Abstract
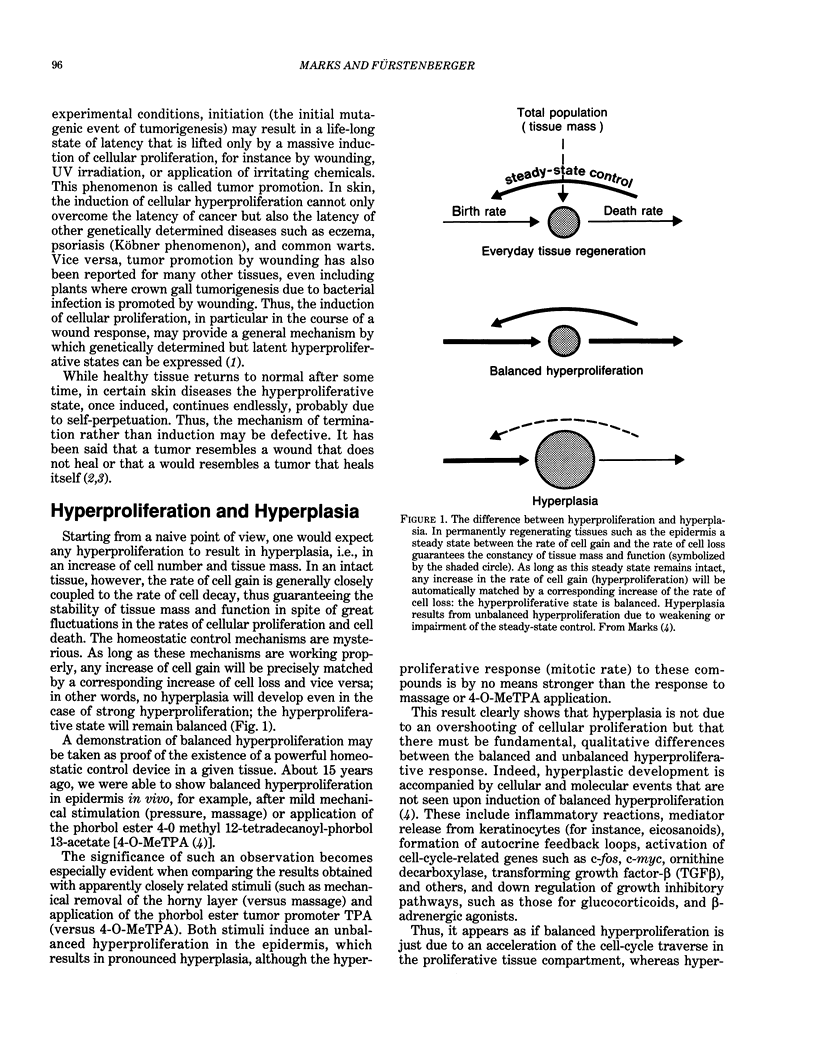
The skin, in particular the epidermis, offers unique opportunities to investigate the induction and control of cellular proliferation and tissue homeostasis both under in vivo and in vitro conditions. Moreover, it represents one of the most feasible model systems for experimental cancer research. As the primary border of the body, the skin has important protective and defensive functions. A general response to external injury consists of a thickening of the epithelial layer (epidermal hyperplasia) combined with an inflammatory reaction. This hyperplastic transformation of the skin is a critical condition of skin tumor development (i.e., conversion and promotion) and of the wound response. It is believed to be due to a transformation of keratinocytes into an activated state characterized by an increased rate of proliferation and the ability to release a series of growth factors and other cytokines that coordinate the defense reaction (e.g., hyperproliferation, recruitment of leukocytes, activation of the immune system) along auto- and paracrine feedback loops. The initial and probably later phases of this response depend critically on a local release of eicosanoids such as prostaglandins and lipoxygenase-generated factors. A unique reaction seen upon phorbol ester treatment of mouse skin is a strong induction of the enzyme 8-lipoxygenase, which might be involved in skin tumor development by catalyzing the generation of clastogenic metabolites thought to play a role in the conversion stage. Hyperplasia may be considered to be the result of an imbalance between the rates of cell gain and cell loss.(ABSTRACT TRUNCATED AT 250 WORDS)
Full text
PDF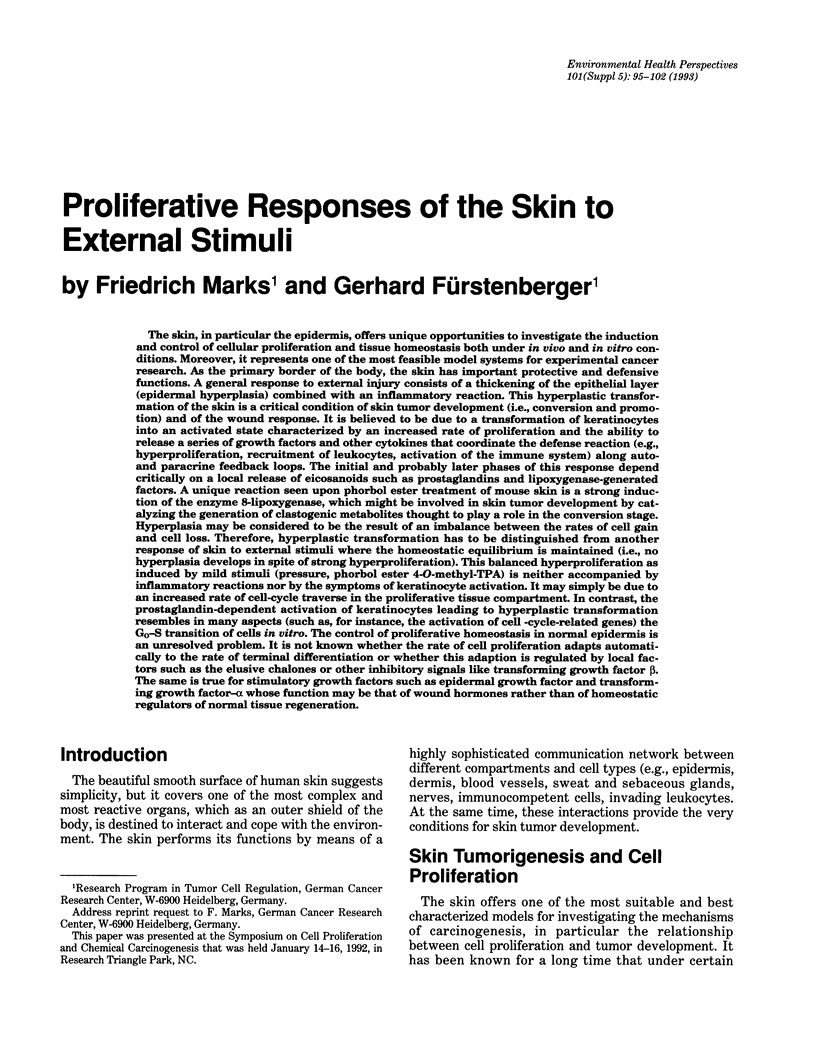


Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Barker J. N., Mitra R. S., Griffiths C. E., Dixit V. M., Nickoloff B. J. Keratinocytes as initiators of inflammation. Lancet. 1991 Jan 26;337(8735):211–214. doi: 10.1016/0140-6736(91)92168-2. [DOI] [PubMed] [Google Scholar]
- Barnard J. A., Lyons R. M., Moses H. L. The cell biology of transforming growth factor beta. Biochim Biophys Acta. 1990 Jun 1;1032(1):79–87. doi: 10.1016/0304-419x(90)90013-q. [DOI] [PubMed] [Google Scholar]
- Bertsch S., Csontos K., Schweizer J., Marks F. Effect of mechanical stimulation on cell proliferation in mouse epidermis and on growth regulation by endogenous factors (chalones). Cell Tissue Kinet. 1976 Sep;9(5):445–457. doi: 10.1111/j.1365-2184.1976.tb01295.x. [DOI] [PubMed] [Google Scholar]
