Abstract
RWJ-54428 (MC-02,479) is a new cephalosporin active against gram-positive bacteria, including methicillin-resistant Staphylococcus aureus (MRSA). The potency of this new cephalosporin against MRSA is related to a high affinity for penicillin-binding protein 2a (PBP 2a), as assessed in a competition assay using biotinylated ampicillin as the reporter molecule. RWJ-54428 had high activity against MRSA strains COL and 67-0 (MIC of 1 μg/ml) and also showed affinity for PBP 2a, with a 50% inhibitory concentration (IC50) of 0.7 μg/ml. RWJ-54428 also displayed excellent affinity for PBP 5 from Enterococcus hirae R40, with an IC50 of 0.8 μg/ml and a MIC of 0.5 μg/ml. The affinity of RWJ-54428 for PBPs of β-lactam-susceptible S. aureus (MSSA), enterococci (E. hirae), and Streptococcus pneumoniae showed that the good affinity of RWJ-54428 for MRSA PBP 2a and E. hirae PBP 5 does not compromise its binding to susceptible PBPs. RWJ-54428 showed stability to hydrolysis by purified type A β-lactamase isolated from S. aureus PC1. In addition, RWJ-54428 displayed low MICs against strains of S. aureus bearing the four classes of staphylococcal β-lactamases, including β-lactamase hyperproducers. The frequency of isolation of resistant mutants to RWJ-54428 from MRSA strains was very low. In summary, RWJ-54428 has high affinity to multiple PBPs and is stable to β-lactamase, properties that may explain our inability to find resistance by standard methods. These data are consistent with its excellent activity against β-lactam-resistant gram-positive bacteria.
β-Lactam antibiotics exert their antibacterial effect through covalent interactions with penicillin-binding proteins (PBPs). PBPs are anchored in the bacterial cytoplasmic membrane and are involved in the last steps of cell wall peptidoglycan synthesis. Most bacterial species possess multiple PBPs, differing in enzymatic function, molecular weight, and affinity for β-lactam antibiotics. Although resistance to β-lactam antibiotics is often associated with production of β-lactamase, target alterations have been found to mediate high-level β-lactam resistance in staphylococci, enterococci, and pneumococci (38).
The genetic determinant of methicillin resistance in staphylococci has been identified as the mec DNA. This 30- to 50-kb region of foreign DNA is found only in methicillin-resistant staphylococci (39). This DNA region contains the gene mecA encoding PBP 2a, which has low affinity for β-lactam antibiotics (5-6).
Resistance to β-lactams among other gram-positive bacteria has been reported with increasing frequency. High-level ampicillin resistance is frequently observed in vancomycin-resistant Enterococcus faecium (24). This high-level resistance is mediated by overproduction of some PBPs and a further decrease in the affinity of these enzymes for β-lactam antibiotics (13). Penicillin resistance can now be found in 25% of clinical isolates of Streptococcus pneumoniae and viridans group streptococci worldwide (18). Resistance to penicillins and cephalosporins in streptococci is mediated by target site mutations in PBPs (6, 13, 32, 35).
β-Lactamase enzymes are responsible for resistance to antimicrobial therapy (2) In bacteria, the genes coding for these enzymes can be found on the chromosome, on plasmids, or on transposable elements (17). Currently, more than 90% of Staphylococcus aureus isolates worldwide are resistant to penicillin (8, 29, 31). The resistance genes have spread from staphylococci, and in 1982, penicillinase genes were first reported in Enterococcus faecalis (25-26).
Four immunotypic variants of S. aureus β-lactamase, termed A, B, C, and D, have been identified and characterized (19, 41). S. aureus β-lactamases are penicillin-hydrolyzing enzymes inhibited by clavulanic acid and, as such, are part of group 2a of Bush's classification (2).
RWJ-54428 is a new cephalosporin with a broad gram-positive spectrum of activity, which includes methicillin-resistant S. aureus (MRSA), methicillin-resistant coagulase-negative staphylococci, enterococci, and pneumococci highly resistant to other β-lactam antibiotics (3). This paper summarizes studies that were performed to determine the affinity of RWJ-54428 for several PBPs of Staphylococcus, Enterococcus, and Streptococcus and the stability of RWJ-54428 to relevant β-lactamases.
(Part of this work was previously disclosed in poster presentations [S. Chamberland, C. Chan, J. Blais, K. M. Mathias, F. Malouin, and V. J. Lee, Abstr. 37th Intersci. Conf. Antimicrob. Agents Chemother., abstr. F-178, 1997; M. K Hoang, S. Chamberland, D. Griffith, and M. Dudley, Abstr. 38th Intersci. Conf. Antimicrob. Agents Chemother., abstr. F-016, 1998; T. Nguyen, E. Liu, F. Malouin, J. Blais, and S. Chamberland, Abstr. 38th Intersci. Conf. Antimicrob. Agents Chemother., abstr. F-017, 1998].)
MATERIALS AND METHODS
Bacterial strains.
Seven strains of methicillin-susceptible S. aureus (MSSA) representing four distinct staphylococcal β-lactamases (types A, B, C, and D) were studied (19). MRSA strains included COL, a β-lactamase negative homogeneously methicillin-resistant strain (14), strain 76, a β-lactamase-positive strain of MRSA (30), and a heterogeneously resistant strain of MRSA (strain 67-0) (14). Three strains of E. faecalis were also included: E. faecalis V583, a vanB-mediated vancomycin-resistant strain (10), was the β-lactamase negative control, whereas E. faecalis strain Beirut and strain HH22 produced type A β-lactamase. Enterococcus hirae R40, a derivative of E. hirae ATCC 9790 highly resistant to ampicillin, was used to study the affinity of RWJ-54428 for PBP 5 (11). Several genetically characterized strains of S. pneumoniae were used to study the affinity of RWJ-54428 for streptococcal PBPs (12): strains 43350 (serotype 23F), 2039 (serotype 6A), and 637 (serotype 23F). They were representative of the main European clones or had a serotype preferentially found in South Africa (36). The laboratory strain R6 was also used as a reference (1).
