Abstract
Objective
This study examined the relationship between initiation of outpatient mental health service use and level of child welfare involvement.
Methods
Three levels of child welfare involvement were examined: in-home care and no child welfare services beyond an initial investigation, in-home care and additional child welfare services, and placement in out-of-home care (foster care). Longitudinal data were collected for a subsample of children (N=3,592) aged two through 14 years who were enrolled in the National Survey of Child and Adolescent Well-Being, a nationally representative sample of children undergoing investigation for abuse or neglect. Event history analysis was used to model relative risk of initiation of mental health service use over time.
Results
Hazard functions revealed a large increase in onset of mental health services immediately after the time of the initial contact with child welfare, varying by level of child welfare involvement and leveling off by three months after the initial contact. The multivariate Cox proportional-hazards model indicated that compared with children who were placed in out-of-home care, those in in-home care who did not receive any further child welfare services were about one-third as likely to use mental health services and those in in-home care who received additional child welfare services were one-half as likely to use mental health services. Other covariates in the model predicted mental health service use, including being older, being Caucasian, having a history of maltreatment (specifically, physical abuse, physical neglect, or abandonment), being uninsured, and need for mental health services, as measured by the Child Behavior Checklist.
Conclusions
Contact with child welfare functions as a gateway into mental health services for children in child welfare, even when need for such services is controlled for.
Each year thousands of children in the United States come into contact with the child welfare and protective service systems (hereafter, termed “child welfare”) because of allegations of abuse or neglect. In 2002 an estimated 896,000 children were determined after investigation to be victims of child abuse or neglect. Of these children, more than four-fifths remained in their homes of origin and received varying levels of in-home child welfare services; the rest were placed into foster care (1).
Children investigated by child welfare are at high risk of mental health problems. Research over the past decade has clearly documented high rates of emotional and behavioral problems among children removed from their homes and placed into out-of-home care (2–7). In addition, high rates of need have been documented among children who receive child welfare services but remain in their homes of origin (2,8,9).
Also, rates of mental health service use in this population are known to be high (5). Consistent results for children in out-of-home care have emerged from analyses of Medicaid administrative data from California, Washington State, and Pennsylvania, as well as caregiver survey data from California and North Carolina (9–14). Children in out-of-home care use mental health services at rates approximately five to eight times those of children who live in poverty (5,15); these rates are comparable to those of disabled children who receive Supplemental Security Income (12). The high rates of mental health service use among children in foster care have led some to hypothesize that the foster care system may act as a gateway into mental health care (5). However, no longitudinal studies have directly examined the degree to which placement in out-of-home care functions as a gateway into mental health services.
Even less is known about mental health service use for children who undergo investigation for abuse or neglect but remain in their homes of origin. Farmer and colleagues’ (9) Great Smoky Mountains study indicated that children who have contact with social services and remain in their home of origin have lifetime rates of mental health service use comparable to those of children in out-of-home care. The study also showed that contact with social services (with or without placement in foster care) was associated with rates of service use that were higher than those of children who live in poverty with no social service contact. In contrast, recent analyses suggest that children who live in their homes of origin have high levels of need but do not have access to services at the same rate as children in out-of-home care (2,16). Little information exists about rates of mental health service use among the large numbers of children in homes where no child welfare services are provided beyond an initial investigation.
Existing research thus raises questions about whether contact with child welfare services results in increased mental health service use. If the answer to this question is affirmative, a subsequent question involves the degree to which the onset of mental health service use is driven by contact with child welfare (investigative services) or by placement in out-of-home care. Understanding the role that child welfare plays in the onset of mental health service use for these vulnerable children has important implications for mental health services and policies because of the substantial risks of emotional and behavioral problems faced by all children who come into contact with child welfare, whether or not they are removed from their homes of origin.
This study used event history analysis to address the following questions: Does the likelihood of mental health service use increase upon contact with child welfare? Do increases in mental health service use follow similar trajectories for children whose families have different levels of involvement with child welfare, including those who receive in-home care but do not receive child welfare services beyond an initial investigation, those who receive in-home care and additional child welfare services, and those who are placed in out-of-home care? When the analyses control for known covariates from previous studies, does level of child welfare involvement explain mental health service use?
