Abstract
Background
Benzodiazepine use by elderly patients is associated with adverse outcomes including increased risk of falls and fractures, motor vehicle accidents and cognitive impairment. Recent studies suggest that individualized feedback and education to physicians may improve drug prescribing. In this study, we evaluated an intervention to address the inappropriate prescribing of benzodiazepines for elderly patients.
Methods
We identified 1624 primary care physicians who wrote at least 10 prescriptions for the target drugs in a 2-month period and randomly assigned these physicians to the intervention group or the control group. We obtained data from the Ontario Drug Benefit claims database, which covers all Ontario residents aged 65 years and over for drugs selected from a minimally restrictive formulary. Every 2 months for 6 months, confidential profiles of benzodiazepine prescription use coupled with evidence-based educational bulletins were mailed to the intervention group. The control group received feedback and educational bulletins about first-line antihypertension drug prescribing for elderly patients. Our main outcome measures were reductions in the proportion of each physician's total benzodiazepine prescriptions for long-acting agents, combinations of benzodiazepines with other psychoactive medications (including other benzodiazepines) and long-term benzodiazepine therapy.
Results
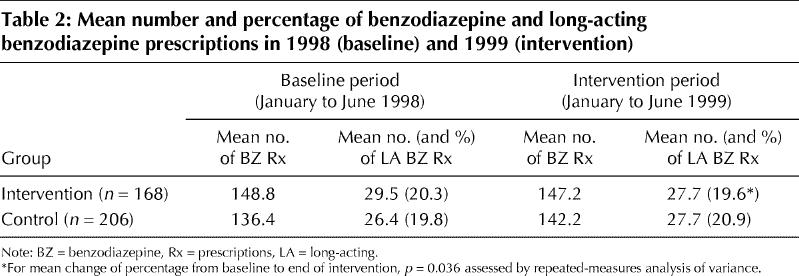
After randomization, 168 physicians agreed to be in the intervention group and 206 in the control group. Their demographic and prescribing characteristics were similar. Although the proportion of long-acting benzodiazepine prescriptions decreased by 0.7% in the intervention group between the baseline period and the end of the intervention period (from 20.3%, or a mean of 29.5 prescriptions, to 19.6%, or a mean of 27.7 prescriptions) and increased by 1.1% in the control group (from 19.8%, or a mean of 26.4 prescriptions, to 20.9%, or a mean of 27.7 prescriptions) (p = 0.036), this difference was not clinically significant. There was no significant difference over the study period in either combination prescribing of benzodiazepines or in prescriptions for long-term benzodiazepine therapy.
Interpretation
We did not find that a program of confidential feedback and educational material offered to Ontario primary care physicians had a clinically significant impact on their benzodiazepine prescribing.
Benzodiazepines are widely prescribed for people over the age of 65 years. Their use has been associated with a number of adverse outcomes including cognitive impairment,1 an increased risk of falls and hip fractures, especially in people with coexisting medical illness,2,3 and motor vehicle accidents.4 The risks are greater with long-acting agents and during the first few weeks after drug initiation. In spite of the risks, there is evidence that benzodiazepines may be overprescribed to elderly people.5,6 Among the problems identified are the overprescription of long-acting benzodiazepines, high rates of benzodiazepine use in combination with other psychoactive drugs and the prescribing of benzodiazepines for long-term use.5,6
There are currently no accepted clinical practice guidelines for the safe and effective use of benzodiazepines, but these drugs are useful in treating insomnia, anxiety symptoms and alcohol withdrawal. Manufacturers recommend short-term use only (< 3 weeks). A recent meta-analysis suggests that short-acting benzodiazepines may be effective for the short-term treatment of situational insomnia;7 however, cognitive behavioural therapy is as effective for the treatment of insomnia in elderly people as benzodiazepines and is more durable in its effects.8
Hux and colleagues demonstrated that a simple mailed educational intervention combined with individualized feedback was an effective way to improve antibiotic prescribing.9 We wished to evaluate whether a similar program could be used to improve the prescribing of benzodiazepine hypnotic sedatives to elderly people. We hypothesized that the feedback and education intervention would lead to reductions in the prescribing of long-acting benzodiazepines, long-term benzodiazepine prescriptions and potentially harmful combinations of benzodiazepines with other psychoactive drugs.