Antibiotics.
RWJ-54428 was supplied as the mono-methanesulfonate salt. A stock solution of 2 mg of active RWJ-54428/ml was prepared in a 1:1 solution of dimethyl sulfoxide-sterile water. For the PBP binding assay, a stock solution of 5 mg of RWJ-54428/ml was prepared in sterile water. Commercially available antibiotics were obtained from various sources: ampicillin, cefaclor, cefamandole, cefazolin, cefotaxime, ceftazidime, cephalothin, cephaloridine, erythromycin, methicillin, nafcillin, oxacillin, penicillin G, and vancomycin were obtained from Sigma Chemical Co. Imipenem-cilastatin (Primaxin) was purchased from Merck. All antibiotics, except imipenem and erythromycin, were prepared at a concentration of 10 mg/ml in sterile water. Imipenem was prepared at a concentration of 5 mg/ml in sterile water. Erythromycin was prepared at a concentration of 5 mg/ml in ethanol. Stock solutions were aliquoted and kept frozen at −80°. Each aliquot was rapidly thawed and only used once.
Antibiotic susceptibility testing.
Susceptibility tests were performed using a broth microdilution assay according to NCCLS reference methods (28) in a final volume of 100 μl, using cation-adjusted Mueller-Hinton broth (CAMHB) (Difco). The culture medium was supplemented with 2% NaCl when testing β-lactam antibiotics against S. aureus isolates. The MICs of the drugs for streptococci were determined in CAMHB supplemented with 2.5% lysed horse blood (Remel).
Antibiotics were prepared at a concentration equivalent to two times the highest desired final concentration. Antibiotics were then diluted directly in the 96-well microtiter plates by serial twofold dilution by using a multichannel pipette. Microtiter plates were incubated for 24 h at 35°C and were read using a microtiter plate reader (Molecular Devices) at 650 nm as well as by visual observation using a microtiter plate reading mirror. Inoculum effect studies were carried out by performing susceptibility testing using both agar dilution and broth microdilution methods, as previously described (28), with modification of the starting inoculum.
Affinity for PBPs: preparation of bacterial membranes.
Membrane-based PBP assays were used for measurement of RWJ-54428 affinity to MRSA PBP 2a and E. hirae PBP 5. MRSA strain S. aureus 67-0 was grown at 35°C in tryptic soy broth (Difco) containing 5 μg of nafcillin/ml, and the cell membrane fraction was extracted as described below. E. hirae R40 was grown at 35°C in brain heart infusion (Difco) without antibiotic. In both cases, exponentially growing cells were harvested by centrifugation, washed, and stored at −80°C. Frozen cells were rapidly thawed, and initial cellular lysis was carried out in 50 mM Tris buffer (pH 7.5) containing lysostaphin (100 μg/ml) or lysozyme (500 μg/ml), 100 mM NaCl, 5 mM MgCl2, 1 mM phenylmethylsulfonyl fluoride, and 20 μg of DNase I and RNase A per ml at 35°C for 1 h before cells were mechanically disrupted using a French pressure cell. Unbroken cells were removed by low-speed centrifugation. Membranes were separated by differential ultracentrifugation from the cell extract and suspended in 10 mM Tris-HCl (pH 7) to a final concentration of 10 mg of protein/ml (4, 11).
Competition assays.
PBPs were labeled using a biotinylated ampicillin (BIO-AMP) according to the method described by Dargis and Malouin (7). The reporter molecule, BIO-AMP, was also prepared as previously described (7). To selectively label PBP 2a from staphylococcal membrane preparations, samples were first incubated with 100 μg of clavulanic acid/ml for 10 min at 35°C to saturate high-affinity PBPs (PBPs 1, 2, and 3). The extremely low affinity of clavulanate for MRSA PBP 2a relative to that for the other PBPs was previously reported by Chambers and Sachdeva (4). The relative binding affinity of β-lactams for PBP 2a was then assayed, in a competition assay, by adding increasing concentrations of the test compound to aliquots of the reaction mixture containing 20 μg of membrane preparation for 15 min at 35°C prior to the addition of BIO-AMP (20 μM final concentration) for an additional 15 min. Clavulanic acid was omitted in experiments determining the binding of the test compounds to any other PBPs. Samples were then boiled for 4 min in electrophoretic loading buffer containing sodium dodecyl sulfate (SDS), and proteins were separated by electrophoresis on an SDS-polyacrylamide discontinuous gel system (5% stacking and 8% separating gels). After electrophoresis, proteins were transferred onto nitrocellulose membranes. Electrophoretic PBP profiles were detected on blots by using an ECL chemiluminescence reagent system (Amersham), on the basis of the interaction of BIO-AMP-PBP complexes and an avidin-peroxidase conjugate (Bio-Rad Laboratories) (7). The concentration of the test β-lactam needed to block 50% of the subsequent binding of BIO-AMP to each PBP of interest (50% inhibitory concentration [IC50]) was determined by scanning the PBP profiles obtained on an ECL hyperfilm (Amersham) or on a chemiluminescence screen using a Molecular Imager (Bio-Rad). In some cases, the binding of the test β-lactam to the entire PBP set was evaluated by measuring the reduction of the overall chemiluminescence signal compared to that of the control PBP profile obtained in the absence of the test β-lactam and was expressed as the percentage of inhibition of BIO-AMP binding to PBPs.
Whole-cell assays.
PBP competition assays for MSSA and S. pneumoniae strains were performed with intact bacterial cells. For each concentration of test compound, an aliquot of freshly grown cells (equivalent to 1 ml of a bacterial suspension with an A600 of 0.4) was substituted for the cell membrane preparation in the competition assay described above. After the 15-min incubation period, the labeling reaction was quickly stopped by the addition of ice-cold unlabeled penicillin G (1 mg/ml) and cells were collected by centrifugation. Cells were suspended in a lysis buffer (described above) for 15 min at 37°C, and cell debris were collected by centrifugation in a tabletop Avanti centrifuge (Beckman) with the F3606 rotor at maximum speed for 20 min. Supernatants were removed, electrophoretic loading buffer was added to the membrane pellet, and samples were boiled for 4 min before separation of proteins on SDS-polyacrylamide gel electrophoresis and transfer onto nitrocellulose membrane as described above.