The high rates of mental health service use among children in foster care have led some to hypothesize that the foster care system may act as a gateway into mental health care.
Methods
This research used data from the National Survey of Child and Adolescent Well-Being (NSCAW), the first national prospective study that examined the experiences of children and families involved with child welfare. The NSCAW cohort included children, from birth to the age of 14 years at the time of sampling, who had contact with the child welfare system during a 15-month period that began in October 1999. The final sample included 5,501 children. Further details of the NSCAW sampling plan and procedures have been described in detail elsewhere (Biemer P, Liu J, Iannacchione I, et al, unpublished data, 1998). Approval for this study was given by the U.S. Office of Management and Budget and the institutional review boards of the Research Triangle Institute, the University of North Carolina, Children’s Hospital, San Diego, and by state or county institutional review boards that represented communities involved with the study. Face-to-face informed consent was obtained by trained field representatives at the time of the baseline interview in accordance with the principles outlined in the Declaration of Helsinki (17).
This research investigated a selected subset of children (N=3,592) who were at least two years of age at the baseline interview. This subset was selected to correspond to the age-related measures of need for mental health services applied in this research.
Procedures
Field representatives conducted face-to-face interviews with child welfare workers and caregivers; data were entered directly onto laptop computers. Baseline interviews with child welfare workers were completed a mean±SD of 5.1±2.1 months after the onset of the child welfare investigation and were compared with caregivers a mean of 5.5±2.0 months after the onset of the investigation. Wave 2 and wave 3 follow-up interviews with caregivers were conducted on average 13.6±1.7 and 20.5±1.3 months, respectively, after the onset of the child welfare investigation.
Measures
Baseline levels of child welfare involvement were obtained from case records and interviews with the child welfare worker. The levels of involvement were documented: resides in the home with a biological parent and did not receive child welfare services beyond an initial investigation, resides in the home with a biological parent and received additional child welfare services, and was placed in out-of-home care (foster care).
Sociodemographic characteristics of the children (age, gender, and race or ethnicity) were obtained from caregivers.
Maltreatment history was obtained from child welfare workers who identified alleged types of maltreatment for the current episode of child welfare involvement by using a modified Maltreatment Classification Scale (18). Children could receive codes for more than one type of maltreatment. Six dummy-coded maltreatment variables were created: physical abuse, sexual abuse, emotional abuse, supervisory neglect, physical neglect, and abandonment.
Need for mental health services was obtained from caregivers through the Child Behavior Checklist (CBCL) (19). The CBCL is a widely used measure of behavior problems with established reliability and validity that has been standardized by age and gender with large populations of children from different socioeconomic backgrounds (19) and has previously been used in research with child welfare populations (5,20,21). Two forms of the CBCL were used: one for children aged two to three years and another for children aged four to 18 years. Three standardized scores, normed by age and gender, were obtained: an internalizing problems score, an externalizing problems score, and a total problems score. Youths were considered in need of mental health services if they scored in the clinical range (64 or above) on the internalizing, externalizing, or total problem subscales of the CBCL. The clinical cutoff point, rather than the borderline range, was used in the multivariate model to avoid inflating the estimate of need.
Use of mental health services was measured by using an adapted version of the Child and Adolescent Services Assessment (22). Caregivers were asked at baseline, 12 months, and 18 months about service use from the following settings: clinic-based specialty mental health services (for example, community mental health clinics); therapeutic nursery; day treatment; private professionals, such as psychiatrists, psychologists, social workers, and psychiatric nurses; and family doctors or other medical doctors. A variable was created for the month of the first mental health service, ranging from five months before the contact date (initiation of the child welfare investigation) to the time of the 18-month interview.
Analyses
This study used event history analysis to examine the relationship between the level of child welfare involvement and the likelihood of the onset of mental health service use, while the analyses controlled for key covariates identified in previous research. This statistical approach has been used to describe changes in the likelihood of an event across time for different groups.