Methods
We obtained the names, addresses and prescriber identification numbers of 2800 primary care physicians and attempted to link these with the Ontario Drug Benefit database. We successfully linked the names and prescriber numbers of 2520 physicians. To reduce the chance of contamination between the study arms or reinforcement of the intervention through participant interaction, we did not select physicians with the same address as another participant. Baseline prescribing patterns were screened to ensure that potential participants wrote at least 10 prescriptions for the target drugs in a 2-month period. Of the remaining 1624 eligible physicians, 812 were randomly assigned to the intervention group and 812 to the control group. Randomization was carried out before consent, following Zelen's method,10 because it was important that control physicians did not know that their prescribing patterns were being compared with those of the physicians in the intervention group (Fig. 1).11 The control group received a similar feedback and education program about prescribing first-line antihypertensive drugs.
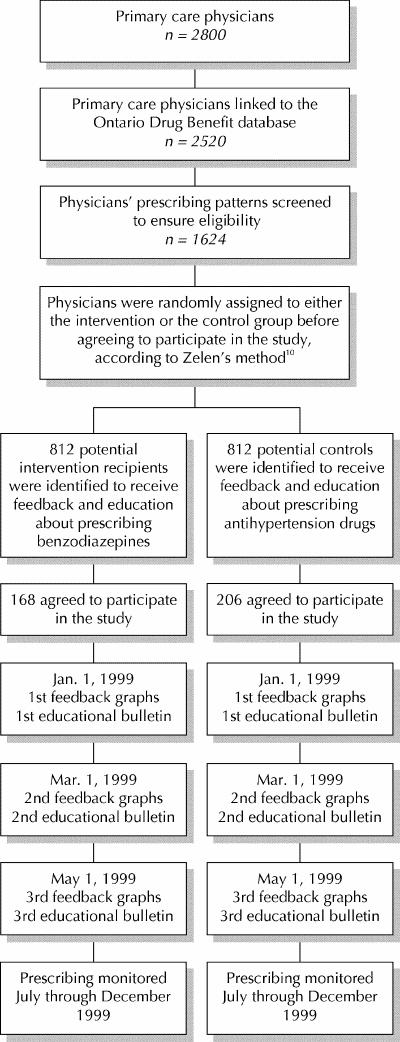
Fig. 1: Study outline.
Physicians who were randomly assigned to the intervention were invited to consent to a program of feedback about their prescribing and education about benzodiazepine prescribing for elderly people. The physicians were assured that a strict confidentiality protocol was in place whereby no one on the project staff would have access to both their name and their profile, nor would their profiles be made available to the Ontario Ministry of Health and Long-Term Care or any outside agency. It was made clear to study participants that no judgement was being made about the appropriateness of the individual prescriptions, because the claims data did not include sufficient clinical information to make such an evaluation. Initial invitations to participate were followed by 2 reminders to nonresponders at 2-week intervals. Eight packages were returned as undeliverable. Responses were received from 355 of the 804 who received packages, of whom 168 wished to participate, giving an overall consent rate of 21%.
Because physicians who consent to educational interventions may have practices that differ systematically from those who do not give their consent, we also identified a control group of individuals who agreed to participate in the study. Participants in the control arm of the study agreed to receive educational material and feedback about their antihypertensive prescribing for elderly patients. Three packages were returned as undeliverable. Responses were received from 381 of the 809 physicians who received packages, of whom 206 wished to participate, giving an overall consent rate of 25%.
