Abstract
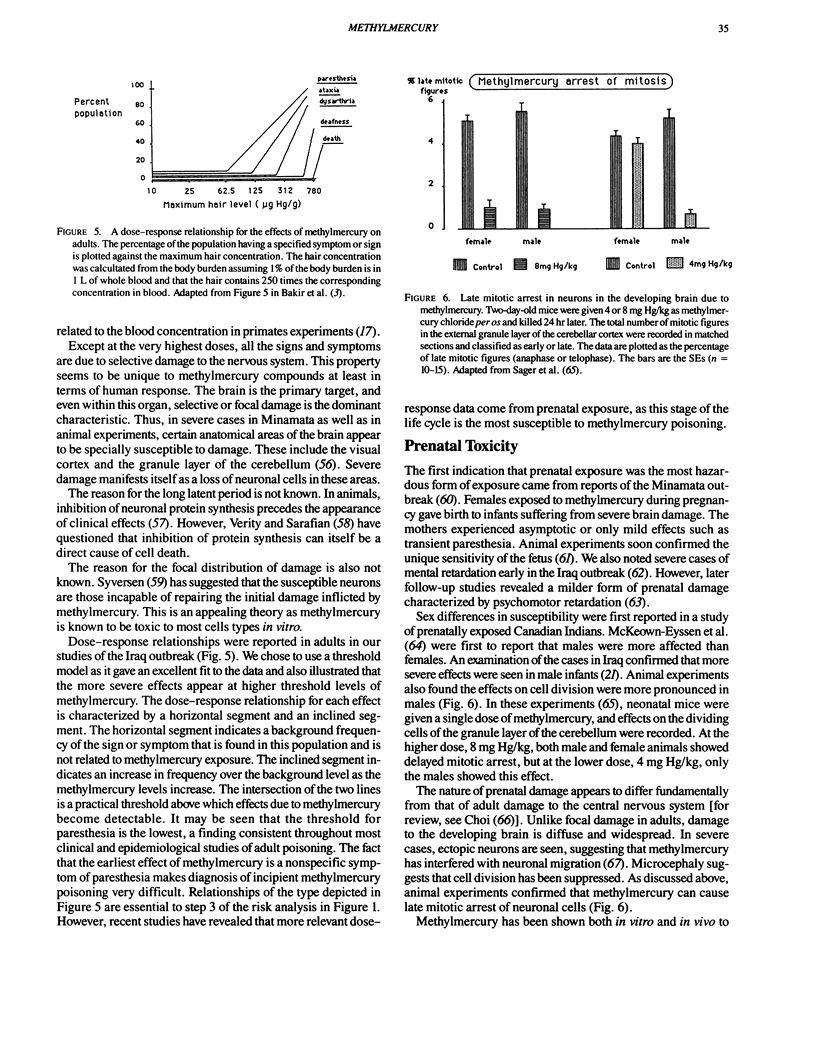
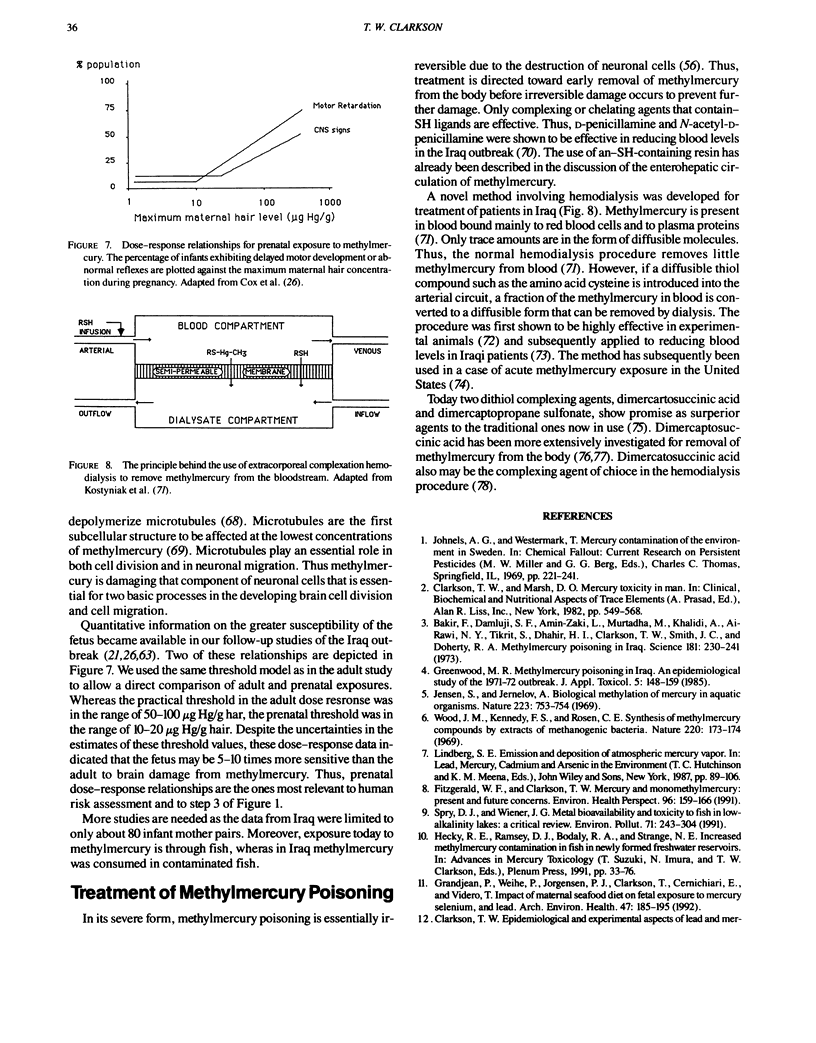
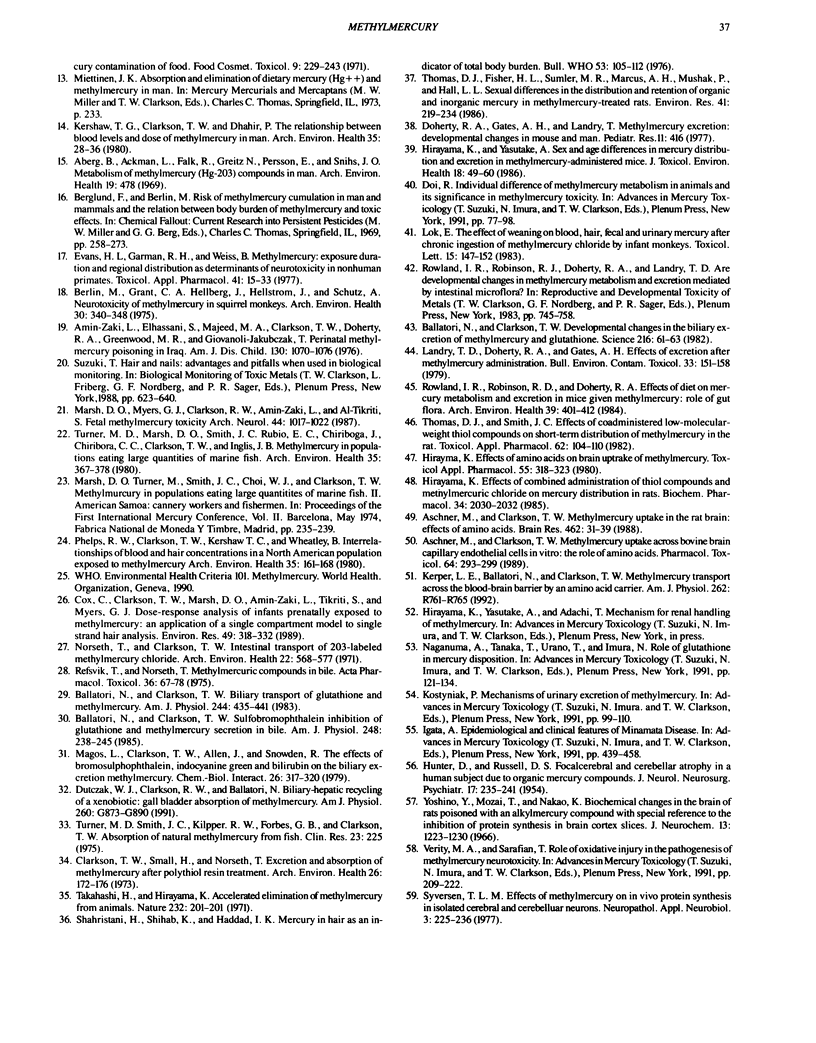
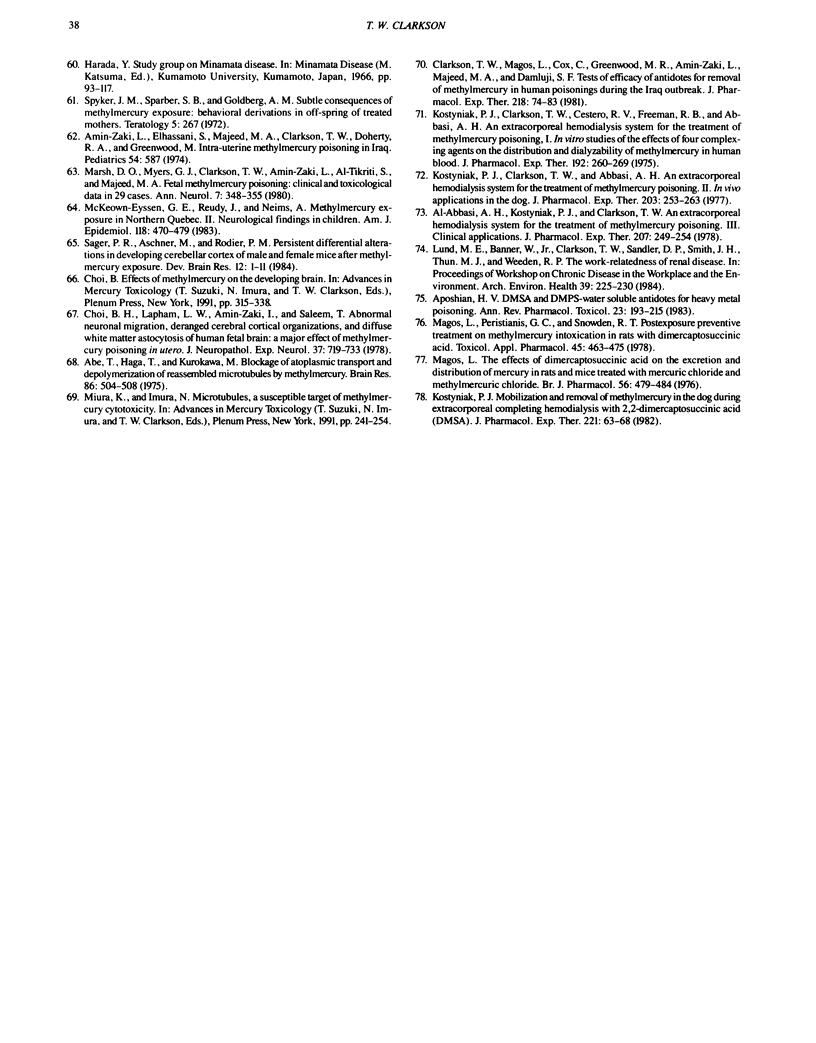
In the past, methylmercury compounds were manufactured as fungicides or appeared as unwanted byproducts of the chemical industry, but today the methylation of inorganic mercury in aquatic sediments and soils is the predominant if not the sole source of methylmercury. This form of mercury is bioaccumulated to a high degree in aquatic food chains to attain its highest concentrations in edible tissues in long-lived predatory fish living in both fresh and ocean waters. It is well absorbed from the diet and distributes within a few days to all tissues in the body. It crosses without hindrance the blood-brain and placental barriers to reach its principal target tissue, the brain. It is eliminated chiefly in the feces after conversion to inorganic mercury. The biological half-time of methylmercury in human tissues is about 50 days, but there is wide individual variation. Adult poisoning is characterized by focal damage to discrete anatomical areas of the brain such as the visual cortex and granule layer of the cerebellum. A latent period of weeks or months may ensue before the appearance of signs and symptoms of poisoning. The latter manifest themselves as paresthesia, ataxia, constriction of the visual fields, and hearing loss. The prenatal period is the most sensitive stage of the life cycle to methylmercury. Prenatally poisoned infants exhibit a range of effects from severe cerebral palsy to subtle developmental delays. Methylmercury is believed to inhibit those processes in the brain specially involved in development and growth such as neuronal cell division and migration.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Abe T., Haga T., Kurokawa M. Blockage of axoplasmic transport and depolymerisation of reassembled microtubules by methyl mercury. Brain Res. 1975 Mar 28;86(3):504–508. doi: 10.1016/0006-8993(75)90904-x. [DOI] [PubMed] [Google Scholar]