Univariate analyses were initially conducted to assess the reliability of these associations. Subsequent to univariate analyses, a test of the proportionality assumption was conducted by testing for an interaction between each of the covariates and time (23). No signification interactions were found, and a proportional hazards model was employed to simultaneously estimate the relationships of multiple predictors with the likelihood of initiation of mental health service use. The proportional hazards model provides relative risk ratios for each variable included in the model while controlling for the other variables in the model. Because data were collected from respondents across multiple time points, early censoring (that is, before 18 months after contact with child welfare) occurred for some observations. However, such censoring was addressed naturally as part of the multivariate Cox proportional-hazards model. Sample weights and the two-stage cluster sample design were accounted for in all analyses, which used the statistical software SUDAAN, version 8.0 (24).
Results
Sample characteristics
Table 1 displays the sample’s weighted data. Two-thirds of the sample (2,486 children, or 69.0 percent) were six to 14 years old, and the proportions of males and females were equivalent. A majority of children were Caucasian (1,622 children, or 46.7 percent) or African American (1,078 children, or 28.4 percent). Almost one-third of the children (1,454 children, or 37.4 percent) had a T score on the CBCL total problem, externalizing, or internalizing subscales at or above 64. Physical abuse, physical neglect, and supervisory neglect were the most common types of abuse experienced. Most children (2,363 children, or 58.7 percent) had public insurance. For the level of child welfare involvement, 1,350 children (70.9 percent) remained in their home of origin and did not receive further child welfare services, 1,534 children (21.1 percent) remained in their home of origin and received additional child welfare services, and 708 (8.1 percent) were placed in out-of-home care. Table 1 also includes the proportion of children who received mental health services for each of the variables included in the multivariate model.
Table 1.
Use of outpatient mental health services in a cohort of children investigated by child welfare for alleged child abuse or neglect, as reported by caregiversa
| Total (N=3,592)
|
Received outpatient mental health services (N=1,116)b |
||||
|---|---|---|---|---|---|
| Baseline characteristics of children | N | % | N | % | SE |
| Child welfare involvement | |||||
| In-home care and did not receive further child welfare services | 1,350 | 70.9 | 250 | 18.2 | 1.7 |
| In-home care and received additional child welfare services | 1,534 | 21.1 | 485 | 24.3 | 2.6 |
| Out-of-home care | 708 | 8.1 | 381 | 50.7 | 4.3 |
| Age (years) | |||||
| 2 to 3 | 578 | 14.4 | 84 | 9.2 | 1.9 |
| 4 to 5 | 528 | 16.6 | 138 | 21.7 | 3.5 |
| 6 to 10 | 1,402 | 41.9 | 457 | 20.5 | 2.5 |
| 11 to 14 | 1,084 | 27.1 | 437 | 31.7 | 3.0 |
| Gender | |||||
| Female | 1,886 | 50.6 | 590 | 22.1 | 2.1 |
| Male | 1,706 | 49.4 | 526 | 22.1 | 1.9 |
| Race or ethnicity | |||||
| Caucasian | 1,622 | 46.7 | 597 | 26.2 | 1.9 |
| African American | 1,078 | 28.4 | 259 | 17.8 | 2.1 |
| Hispanic | 606 | 17.8 | 162 | 18.8 | 4.2 |
| Other | 276 | 7.1 | 95 | 21.5 | 4.8 |
| Child Behavior Checklist scorec | |||||
| 64 or greater | 1,454 | 37.4 | 682 | 34.9 | 2.8 |
| Less than 64 | 2,100 | 62.6 | 420 | 14.4 | 1.6 |
| Maltreatment type (not mutually exclusive) | |||||
| Physical abuse | |||||
| Yes | 1,078 | 35.4 | 372 | 26.4 | 2.7 |
| No | 2,239 | 64.6 | 675 | 20.1 | 1.5 |
| Sexual abuse | |||||
| Yes | 609 | 13.3 | 265 | 25.4 | 3.6 |
| No | 2,708 | 86.7 | 782 | 21.9 | 1.7 |
| Physical neglect | |||||
| Yes | 861 | 24.8 | 246 | 16.4 | 2.3 |
| No | 2,456 | 75.2 | 801 | 24.3 | 1.8 |
| Supervisory neglect | |||||
| Yes | 1,376 | 39.5 | 416 | 22.6 | 2.4 |
| No | 1,941 | 60.5 | 631 | 22.1 | 1.8 |
| Emotional abuse | |||||
| Yes | 429 | 11.9 | 160 | 27.3 | 5.8 |
| No | 2,888 | 88.1 | 887 | 21.7 | 1.4 |
| Abandonment | |||||
| Yes | 151 | 1.9 | 64 | 37.4 | 9.5 |
| No | 3,166 | 98.1 | 983 | 22.0 | 1.5 |
| Insurance status | |||||
| Public | 2,363 | 58.7 | 784 | 23.5 | 2.0 |
| Private and military | 805 | 28.4 | 230 | 22.4 | 2.3 |
| No insurance | 365 | 12.9 | 84 | 14.6 | 3.5 |
Outpatient mental health services received since investigation start date. Ns are unweighted, and percentages are weighted.
