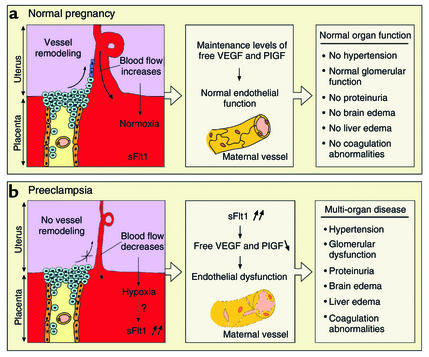
The occurrence of seizures (eclampsia, from the Greek “eklampsis,” sudden flashing) has been a long-known and feared complication of pregnancy, often killing both mother and child. Preeclampsia, or the condition preceding full-blown eclampsia, affects up to 5% of pregnant women and is diagnosed by the onset of hypertension and proteinuria in the second trimester (1). Preeclampsia may eventually progress to glomerular malfunction, thrombocytopenia, liver and brain edema, and associated life-threatening seizures (2) (Figure 1). Preeclampsia has been sometimes termed the “disease of theories,” as several models for its pathogenesis have been proposed. But, as of today, no satisfactory unifying hypothesis has emerged (1). The restricted occurrence of preeclampsia to humans and primates and the lack of a suitable animal model have hampered the understanding of its pathogenesis (3). In this issue of the JCI, S.E. Maynard et al. (4) report the novel insight that circulating levels of two angiogenic growth factors, VEGF and placental growth factor (PlGF), may play a more important role than previously believed. In particular, the authors propose that, in pregnant women with preeclampsia, the placenta produces elevated levels of the soluble fms-like tyrosine kinase 1 (sFlt1) receptor, which captures free VEGF and PlGF. As a result, the normal vasculature in the kidney, brain, lungs, and other organs is deprived of essential survival and maintenance signals and becomes dysfunctional (Figure 1). As the authors show in their rodent model, this may lead to the development of hypertension and renal disease, reminiscent of preeclampsia in humans. In another study in this issue, V. Eremina et al. (5) provide additional evidence for a critical role of VEGF in renal disease during preeclampsia. These authors demonstrate that mice lacking one VEGF allele in renal podocytes develop the typical renal pathology found in pregnant women with preeclampsia. These studies therefore shed unprecedented light on the pathogenesis of preeclampsia and offer novel therapeutic opportunities for this disease.
Figure 1.
Hypothesis on the role of sFlt1 in preeclampsia. (a) During normal pregnancy, the uterine spiral arteries are infiltrated and remodeled by endovascular invasive trophoblasts, thereby increasing blood flow significantly in order to meet the oxygen and nutrient demands of the fetus. (b) In the placenta of preeclamptic women, trophoblast invasion does not occur and blood flow is reduced, resulting in placental hypoxia. In addition, increased amounts of soluble Flt1 (sFlt1) are produced by the placenta and scavenge VEGF and PlGF, thereby lowering circulating levels of unbound VEGF and PlGF. This altered balance causes generalized endothelial dysfunction, resulting in multi-organ disease. It remains unknown whether hypoxia is the trigger for stimulating sFlt1 secretion in the placenta of preeclamptic mothers and whether the higher sFlt1 levels interfere with trophoblast invasion and spiral artery remodeling.
sFlt1: a likely candidate preeclampsia factor
For the fetus to develop normally, it must receive sufficient oxygen and nutrients (6). These are supplied via the maternal spiral arteries in the uterus. During normal pregnancy, cytotrophoblasts convert from an epithelial to an endothelial phenotype (a process termed pseudo-vasculogenesis) and invade maternal spiral arteries. This vascular remodeling increases the bulk flow and the supply of nutrients and oxygen to the fetus by the end of the first trimester (7, 8) (Figure 1). Vascular factors such as VEGF, angiopoietins, and ephrins have been implicated in this process (7). In preeclampsia, pseudo-vasculogenesis is defective, and the resultant placental ischemia has been proposed to trigger the release of unknown placenta-derived factors. The latter would induce systemic endothelial dysfunction and thereby contribute to the renal, cardiovascular, and neurological defects of preeclampsia (Figure 1). Despite intensive efforts, the precise nature of the placenta-derived preeclampsia factors has remained enigmatic for years.
In their study, Maynard et al. (4) may have discovered a likely candidate preeclampsia factor. Indeed, having used gene profiling, these authors report that the placenta of pregnant women with preeclampsia produced increased levels of sFlt1. Flt1, binding VEGF and its homologue PlGF, exists in two forms: a membrane-bound receptor tyrosine kinase which transmits angiogenic signals (Flt1), and a soluble secreted ectodomain which only captures VEGF and PlGF (sFlt1). As sFlt1 lacks a cytosolic domain, its function is restricted to regulating (reducing) the levels of free VEGF and PlGF available to signal via intact Flt1 and fetal liver kinase-1. Even though sFlt1 may be one of the few, if not the only, inhibitor of VEGF known today, it remained unknown whether it might contribute to any sort of human disease.