- Aberg B., Ekman L., Falk R., Greitz U., Persson G., Snihs J. O. Metabolism of methyl mercury (203Hg) compounds in man. Arch Environ Health. 1969 Oct;19(4):478–484. doi: 10.1080/00039896.1969.10666872. [DOI] [PubMed] [Google Scholar]
- Al-Abbasi A. H., Kostyniak P. J., Clarkson T. W. An extracorporeal complexing hemodialysis system for the treatment of methylmercury poisoning. III. Clinical applications. J Pharmacol Exp Ther. 1978 Oct;207(1):249–254. [PubMed] [Google Scholar]
- Al-Shahristani H., Shihab K., Al-Haddad I. K. Mercury in hair as an indicator of total body burden. Bull World Health Organ. 1976;53 (Suppl):105–112. [PMC free article] [PubMed] [Google Scholar]
- Amin-Zaki L., Elhassani S., Majeed M. A., Clarkson T. W., Doherty R. A., Greenwood M. R., Giovanoli-Jakubczak T. Perinatal methylmercury poisoning in Iraq. Am J Dis Child. 1976 Oct;130(10):1070–1076. doi: 10.1001/archpedi.1976.02120110032004. [DOI] [PubMed] [Google Scholar]
- Amin-Zaki L., Elhassani S., Majeed M. A., Clarkson T. W., Doherty R. A., Greenwood M. Intra-uterine methylmercury poisoning in Iraq. Pediatrics. 1974 Nov;54(5):587–595. [PubMed] [Google Scholar]
- Aposhian H. V. DMSA and DMPS--water soluble antidotes for heavy metal poisoning. Annu Rev Pharmacol Toxicol. 1983;23:193–215. doi: 10.1146/annurev.pa.23.040183.001205. [DOI] [PubMed] [Google Scholar]
- Aschner M., Clarkson T. W. Methyl mercury uptake across bovine brain capillary endothelial cells in vitro: the role of amino acids. Pharmacol Toxicol. 1989 Mar;64(3):293–297. doi: 10.1111/j.1600-0773.1989.tb00650.x. [DOI] [PubMed] [Google Scholar]
- Aschner M., Clarkson T. W. Uptake of methylmercury in the rat brain: effects of amino acids. Brain Res. 1988 Oct 11;462(1):31–39. doi: 10.1016/0006-8993(88)90581-1. [DOI] [PubMed] [Google Scholar]
- Bakir F., Damluji S. F., Amin-Zaki L., Murtadha M., Khalidi A., al-Rawi N. Y., Tikriti S., Dahahir H. I., Clarkson T. W., Smith J. C. Methylmercury poisoning in Iraq. Science. 1973 Jul 20;181(4096):230–241. doi: 10.1126/science.181.4096.230. [DOI] [PubMed] [Google Scholar]
- Ballatori N., Clarkson T. W. Developmental changes in the biliary excretion of methylmercury and glutathione. Science. 1982 Apr 2;216(4541):61–63. doi: 10.1126/science.7063871. [DOI] [PubMed] [Google Scholar]
