Abstract
Rhinovirus type 16 was found to replicate in mouse L cells that express the viral receptor, human intercellular adhesion molecule 1 (ICAM-1). However, infection of these cells at a low multiplicity of infection leads to no discernible cytopathic effect, and low virus titers are produced. A variant virus, 16/L, was isolated after alternate passage of rhinovirus 16 between HeLa and ICAM-1 L cells. Infection of mouse cells with 16/L leads to higher virus titers, increased production of RNA, and total cytopathic effect. Three amino acid changes were identified in the P2 region of virus 16/L, and the adaptation phenotype mapped to two changes in protein 2C. The characterization of a rhinovirus host range mutant will facilitate the investigation of cellular proteins required for efficient viral growth and the development of a murine model for rhinovirus infection.
Human rhinoviruses (HRVs) are responsible for the majority of common cold infections (reviewed in reference 32). Although the upper respiratory tract infections caused by rhinoviruses are generally mild in the healthy population, they pose a serious health risk for patients with chronic respiratory diseases such as asthma or cystic fibrosis. The common cold is implicated in approximately half of the most severe asthma attacks in adults (28) and in 80 to 85% of asthma exacerbations in children (22). Approximately 30% of pulmonary exacerbations in patients with cystic fibrosis are preceded by viral respiratory tract infections, of which half are caused by rhinoviruses (29, 33). In addition, antibiotics are often prescribed inappropriately for rhinovirus infections, contributing to increased drug resistance (9, 37, 49). Because there are no effective treatments, rhinovirus infections are also a significant socioeconomic problem due to loss of work and school days, as well as doctor visits.
The symptoms of a rhinovirus infection are largely immune mediated (19, 41, 52) and occur after virus levels have peaked in the infected host (26). These features have hindered the design of therapeutically useful antiviral drugs. Anti-inflammatory drugs such as antihistamines and decongestants are also largely ineffective (26, 40). The lack of a small animal model to study the pathogenesis of rhinovirus infection has hampered the design of drugs that would be more efficacious in the treatment or prevention of infection. The chimpanzee, the only nonhuman animal susceptible to rhinovirus, is an impractical model because it is costly and difficult to work with. A murine model would permit study of the immunological response to infection and perhaps uncover additional drug targets.
HRVs are members of the Picornaviridae. More than 100 serotypes of HRVs have been identified and are divided into major and minor groups depending on receptor utilization. The receptor for the major group of rhinoviruses is human intercellular adhesion molecule 1 (ICAM-1), and a low-density-lipoprotein receptor-like protein is the receptor for the minor group rhinoviruses. Rhinoviruses are nonenveloped viruses with an icosahedral capsid enclosing a single-stranded, positive-sense RNA genome that is translated after cell entry. The viral polyprotein is divided into a P1 region, which encodes the capsid proteins VP1, VP2, VP3, and VP4, and the P2 and P3 regions, which include proteins 2APro, 2B, 2C, 3A, 3B (VPg), 3CPro, and 3DPol. Viral proteases cleave the polyprotein into the component viral proteins, with the cleavage end products, as well as some of the precursors, having independent functions.
Mouse cell lines are not permissive for infection by most minor group rhinovirus serotypes, even though the cells produce low-density-lipoprotein receptor. The exceptions are serotype HRV1A (34) and a variant of HRV2 (HRV2/L) selected by passage in mouse cells (51). The P2 proteins of HRV2/L and HRV2 migrate differently on protein gels, but the changes required for adaptation to mouse cells have not been identified (51). In contrast, ICAM-1 is not present on the surface of mouse cells. It is believed that mouse cell lines are neither susceptible nor permissive for infection with the major group HRVs. However, a variant of major group HRV39 obtained after transfection of mouse L cells with viral RNA was able to replicate and produce altered P2 proteins (25).