22.1 percent of the children received outpatient mental health services; SE=1.5
Possible scores range from 0 to 100, with higher scores indicating increased need.
Use of mental health services during the study period
Figure 1 displays the smoothed hazard rate for the onset of mental health service use over time for each of the three levels of involvement. To stabilize and discern the shape of the hazard function, kernel smoothing was used (25). The graph indicates that the likelihood of the onset of mental health service use increased immediately after contact with child welfare for all three study groups. However, the increase in the hazard rate for children in out-of-home care was much larger than that for children who remained in their homes. For all groups, the likelihood of the onset of mental health service use decreased after the initial contact with child welfare, remaining higher than the rate before the contact date only for children in out-of-home care.
Figure 1.
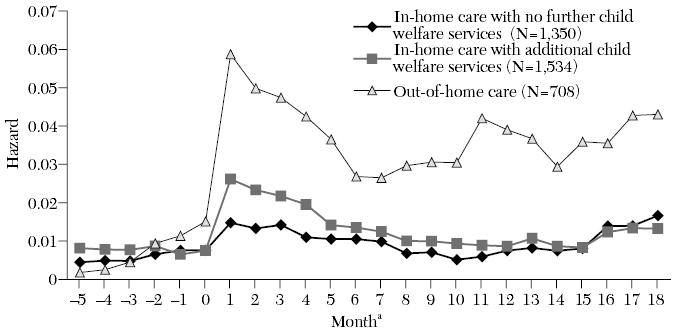
Smoothed hazard function displaying onset of mental health service use over time in a cohort of children investigated for possible child abuse or neglect, by level of child welfare involvement (N=3,592)
a Time frame is from five months before the initial contact with child welfare to 18 months after the contact; time zero is the contact date with child welfare.
Figure 2 further examines service use over time and displays the cumulative percentage of children who used mental health services by level of involvement. The cumulative percentage of children who used mental health services increased most rapidly for children in out-of-home care and most slowly for children in in-home care who did not receive any further child welfare services.
Figure 2.
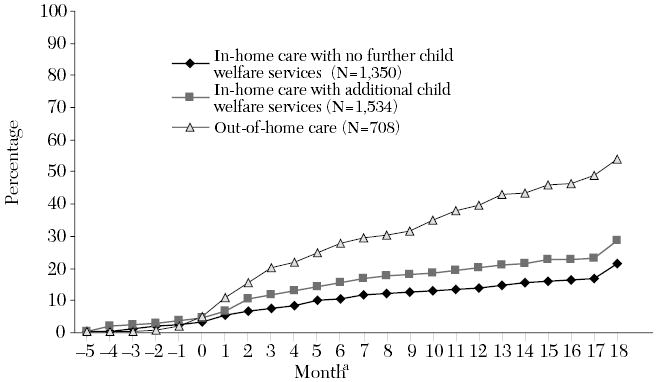
Cumulative percentage of mental health service use over time in a cohort of children investigated for possible child abuse or neglect, by level of child welfare involvement (N=3,592)
a Percentages are weighted. Time frame is from five months before the initial contact with child welfare to 18 months after the contact; time zero is contact date with child welfare.