- Berlin M., Grant C. A., Hellberg J., Hellström J., Schültz A. Neurotoxicity of methylmercury in squirrel monkeys. Cerebral cortical pathology, interference with scotopic vision, and changes in operant behavior. Arch Environ Health. 1975 Jul;30(7):340–348. doi: 10.1080/00039896.1975.10666717. [DOI] [PubMed] [Google Scholar]
- Choi B. H., Lapham L. W., Amin-Zaki L., Saleem T. Abnormal neuronal migration, deranged cerebral cortical organization, and diffuse white matter astrocytosis of human fetal brain: a major effect of methylmercury poisoning in utero. J Neuropathol Exp Neurol. 1978 Nov-Dec;37(6):719–733. doi: 10.1097/00005072-197811000-00001. [DOI] [PubMed] [Google Scholar]
- Clarkson T. W. Epidemiological and experimental aspects of lead and mercury contamination of food. Food Cosmet Toxicol. 1971 Apr;9(2):229–243. doi: 10.1016/0015-6264(71)90308-7. [DOI] [PubMed] [Google Scholar]
- Clarkson T. W., Magos L., Cox C., Greenwood M. R., Amin-Zaki L., Majeed M. A., Al-Damluji S. F. Tests of efficacy of antidotes for removal of methylmercury in human poisoning during the Iraq outbreak. J Pharmacol Exp Ther. 1981 Jul;218(1):74–83. [PubMed] [Google Scholar]
- Clarkson T. W., Small H., Norseth T. Excretion and absorption of methyl mercury after polythiol resin treatment. Arch Environ Health. 1973 Apr;26(4):173–176. doi: 10.1080/00039896.1973.10666251. [DOI] [PubMed] [Google Scholar]
- Cox C., Clarkson T. W., Marsh D. O., Amin-Zaki L., Tikriti S., Myers G. G. Dose-response analysis of infants prenatally exposed to methyl mercury: an application of a single compartment model to single-strand hair analysis. Environ Res. 1989 Aug;49(2):318–332. doi: 10.1016/s0013-9351(89)80075-1. [DOI] [PubMed] [Google Scholar]
- Dutczak W. J., Clarkson T. W., Ballatori N. Biliary-hepatic recycling of a xenobiotic: gallbladder absorption of methyl mercury. Am J Physiol. 1991 Jun;260(6 Pt 1):G873–G880. doi: 10.1152/ajpgi.1991.260.6.G873. [DOI] [PubMed] [Google Scholar]
- Evans H. L., Garman R. H., Weiss B. Methylmercury: exposure duration and regional distribution as determinants of neurotoxicity in nonhuman primates. Toxicol Appl Pharmacol. 1977 Jul;41(1):15–33. doi: 10.1016/0041-008x(77)90051-5. [DOI] [PubMed] [Google Scholar]
