Case
A 40-year-old woman comes to the family practice clinic for a routine annual visit. She reports a 6-month history of progressively severe episodic shortness of breath, cough, wheeze and chest tightness. You question her about associated symptoms, the timing and frequency of the symptoms, and triggering or exacerbating factors. You ask about environmental exposures in the home and workplace and any temporal associations of the symptoms with such exposures, including any change in severity of symptoms on weekends or holidays, as is your routine for patients with new-onset or worsening asthma. She reports that symptoms typically worsen in the evenings and that they cleared while she was at home over the Christmas holidays. You note from your records that at the time of her previous visit she was working at an electronics factory, and you question her more closely about possible exposures to chemicals at work, but she is unsure what compounds are used. The results of a physical examination are normal.
Asthma is a common condition, often starting or recurring in adult life. For example, in a recent survey about 4% to 6% of men and 5% to 10% of women 20 to 44 years of age in 6 Canadian cities reported current use of asthma medication.1 Occupational asthma from various causes is being diagnosed with increasing frequency. This article reviews the classification, diagnosis, investigation and management of occupational asthma.
Classification of work-related asthma
Aggravation of pre-existing or coincidental asthma
Workplace exposures to potential irritants, such as cold, dry air, dusts, smoke, fumes and sprays, or exertion at work may aggravate asthma, especially in patients with moderate or severe forms of the disease and in those not receiving optimal treatment. Such aggravation of pre-existing disease is different from occupational asthma (i.e., asthma caused by some aspect of the workplace). Optimization of asthma management and, if needed, reduction of workplace exposures to respiratory irritants often allow patients with this type of work-related asthma to continue in the same job.
Occupational asthma
Occupational asthma is asthma caused by some aspect of the workplace environment.2 It is important to distinguish occupational asthma from aggravation of pre-existing asthma, because the management and compensation can differ. The more common type of occupational asthma, accounting for over 90% of cases, is sensitizer-induced occupational asthma, caused by an IgE-mediated or other immune response to specific workplace agents: high- molecular-weight sensitizers (such as animal proteins, flour or natural rubber latex) and low-molecular-weight chemicals (such as diisocyanates, colophony [a pine resin product] or epoxy compounds). Once a person has been sensitized to one of these materials, even exposure to extremely low quantities will exacerbate the asthma. The less common form of occupational asthma, accounting for about 7% of cases, is irritant-induced occupational asthma, which occurs after accidental exposure to very high inhaled concentrations of a workplace irritant. Given that both forms account for only a small proportion of all cases of adult asthma (about 10%)3 and can be caused by numerous workplace agents,4 the diagnosis of occupational asthma can easily be overlooked in primary care practice unless it is routinely considered in the assessment of new-onset asthma in a working adult.
Irritant-induced occupational asthma should be suspected if the symptoms first began within 24 hours after accidental exposure to a high inhaled concentration of a workplace irritant, whereas sensitizer-induced occupational asthma should be suspected if the symptoms begin during a period when the patient is working, are worse at work or in the evenings after work, and diminish during weekends or holidays. If any of these situations apply, further investigations are needed.
Diagnosis of occupational asthma
Irritant-induced occupational asthma
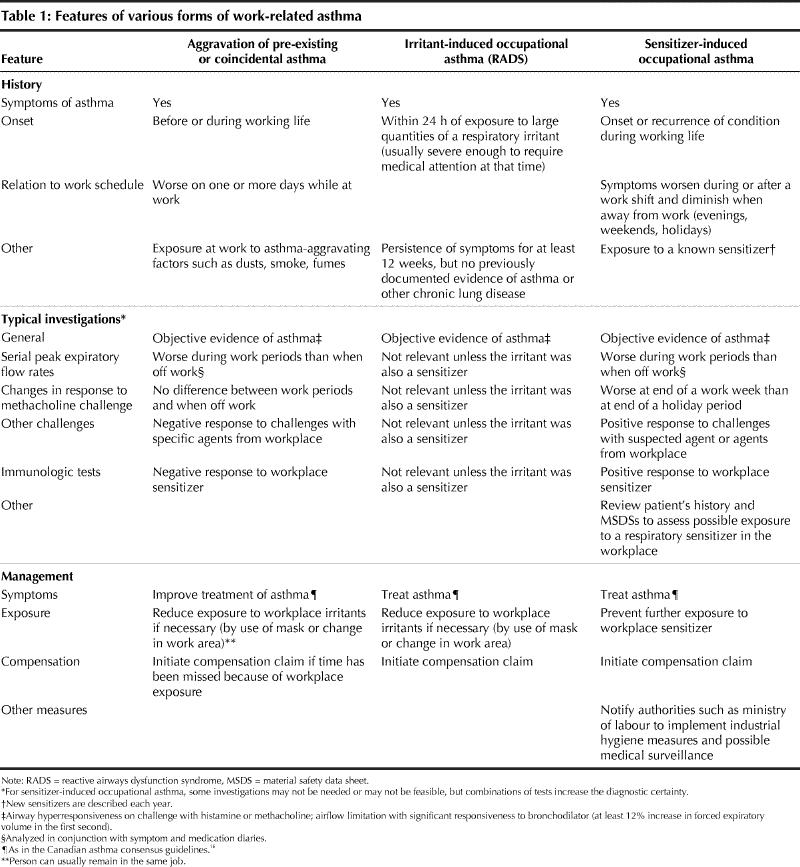
The most definitive form of irritant-induced asthma5 is reactive airways dysfunction syndrome.6 The diagnostic criteria for reactive airways dysfunction syndrome are shown in Table 1. Patients with this or the less strictly defined forms of irritant-induced asthma5,6 may be entitled to provincial workers' compensation for asthma caused by the workplace. Furthermore, modification of the work environment may be required to reduce exposure to aggravating irritants and to reduce the risk of future accidental exposures affecting the same worker or others.
