagene, La Jolla, Calif.), as recommended by the manufacturer. PCR elongation times and temperatures were adjusted according to the expected size of the PCR product and the nucleotide sequences of the primers, respectively.
The QRDRs of the gyrA and gyrB genes for DNA gyrase and the parC and parE genes for DNA topoisomerase IV were amplified by PCR with specific primers (Table 2) and chromosomal DNA of fluoroquinolone-resistant and -susceptible L. monocytogenes strains as the template.
TABLE 2.
Primers used for PCR and sequencing
| Primer | Sequence (5′-3′)a | Location |
|---|---|---|
| gyrA-F | AGTGTAATTGTTGCCCG | bp 82-98 of gyrA |
| gyrA-R | ATATCGCCATCAACCGA | bp 350-334 of gyrA |
| gyrB-F | AAGCGCGCGCGTGAAGT | bp 1192-1208 of gyrB |
| gyrB-R | CGAGATTTAGAAACGTC | bp 1499-1483 of gyrB |
| parC-F | GAACGTGCGCTTCCAGA | bp 91-107 of parC |
| parC-R | GTTGCATAACCAGCGGA | bp 539-523 of parC |
| parE-F | GGAAAATTAACGCCAGC | bp 1222-1238 of parE |
| parE-R | TCGGTCATGATAACTAC | bp 1499-1483 of parE |
| lmo-F | ATCGTGAACTTAATGGTGG | 198 bp upstream from lde start codon |
| lmo-R | ATCCTCATATAACTCAAGCG | 112 bp downstream from lde stop codon |
| M13-F | GTTGTAAAACGACGGCCAGT | Used for pCR2 and pKSV7 vectors |
| M13-R | TCACACAGGAAACAGCTATGA | Used for pCR2 and pKSV7 vectors |
The primers were designed from the sequence of L. monocytogenes EGDe (GenBank accession number AL591824).
E. coli transformation was performed by the protocol provided by Invitrogen, and electrotransformation of L. monocytogenes was as described previously (16) and was done with a Gene Pulser apparatus (Bio-Rad).
Insertional mutagenesis of lde gene.
A fragment internal to the lde gene of L. monocytogenes CLIP 21369 was amplified with the specific oligodeoxynucleotides LDE-F (5′-GGGGTACCCCAGAATTTGTATGTTGTCTGGG-3′), which harbors a KpnI site (underlined), and LDE-R (5′-CGGGATCCCGTACGAGGAAGATCTCCGTA-3′), which contains a BamHI site (underlined). After digestion of the 1,105-bp PCR product with KpnI and BamHI, the fragment was cloned into similarly digested pKSV7 DNA. The recombinant plasmid pAT778 DNA was introduced into CLIP 21369 by electrotransformation, and transformants were selected for chloramphenicol resistance at 30°C. At 43°C chloramphenicol resistance in transformants can be maintained only following integrative recombination of the plasmid. Total DNA from three chloramphenicol-resistant clones was analyzed by PCR with the M13 reverse and forward primers and with two specific primers whose sequences are complementary to the sequences of the flanking regions of the lde gene in the L. monocytogenes chromosome (Table 2). The sequences of the amplification products were determined.
DNA sequence determination and analysis.
DNA sequencing was performed with a CEQ 2000 DNA analysis system automatic sequencer (Beckman Coulter, Palo Alto, Calif.). Nucleotide sequence data were analyzed with the GCG sequence analysis software package (version 10.1; Genetics Computer Group, Madison, Wis.). BLAST program searches were performed by using the National Center for Biotechnology Information website (http://www.ncbi.nlm.nih.gov). Transmembrane sequences (TMSs) were identified by using the TMHMM program at ExPASy (http://www.expasy.ch/). Multiple-sequence alignment was performed with the ClustalW program (version 1.82) at the Institut Pasteur website (http://www.bioweb.pasteur.fr/).
RESULTS AND DISCUSSION
Properties of the L. monocytogenes strains.