- Fitzgerald W. F., Clarkson T. W. Mercury and monomethylmercury: present and future concerns. Environ Health Perspect. 1991 Dec;96:159–166. doi: 10.1289/ehp.9196159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grandjean P., Weihe P., Jørgensen P. J., Clarkson T., Cernichiari E., Viderø T. Impact of maternal seafood diet on fetal exposure to mercury, selenium, and lead. Arch Environ Health. 1992 May-Jun;47(3):185–195. doi: 10.1080/00039896.1992.9938348. [DOI] [PubMed] [Google Scholar]
- Greenwood M. R. Methylmercury poisoning in Iraq. An epidemiological study of the 1971-1972 outbreak. J Appl Toxicol. 1985 Jun;5(3):148–159. doi: 10.1002/jat.2550050305. [DOI] [PubMed] [Google Scholar]
- HUNTER D., RUSSELL D. S. Focal cerebellar and cerebellar atrophy in a human subject due to organic mercury compounds. J Neurol Neurosurg Psychiatry. 1954 Nov;17(4):235–241. doi: 10.1136/jnnp.17.4.235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hirayama K. Effect of amino acids on brain uptake of methyl mercury. Toxicol Appl Pharmacol. 1980 Sep 15;55(2):318–323. doi: 10.1016/0041-008x(80)90093-9. [DOI] [PubMed] [Google Scholar]
- Hirayama K. Effects of combined administration of thiol compounds and methylmercury chloride on mercury distribution in rats. Biochem Pharmacol. 1985 Jun 1;34(11):2030–2032. doi: 10.1016/0006-2952(85)90328-4. [DOI] [PubMed] [Google Scholar]
- Hirayama K., Yasutake A. Sex and age differences in mercury distribution and excretion in methylmercury-administered mice. J Toxicol Environ Health. 1986;18(1):49–60. doi: 10.1080/15287398609530847. [DOI] [PubMed] [Google Scholar]
- Jensen S., Jernelöv A. Biological methylation of mercury in aquatic organisms. Nature. 1969 Aug 16;223(5207):753–754. doi: 10.1038/223753a0. [DOI] [PubMed] [Google Scholar]
- Kerper L. E., Ballatori N., Clarkson T. W. Methylmercury transport across the blood-brain barrier by an amino acid carrier. Am J Physiol. 1992 May;262(5 Pt 2):R761–R765. doi: 10.1152/ajpregu.1992.262.5.R761. [DOI] [PubMed] [Google Scholar]