β-Lactamase preparation.
Extracellular β-lactamase was purified from S. aureus PC1 producing type A β-lactamase. Staphylococcal β-lactamase extract was prepared by the method described by Kernodle et al. (20-21).
β-Lactamase stability assay.
Analysis of the kinetics of hydrolysis by purified PC1 β-lactamase was performed as follows: a concentration of 100 μM antibiotic was used in 0.1 M sodium phosphate buffer, pH 7.0. Reactions were followed at wavelengths which corresponded to the maximal change in absorbance between the unhydrolyzed substrate and the hydrolyzed product for each β-lactam, as follows: cephaloridine (254 nm), cefamandole (269 nm), cefazolin (272 nm), cefaclor (264 nm), penicillin G (232 nm), ampicillin (235 nm), nitrocefin (486 nm), and RWJ-54428 (290 nm). Selection of the wavelength to study the β-lactamase stability of RWJ-54428 was based on the results of validation assays, which demonstrated the disappearance of RWJ-54428 following the addition of sodium hydroxide. The assay was performed in a 1-cm quartz cuvette at room temperature, using a Perkin-Elmer Lambda Bio UV/VIS spectrometer. Only the initial linear part of the curve was used in calculations of the β-lactamase hydrolysis rate. Results were expressed as the relative rate of hydrolysis (RRH), and cephaloridine hydrolysis was set at 100%. The β-lactamase stability assay was repeated three times using three different preparations of enzymes. The results presented below in Table 4 are representative of one of the assays. The compound ranking order was similar in each of the assays performed.
TABLE 4.
RRH of RWJ-54428 and other β-lactam antibiotics by the purified PC1 β-lactamase of S. aureus
| Antibiotic | RRHa | Strain PC1b MIC (μg/ml) |
|---|---|---|
| Cephaloridine | 100 | 0.5 |
| RWJ-54428 | 33 | 0.5 |
| Penicillin G | 1,791 | 64 |
| Ampicillin | 987 | 32 |
| Cefamandole | 40 | 1 |
| Cefazolin | 35 | 1 |
| Cefaclor | 213 | 2 |
| Nitrocefin | 1,821 | NDc |
Expressed as a percentage of the RRH of cephaloridine.
MICs were determined by a broth microdilution method.
ND, not done.
Resistance selection.
Selection of resistance to RWJ-54428 was studied in six strains of MSSA and two strains of MRSA. For each S. aureus strain, a single isolated colony was grown overnight in 8 ml of MHB. A volume of 250 μl of each bacterial suspension (undiluted and diluted) was then applied onto solid medium containing various concentrations of RWJ-54428 by using the Autoplate 4000 (Spiral Biotech, Inc.). Inocula were determined by applying 10-μl drops of 10-fold dilutions onto tryptic soy agar (TSA; Difco) plates. The plates were incubated at 35°C for 48 h. CFU were counted after 24 and 48 h of incubation at 35°C. Ratios of the number of colonies on the drug-containing plates to that on the control plates were calculated as the in vitro frequency of isolation of CFU for each strain tested. If colonies were isolated from drug-containing agar, their susceptibility to RWJ-54428 was compared to that of the parent strain by using the spiral gradient endpoint method (Spiral Biotech, Inc.).
RESULTS
Affinity of PBPs.
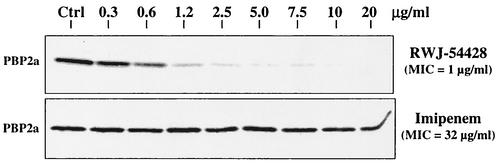
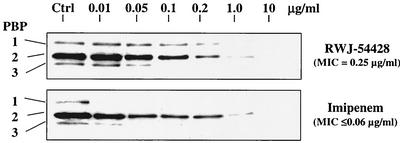
The results of competition assays for PBPs with RWJ-54428 and imipenem are shown in Fig. 2 and 3, and a comparison of IC50 values is shown in Table 1. RWJ-54428 had a higher affinity for MRSA PBP 2a (IC50 = 0.7 μg/ml) than imipenem (IC50 = 30 μg/ml). There was a generally good correlation between β-lactam MICs and affinities to MRSA PBP 2a (Table 1).
FIG. 2.
PBP competition assay demonstrating the affinity of RWJ-54428 toward PBP 2a of MRSA strain 67-0 in comparison to that with imipenem.
FIG. 3.
Whole-cell PBP competition assay demonstrating the affinity of RWJ-54428 toward the PBPs of MSSA strain ATCC 29213 in comparison to that with imipenem.
TABLE 1.