Screening of clinical L. monocytogenes isolates for fluoroquinolone resistance led to the detection of five ciprofloxacin-resistant strains (Table 1). The disk agar diffusion test showed that the five isolates were susceptible to ampicillin, chloramphenicol, erythromycin, gentamicin, kanamycin, minocycline, streptomycin, tetracycline, trimethoprim, and vancomycin (data not shown). The clinical isolates belonged to various serovars (Table 1), and pulsed-field gel electrophoresis of total DNA after digestion with the AscI or ApaI restriction endonuclease revealed different profiles (data not shown). These results indicate that the resistant isolates were not clonally related.
The MICs of fluoroquinolones and dyes for the clinical isolates and susceptible strain EGDe were determined by the E-test and agar dilution, respectively (Table 1). The clinical isolates were resistant to ciprofloxacin and norfloxacin, and in the presence of reserpine, a fourfold or greater decrease in the level of resistance to these hydrophilic quinolones was observed. By contrast, the MICs of relatively hydrophilic agents (levofloxacin and moxifloxacin) and hydrophobic drugs (gatifloxacin, sparfloxacin, and trovafloxacin) (Table 1 and data not shown) were not significantly altered (onefold or less decrease). These data, together with the reproducible twofold reduction in the MICs of the dyes tested, suggested that efflux was responsible for the resistance.
Partial sequencing of gyr and par genes.
Pairs of primers designed from the genome of L. monocytogenes EGDe (Table 2) were used to amplify and sequence the QRDRs of gyrA, gyrB, parC, and parE. No differences in the sequences of susceptible strain EGDe (5, 13) and the five ciprofloxacin-resistant isolates were found (data not shown).
Characterization of lde gene.
In gram-positive bacteria, four multidrug efflux transporters that use the proton motive force present across the cytoplasmic membrane to extrude a variety of toxic compounds including fluoroquinolones and dyes have been described: Bmr from Bacillus subtilis (15), NorA from Staphylococcus aureus (26), PmrA from Streptococcus pneumoniae (4), and EmeA from Enterococcus faecalis (10). They belong to the major facilitator superfamily (MFS) of secondary multidrug transporters, share a common structure with 12 TMSs, and are closely related phylogenetically (17, 21).
The family-specific motifs of the MFS proteins were used to identify structural genes for putative multidrug exporter proteins in the genome of L. monocytogenes EGDe: (i) a search for the gxxxGPxxGGxl C motif (where x is any amino acid, a capital letter indicates that the amino acid occurs in >70% of the examined sequences, and a lowercase letter indicates that the amino acid occurs in <40% of the examined sequences) for multidrug transporters resulted in the identification of 10 genes for multidrug exporter proteins; (ii) Kyte-Doolittle hydropathy plots detected five 14-TMS and five 12-TMS exporters; and (iii) Blast comparison of the 12-TMS putative efflux pumps identified the lde gene (formerly lmo2741 [5]), which encodes a 402-amino-acid protein that displayed 44% identity with PmrA from S. pneumoniae (Table 3).
TABLE 3.
Identities between the proteins deduced from the lmo gene of L. monocytogenes EGDe and those from 12-TMS MFS-type efflux proteins from gram-positive bacteria
| Sequence compared | % Identitya
|
|||
|---|---|---|---|---|
| Bmr | NorA | EmeA | PmrA | |
| Lmo 0839 | 29 | 25 | 27 | 26 |
| Lmo 0872 | 22 | 24 | 21 | 26 |
| MdrL (Lmo 1409) | 24 | 25 | 26 | 25 |
| Lmo 2377 | 26 | 24 | 25 | 32 |
| Lde (Lmo 2741) | 25 | 24 | 29 | 44 |
Bmr, from B. subtilis (GenBank accession number L25604); NorA, from S. aureus (GenBank accession number AB019536); EmeA, from E. faecalis (10); PmrA, from S. pneumoniae (GenBank accession number AJ007367); MdrL, from L. monocytogenes (14); Lde, from L. monocytogenes EGDe (this study and GenBank accession number AL591824).