Altered angiogenic balance causes general endothelial dysfunction
How then can elevated circulating levels of sFlt1 contribute to preeclampsia? Whereas dynamic surges of high VEGF levels mediate angiogenesis in the embryo and in the adult during disease, continuous low levels of VEGF are required for endothelial cells to survive prolonged periods and function properly. Thus, when sFlt1 plasma levels rise, they may reduce the circulating VEGF and PlGF levels below a critical threshold required for maintenance of the established vasculature in the adult. The resultant endothelial dysfunction may disrupt the blood-brain barrier and cause intracranial hypertension, result in edema in the liver, and affect glomerular function. Indeed, Eremina et al. (5) demonstrate that glomerular capillary function is under the strict gene-dosage–dependent control of VEGF. That is, when VEGF levels in the renal prodocytes drop 50%, glomerular endothelial cells swell, capillary loops collapse, and proteinuria develops — as in preeclampsia. We previously demonstrated that absence of the VEGF164 and VEGF188 isoforms impairs glomerular filtration (9). Endothelial dysfunction may also deregulate hemostasis and trigger thrombocytopenia. By inducing vasodilation, VEGF also induces hypotension, and thus lower circulating VEGF levels will cause elevated blood pressure, another hallmark of preeclampsia. Thus, the sFlt1 hypothesis allows the proposal of a unifying model, explaining, perhaps not all, but at least several, of the hallmark symptoms of preeclampsia.
As insightful as these studies are, they do not address the question as to what upregulates sFlt1 expression in the placenta in preeclampsia. Hypoxia upregulates Flt1 expression and, since the placenta is hypoxic in pregnant women with preeclampsia, could be responsible (Figure 1). It also remains to be determined whether the elevated sFlt1 levels in the placenta would not further aggravate the disease by impairing VEGF-dependent pseudo-vasculogenesis and maternal spiral artery remodeling.
What medical implications do these studies suggest? First, strategies designed to normalize circulating free VEGF and PlGF levels might be expected to halt progression of the disease. Second, chronic administration of VEGF inhibitors, currently being evaluated for their therapeutic potential to inhibit cancer, retinal neovascularization, and chronic inflammation, may pose a risk of endothelial dysfunction, renal insufficiency, and hypertension. Results from ongoing clinical trials support this notion. Third, renal parameters and blood pressure might be used as surrogate markers of the success of anti-angiogenesis therapy — the angiogenesis field desperately needs such markers. At the very least, these studies raise new hopes that novel strategies may be designed to combat preeclampsia and thereby improve the chances of the mother and child for a healthy future.
Footnotes
See the related article beginning on page 649.
Conflict of interest: The authors have declared that no conflict of interest exists.
Nonstandard abbreviations used: placental growth factor (PlGF); fms-like tyrosine kinase 1 (Flt1); soluble Flt1 (sFlt1).
References
- 1.Roberts JM, Cooper DW. Pathogenesis and genetics of pre-eclampsia. Lancet. 2001;357:53–56. doi: 10.1016/s0140-6736(00)03577-7. [DOI] [PubMed] [Google Scholar]
- 2.Pridjian G, Puschett JB. Preeclampsia. Part 1: clinical and pathophysiologic considerations. Obstet. Gynecol. Surv. 2002;57:598–618. doi: 10.1097/00006254-200209000-00023. [DOI] [PubMed] [Google Scholar]
- 3.Podjarny E, Baylis C, Losonczy G. Animal models of preeclampsia. Semin. Perinatol. 1999;23:2–13. doi: 10.1016/s0146-0005(99)80055-x. [DOI] [PubMed] [Google Scholar]
- 4.Maynard SE, et al. Excess placental soluble fms-like tyrosine kinase 1 (sFlt1) may contribute to endothelial dysfunction, hypertension, and proteinuria in preeclampsia. J. Clin. Invest. 2003;111:649–658. doi:10.1172/JCI200317189. doi: 10.1172/JCI17189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Eremina V, et al. Glomerular-specific alterations of VEGF-A expression lead to distinct congenital and acquired renal diseases. J. Clin. Invest. 2003;111:707–716. doi:10.1172/JCI200317423. doi: 10.1172/JCI17423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.King BF. Ultrastructural differentiation of stromal and vascular components in early macaque placental villi. Am. J. Anat. 1987;178:30–44. doi: 10.1002/aja.1001780105. [DOI] [PubMed] [Google Scholar]
- 7.Goldman-Wohl D, Yagel S. Regulation of trophoblast invasion: from normal implantation to pre-eclampsia. Mol. Cell. Endocrinol. 2002;187:233–238. doi: 10.1016/s0303-7207(01)00687-6. [DOI] [PubMed] [Google Scholar]
- 8.Zhou Y, et al. Vascular endothelial growth factor ligands and receptors that regulate human cytotrophoblast survival are dysregulated in severe preeclampsia and hemolysis, elevated liver enzymes, and low platelets syndrome. Am. J. Pathol. 2002;160:1405–1423. doi: 10.1016/S0002-9440(10)62567-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mattot V, et al. Loss of the VEGF(164) and VEGF(188) isoforms impairs postnatal glomerular angiogenesis and renal arteriogenesis in mice. J. Am. Soc. Nephrol. 2002;13:1548–1560. doi: 10.1097/01.asn.0000013925.19218.7b. [DOI] [PubMed] [Google Scholar]