Binding affinity of RWJ-54428 and known β-lactam antibiotics toward a selection of PBPs from β-lactam-susceptible and -resistant gram-positive bacteria
| Bacteria | Antibiotic | MIC (μg/ml) | IC50 for indicated PBP in competition assays (μg/ml)
|
|||||
|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 2a | 3 | 4 | 5 | |||
| MRSA 67-0 | RWJ-54428 | 1 | —a | — | 0.7 | — | — | — |
| Ampicillin | 16 | — | — | 23 | — | — | — | |
| Imipenem | 32 | — | — | 30 | — | — | — | |
| Penicillin G | 16 | — | — | 48 | — | — | — | |
| Cefazolin | 256 | — | — | 238 | — | — | — | |
| Oxacillin | 64 | — | — | 272 | — | — | — | |
| Cefotaxime | 128 | — | — | 363 | — | — | — | |
| Cephalothin | 128 | — | — | 363 | — | — | — | |
| Nafcillin | 256 | — | — | 385 | — | — | — | |
| Methicillin | 512 | — | — | 587 | — | — | — | |
| MSSA ATCC 29213 | RWJ-54428 | 0.25 | 0.2 | 0.2 | NAb | 0.1 | — | — |
| Cefaclor | 0.5 | 0.3 | >8 | NAb | <0.03 | — | — | |
| Methicillin | 1 | 0.6 | 6.6 | NAb | — | — | — | |
| Nafcillin | 0.5 | 0.3 | 0.4 | NAb | 0.3 | — | — | |
| Imipenem | <0.06 | <0.01 | 0.03 | NAb | 0.04 | — | — | |
| E. hirae R40 | RWJ-54428 | 0.5 | — | — | NAb | <0.5 | <0.5 | 0.8 |
| Imipenem | 32 | — | — | NAb | <0.5 | <0.5 | 8.6 | |
| S. pneumoniae R6c | RWJ-54428 | <0.06 | 0.1 | 0.2 | 0.05 | 0.2 | 0.1 | — |
| Penicillin G | <0.06 | 0.04 | 0.04 | 0.03 | 0.2 | 0.03 | — | |
—, not determined.
NA, not applicable.
For S. pneumoniae R6, PBPs, 1a, 1b, 2x, 2a, 2b, and 3 (columns from left to right) were evaluated.
RWJ-54428 has high affinity for the well-characterized E. hirae PBP 5. The IC50 values for E. hirae PBP 5 were 0.8 and 8.6 μg/ml for RWJ-54428 and imipenem, respectively (Table 1).
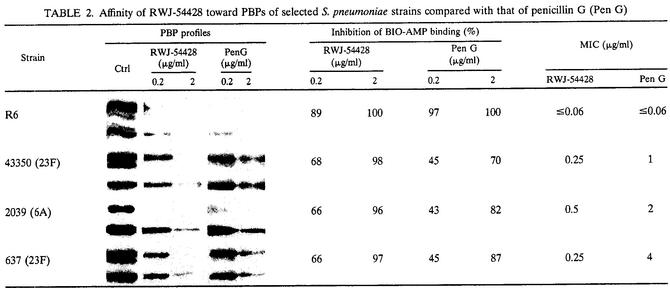
RWJ-54428 has high affinity for multiple PBP targets from both β-lactam-susceptible and -resistant gram-positive strains. RWJ-54428 showed IC50 values comparable to those of other traditional β-lactams, such as nafcillin for MSSA, imipenem for E. hirae, and penicillin G for S. pneumoniae, in the sense that the low MIC could be associated with the IC50 for one or more PBPs. As opposed to that seen against MRSA PBP 2a, imipenem was very potent and showed very low IC50 values for MSSA PBPs (Table 1 and Fig. 3). Table 2 compares the binding of RWJ-54428 to that of penicillin G for PBPs from penicillin-susceptible, penicillin-intermediate, and penicillin-resistant isolates of S. pneumoniae. By measuring the residual chemiluminescence signal of BIO-AMP in the presence of RWJ-54428 compared to that measured in the control PBP profiles, it was shown that the overall binding of RWJ-54428 for S. pneumoniae PBPs was equivalent to or surpassed that of penicillin G in PBP competition assays (Table 2).
TABLE 2.
Affinity of RWJ-54428 toward PBPs of selected S. pneumoniae strains compared with that of penicillin G (Pen G)
Stability of RWJ-54428 to β-lactamases.
Comparison of the stability of RWJ-54428 to staphylococcal and enterococcal β-lactamases is shown in Table 3. There was no more than a twofold difference in the RWJ-54428 MIC between MSSA ATCC 25923, a β-lactamase-negative strain, and MSSA strains producing type A, B, and D β-lactamases. A fourfold-higher MIC was observed in MSSA PC1, which overproduces type A β-lactamase, and MSSA V137, which produces a type C β-lactamase. For these two strains, MICs of RWJ-54428 were 0.5 μg/ml. In MRSA strains, there was only a twofold difference in the RWJ-54428 MIC between a β-lactamase-positive strain (MRSA 76) and a β-lactamase-negative strain (MRSA COL). In contrast, β-lactamase production in MSSA was associated with a 32- to 4,096-fold-higher penicillin G MIC, 16- to 512-fold-higher ampicillin MIC, and 4- to 8-fold-higher cefamandole and cefaclor MICs compared to those for the β-lactamase-negative control strain (ATCC 25923).
TABLE 3.
Susceptibility of staphylococci and enterococci producing β-lactamases to RWJ-54428 and other β-lactam antibiotics
| Bacteria | β-Lactamasea
|
MIC (μg/ml)b
|
|||||
|---|---|---|---|---|---|---|---|
| Type | Level | RWJ | PEN G | AMP | FAM | CEC | |
| MSSA ATCC 25923 | Neg.c | 0 | 0.125 | 0.015 | 0.06 | 0.25 | 0.125 |
| MSSA ATCC 29213 | A | 0.006 | 0.25 | 0.5 | 1 | 0.25 | 0.5 |
| MSSA NCTC 9789 | A | 0.088 | 0.25 | 32 | 16 | 1 | 1 |
| MSSA PC1 | A | 0.201 | 0.5 | 64 | 32 | 1 | 2 |
| MSSA 22260 | B | 0.024 | 0.125 | 4 | 4 | 2 | 1 |
| MSSA V137 | C | 0.034 | 0.5 | 8 | 8 | 2 | 1 |
| MSSA FAR19 | D | 0.030 | 0.25 | 4 | 2 | 1 | 1 |
| MRSA COL | Neg.c | 0 | 1 | 16 | 16 | >8 | >8 |
| MRSA 76 | Pos.d | NAe | 2 | 64 | >32 | >8 | >8 |
| E. faecalis VanB | Neg.c | 0 | 0.125 | NDf | 1 | NDf | NDf |
| E. faecalis Beirut | A | NAe | ≤0.0625 | NDf | 2 | NDf | NDf |
| E. faecalis HH22 | A | NAe | ≤0.0625 | NDf | 8 | NDf | NDf |
From Kernodle et al. (12, 13). The activity was reported as micromoles of nitrocefin degraded per minute per cell mass after induction.