Table 1
Sensitizer-induced occupational asthma
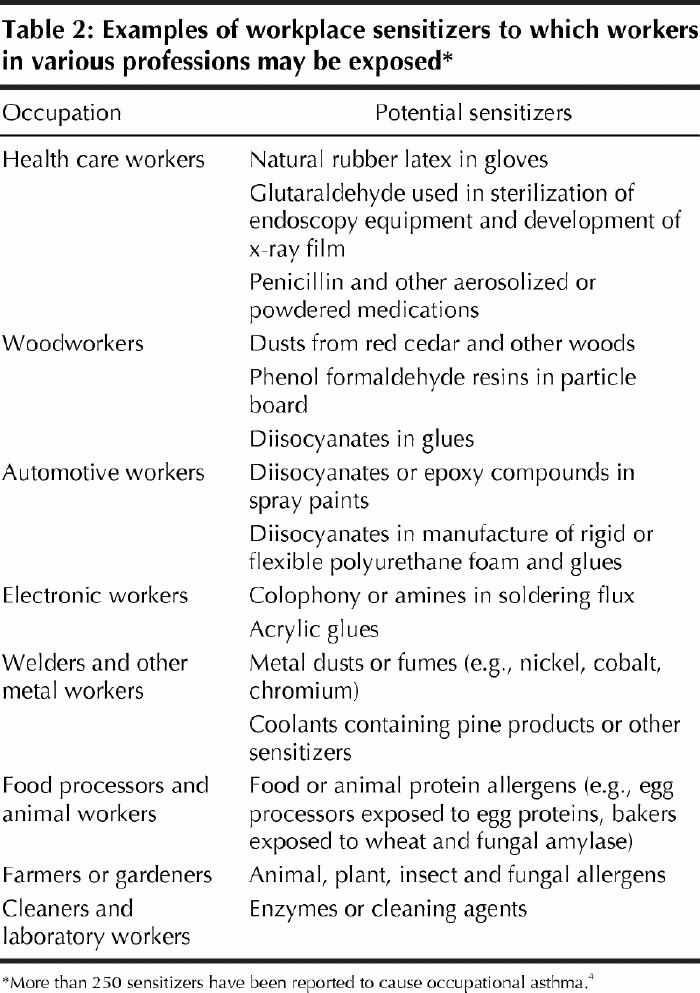
Some examples of the more than 250 agents that can cause sensitizer-induced occupational asthma are listed in Table 2. If this form of occupational asthma is suspected from the patient's history, objective investigation is required to confirm or refute the diagnosis,7,8 since the implications for the patient's work situation differ for this and other forms of work-related asthma. Patients with confirmed sensitizer-induced occupational asthma should have no further exposure to the causative agent, since the best outcome is achieved with early diagnosis and complete avoidance of exposure.9 These measures will probably result in economic loss, even if a compensation claim is accepted, so an objectively confirmed diagnosis is very important.