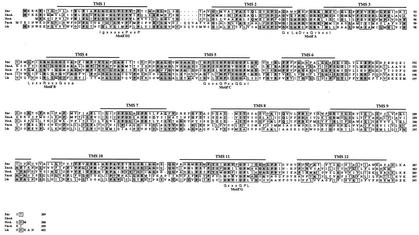
The sequence alignments of the Bmr, NorA, EmeA, PmrA, and Lde proteins are shown in Fig. 1. TMS prediction with the TMHMM program indicated that the 12 TMSs of the Lde efflux pump were at positions similar to those of other 12-TMS proton-dependent efflux pumps (17), with the N and C termini located in the cytoplasm. The translocase consensus sequence (motif A) located in the loop between TMS 2 and TMS 3 and the drug extrusion consensus sequence (motif C) at the end of TMS 5 were conserved in all five sequences. Other motifs, in particular, D2 and G, that are exclusive to the 12-TMS family suggested that Lde is a new member of MFS family 2, which consists of 12-TMS exporters (17, 21).
FIG. 1.
Alignment of the deduced sequences of 12-TMS MFS proteins from gram-positive bacteria. Bmr, from B. subtilis (GenBank accession number L25604); EmeA, from E. faecalis (10); NorA, from S. aureus (GenBank accession number AB019536); PmrA, from S. pneumoniae (GenBank accession number AJ007367); Lde, from L. monocytogenes EGDe (this study and GenBank accession number AL591984). Identical amino acids are indicated by boldface letters on a black background, and conservative substitutions are indicated by letters on a grey background. The horizontal lines above the alignment indicate the locations of the 12 TMSs (1 to 12). Highly conserved motifs (motifs A, B, C, D2, and G) are displayed below the alignment.
Inactivation of Lde efflux system.
To determine if the Lde pump is involved in resistance to fluoroquinolones and dyes, we inactivated the lde gene by insertion. Two specific primers, LDE-F and LDE-R, were used to amplify a 1,105-bp fragment internal to lde that was ligated into vector pKSV7, which is thermosensitive for replication, to generate pAT778. Plasmid pAT778 DNA was introduced into CLIP 21369 by electrotransformation, and at a high temperature homologous recombination in the chromosome for disruption of lde was favored. Transformants resistant to chloramphenicol at 43°C were found to be susceptible to fluoroquinolones by disk diffusion. Clones were analyzed by PCR and sequencing; and strain BM4497, which has a single integrated copy of pAT778 in the lde gene, was studied further (data not shown).
The MICs of fluoroquinolones and dyes for strain BM4497 were determined. The strain was three- to fourfold more sensitive than parental strain CLIP 21369 to ciprofloxacin and norfloxacin and two times more sensitive to dyes, and its susceptibility was not affected by the presence of reserpine (Table 1). These results indicate that lde is responsible for fluoroquinolone resistance and, in part, for acridine orange and ethidium bromide resistance in L. monocytogenes CLIP 21369. The lde gene was found by PCR in all six strains of L. monocytogenes examined, irrespective of their susceptibilities to quinolones. It is therefore likely that resistance results from an increase in the level of expression of the pump.
In summary, we have demonstrated that lde encodes a multidrug efflux pump associated with resistance to hydrophilic fluoroquinolones in L. monocytogenes. Because of the ubiquitous distribution of L. monocytogenes, this bacterial species is exposed to a wide variety of drugs, and thus, active efflux could contribute to the adaptation of Listeria to these environmental challenges (14). Trends in the use of antimicrobials in France between 1980-1981 and 1990-1991 revealed that the overall rate of antibiotic use increased by 3.7% a year. During that time, the rate of use of all quinolones increased by 5.7% per year, even when the rate of use of nonfluorated quinolones decreased by 4.7% (7). Our observations indicate that increasing use of fluoroquinolones can select resistant mutants in nontarget species.