RWJ, RWJ-54428; PEN G, penicillin G; AMP, ampicillin; FAM, cefamandole; CEC, cefaclor.
Neg., β-lactamase-negative strain.
Pos., β-lactamase-positive strain for which the enzyme type was not determined.
NA, not available.
ND, not done.
The hydrolysis of RWJ-54428 and other β-lactam antibiotics related to cephaloridine by purified PC1 β-lactamase of S. aureus was studied (Table 4). The hydrolysis of RWJ-54428 by type A β-lactamase was low, indicating stability of this new cephalosporin to this enzyme. PC1 staphylococcal enzyme preferentially hydrolyzes penicillins, as the RRHs for penicillin and ampicillin were 30- to 55-fold greater than those observed for RWJ-54428. RWJ-54428 has rates of hydrolysis that are comparable to those of cefazolin.
In vitro inoculum effect.
The effect of inoculum size on the in vitro activity of RWJ-54428 against various strains of S. aureus was determined by using broth microdilution and agar dilution methods. In the agar dilution assays (Table 5), there was no significant increase in the MIC of RWJ-54428 for strains with inocula ranging from 5 × 104 to 5 × 107 CFU/spot. Only twofold variations in susceptibility to RWJ-54428 were observed for the S. aureus strains tested, including β-lactamase-positive strains. In contrast, the activity of penicillin G, which is highly susceptible to degradation by staphylococcal β-lactamases, against β-lactamase-positive strains was dramatically reduced (by 16- to 128-fold) with a 100-fold larger inoculum. There was a two- to eightfold increase in MICs of cefamandole and cefaclor when tested against the β-lactamase-positive MSSA strains at an inoculum 1,000-fold larger (i.e., >107 CFU/spot).
TABLE 5.
Effect of inoculum size on activity of RWJ-54428 against MRSA and MSSA strains with various types and levels of production of β-lactamase, as determined using the agar dilution assay
| S. aureus strain | β-Lactamasea
|
Antibiotic | MIC (μg/ml) at CFU/spot inoculum size:
|
||||
|---|---|---|---|---|---|---|---|
| Type | Level | 5 × 104 | 5 × 105 | 5 × 106 | 5 × 107 | ||
| MSSA | |||||||
| ATCC 25923 | Neg.b | 0 | RWJ-54428 | 0.125 | 0.125 | 0.25 | 0.25 |
| Cefamandole | 0.25 | 0.5 | 0.5 | 0.5 | |||
| Cefaclor | 1 | 1 | 2 | 2 | |||
| Penicillin G | ≤0.03 | ≤0.03 | ≤0.03 | ≤0.03 | |||
| ATCC 29213 | A | 0.006 | RWJ-54428 | 0.25 | 0.25 | 0.25 | 0.25 |
| Cefamandole | 0.5 | 0.5 | 1 | 1 | |||
| Cefaclor | 1 | 2 | 2 | 8 | |||
| Penicillin G | 0.125 | 0.25 | 2 | 32 | |||
| NCTC 9789 | A | 0.088 | RWJ-54428 | 0.25 | 0.25 | 0.25 | 0.5 |
| Cefamandole | 0.5 | 1 | 1 | 4 | |||
| Cefaclor | 2 | 4 | 8 | >8 | |||
| Penicillin G | 1 | 8 | >64 | >64 | |||
| Vancomycin | 0.5 | 1 | 2 | 16 | |||
| 22260 | B | 0.24 | RWJ-54428 | 0.25 | 0.25 | 0.25 | 0.25 |
| Cefamandole | 0.5 | 1 | 2 | 4 | |||
| Cefaclor | 2 | 2 | 4 | 8 | |||
| Penicillin G | 0.5 | 2 | 32 | >64 | |||
| V137 | C | 0.034 | RWJ-54428 | 0.25 | 0.25 | 0.5 | 0.5 |
| Cefamandole | 1 | 1 | 2 | 8 | |||
| Cefaclor | 2 | 4 | 8 | >8 | |||
| Penicillin G | 1 | 8 | 64 | >64 | |||
| FAR19 | D | 0.03 | RWJ-54428 | 0.25 | 0.25 | 0.25 | 0.25 |
| Cefamandole | 0.5 | 0.5 | 1 | 2 | |||
| Cefaclor | 1 | 2 | 4 | 8 | |||
| Penicillin G | 0.25 | 1 | 32 | >64 | |||
| MRSA | |||||||
| COL | Neg.b | NAd | RWJ-54428 | 1 | 1 | 1 | 1 |
| Cefamandole | >8 | >8 | >8 | >8 | |||
| Penicillin G | 16 | 32 | 32 | 32 | |||
| Vancomycin | 2 | 2 | 2 | 4 | |||
| 76 | Pos.c | NA | RWJ-54428 | 1 | 1 | 1 | 1 |
| Cefamandole | >8 | >8 | >8 | >8 | |||
| Penicillin G | 32 | 64 | >64 | >64 | |||
| Vancomycin | 1 | 1 | 2 | 8 | |||
In broth microdilution assays, the susceptibilities of MRSA and MSSA strains to RWJ-54428 were reduced by two- to eightfold only when the inoculum was equal or greater than 500 times (∼108 CFU/ml) the NCCLS recommended inoculum (data not shown). The eightfold increase in MIC was observed in a β-lactamase-negative strain, indicating that β-lactamase does not contribute to this observation. In contrast, strong inoculum effects (2- to 256-fold increases in MICs) were noted for commercially available antibiotics such as cefamandole, cefaclor, cefazolin, cefotaxime, ampicillin, penicillin G, and vancomycin with inocula 50 times the NCCLS recommended inoculum size (data not shown).