- Clark-Lewis I., Murray A. W. Tumor promotion and the induction of epidermal ornithine decarboxylase activity in mechanically stimulated mouse skin. Cancer Res. 1978 Mar;38(3):494–497. [PubMed] [Google Scholar]
- Coffey R. J., Jr, Sipes N. J., Bascom C. C., Graves-Deal R., Pennington C. Y., Weissman B. E., Moses H. L. Growth modulation of mouse keratinocytes by transforming growth factors. Cancer Res. 1988 Mar 15;48(6):1596–1602. [PubMed] [Google Scholar]
- Dvorak H. F. Tumors: wounds that do not heal. Similarities between tumor stroma generation and wound healing. N Engl J Med. 1986 Dec 25;315(26):1650–1659. doi: 10.1056/NEJM198612253152606. [DOI] [PubMed] [Google Scholar]
- Folkman J., Klagsbrun M. Angiogenic factors. Science. 1987 Jan 23;235(4787):442–447. doi: 10.1126/science.2432664. [DOI] [PubMed] [Google Scholar]
- Folkman J. Tumor angiogenesis. Adv Cancer Res. 1985;43:175–203. doi: 10.1016/s0065-230x(08)60946-x. [DOI] [PubMed] [Google Scholar]
- Fürstenberger G., Berry D. L., Sorg B., Marks F. Skin tumor promotion by phorbol esters is a two-stage process. Proc Natl Acad Sci U S A. 1981 Dec;78(12):7722–7726. doi: 10.1073/pnas.78.12.7722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fürstenberger G., Rogers M., Schnapke R., Bauer G., Höfler P., Marks F. Stimulatory role of transforming growth factors in multistage skin carcinogenesis: possible explanation for the tumor-inducing effect of wounding in initiated NMRI mouse skin. Int J Cancer. 1989 May 15;43(5):915–921. doi: 10.1002/ijc.2910430531. [DOI] [PubMed] [Google Scholar]
- Glick A. B., Sporn M. B., Yuspa S. H. Altered regulation of TGF-beta 1 and TGF-alpha in primary keratinocytes and papillomas expressing v-Ha-ras. Mol Carcinog. 1991;4(3):210–219. doi: 10.1002/mc.2940040308. [DOI] [PubMed] [Google Scholar]
- Haddow A. Molecular repair, wound healing, and carcinogenesis: tumor production a possible overhealing? Adv Cancer Res. 1972;16:181–234. doi: 10.1016/s0065-230x(08)60341-3. [DOI] [PubMed] [Google Scholar]
- Kane C. J., Hebda P. A., Mansbridge J. N., Hanawalt P. C. Direct evidence for spatial and temporal regulation of transforming growth factor beta 1 expression during cutaneous wound healing. J Cell Physiol. 1991 Jul;148(1):157–173. doi: 10.1002/jcp.1041480119. [DOI] [PubMed] [Google Scholar]
- Kupper T. S. The activated keratinocyte: a model for inducible cytokine production by non-bone marrow-derived cells in cutaneous inflammatory and immune responses. J Invest Dermatol. 1990 Jun;94(6 Suppl):146S–150S. doi: 10.1111/1523-1747.ep12876130. [DOI] [PubMed] [Google Scholar]