We next examined mental health service use by need for each of the three groups (percentages are weighted). Need varied by level of child welfare involvement: 356 children (53.4 percent) in out-of-home care scored at or above the cutoff point of 64, compared with 476 (35.4 percent) in in-home care who did not receive any further child welfare services and 622 (38.5 percent) in in-home care who received additional child welfare services (in-home care and no child welfare services compared with placement in out-of-home care, N=2,034, χ2=12.64, df=1, p<.001; in-home care and additional child welfare services compared with out-of-home care, N=2.214, χ2= 10.35, df=1, p<.002). We then examined service use for children with CBCL scores greater than or equal to 64. A total of 245 children placed in out-of-home care (64.0 percent) had CBCL scores at or above the cutoff point of 64 and had initiated mental health service use during the 18-month study period, compared with 285 (35.4 percent) of those in in-home care who received additional child welfare services and 152 (29.8 percent) of those in in-home care who did not receive further child welfare services (in-home care and no child welfare services compared with out-of-home care, N=832, χ2=17.58, df=1, p<.001; in-home care and additional child welfare services compared with out-of-home care, N=978, χ2=12.06, df= 1, p<.001).
Multivariate analyses
As shown in Table 2, further exploration of the impact of child welfare involvement was conducted by using a multivariate Cox proportional-hazards model. Our principal research question: Does level of child welfare involvement contribute to mental health service use above and beyond the impact of sociodemographic and need factors previously described in the research literature?
Table 2.
Multivariate model of use of outpatient mental health services in a cohort of children investigated by child welfare for alleged child abuse or neglect, as reported by caregivers (N=3,117)a
| Baseline characteristics of children | Beta estimate | SE | Hazard ratio | 95% CI | p |
|---|---|---|---|---|---|
| Child welfare involvement | <.001 | ||||
| In-home care and did not receive further child welfare services | −1.18 | .22 | .31 | .20–.47 | |
| In-home care and received further child welfare services | −.81 | .21 | .45 | .29–.68 | |
| Out-of-home care | — | 1.00 | |||
| Age (years) | .02 | ||||
| 2 to 3 | −1.07 | .33 | .34 | .18–.66 | |
| 4 to 5 | −.18 | .23 | .84 | .53–1.33 | |
| 6 to 10 | −.3 | .19 | .74 | .51–1.07 | |
| 11 to 14 | — | 1.00 | |||
| Gender | .51 | ||||
| Male | .12 | .19 | 1.13 | .78–1.65 | |
| Female | — | ||||
| Race or ethnicity | .01 | ||||
| African American | −.59 | .2 | .55 | .37–.82 | |
| Hispanic | −.51 | .25 | .60 | .36–1.00 | |
| Other | −.3 | .29 | .74 | .41–1.32 | |
| Caucasian | — | 1.00 | |||
| Maltreatment type (not mutually exclusive) | |||||
| Physical abuse (reference, not abused) | .31 | .15 | 1.36 | 1.01–1.83 | <.05 |
| Sexual abuse (reference, not abused) | .25 | .2 | 1.28 | .86–1.93 | .22 |
| Physical neglect (reference, not neglected) | −.43 | .2 | .65 | .44–.98 | .04 |
| Supervisory neglect (reference, not neglected) | .02 | .13 | 1.02 | .78–1.33 | .88 |
| Emotional abuse (reference, not abused) | .10 | .22 | 1.10 | .71–1.71 | .67 |
| Abandonment (reference, not abandoned) | .61 | .23 | 1.85 | 1.17–2.93 | <.01 |
| Child Behavior Checklist scoreb | |||||
| 64 or greater | .87 | .17 | 2.39 | 1.71–3.33 | <.001 |
| Less than 64 | — | ||||
| Insurance | <.05 | ||||
| Public | .69 | .28 | 1.99 | 1.15–3.46 | |
| Private and military | .65 | .3 | 1.91 | 1.05–3.49 | |
| None | — | 1.00 |
Event history analysis models the risk or hazard of an event occurring. The interpretation of the risk ratio is analogous to that of an odds ratio.