In studies conducted with RWJ-54428 in the broth microdilution assay, samples from sub-MIC wells at higher inocula were streaked onto antibiotic-free TSA plates and incubated aerobically at 35°C for 24 h. When colonies were isolated, their susceptibility to RWJ-54428 was determined. There was no change in susceptibility for these isolated colonies compared to the parent strains.
Selection of resistance.
Attempts to select and obtain S. aureus isolates resistant to RWJ-54428 were unsuccessful. In the instances where growth was observed and colonies were picked from the selective media, endpoint susceptibility tests showed that these isolates were as susceptible as the parental strains to RWJ-54428, with MICs varying by no more than twofold. This was the case whether the test strain used in these frequency-of-resistance studies was MRSA, MSSA, β-lactamase-positive or -negative, or when the inoculum was as large as 109 CFU/ml.
DISCUSSION
The quest for a β-lactam that inhibits MRSA PBP 2a has now been conducted for several years. Many studies have aimed at characterizing structural and enzymatic features of this low-affinity PBP target (22, 33, 37). RWJ-54428 is a new parenteral cephalosporin with potent activity against multidrug-resistant gram-positive bacteria, including staphylococci, enterococci, and pneumococci highly resistant to other β-lactam antibiotics (3). The potent activities of RWJ-54428 against β-lactam-resistant staphylococci and enterococci were correlated with high affinities for staphylococcal PBP 2a and PBP 5 from enterococci, both major determinants of resistance to β-lactam antibiotics. The enhanced binding of RWJ-54428 to MRSA PBP 2a is correlated to a pharmacophore that is structurally distinct from that of other reported anti-MRSA β-lactams (16). The pharmacophore of RWJ-54428 also provides binding affinity to E. hirae PBP 5, which shares some common features with MRSA PBP 2a and E. faecium PBP 5 (9, 40). The high affinity of RWJ-54428 to PBP 5 is consistent with previously reported susceptibility data against 100 isolates of ampicillin-resistant E. faecium showing that RWJ-54428 has activity against these isolates (RWJ-54428 MIC at which 50% of isolates are inhibited [MIC50] of 4 μg/ml; MIC90 of 8 μg/ml) (3). However, not all reported anti-MRSA β-lactams have affinity for the enterococcal PBP 5 and, consequently, inhibitory activities against that species may greatly vary (15, 23, 27).
Although we demonstrated the potent in vitro activity against a large number of clinical isolates of methicillin-resistant and methicillin-susceptible staphylococci (S. aureus and coagulase-negative staphylococci), enterococci, and pneumococci (3), we needed to verify that the high-affinity PBP 2a/PBP 5 pharmacophore of RWJ-54428 did not impede binding to other crucial PBP targets found in β-lactam-susceptible organisms. The affinity of RWJ-54428 for PBPs of S. aureus, E. hirae, and S. pneumoniae was high. RWJ-54428 binds well to both resistant and susceptible PBPs from staphylococci, enterococci, and pneumococci. The low MICs of RWJ-54428 for these β-lactam-susceptible gram-positive bacteria were associated with low IC50 values for one or more PBPs. Studies with penicillin-susceptible, -intermediate, and -resistant pneumococci demonstrated that RWJ-54428 also has high affinity for penicillin-resistant and -susceptible PBPs in pneumococci.
The β-lactamase stability of RWJ-54428 was demonstrated by comparing the susceptibilities of various strains of S. aureus producing several types and amounts of β-lactamases (A, B, C, and D). The stability of RWJ-54428 to staphylococcal β-lactamase was further substantiated with biochemical studies. Partly purified PC1 enzyme was used to determine the RRHs for RWJ-54428 and several other β-lactam antibiotics. The RRH of RWJ-54428 by type A staphylococcal β-lactamase was low compared to those of other β-lactams, indicating increased stability of this new cephalosporin to this enzyme. RRHs for reference compounds were in accordance with previously published data: penicillin G RRH, 1,869; ampicillin RRH, 675; cefamandole RRH, 6.4; cefazolin RRH, 30.6; and nitrocefin RRH, 2,034 (41).
Significant inoculum effects with S. aureus have been reported for antibiotics susceptible to hydrolysis by β-lactamases, but not for β-lactamase-stable β-lactam antibiotics (34). In agar dilution assays and microdilution broth assays, increasing inoculum size did not significantly reduce the activity of RWJ-54428 against the MSSA and MRSA strains studied, regardless of the production of β-lactamase or the type of enzyme produced by these strains (type A, B, C, or D).
Numerous efforts to isolate spontaneous resistant mutants of S. aureus by passage on media containing various concentrations of RWJ-54428 were unsuccessful. In these studies, the production of β-lactamase in various strains of S. aureus did not provide more opportunities to select resistance to RWJ-54428. Both the high affinity of RWJ-54428 for multiple PBPs and its stability to staphylococcal β-lactamases are attributes that may reduce the rate of isolation of resistance to this new cephalosporin in S. aureus.
In summary, RWJ-54428 is a new cephalosporin with potent activity against staphylococci, including MRSA. The enhanced activity of RWJ-54428 against MRSA is associated with high affinity for PBP 2a, the primary determinant of methicillin resistance in Staphylococcus spp. (6). This corroborates the potent antistaphylococcal activity of RWJ-54428 that was previously reported against a large population of strains demonstrating MIC90s of 0.5, 2, and 2 μg/ml against MSSA, MRSA, and MR coagulase-negative staphylococci, respectively (3). RWJ-54428 also binds to multiple PBPs from gram-positive bacteria. These properties combined with a stability to staphylococcal β-lactamase render RWJ-54428 a potent agent for resistant gram-positive strains and species of clinical importance.
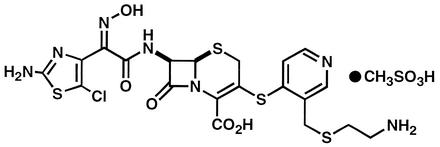
FIG. 1.
RWJ-54428 (MC-02,479) chemical structure.
Acknowledgments
We thank B. Murray, R. Fontana, R. Hakenbeck, and D. Kernodle for the enterococci, pneumococci, and MSSA strains with distinct β-lactamases.