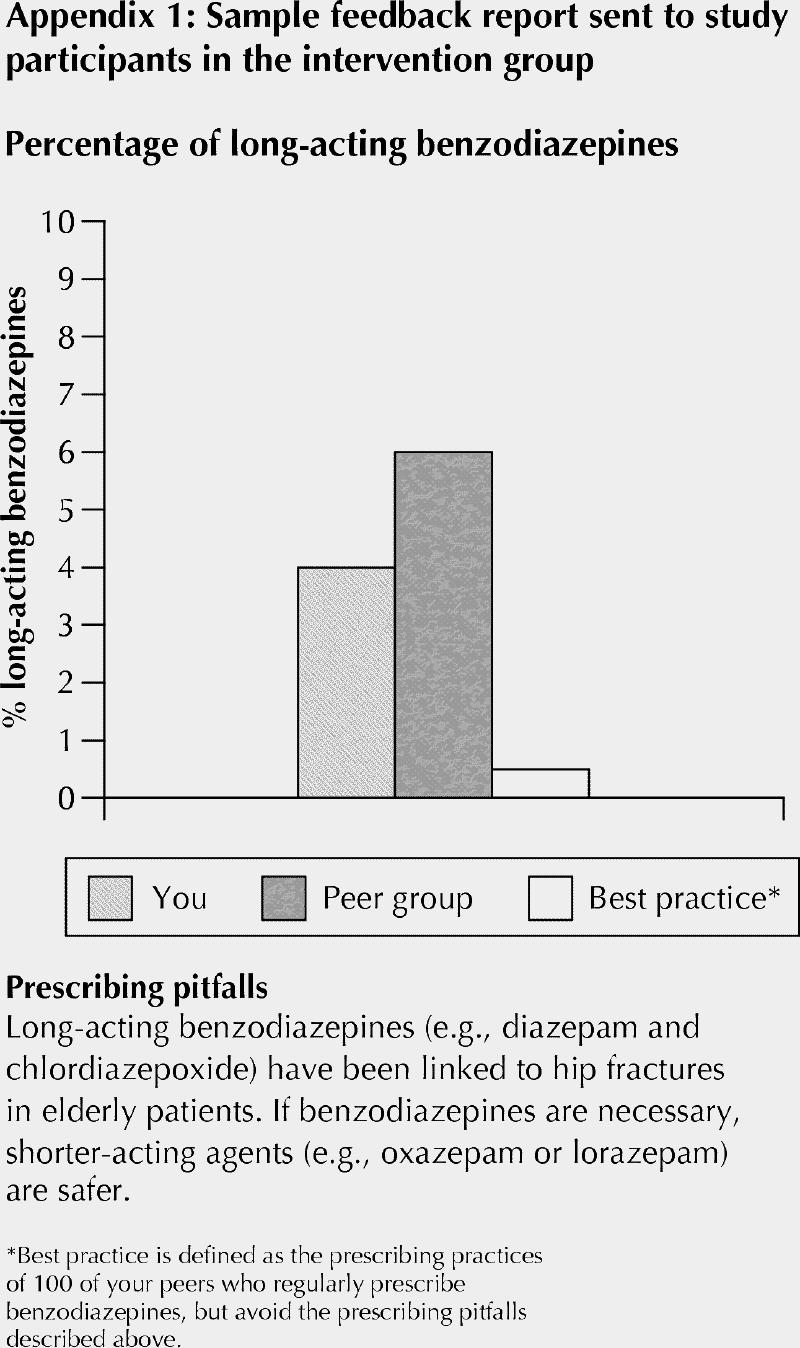
The intervention consisted of mailed packages of feedback about the participants' prescribing and evidence-based educational materials, which were sent every 2 months for 6 months. The initial feedback report, mailed Jan. 1, 1999, gave baseline data for January and February 1998. Feedback pertaining to baseline data for March and April 1998 was mailed on Mar. 1, 1999, and feedback pertaining to baseline data for May and June 1998 was mailed on May 1, 1999. Feedback was presented as bar graphs comparing the prescriber with his or her peers and with a hypothetical “best practice” in 4 categories: (1) number of prescriptions per 100 seniors, (2) percentage of long-acting benzodiazepines prescribed, (3) duration of therapy (% of prescriptions for longer than 3 months) and (4) combination therapy (% of benzodiazepine and psychoactive drug combinations). The “best practice” was defined as the benzodiazepine-prescribing patterns of 100 physicians who regularly prescribed benzodiazepines but avoided the pitfalls of using long-acting drugs, combinations of drugs and long-term therapy. This was included in the graphs in order to counteract the potential social desirability effect of the peer group comparison. A sample feedback report is shown in Appendix 1 (an expanded version of Appendix 1 may be found on www.cmaj.ca).