- Luger T. A., Schwarz T. Evidence for an epidermal cytokine network. J Invest Dermatol. 1990 Dec;95(6 Suppl):100S–104S. doi: 10.1111/1523-1747.ep12874944. [DOI] [PubMed] [Google Scholar]
- Marks F., Fürstenberger G. The conversion stage of skin carcinogenesis. Carcinogenesis. 1990 Dec;11(12):2085–2092. doi: 10.1093/carcin/11.12.2085. [DOI] [PubMed] [Google Scholar]
- Marks F., Hanke B., Thastrup O., Fürstenberger G. Stimulatory effect of thapsigargin, a non-TPA-type tumor promoter, on arachidonic acid metabolism in the murine keratinocyte line HEL30 and on epidermal cell proliferation in vivo as compared to the effects of phorbol ester TPA. Carcinogenesis. 1991 Aug;12(8):1491–1497. doi: 10.1093/carcin/12.8.1491. [DOI] [PubMed] [Google Scholar]
- McKay I. A., Leigh I. M. Epidermal cytokines and their roles in cutaneous wound healing. Br J Dermatol. 1991 Jun;124(6):513–518. doi: 10.1111/j.1365-2133.1991.tb04942.x. [DOI] [PubMed] [Google Scholar]
- Nickoloff B. J., Griffiths C. E., Barker J. N. The role of adhesion molecules, chemotactic factors, and cytokines in inflammatory and neoplastic skin disease--1990 update. J Invest Dermatol. 1990 Jun;94(6 Suppl):151S–157S. doi: 10.1111/1523-1747.ep12876134. [DOI] [PubMed] [Google Scholar]
- Norris D. A. Cytokine modulation of adhesion molecules in the regulation of immunologic cytotoxicity of epidermal targets. J Invest Dermatol. 1990 Dec;95(6 Suppl):111S–120S. doi: 10.1111/1523-1747.ep12874977. [DOI] [PubMed] [Google Scholar]
- Ochi T., Cerutti P. A. Clastogenic action of hydroperoxy-5,8,11,13-icosatetraenoic acids on the mouse embryo fibroblasts C3H/10T1/2. Proc Natl Acad Sci U S A. 1987 Feb;84(4):990–994. doi: 10.1073/pnas.84.4.990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sisskin E. E., Gray T., Barrett J. C. Correlation between sensitivity to tumor promotion and sustained epidermal hyperplasia of mice and rats treated with 12-O-tetra-decanoylphorbol-13-acetate. Carcinogenesis. 1982;3(4):403–407. doi: 10.1093/carcin/3.4.403. [DOI] [PubMed] [Google Scholar]
- Slaga T. J., Fischer S. M., Nelson K., Gleason G. L. Studies on the mechanism of skin tumor promotion: evidence for several stages in promotion. Proc Natl Acad Sci U S A. 1980 Jun;77(6):3659–3663. doi: 10.1073/pnas.77.6.3659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wahl S. M., Wong H., McCartney-Francis N. Role of growth factors in inflammation and repair. J Cell Biochem. 1989 Jun;40(2):193–199. doi: 10.1002/jcb.240400208. [DOI] [PubMed] [Google Scholar]
- di Giovine F. S., Duff G. W. Interleukin 1: the first interleukin. Immunol Today. 1990 Jan;11(1):13–20. doi: 10.1016/0167-5699(90)90005-t. [DOI] [PubMed] [Google Scholar]