The work described herein was conducted as part of a research collaboration with the R.W. Johnson Pharmaceutical Institute.
REFERENCES
- 1.Avery, O. T., C. M. MacLeod, and M. McCarty. 1944. Studies on the chemical nature of the substance inducing transformation of pneumococcal types. J. Exp. Med. 79:137-158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bush, K., G. A. Jacoby, and A. A. Medeiros. 1995. A functional classification scheme for β-lactamases and its correlation with molecular structure. Antimicrob. Agents Chemother. 39:1211-1233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chamberland, S., J. Blais, M. Hoang, C. Dinh, D. Cotter, E. Bond, C. Gannon, C. Park, F. Malouin, and M. N. Dudley. 2001. In vitro activity of RWJ-54428 (MC-02,479) against multiresistant gram-positive bacteria. Antimicrob. Agents Chemother. 45:1422-1430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chambers, H. F., and M. Sachdeva. 1990. Binding of β-lactam antibiotics to penicillin-binding proteins in methicillin-resistant Staphylococcus aureus. J. Infect. Dis. 161:1170-1176. [DOI] [PubMed] [Google Scholar]
- 5.Chambers, H. F. 1997. Methicillin resistance in staphylococci: molecular and biochemical basis and clinical implications. Clin. Microbiol. Rev. 10:781-791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chambers, H. F. 1999. Penicillin-binding protein-mediated resistance in pneumococci and staphylococci. J. Infect. Dis. 179(Suppl. 2):S353-S359. [DOI] [PubMed] [Google Scholar]
- 7.Dargis, M., and F. Malouin. 1994. Use of biotinylated β-lactams and chemiluminescence for study and purification of PBPs in bacteria. Antimicrob. Agents Chemother. 38:973-980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Doern, G. V., R. N. Jones, M. A. Pfaller, K. C. Kugler, and M. L. Beach. 1999. Bacterial pathogens isolated from patients with skin and soft tissue infections: frequency of occurrence and antimicrobial susceptibility patterns from the SENTRY antimicrobial surveillance program (United States and Canada, 1997). Diagn. Microbiol. Infect. Dis. 34:65-72. [DOI] [PubMed] [Google Scholar]
- 9.El Kharroubi, A., P. Jacques, G. Piras, J. Van Beeumen, J. Coyette, and J. M. Ghuysen. 1991. The Enterococcus hirae R40 penicillin-binding protein 5 and the methicillin-resistant Staphylococcus aureus penicillin-binding protein 2′ are similar. Biochem. J. 280:463-469. [PMC free article] [PubMed] [Google Scholar]
- 10.Evers, S., D. F. Sahm, and P. Courvalin. 1993. The vanB gene of vancomycin-resistant Enterococcus faecalis V583 is structurally related to genes encoding d-ala:d-ala ligases and glycopeptide-resistance proteins VanA and VanC. Gene 124:143-144. [DOI] [PubMed] [Google Scholar]
- 11.Fontana, R., R. Cerini, P. Longoni, A. Grossato, and P. Canepari. 1983. Identification of a streptococcal PBP that reacts very slowly with penicillin. J. Bacteriol. 155:1343-1350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hakenbeck, R., T. Briese, L. Chalkley, H. Ellerbrok, R. Kalliokoski, C. Latorre, M. Leinonen, and C. Martin. 1991. Antigenic variation of penicillin-binding proteins from penicillin-resistant clinical strains of Streptococcus pneumoniae. J. Infect. Dis. 164:313-319. [DOI] [PubMed] [Google Scholar]
- 13.Hakenbeck, R. 1998. Resistant penicillin-binding proteins. Cell. Mol. Life Sci. 54:332-340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hartman, B. J., and A. Tomasz. 1984. Low-affinity penicillin-binding protein associated with beta-lactam resistance in Staphylococcus aureus. J. Bacteriol. 158:513-516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hebeisen, P., I. Heinze-Krauss, P. Angehrn, P. Hohl, M. G. P. Page, and R. L. Then. 2001. In vitro and in vivo properties of Ro 63-9141, a novel broad-spectrum cephalosporin with activity against methicillin-resistant staphylococci. Antimicrob. Agents Chemother. 45:825-836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hecker, S. J., T. W. Glinka, A. Cho, Z. J. Zhang, M. E. Price, S. Chamberland, D. Griffith, and V. J. Lee. 2000. Discovery of RWJ-54428 (MC-02,479), a new cephalosporin active against resistant gram-positive bacteria. J. Antibiot. 53:1272-1281. [DOI] [PubMed] [Google Scholar]
- 17.Jacoby, G. A., and G. L. Archer. 1991. New mechanisms of bacterial resistance to antimicrobial agents. N. Engl. J. Med. 324:601-612. [DOI] [PubMed] [Google Scholar]
- 18.Jones, R. N., and W. R. Wilson. 1998. Epidemiology, laboratory detection, and therapy of penicillin-resistant streptococcal infections. Diagn. Microbiol. Infect. Dis. 31:453-459. [DOI] [PubMed] [Google Scholar]
- 19.Kernodle, D. S., C. W. Stratton, L. W. McMurray, J. R. Chipley, and P. A. McGraw. 1989. Differentiation of β-lactamase variants of Staphylococcus aureus by substrate hydrolysis profiles. J. Infect. Dis. 159:103-108. [DOI] [PubMed] [Google Scholar]
- 20.Kernodle, D. S., D. J. Zygmunt, P. A. McGraw, and J. R. Chipley. 1990. Purification of Staphylococcus aureus β-lactamases by using sequential cation-exchange and affinity chromatography. Antimicrob. Agents Chemother. 34:2177-2183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kernodle, D. S., P. A. McGraw, C. W. Stratton, and A. B. Kaiser. 1990. Use of extracts versus whole-cell bacterial suspensions in the identification of Staphylococcus aureus β-lactamase variants. Antimicrob. Agents Chemother. 34:420-425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lu, W.-P., Y. Sun, M. D. Bauer, S. Paule, P. M. Koenigs, and W. G. Kraft. 1999. Penicillin-binding protein 2a from methicillin-resistant Staphylococcus aureus: kinetic characterization of its interactions with β-lactams using electrospray mass spectrometry. Biochemistry 38:6537-6546. [DOI] [PubMed] [Google Scholar]