Acknowledgments
This work was supported in part by a Bristol-Myers Squibb Unrestricted Biomedical Research Grant in Infectious Diseases.
We thank P. Glaser, P. Cossart, and the Listeria Consortium for access to the L. monocytogenes EGDe sequence prior to publication.
REFERENCES
- 1.Charpentier, E., and P. Courvalin. 1999. Antibiotic resistance in Listeria spp. Antimicrob. Agents Chemother. 43:2103-2108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Charpentier, E., G. Gerbaud, and P. Courvalin. 1999. Conjugative mobilization of the rolling-circle plasmid pIP823 from Listeria monocytogenes BM4293 among gram-positive and gram-negative bacteria. J. Bacteriol. 181:3368-3374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Farber, J. M., and P. I. Peterkin. 1991. Listeria monocytogenes, a food-borne pathogen. Microbiol. Rev. 55:476-511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gill, M. J., N. P. Brenwald, and R. Wise. 1999. Identification of an efflux pump gene, pmrA, associated with fluoroquinolone resistance in Streptococcus pneumoniae. Antimicrob. Agents Chemother. 43:187-189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Glaser, P., L. Frangeul, C. Buchrieser, C. Rusniok, A. Amend, F. Baquero, P. Berche, H. Bloecker, P. Brandt, T. Chakraborty, A. Charbit, F. Chetouani, E. Couvé, A. de Daruvar, P. Dehoux, E. Domann, G. Domínguez-Bernal, E. Duchaud, L. Durant, O. Dussurget, K.-D. Entian, H. Fsihi, F. Garcia-Del Portillo, P. Garrido, L. Gautier, W. Goebel, N. Gómez-López, T. Hain, J. Hauf, D. Jackson, L.-M. Jones, U. Kaerst, J. Kreft, M. Kuhn, F. Kunst, G. Kurapkat, E. Madueño, A. Maitournam, J. Mata Vicente, E. Ng, H. Nedjari, G. Nordsiek, S. Novella, B. de Pablos, J.-C. Pérez-Diaz, R. Purcell, B. Remmel, M. Rose, T. Schlueter, N. Simoes, A. Tierrez, J.-A. Vázquez-Boland, H. Voss, J. Wehland, and P. Cossart. 2001. Comparative genomics of Listeria species. Science 294:849-852. [DOI] [PubMed] [Google Scholar]
- 6.Graves, L. M., and B. Swaminathan. 2001. PulseNet standardized protocol for subtyping Listeria monocytogenes by macrorestriction and pulsed-field gel electrophoresis. Int. J. Food Microbiol. 65:55-62. [DOI] [PubMed] [Google Scholar]
- 7.Guillemot, D., P. Maison, C. Carbon, B. Balkau, F. Vauzelle-Kervroëdan, C. Sermet, G. Bouvenot, and E. Eschwège. 1998. Trends in antimicrobial drug use in the community—France, 1981-1992. J. Infect. Dis. 177:492-497. [DOI] [PubMed] [Google Scholar]
- 8.Hadorn, K., H. Hächler, A. Schaffner, and F. H. Kayser. 1993. Genetic characterization of plasmid-encoded multiple antibiotic resistance in a strain of Listeria monocytogenes causing endocarditis. Eur. Clin. Microbiol. Infect. Dis. 12:928-937. [DOI] [PubMed] [Google Scholar]
- 9.Hof, H., T. Nichterlein, and M. Kretschmar. 1997. Management of listeriosis. Clin. Microbiol. Rev. 10:345-357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jonas, B. M., B. E. Murray, and G. M. Weinstock. 2001. Characterization of emeA, a norA homolog and multidrug resistance efflux pump, in Enterococcus faecalis. Antimicrob. Agents Chemother. 45:3574-3579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jones, E. M., and A. P. MacGowan. 1995. Antimicrobial chemotherapy of human infection due to Listeria monocytogenes. Eur. J. Clin. Microbiol. Infect. Dis. 14:165-175. [DOI] [PubMed] [Google Scholar]
- 12.Koehler, T., and J.-C. Pechere. 1998. Bacterial resistance to quinolones: mechanisms and clinical implications, p. 117-142. In V. T. Andriole (ed.), The quinolones, 2nd ed. Academic Press, Inc., San Diego, Calif.