We show here that HRV16 replicates in mouse L cells after transfection of viral RNA or after infection of L cells stably expressing human ICAM-1 (ICAM-L cells). Virus replication in ICAM-L cells produced low viral titers and no cell death. After 35 alternate passages of HRV16 between ICAM-L cells and HeLa cells, a variant (16/L) was isolated. This virus replicates to higher titers in ICAM-L cells, produces increased amounts of viral RNA, and causes cell death. The mutations responsible for the adapted phenotype are located in the region of the viral genome that encodes the multifunctional proteins 2BC and 2C. Both proteins are part of the viral RNA replication complex (7, 11, 42), but their functions are distinct. 2BC is involved in membrane rearrangement during infection (12, 36, 44, 45). The 2C protein is an NTPase that is required for viral replication, but little is known about its interactions with cellular proteins (8, 24, 27, 30, 31). Identification of a rhinovirus host range mutant will facilitate the study of protein-protein interactions between the host cell and the virus that are required for replication.
MATERIALS AND METHODS
Cells and viruses.
L cells (mouse embryonic fibroblasts) and HeLa cells were maintained in Dulbecco modified Eagle medium (DMEM) containing 10% bovine calf serum and 5% penicillin-streptomycin (Gibco). Mouse L cells stably expressing ICAM-1 were isolated by cotransforming L cells with a plasmid encoding puromycin resistance and pEFBOS-ICAM1, a mammalian expression vector encoding human ICAM-1 protein (provided courtesy of Darren Shafren). Transformants were selected in DMEM containing 10% bovine calf serum, 5% penicillin-streptomycin, and 8 μg of puromycin/ml. Approximately 3 weeks later, ICAM-expressing cells were sorted by flow cytometry with a fluorescein isothiocyanate-conjugated anti-CD54 antibody (Chemicon). Single cells of the ICAM-1-expressing population were cloned and expanded. ICAM-L cells were maintained in selection medium containing 8 μg of puromycin/ml. Stocks of HRV16 were made by transfection of HeLa cells with RNA transcripts produced from pRV16.11, an infectious clone of HRV16 (kindly provided by Wai-Ming Lee, University of Wisconsin). RNA transcripts were produced by in vitro transcription of a linearized template by using T7 RNA polymerase (Invitrogen) and introduced into cells with DEAE-dextran. Cells were subjected to three freeze-thaw cycles, and virus was plaque purified twice. Transfection and plaque purification were carried out at 33°C.
Identification of rhinovirus variants.
After approximately 30 alternate passages of HRV16 between HeLa and ICAM-L cells, cytopathic effects (cell rounding and detachment from the monolayer) became evident in infected ICAM-L cells. The virus was passed four more times exclusively on ICAM-L cells, and a plaque-purified stock was made. Initially virus was harvested 48 h postinfection. Halfway through the adaptive passages, virus was collected earlier after it was found that peak levels of virus production occurred in ICAM-L cells 12 to 24 h postinfection and in HeLa cells 36 to 48 h postinfection.
Isolation of viral RNA.
Supernatants from virus-infected cells were centrifuged in an SW41 rotor (Beckman) for 2 h at 40,000 rpm. The pellet was resuspended in 150 μl of NTE buffer (100 mM NaCl, 50 mM Tris-HCl [pH 8.0], 10 mM EDTA), and 1.5 ml of TRIzol reagent (Invitrogen) was added. The mixture was divided and incubated for 5 min in 1.5-ml microcentrifuge tubes. Then, 400 μl of chloroform was added, and the tubes were centrifuged for 15 min at 12,000 × g at 4°C. The aqueous phase was placed in fresh tubes, and 1 μl of RNasin (Promega) was added. Equal volumes of isopropanol were added, and the mixtures were centrifuged at 12,000 × g for 10 min after a 30-min incubation at room temperature. The RNA pellet was washed with 70% ethanol, air dried, resuspended in 10 mM dithiothreitol with 5% (vol/vol) RNasin, and stored at −80°C.
Isolation of 16/L infectious DNA clone.
cDNA was produced from viral RNA by reverse transcription with Superscript II (Gibco) at 42°C for 1 h with a virus-specific primer with the sequence 5′-CGCGCATGCTTTTTTTTTTTTTTTTATAAAACTAACAAACTATTC-3′. The primer was designed to include an SphI site after the poly-A sequence in the viral RNA. The sample was incubated with 1 μl of RNase H (Pharmacia Biotech) and subjected to PCR by using the Expand Long-Template system (buffer 1; Roche) according to the manufacturer's protocol. The same 3′ primer was used with a 5′ primer containing a SacI site and a T7 promoter with the sequence 5′-CGCGAGCTCTAATACGACTCACTATAGGTTAAAACTGGATCTGGGTTGTTCCC-3′. The full-length PCR product was cleaved with SacI and SphI, cloned into pUC19, and propagated in Escherichia coli DH5α. The complete nucleotide sequences of both the parent pRV16.11 and the adapted virus pUCRV16/L were determined.