- Kershaw T. G., Clarkson T. W., Dhahir P. H. The relationship between blood levels and dose of methylmercury in man. Arch Environ Health. 1980 Jan-Feb;35(1):28–36. doi: 10.1080/00039896.1980.10667458. [DOI] [PubMed] [Google Scholar]
- Kostyniak P. J., Clarkson T. W., Abbasi A. H. An extracorporeal complexing hemodialysis system for the treatment of methylmercury poisoning. II. In vivo applications in the dog. J Pharmacol Exp Ther. 1977 Nov;203(2):253–263. [PubMed] [Google Scholar]
- Kostyniak P. J., Clarkson T. W., Cestero R. V., Freeman R. B., Abbasi A. H. An extracorporeal complexing hemodialysis system for the treatment of methylmercury poisoning. I. In vitro studies of the effects of four complexing agents on the distribution and dialyzability of methylmercury in human blood. J Pharmacol Exp Ther. 1975 Feb;192(2):260–269. [PubMed] [Google Scholar]
- Kostyniak P. J. Mobilization and removal of methylmercury in the dog during extracorporeal complexing hemodialysis with 2,3-dimercaptosuccinic acid (DMSA). J Pharmacol Exp Ther. 1982 Apr;221(1):63–68. [PubMed] [Google Scholar]
- Landrigan P. J., Goyer R. A., Clarkson T. W., Sandler D. P., Smith J. H., Thun M. J., Wedeen R. P. The work-relatedness of renal disease. Arch Environ Health. 1984 May-Jun;39(3):225–230. doi: 10.1080/00039896.1984.9939529. [DOI] [PubMed] [Google Scholar]
- Landry T. D., Doherty R. A., Gates A. H. Effects of three diets on mercury excretion after methylmercury administration. Bull Environ Contam Toxicol. 1979 May;22(1-2):151–158. doi: 10.1007/BF02026922. [DOI] [PubMed] [Google Scholar]
- Lok E. The effect of weaning on blood, hair, fecal and urinary mercury after chronic ingestion of methylmercuric chloride by infant monkeys. Toxicol Lett. 1983 Feb;15(2-3):147–152. doi: 10.1016/0378-4274(83)90208-4. [DOI] [PubMed] [Google Scholar]
- Magos L., Clarkson T. W., Allen J., Snowden R. The effects of bromosulphophthalein, indocyanine green and bilirubin on the biliary excretion of methylmercury. Chem Biol Interact. 1979 Aug;26(3):317–320. doi: 10.1016/0009-2797(79)90034-6. [DOI] [PubMed] [Google Scholar]