- 13.Lampidis, R., D. Kostrewa, and H. Hof. 2002. Molecular characterization of the genes encoding DNA gyrase and topoisomerase IV of Listeria monocytogenes. J. Antimicrob. Chemother. 49:917-924. [DOI] [PubMed] [Google Scholar]
- 14.Mata, M. T., F. Baquero, and J. C. Pérez-Diaz. 2000. A multidrug efflux transporter in Listeria monocytogenes. FEMS Microbiol. Lett. 187:185-188. [DOI] [PubMed] [Google Scholar]
- 15.Neyfakh, A. A., V. E. Bidnenko, and L. B. Chen. 1991. Efflux-mediated multidrug resistance in Bacillus subtilis: similarities and dissimilarities with the mammalian system. Proc. Natl. Acad. Sci. USA 88:4781-4785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Park, S. F., and G. S. Stewart. 1990. High-efficiency transformation of Listeria monocytogenes by electroporation of penicillin-treated cells. Gene 94:129-132. [DOI] [PubMed] [Google Scholar]
- 17.Paulsen, I. T., M. H. Brown, and R. A. Skurray. 1996. Proton-dependent multidrug efflux systems. Microbiol. Rev. 60:575-608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pinner, R. W., A. Schuchat, B. Swaminathan, P. S. Hayes, K. A. Deaver, R. E. Weaver, B. D. Plikaytis, M. Reeves, C. V. Broome, J. D. Wenger, and the Listeria Study Group. 1992. Role of foods in sporadic listeriosis. II. Microbiologic and epidemiologic investigation. JAMA 267:2046-2050. [PubMed] [Google Scholar]
- 19.Poyart-Salmeron, C., C. Carlier, P. Trieu-Cuot, A.-L. Courtieu, and P. Courvalin. 1990. Transferable plasmid-mediated antibiotic resistance in Listeria monocytogenes. Lancet 335:1422-1426. [DOI] [PubMed] [Google Scholar]
- 20.Poyart-Salmeron, C., P. Trieu-Cuot, C. Carlier, A. MacGowan, J. McLauchlin, and P. Courvalin. 1992. Genetic basis of tetracycline resistance in clinical isolates of Listeria monocytogenes. Antimicrob. Agents Chemother. 36:463-466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Putman, M., H. W. van Veen, and W. N. Konings. 2000. Molecular properties of bacterial multidrug transporters. Microbiol. Mol. Biol. Rev. 64:672-693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rocourt, J. 1990. Listeria et listériose humaine. Ann. Inst. Pasteur 1:25-30. [Google Scholar]
- 23.Seeliger, H. P. R., and K. Höhne. 1979. Serotyping of Listeria monocytogenes and related species, p. 33-48. In T. Bergan and J. Norris (ed.), Methods in microbiology. Academic Press, New York, N.Y.
- 24.Smith, K., and P. Yougman. 1992. Use of a new integrational vector to investigate compartment-specific expression of the Bacillus subtilis spoIIM gene. Biochimie 74:705-711. [DOI] [PubMed] [Google Scholar]
- 25.Steers, E., E. L. Foltz, B. S. Graves, and J. Riden. 1959. An inocula replicating apparatus for routine testing of bacterial susceptibility to antibiotics. Antimicrob. Chemother. (Basel) 9:307-311. [PubMed] [Google Scholar]
- 26.Yoshida, H., M. Bogaki, S. Nakamura, K. Ubukata, and M. Konno. 1990. Nucleotide sequence and characterization of the Staphylococcus aureus norA gene, which confers resistance to quinolones. J. Bacteriol. 172:6942-6949. [DOI] [PMC free article] [PubMed] [Google Scholar]