Table 2
Approximately 96% of people with sensitizer-induced occupational asthma have a history consistent with this diagnosis. However, the specificity of history is poor, and only 25% of those with an appropriate history actually have sensitizer-induced occupational asthma.10 Thus, a negative history is more reliable in excluding a diagnosis than a positive history is in confirming it. The wide differential diagnosis for patients with a history suspicious for sensitizer- induced occupational asthma includes asthma coincidental to the workplace, unrelated asthma that is aggravated by exposure to nonspecific irritants at work and nonasthmatic causes of asthma-like symptoms (such as rhinitis with postnasal drip, acute or chronic bronchitis, gastroesophageal reflux or cardiac asthma).
The steps in diagnosing sensitizer-induced occupational asthma are presented in Table 1. Patients with suspected sensitizer-induced occupational asthma should be referred as soon as possible to a specialist (a respirologist, an allergist or an occupational physician) with expertise in this area. However, the investigations (as outlined in Table 1) are most helpful if they can be performed while the patient is still working in the suspected causative work area; the primary care physician may be able to initiate some of these.
Assessments and investigations
Confirm asthma
The initial diagnostic step is to objectively confirm or refute the diagnosis of asthma by means of pulmonary function tests before and after administration of a bronchodilator, with or without a histamine or methacholine challenge test, according to a standard protocol.11 These investigations should be arranged while the patient is still employed and should take place within 24 hours of the patient's usual work exposure. Normal results at that time, especially a normal response to methacholine challenge, virtually exclude a diagnosis of occupational asthma (although a few patients with diisocyanate-induced asthma but normal results on methacholine challenge have been described).12
Assess exposure
Affected patients may not be aware of the chemicals to which they are exposed at work. Additional information can be obtained from the workplace in the form of material safety data sheets (MSDSs). Employers are required to have an MSDS available on site for any hazardous material that accounts for 1% or more of any workplace substance. The specialist should review the MSDSs for all agents to which the patient may have airborne exposure, including those used by coworkers. Further details on chemicals not listed on the sheets can be requested by phoning the contact number given on the MSDS (usually the manufacturer of the hazardous material).
Assess relation between asthma and the workplace
Several studies,7,8 including guidelines from the Canadian Thoracic Society,8 have assessed the value of investigations for occupational asthma. Each investigative measure (Table 1) can have false-positive and false-negative outcomes. It is therefore important for the physician interpreting the test results to be aware of confounding factors8 and to undertake as many investigations as are feasible for an individual patient. Such comprehensive testing and interpretation usually requires referral to a specialist.
Serial monitoring of peak expiratory flow and paired methacholine challenges
Peak expiratory flow meters are inexpensive and can be given to the patient in a primary care setting. The patient records peak expiratory flow rate (PEFR) 4 times a day and completes symptom and medication diaries during periods of regular work and periods off work (e.g., weekends and holidays).13 The flow meters are useful as a component of an occupational asthma investigation, but patients must be instructed as to correct use. If possible, medications (other than as-needed bronchodilators) are kept at stable, regular dosages during this period, sufficient to control but not completely suppress symptoms. Compliance in completing the symptom, medication and PEFR diaries is often poor. However, in cases where the patient has kept records with enough information to assess the relation between symptoms and work schedule over several weeks of work and over a holiday period, the sensitivity and specificity of serial PEFRs has been higher (at 73% and 100% respectively) than for other, more objective tests.14 Nonetheless, differences in symptoms and PEFR readings between periods at work and periods off work may not be sufficient to distinguish aggravation of asthma from occupational asthma. Performing methacholine challenges at the end of a work week and again at the end of a holiday period can provide additional helpful information. A threefold or greater decline in methacholine reactivity (i.e., an increase in PC20, the provocation concentration of methacholine causing a 20% drop in forced expiratory volume in the first second) after a period away from work is strongly supportive of occupational asthma, rather than aggravation of asthma; however, lack of a change of this magnitude does not exclude occupational asthma, since hyperresponsiveness may persist for several months or years.
Immunological tests
A positive skin prick response to an agent from the workplace supports a diagnosis of occupational asthma if it is associated with appropriate pulmonary function changes, but is not diagnostic as a sole investigation. Immunological tests (skin tests or in vitro assays for specific IgE antibodies15) are often limited by the lack of commercially available or standardized reagents.
If the patient has left the implicated workplace and cannot or will not return on a trial basis for the workplace- related peak flow and methacholine testing, an objective physiological diagnosis may require challenges with specific agents in a specialized facility (usually an academic centre specializing in occupational lung disease).