- 23.Matsumoto, M., H. Tamaoka, H. Ishikawa, and M. Kikuchi. 1998. In vitro and in vivo antibacterial activities of OPC-20011, a novel parenteral broad-spectrum 2-oxaisocephem antibiotic. Antimicrob. Agents Chemother. 42:2943-2949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Murray, B. E. 1998. Diversity among multidrug-resistant enterococci. Emerg. Infect. Dis. 4:37-47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Murray, B. E., and B. Mederski-Samoraj. 1983. Transferable β-lactamase: a new mechanism for in vitro penicillin resistance in Streptococcus faecalis. J. Clin. Investig. 72:1168-1171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Murray, B. E., K. V. Singh, S. M. Markowitz, H. A. Lopardo, J. E. Patterson, M. J. Zervos, E. Rubeglio, G. M. Caputo, R. Nasnas, L. S. Moore, E. S. Wong, and G. Weinstosk. 1991. Evidence for clonal spread of a single strain of β-lactamase-producing Enterococcus (Streptococcus) faecalis to six hospitals in five states. J. Infect. Dis. 163:780-785. [DOI] [PubMed] [Google Scholar]
- 27.Nagano, R., K. Shibata, Y. Adachi, H. Imamura, T. Hashizume, and H. Morishima. 2000. In vitro activities of novel trans-3,5-disubstituted pyrrolidinylthio-1 β-methylcarbapenems with potent activities against methicillin-resistant Staphylococcus aureus and Pseudomonas aeruginosa. Antimicrob. Agents Chemother. 44:489-495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.National Committee for Clinical Laboratory Standards. 1997. Methods for dilution of antimicrobial susceptibility tests for bacteria that grow aerobically, 4th ed., vol. 17, no. 2. Approved standard M7-A4. National Committee for Clinical Laboratory Standards, Wayne, Pa.
- 29.O'Brien, T. K., and The International Survey of Antibiotic Resistance Group. 1986. Resistance to antibiotics at medical centers in different parts of the world. J. Antimicrob. Chemother. 18(Suppl. C):243-253. [DOI] [PubMed] [Google Scholar]
- 30.Peacock, J. E., F. J. Marsik, and R. P. Wenzel. 1980. Methicillin-resistant Staphylococcus aureus: introduction and spread within a hospital. Ann. Intern. Med. 93:526-532. [DOI] [PubMed] [Google Scholar]
- 31.Pfaller, M. A., R. N. Jones, G. V. Doern, and K. Kugler. 1998. Bacterial pathogens isolated from patients with bloodstream infection: frequencies of occurrence and antimicrobial susceptibility patterns from the SENTRY antimicrobial surveillance program (United States and Canada, 1997). Antimicrob. Agents Chemother. 42:1762-1770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Reichmann, P., A. Konig, A. Marton, and R. Hakenbeck. 1996. Penicillin-binding proteins as resistance determinants in clinical isolates of Streptococcus pneumoniae. Microb. Drug Resist. 2:177-181. [DOI] [PubMed] [Google Scholar]
- 33.Roychoudhury, S., J. E. Dotzlaf, S. Ghag, and W.-K. Yeh. 1994. Purification, properties, and kinetics of enzymatic acylation with β-lactams of soluble penicillin-binding protein 2a, a major factor in methicillin-resistant Staphylococcus aureus. J. Biol. Chem. 269:12067-12073. [PubMed] [Google Scholar]
- 34.Sabath, L. D., C. Garner, C. Wilcox, and M. Finland. 1975. Effect on inoculum and of beta-lactamase on the anti-staphylococcal activity of thirteen penicillins and cephalosporins. Antimicrob. Agents Chemother. 8:344-349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Severin, A., et al. 1997. Abnormal physiological properties and altered cell wall composition in Streptococcus pneumoniae grown in the presence of clavulanic acid. Antimicrob. Agents Chemother. 41:504-510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Sibold, C., J. Wang, J. Henrichsen, and R. Hakenbeck. 1992. Genetic relationships of penicillin-susceptible and -resistant Streptococcus pneumoniae strains isolated on different continents. Infect. Immun. 60:4119-4126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sun, Y., M. D. Bauer, and W. Lu. 1998. Identification of the active site serine of penicillin-binding protein 2a from methicillin-resistant Staphylococcus aureus by electrospray mass spectrometry. J. Mass Spectrom. 33:1009-1016. [DOI] [PubMed] [Google Scholar]
- 38.Tomasz, A., and R. Munoz. 1995. β-Lactam antibiotic resistance in gram-positive bacterial pathogens of the upper respiratory tract: a brief overview of mechanisms. Microb. Drug Resist. 1:103-109. [DOI] [PubMed] [Google Scholar]
- 39.Wu, S. W., H. deLencastre, and A. Tomasz. 2001. Recruitment of the mecA gene homologue of Staphylococcus sciuri into a resistant determinant and expression of the resistant phenotype in Staphylococcus aureus. J. Bacteriol. 183:2417-2424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Zorzi, W., X. Y. Zhou, O. Dardenne, J. Lamotte, D. Raze, J. Pierre, L. Gutmann, and J. Coyette. 1996. Structure of the low-affinity penicillin-binding protein 5 PBP5fm in wild-type and highly penicillin-resistant strains of Enterococcus faecium. J. Bacteriol. 178:4948-4957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Zygmunt, D. J., C. W. Stratton, and D. S. Kernodle. 1992. Characterization of four β-lactamases produces by Staphylococcus aureus. Antimicrob. Agents Chemother. 36:440-445. [DOI] [PMC free article] [PubMed] [Google Scholar]