The educational bulletins that accompanied the feedback profiles were written in a brief, informal style with an emphasis on practical tips. In addition, we included information sheets that physicians could give to patients. These were relatively simply designed in order to distinguish them from commercial promotional materials. Topics and content were selected on the basis of focus group work with 3 groups of primary care physicians, regarding challenges in the safe and effective prescribing of benzodiazepines for elderly patients.
We prepared the feedback profiles from claims data for prescriptions under the Ontario Drug Benefit program. Available data fields included date of filling of the prescription, drug identification number, quantity, professional fee, charges claimed from the Ontario Drug Benefit program, and scrambled patient and physician identification numbers whereby the drug history of an individual patient or prescriber could be assembled but could not be linked to that person's identity. For the study physicians, we extracted claims for all benzodiazepines from the dataset.
We evaluated participants' satisfaction with the intervention through a mailed survey to the 168 participants in the intervention group.
The intervention was offered from Jan. 1, 1999, to June 30, 1999, and January through June 1998 was chosen to be the baseline period. The “washout” (post-intervention monitoring period) was from July 1, 1999, to Dec. 31, 1999.
We calculated the percentage of long-acting benzodiazepine prescriptions as a proportion of all benzodiazepine prescriptions for each physician. We defined the following as long-acting drugs: chlordiazepoxide, clonazepam, clorazepate, diazepam, nitrazepam and flurazepam. Alprazolam, bromazepam, lorazepam, oxazepam, triazolam and temazepam were defined as short-acting drugs. To obtain the percentage of seniors on long-term therapy, we divided the number of patients who were prescribed long-term benzodiazepine therapy by the number of all seniors receiving benzodiazepine prescriptions from each physician. Long-term therapy was defined as benzodiazepine therapy lasting 60 days or more. We used the recommended daily dose to calculate the duration of each prescription, which had to be from the same physician who was participating in our study. We calculated the percentage of benzodiazepine prescriptions considered to be combination therapy as a proportion of the total number of benzodiazepine prescriptions. Combination therapy was identified where 1 or more psychoactive drugs from a pre-defined list were prescribed concurrently with a benzodiazepine. The drugs had to be prescribed by the same physician who was participating in our study, and the dispensing date of the benzodiazepine prescription minus the dispensing date of the other prescription had to equal 7 days or less.
Ethics approval for the study was received from the Research Ethics Board at Women's College and at the University of Toronto, Toronto, Ont.
Results
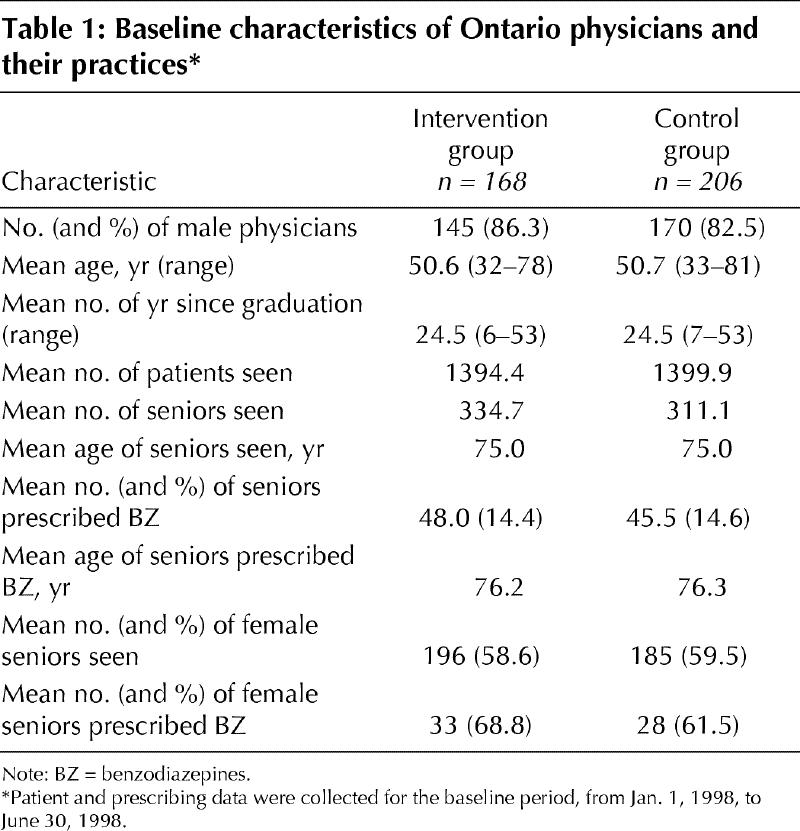
Physicians in the intervention and control arms of the study were similar with respect to age and years since graduation. There was a slightly higher proportion of female physicians in the control group (Table 1). There were no significant differences in baseline benzodiazepine prescribing patterns between the 2 groups.