Management
Aggravation of pre-existing asthma
For patients with aggravation of pre-existing asthma, the best approach is to optimize medical management of the asthma, by limiting exposure to relevant environmental allergens and nonoccupational irritants such as tobacco smoke and by prescribing appropriate medications and providing suitable education to ensure that the patient understands how to use the drugs and the importance of compliance.16 The patient can usually stay in the same job, but it may be necessary to reduce exposure to nonspecific workplace triggers,8 for example by moving to a different work area, making changes in the ventilation system or in work processes, or using an appropriate respirator for short-term exposures to irritants, as advised by an occupational hygienist familiar with the exposures.17 If the asthma is severe, then a change in occupation to a relatively sedentary job in a clean environment may be needed to enable the patient to continue work.
Irritant-induced occupational asthma
Workers with occupational asthma induced by exposure to an irritant at work should be managed in the same way as those with aggravation of pre-existing asthma, with the addition of appropriate precautions8 (e.g., health and safety education, better workplace containment of respiratory irritants, improved ventilation and use of respiratory protection as necessary17) to ensure that there is no risk of further exposure to high inhaled concentrations of the irritant (Table 1).
Sensitizer-induced occupational asthma
For a patient with occupational asthma induced by a respiratory sensitizer, a workers' compensation claim should be pursued, if applicable. Once the decision on the claim has been made, steps should be taken to prevent further exposure to the agent,8 and the worker should receive the same types of medical treatment as people with nonoccupational asthma (Table 1). In addition, the provincial ministry of labour or a workplace physician (or both) should be notified as to the possible risk of occupational asthma in other workers because of continuing exposure to the causative agent.
Case revisited
This patient's work consisted of soldering electronic parts for a small company. Her symptoms worsened in the evenings on workdays and diminished on weekends and holidays. MSDSs from the workplace indicated that the soldering flux used at the site contained colophony, a pine resin product that is known to be a respiratory sensitizer.18 She was not aware of any coworkers with similar symptoms. Pulmonary function tests performed near the end of a work week confirmed asthma. Regular use of an inhaled steroid was prescribed, along with an inhaled bronchodilator when needed. She was referred to a respirologist for assessment of possible occupational asthma. Before the assessment, she was instructed to record symptoms, serial PEFRs and medication use. She brought this documentation, along with copies of the MSDSs from her workplace, to the appointment with the specialist for interpretation. Assessment by the respirologist confirmed occupational asthma, likely secondary to exposure to colophony: the variability in her PEFR was worse on working days, and methacholine hyperresponsiveness was 3 times as great (i.e., methacholine PC20 was 3 times lower) at the end of a work week than at the end of a holiday period. A workers' compensation claim was submitted and accepted, and she was retrained for office work. The symptoms cleared 3 months after she left her previous position, and she needed no further medication. The provincial ministry of labour reviewed conditions in the workplace and advised modifications to the ventilation system to reduce workers' exposure to fumes from the soldering flux.
Key points .
If new-onset asthma develops during a person's working life, occupational asthma should be considered.
Exposure to irritants in the workplace commonly aggravates underlying asthma, but this condition is managed differently from occupational asthma, and compensation also differs.
Occupational asthma should be suspected if symptoms began within 24 hours of exposure to high levels of an irritant at work (irritant-induced occupational asthma) or if symptoms worsen while the person is at work or shortly after he or she leaves work and diminish on weekends and holidays (sensitizer-induced occupational asthma).
Objective investigations are needed, because a diagnosis of occupational asthma often has significant implications for the person's working situation. Furthermore, a history consistent with occupational asthma has poor specificity for the diagnosis.
Unless the patient's asthma is severe and cannot be controlled, the primary care physician should advise the patient not to stop working until the diagnosis has been confirmed.
Early referral to a specialist is usually needed for full investigation.
The primary care physician can initiate investigations to confirm that the symptoms are due to asthma and to begin serial monitoring of peak flow.
In cases of sensitizer-induced occupational asthma, early, accurate diagnosis and avoidance of further exposure are associated with the best prognosis.
A patient with irritant-induced occupational asthma may be able to continue with his or her job, with changes in the workplace, if necessary, to prevent further high-level exposure to irritants.
Patients with workplace aggravation of existing asthma should be assessed to ensure that measures to manage the asthma are optimal. Although measures to reduce exposure to workplace irritants may be required, such patients are often able to continue working in the same job.
Footnotes
This article has been peer reviewed.
Contributors: Drs. Tarlo and Liss both initiated the concept and design of the manuscript. Dr. Tarlo wrote the first draft and contributed to subsequent revisions. Dr. Liss also contributed to subsequent revisions. Both authors approved the final version.
Competing interests: None declared.