Possible scores range from 0 to 100, with higher scores indicating higher need.
With regard to the main variable of interest (child welfare involvement), the multivariate model demonstrated that compared with children in out-of-home care, children in in-home care who did not receive further child welfare services were .31 times as likely to use mental health services, and children in in-home care who received child welfare services were .45 times as likely to receive mental health services (F=14.96, df=2, 3,117, p<.001), even when other variables, such as need, were included in the model.
Several other covariates significantly predicted the onset of outpatient mental health service use when the analyses controlled for the other variables in the model. For age, children aged two to three were .34 times as likely as children aged 11 to 14 years to receive services (F=3.65, df=3, 3,117, p<.05). Rates of service use also differed by race or ethnicity (F=3.92, df=3, 3,117, p=.01). African-American children were .55 times as likely as Caucasian children to receive services. Although Hispanic children were .60 times as likely as Caucasian children to receive services, the confidence interval indicates that the finding was not significant.
Children with need for mental health services, as measured by the CBCL, were 2.39 times as likely as children without such a need to receive services (F= 27.05, df=1, 3,117, p<.001). Children with a history of abandonment were 1.85 times as likely as those without such a history to receive services (F=7.11, df=1, 3,117, p<.01). Other covariates that showed significance included physical abuse (F=4.11, df=1, 3,117, p<.05), physical neglect (F=4.44, df=1, 3,117, p<.05), and insurance (F=3.16, df=2, 3,117, p<.05). Gender and three types of abuse (sexual, emotional, and supervisory neglect) were not related to service use.
Discussion and conclusions
This study demonstrated that child welfare involvement that followed investigation of alleged abuse or neglect acts as a gateway to services: rates of mental health service use for all levels of child welfare involvement increased immediately after contact with child welfare. Second, children who remained in their home without child welfare services were least likely to gain access to mental health services and children in out-of-home care were most likely to gain access to such services, even when the analyses controlled for need. These findings suggest a high level of unmet need, particularly among children who do not enter out-of-home care. Similar to previous studies (21,26–28), our study found that covariates including need, age, race or ethnicity, and type of abuse were also related to service use in the multivariate model.
These findings have several important clinical, research, and policy implications. From these data, it is clear that child welfare involvement acts as a gateway to mental health services, although a precise evaluation of the mechanisms underlying the increase was not possible in the study reported here. The temporal pattern of onset of service use suggests that a brief elevation in service onset occurs for all children after the initial contact. This initial increase may be related to the case worker’s scrutiny of the child’s well-being as part of the investigation, or it may be related to referrals to mental health services generated simultaneously by the health care or school professionals who made the initial referral to child welfare. Over time, only children in out-of-home care continued to enter mental health services at a rate higher than the rate before their contact with child welfare, suggesting that additional mechanisms are in play for these children. Mechanisms might include standardized assessment procedures for evaluating children, as recommended by the Child Welfare League of America and the American Academy of Pediatrics (29); caseworker needs assessment; caregiver pressure on case workers for access to services; or court oversight procedures (26,30). Understanding these potential mechanisms is critical to ensure that children with need are able to gain access to necessary services.
Current findings also point to significant areas of unmet need, particularly for children who remain in their homes, where close to two-thirds of all children with CBCL scores greater than or equal to 64 did not initiate services over the 18-month period after contact with child welfare. Improved identification of need and access to intensive interventions may be important to positively affect developmental and mental health trajectories for these children and potentially negating the need for later out-of-home placement.
The findings also stress that factors other than need, as measured by the CBCL, are related to mental health service use. Some of these findings—for example, the impact of race or ethnicity on service use—have been published previously and relate to factors such as court proceedings and racial or cultural differences in attitudes toward mental health care (16,21,26,28). In addition, our findings about the impact of physical abuse and abandonment suggest that other mental health risk factors that are not measured by the CBCL, such as maltreatment history, also predict mental health services use.