Table 1
There appeared to be a small reduction in the percentage of long-acting benzodiazepines prescribed by the physicians in the intervention group (Table 2). During the intervention period there was no significant difference in the intervention effect among the 3 mailings, but the mean change in percentage from baseline to the end of the intervention period was significantly different for the intervention and control groups (p = 0.036). The intervention had no significant impact on the percentage of seniors who received long-term benzodiazepine therapy or the percentage who were prescribed benzodiazepines in combination with other psychoactive medications.
Table 2
After a single mailing to all 168 participants in the intervention group at the conclusion of the study, 81 completed questionnaires were returned, providing a response rate of 48%. A total of 70% of the respondents indicated that they would readily participate in another similar program.
Interpretation
We found that an intervention that had reasonable success in changing antibiotic prescribing patterns was unsuccessful when applied to benzodiazepine prescribing. We attempted to improve benzodiazepine prescribing for elderly patients using a simple, inexpensive combination of confidential feedback about prescribing and targeted educational materials.
There may be several reasons why this intervention did not have a significant effect on benzodiazepine prescribing. First, it may be easier to change physician prescribing of a “one-time-only” drug such as an antibiotic than of drugs such as benzodiazepines that are commonly prescribed as chronic therapy. Most of the physicians in the focus groups that were conducted to develop the educational materials commented that seniors in their practices who were taking long-acting drugs had taken them for “years” and that both they and their patients were reluctant to discontinue them because there was no perception of harm. Second, there is greater public awareness now of the need to reduce unnecessary antibiotic prescribing than of the known risks of benzodiazepine use. Third, the physicians who consented to participate in this study may be the “best” prescribers and may have optimized their practices, leaving little room for further improvement. Fourth, there may be greater diagnostic uncertainty when it comes to prescribing benzodiazepines rather than antibiotics. It is sometimes difficult, especially with elderly patients, to distinguish between anxiety symptoms and those of depression. The lack of diagnostic data on the prescription claims in our study made it impossible to evaluate the appropriateness of an individual prescription. Finally, in Ontario there are clear evidence-based guidelines for first-line antibiotic prescribing that have been distributed to all primary care physicians by the Ministry of Health and Long-Term Care. Similar guidelines do not exist for benzodiazepines.
Effective interventions to change prescribing behaviour have included features such as local participation in guideline development, clearly defined behavioural goals, multifaceted programs that enable and reinforce appropriate prescribing, and personal contact with the prescriber.12 In future it may be necessary to use such interventions in order to have a greater impact on benzodiazepine prescribing by primary care physicians.
Supplementary Material
Acknowledgments
We gratefully acknowledge the substantial assistance of Ms. Maria Candida Ferreira, Mr. Steve Slade and Ms. Sandy Cummings (Department of Family and Community Medicine) and Ms. Elaine Gort (Institute for Clinical Evaluative Sciences) in the completion of this study.
Appendix 1.
Footnotes
This article has been peer reviewed.