- Magos L., Peristianis G. C., Snowden R. T. Postexposure preventive treatment of methylmercury intoxication in rats with dimercaptosuccinic acid. Toxicol Appl Pharmacol. 1978 Aug;45(2):463–475. doi: 10.1016/0041-008x(78)90109-6. [DOI] [PubMed] [Google Scholar]
- Magos L. The effects of dimercaptosuccinic acid on the excretion and distribution of mercury in rats and mice treated with mercuric chloride and methylmercury chloride. Br J Pharmacol. 1976 Apr;56(4):479–484. doi: 10.1111/j.1476-5381.1976.tb07460.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marsh D. O., Clarkson T. W., Cox C., Myers G. J., Amin-Zaki L., Al-Tikriti S. Fetal methylmercury poisoning. Relationship between concentration in single strands of maternal hair and child effects. Arch Neurol. 1987 Oct;44(10):1017–1022. doi: 10.1001/archneur.1987.00520220023010. [DOI] [PubMed] [Google Scholar]
- Marsh D. O., Myers G. J., Clarkson T. W., Amin-Zaki L., Tikriti S., Majeed M. A. Fetal methylmercury poisoning: clinical and toxicological data on 29 cases. Ann Neurol. 1980 Apr;7(4):348–353. doi: 10.1002/ana.410070412. [DOI] [PubMed] [Google Scholar]
- McKeown-Eyssen G. E., Ruedy J., Neims A. Methyl mercury exposure in northern Quebec. II. Neurologic findings in children. Am J Epidemiol. 1983 Oct;118(4):470–479. doi: 10.1093/oxfordjournals.aje.a113652. [DOI] [PubMed] [Google Scholar]
- Norseth T., Clarkson T. W. Intestinal transport of 203Hg-labeled methyl mercury chloride. Role of biotransformation in rats. Arch Environ Health. 1971 May;22(5):568–577. doi: 10.1080/00039896.1971.10665903. [DOI] [PubMed] [Google Scholar]
- Phelps R. W., Clarkson T. W., Kershaw T. G., Wheatley B. Interrelationships of blood and hair mercury concentrations in a North American population exposed to methylmercury. Arch Environ Health. 1980 May-Jun;35(3):161–168. doi: 10.1080/00039896.1980.10667486. [DOI] [PubMed] [Google Scholar]
- Refsvik T., Norseth T. Methyl mercuric compounds in rat bile. Acta Pharmacol Toxicol (Copenh) 1975 Jan;36(1):67–78. doi: 10.1111/j.1600-0773.1975.tb00772.x. [DOI] [PubMed] [Google Scholar]
- Rowland I. R., Robinson R. D., Doherty R. A. Effects of diet on mercury metabolism and excretion in mice given methylmercury: role of gut flora. Arch Environ Health. 1984 Nov-Dec;39(6):401–408. doi: 10.1080/00039896.1984.10545872. [DOI] [PubMed] [Google Scholar]