This study has several limitations. First, we chose to use the more conservative clinical cutoff point of the CBCL, rather than the borderline cutoff point, to avoid inflating the estimate of need. It is likely that some children who scored below the cutoff point for the clinical range also had clinically relevant problems. Second, we used child welfare involvement at the initial interview as our primary independent variable and did not control for changes in involvement over time. Third, we were unable to look at content of mental health services to determine if visits were primarily focused on assessment, psychosocial support related to the investigation or removal from the home, or treatment of specific disorders. In addition, this study did not investigate factors that predicted duration of mental health services and termination of use or outcomes related to service use.
Nevertheless, this study confirms that mental health service use increased after contact with child welfare and suggests that onset of service use is related to level of involvement in child welfare. It is an important first step in longitudinal analyses of mental health service use for a national cohort of children who were undergoing investigation for possible abuse or neglect. Our findings demonstrate that the child welfare and mental health systems interact in more rational ways than has been previously believed and depicted. However, findings also show that significant gaps in services remain despite considerable need, particularly for children who remain in their homes. Greater attention needs to be paid to identifying children’s need for mental health services at all levels of child welfare involvement and closing the need-use gap. ♦
Acknowledgments
This research was supported through the Caring for Children in Child Welfare (CCCW) study, funded by grant MH-59672-02 from the National Institute of Mental Health. The CCCW is a collaborative effort between the Child and Adolescent Services Research Center at Children’s Hospital–San Diego, the department of psychiatry at the University of Pittsburgh, the Columbus Children’s Hospital, the Epidemiology and Services Research Group at Duke University, and the Research Triangle Institute. It should be noted that this research was conducted in collaboration with the National Survey on Child and Adolescent Well-Being, which was developed under contract with the Administration on Children and Families, U.S. Department of Health and Human Services.
References
- 1.Child Maltreatment 2002. Washington, DC, US Department of Health and Human Services, Administration on Children, Youth and Families, 2004
- 2.Burns B, Phillips S, Wagner R, et al. Mental health need and access to mental health services by youth involved with child welfare: a national survey. Journal of the American Academy of Child Adolescent Psychiatry. 2004;43:960–970. doi: 10.1097/01.chi.0000127590.95585.65. [DOI] [PubMed] [Google Scholar]
- 3.Clausen JM, Landsverk J, Ganger W, et al. Mental health problems of children in foster care. Journal of Child and Family Studies. 1998;7:283–296. [Google Scholar]
- 4.Code Blue: Health Services for Children in Foster Care. Sacramento, Calif, California State University, Sacramento, Institute for Research on Women and Families, 1998
- 5.Landsverk J, Garland AF, Leslie LK. Mental health services for children reported to child protective services, in APSAC Handbook on Child Maltreatment, 2nd ed. Edited by Myers JEB, Hendrix CT, Berliner L, et al. Thousand Oaks, Calif, Sage, 2002
- 6.Pilowsky D. Psychopathology among children placed in family foster care. Psychiatric Services. 1995;46:906–910. doi: 10.1176/ps.46.9.906. [DOI] [PubMed] [Google Scholar]
- 7.Simms MD, Halfon N. The health care needs of children in foster care: a research agenda. Child Welfare. 1994;73:505–24. [PubMed] [Google Scholar]
- 8.Berrick JD, Barth RP, Needell B. A comparison of kinship foster homes and foster family homes: implications for kinship foster care as family preservation. Children and Youth Services Review. 1994;16:33–63. [Google Scholar]