Contributors: Dr. Pimlott was the lead investigator in the study and was involved in all aspects. He contributed to the conception, design and execution of the study and wrote the initial draft and subsequent revisions of the manuscript. Dr. Hux contributed to the conception, design and execution of the study. Drs. Wilson, Kahan and Rosser contributed to the study conception and design and to the development of the educational materials used in the study. Ms. Li conducted the data analysis with input from Drs. Pimlott and Hux. All authors critically reviewed all drafts of the manuscript.
We also gratefully acknowledge the funding of this research project by the physicians of the province of Ontario through the Physicians' Services Incorporated Foundation (PSI grant no. 9742). Dr. Pimlott is a funded Research Scholar in the Department of Family and Community Medicine, Faculty of Medicine, University of Toronto.
Dr. Hux is a Career Scientist of the Ontario Ministry of Health and receives salary support from the Institute for Clinical Evaluative Sciences in Ontario. The opinions, results and conclusions here are those of the authors, and no endorsement by the Ministry of Health or the Institute for Clinical Evaluative Sciences is intended or should be inferred.
Competing interests: None declared.
Correspondence to: Dr. Nicholas J. G. Pimlott, Research Office, Department of Family and Community Medicine, Women's College Campus, Sunnybrook and Women's College Health Sciences Centre, Burton Hall, 60 Grosvenor St., Toronto ON M5S 1B6; fax 416 323-6351; nick.pimlott@utoronto.ca
References
- 1.Rummans TA, Davis Jr. LJ, Morse RM, Ivnik RJ. Learning and memory impairment in older, detoxified benzodiazepine-dependent patients. Mayo Clin Proc 1993;68:731-7. [DOI] [PubMed]
- 2.Ray WA, Griffin MR, Downey W. Benzodiazepines of long and short elimination half-life and the risk of hip fracture. JAMA 1989;262:3303-7. [PubMed]
- 3.Cummings SR, Nevitt MC, Browner WS, Stone K, Fox KM, Ensrud KE, et al. Risk factors for hip fracture in white women. Study of Osteoporotic Fractures Research Group. N Engl J Med 1995;332(12):767-73. [DOI] [PubMed]
- 4.Barbone F, McMahon AD, Davey PG, Morris AD, Reid IC, McDevitt DG, et al. Association of road traffic accidents with benzodiazepine use. Lancet 1998;352:1331-6. [DOI] [PubMed]
- 5.Tamblyn RM, McLeod PJ, Abrahamowicz M, Monette J, Gayton DC, Berkson L, et al. Questionable prescribing for elderly patients in Quebec. CMAJ 1994;150(11):1801-9. [PMC free article] [PubMed]
- 6.McLeod PJ, Huang AR, Tamblyn RM, Gayton, DC. Defining inappropriate prescribing practices for elderly people: a national consensus panel. CMAJ 1997;156(3):385-91. [PMC free article] [PubMed]
- 7.Holbrook AM, Crowther R, Lotter A, Cheng C, King D. Meta-analysis of benzodiazepine use in the treatment of insomnia. CMAJ 2000;162(2):225-33. [PMC free article] [PubMed]
- 8.Morin CM, Colecchi C, Stone J, Sood R, Brink D. Behavioral and pharmacological therapies for late life insomnia. A randomized controlled trial. JAMA 1999;281:991-9. [DOI] [PubMed]
- 9.Hux JE, Melady MP, DeBoer D. Confidential prescriber feedback and education to improve antibiotic use in primary care: a controlled trial. CMAJ 1999; 161(4):388-92. [PMC free article] [PubMed]
- 10.Torgerson DJ, Roland M. What is Zelen's design? BMJ 1998;316:606-8. [DOI] [PMC free article] [PubMed]
- 11.Hart CWM. The Hawthorne experiments. Can J Econ Pol Sci 1942;9:150-63.
- 12.Oxman AD, Thomson MA, Davis DA, Haynes RB. No magic bullets: a systematic review of 102 trials of interventions to improve professional practice. CMAJ 1995;153(10):1423-31. [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