- Sager P. R., Aschner M., Rodier P. M. Persistent, differential alterations in developing cerebellar cortex of male and female mice after methylmercury exposure. Brain Res. 1984 Jan;314(1):1–11. doi: 10.1016/0165-3806(84)90170-6. [DOI] [PubMed] [Google Scholar]
- Spry D. J., Wiener J. G. Metal bioavailability and toxicity to fish in low-alkalinity lakes: A critical review. Environ Pollut. 1991;71(2-4):243–304. doi: 10.1016/0269-7491(91)90034-t. [DOI] [PubMed] [Google Scholar]
- Takahashi H., Hirayama K. Accelerated elimination of methyl mercury from animals. Nature. 1971 Jul 16;232(5307):201–202. doi: 10.1038/232201a0. [DOI] [PubMed] [Google Scholar]
- Thomas D. J., Fisher H. L., Sumler M. R., Marcus A. H., Mushak P., Hall L. L. Sexual differences in the distribution and retention of organic and inorganic mercury in methyl mercury-treated rats. Environ Res. 1986 Oct;41(1):219–234. doi: 10.1016/s0013-9351(86)80184-0. [DOI] [PubMed] [Google Scholar]
- Thomas D. J., Smith J. C. Effects of coadministered low-molecular-weight thiol compounds on short-term distribution of methyl mercury in the rat. Toxicol Appl Pharmacol. 1982 Jan;62(1):104–110. doi: 10.1016/0041-008x(82)90106-5. [DOI] [PubMed] [Google Scholar]
- Turner M. D., Marsh D. O., Smith J. C., Inglis J. B., Clarkson T. W., Rubio C. E., Chiriboga J., Chiriboga C. C. Methylmercury in populations eating large quantities of marine fish. Arch Environ Health. 1980 Nov-Dec;35(6):367–378. doi: 10.1080/00039896.1980.10667521. [DOI] [PubMed] [Google Scholar]
- Wood J. M., Kennedy F. S., Rosen C. G. Synthesis of methyl-mercury compounds by extracts of a methanogenic bacterium. Nature. 1968 Oct 12;220(5163):173–174. doi: 10.1038/220173a0. [DOI] [PubMed] [Google Scholar]
- Yoshino Y., Mozai T., Nakao K. Biochemical changes in the brain in rats poisoned with an alkymercury compound, with special reference to the inhibition of protein synthesis in brain cortex slices. J Neurochem. 1966 Nov;13(11):1223–1230. doi: 10.1111/j.1471-4159.1966.tb04281.x. [DOI] [PubMed] [Google Scholar]