- 9.Farmer EMZ, Burns BJ, Chapman MV, et al. Use of mental health services by youth in contact with social services. Social Services Review. 2001;75:605–624. [Google Scholar]
- 10.Halfon N, Berkowitz G, Klee L. Children in foster care in California: an examination of Medicaid reimbursed health services utilization. Pediatrics. 1992;89:1230–1237. [PubMed] [Google Scholar]
- 11.Halfon N, Berkowitz G, Klee L. Mental health service utilization by children in foster care in California. Pediatrics. 1992;89:1238–1244. [PubMed] [Google Scholar]
- 12.Harman JS, Childs GE, Kelleher KJ. Mental health care utilization and expenditures by children in foster care. Archives of Pediatric and Adolescent Medicine. 2000;154:1114–1117. doi: 10.1001/archpedi.154.11.1114. [DOI] [PubMed] [Google Scholar]
- 13.Landsverk J, Litrownik A, Newton R. et al. Psychological Impact of Child Maltreatment: Final Report to the National Center on Child Abuse and Neglect. San Diego, Child and Family Research Group, 1996
- 14.Takayama JI, Bergman AB, Connell FA. Children in foster care in the state of Washington: health care utilization and expenditures. JAMA. 1994;271:1850–1855. [PubMed] [Google Scholar]
- 15.Bilaver LA, Jaudes PK, Koepke D, et al. The health of children in foster care. Social Services Review. 1999;73:401–417. [Google Scholar]
- 16.Hurlburt MS, Leslie LK, Landsverk J, et al. Contextual predictors of mental health service use among a cohort of children open to child welfare. Archives of General Psychiatry. 2004;61:1217–1224. doi: 10.1001/archpsyc.61.12.1217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.World Medical Association Declaration of Helsinki. ethical principles for medical research involving human subjects. JAMA. 2000;284:3043–3044. [PubMed] [Google Scholar]
- 18.Manly J, Cicchetti D, Barnett D. The impact of subtype, frequency, chronicity, and severity of child maltreatment on social competence and behavior problems. Development and Psychopathology. 1994;6:121–143. [Google Scholar]
- 19.Achenbach TM. Manual for the Child Behavior Checklist/4–18 and 1991 Profile. Burlington, Vt, University of Vermont, Department of Psychiatry, 1991
- 20.Simms MD. The Foster Care Clinic: a community program to identify treatment needs of children in foster care. Journal of Developmental and Behavioral Pediatrics. 1989;10:121–128. [PubMed] [Google Scholar]
- 21.Garland AF, Landsverk J, Hough RL, et al. Type of maltreatment as a predictor of mental health service use for children in foster care. Child Abuse and Neglect. 1996;20:675–688. doi: 10.1016/0145-2134(96)00056-7. [DOI] [PubMed] [Google Scholar]
- 22.Burns BJ, Angold A, Costello EJ. Measuring child, adolescent, and family service use, in Evaluating Mental Health Services for Children. Edited by Bickman L, Rog DJ. San Francisco, Jossey-Bass Publishers, 1992
- 23.Allison PD. Survival Analysis Using the SAS System: A Practical Guide. Cary, NC, SAS Institute, 1995
- 24.Dowd K, Kinsey S, Wheeless S, et al. National Survey of Child and Adolescent Well-Being (NSCAW): Wave 1 Data File User’s Manual. Research Triangle Park, NC, Research Triangle Institute, 2002
- 25.Singer JD, Willett JB. Applied Longitudinal Data Analysis: Modeling Change and Event Occurrence. New York, Oxford University Press, 2003
- 26.Garland AF, Besinger BA. Racial/ethnic differences in court referred pathways to mental health services for children in foster care. Children and Youth Services Review. 1997;19:651–666. [Google Scholar]
- 27.Leslie LK, Kelleher KJ, Burns BJ, et al. Foster care and Medicaid managed care. Child Welfare. 2003;82:367–392. [PubMed] [Google Scholar]
- 28.Leslie LK, Hurlburt MS, Landsverk J, et al. Outpatient mental health services for children in foster care: a national perspective. Child Abuse and Neglect. 2004;28:697–712. doi: 10.1016/j.chiabu.2004.01.004. [DOI] [PubMed] [Google Scholar]
- 29.American Academy of Pediatrics Committee on Early Childhood, Adoption, and Dependent Care. health care of children in foster care. Pediatrics. 1994;93:335–338. [PubMed] [Google Scholar]
- 30.Dicker SD, Gordon E. Harnessing the hidden influence of the courts to enhance the healthy development of foster children. Protecting Children. 2000;16:36–45. [Google Scholar]