Correspondence to: Dr. Susan M. Tarlo, Toronto Western Hospital EC4-009, 399 Bathurst St., Toronto ON M5T 2S8; fax 416 603-6763; susan.tarlo@utoronto.ca
References
- 1.Manfreda J, Becklake MR, Sears MR, Chan-Yeung M, Dimich-Ward H, Siersted HC, et al. Prevalence of asthma symptoms among adults aged 20-44 years in Canada. CMAJ 2001;164(7):995-1001. [PMC free article] [PubMed]
- 2.Bernstein IL, Chan-Yeung M, Malo JL, Bernstein DI. Definition and classification of asthma. In: Asthma in the workplace. 2nd ed. New York: Marcel Dekker Inc.; 1999. p. 1-4.
- 3.Meredith S, Nordman H. Occupational asthma: measures of frequency from four countries. Thorax 1996;51:435-40. [DOI] [PMC free article] [PubMed]
- 4.Chan-Yeung M, Malo JL. Tables of major inducers of occupational asthma. In: Bernstein IL, Chan-Yeung M, Malo JL, Bernstein DI, editors. Asthma in the workplace. 2nd ed. New York: Marcel Dekker Inc.; 1999. p. 683-720.
- 5.Gautrin D, Bernstein IL, Brooks S. Reactive airways dysfunction syndrome or irritant-induced asthma. In: Bernstein IL, Chan-Yeung M, Malo JL, Bernstein DI, editors. Asthma in the workplace. 2nd ed. New York: Marcel Dekker, Inc.; 1999. p. 565-93.
- 6.Tarlo SM, Broder I. Irritant induced asthma. Chest 1989;96:297-300. [DOI] [PubMed]
- 7.Chan-Yeung M. Assessment of asthma in the workplace. ACCP consensus statement. American College of Chest Physicians. Chest 1995;108:1084-117. [DOI] [PubMed]
- 8.Tarlo SM, Boulet LP, Cartier A, Cockcroft D, Cote J, Hargreave FE, et al. Canadian Thoracic Society guidelines for occupational asthma. Can Respir J 1998;5:289-300. [DOI] [PubMed]
- 9.Tarlo SM, Banks DE, Liss G, Broder I. Outcome determinants for isocyanate-induced occupational asthma among compensation claimants. Occup Environ Med 1997;54:756-61. [DOI] [PMC free article] [PubMed]
- 10.Malo JL, Ghezzo H, L'Archeveque J, Lagier F, Perrin B, Cartier A. Is the clinical history a satisfactory means of diagnosing occupational asthma? Am Rev Respir Dis 1991;143:528-32. [DOI] [PubMed]
- 11.American Thoracic Society. Guidelines for methacholine and exercise challenge testing — 1999. Am J Respir Crit Care Med 2000;161:309-29. [DOI] [PubMed]
- 12.Banks DE, Barkman HW Jr, Butcher BT, Hammad YY, Rando RJ, Glindmeyer HW 3rd, et al. Absence of hyperresponsiveness to methacholine in a worker with methylene diphenyl diisocyanate (MDI)-induced asthma. Chest l986;89:389-93. [DOI] [PubMed]
- 13.Moscato G, Godnic-Cvar J, Maestrelli P, Malo JL, Burge PS, Coifman R. Statement on self-monitoring of peak expiratory flows in the investigation of occupational asthma. Subcommittee on Occupational Asthma of the European Academy of Allergy and Clinical Immunology. Eur Resp J 1995;8:1605-10. [PubMed]
- 14.Leroyer C, Perfetti L, Trudeau C, L'Archeveque J, Chan-Yeung M, Malo JL. Comparison of serial monitoring of peak expiratory flow and FEV1 in the diagnosis of occupational asthma. Am J Respir Crit Care Med l998;158:827-32. [DOI] [PubMed]
- 15.Grammer L, Shaughnessy M, Kenamore B. Utility of antibody in identifying individuals who have or will develop anhydride-induced respiratory disease. Chest 1998;114:1199-202. [DOI] [PubMed]
- 16.Boulet LP, Becker A, Bérubé D, Beveridge R, Ernst P, on behalf of the Canadian Asthma Consensus Group. Canadian asthma consensus report, 1999. CMAJ 1999;161(11 Suppl):S1-S62. [PMC free article] [PubMed]
- 17.Martyny J, Glazer CS, Newman LS. Respiratory protection. N Engl J Med 2002;347:824-30. [DOI] [PubMed]
- 18.Burge PS, Edge G, Hawkins R, White V, Taylor AN. Occupational asthma in a factory making flux-cored solder containing colophony. Thorax 1981;36:828-34. [DOI] [PMC free article] [PubMed]