Site-directed mutagenesis.
The 16/MVDN mutant was produced by switching the ClaI/SnaBI DNA fragments of pRV16.11 and pUC16/L. Site-directed mutagenesis of the wild-type pRV16.11 DNA to create the 16/MV, 16/DN, and 16/NS mutants was carried out by PCR. The presence of the mutations was verified by nucleotide sequence analysis.
Measurement of cytopathic effect.
The cytopathic effect was measured by using a trypan blue exclusion assay. This dye is excluded from viable cells but not from dead cells. Infected and uninfected cells were collected by centrifugation and washed once with cold phosphate-buffered saline. The cells were resuspended in phosphate-buffered saline, mixed with an equal volume of trypan blue (Gibco), and counted by using a hematocytometer.
Quantitation of viral RNA.
Slot blot hybridization analysis was performed by extracting total RNA from infected cells with TRIzol and vacuum blotting on a GeneScreen membrane (New England Nuclear). RNA was cross-linked with UV irradiation in a Stratalinker (Stratagene) and baked on the membrane for 2 h at 80°C. The membrane was hybridized with radiolabeled probes specific for either plus- or minus-sense viral RNA produced by in vitro transcription of the EcoRI fragment of pRV16.11 (nucleotides 1580 to 6785) in pBluescript SK II (Stratagene). RNA levels were quantitated by using a PhosphorImager and ImageQuant software (Molecular Dynamics). The values obtained at each time point for each virus were normalized to levels at time zero. These values were then divided by the number obtained for the wild-type virus to provide relative ratios of RNA production.
Rhinovirus plaque assay.
Virus growth was assayed by using a modified version of a plaque assay developed previously (20). Briefly, HeLa cells were seeded on six-well plates for approximately 70% confluence at the time of plaquing. Next, 100-μl portions of serial 10-fold virus dilutions were incubated with cells for 1 h at 33°C on a rocker. Two overlays were added to the infected cells. The first overlay consisted of 2 ml of 1× DMEM, 0.8% Noble agar, 0.1% bovine serum albumin, 40 mM MgCl2, and 10% bovine calf serum. After solidification, a second liquid overlay was added that was composed of 1× DMEM, 0.1% bovine serum albumin, 40 mM MgCl2, 0.2% glucose, 2 mM pyruvate, 4 mM glutamine, and 4 mM oxaloacetic acid. The cells were incubated at 33°C for 72 h and developed by using 10% trichloroacetic acid and crystal violet. All plaque assays were done on HeLa cells; none of the viruses produced plaques on ICAM-L cells.
Thermostability assays.
Virus stocks were diluted to equivalent concentrations and heated at 45°C for 0, 30, 60, 90, and 120 min before plaque assay. Samples were withdrawn at different time points, and the plaque assay was carried out immediately. Levels of virus remaining at each time point were quantified and expressed as a fraction of initial virus titers.
Induction of 2BC and 2BC/L expression.
2BC and 2BC/L were inducibly expressed as fusion proteins with enhanced green fluorescent protein (EGFP) in ICAM-L cells by using the GeneSwitch system (Invitrogen). DNAs encoding 2BC and 2BC/L were amplified from pRV16.11 and pUC16/L, ligated into pEGFP-N1 (Clontech), and then released by cleavage with EcoRI and NotI. The resulting DNA fragment encodes an optimal Kozak consensus sequence, followed by 2BC or 2BC/L and EGFP. A stop codon was included at the end of the sequence, and the fragment was cloned into pGeneV5His-C, an expression plasmid driven by the regulatory fusion protein GAL4-DBD/hPR-LBD/p65-AD. DNA encoding the EGFP protein was also cloned into pGeneV5His-C as a control. Stable cell lines producing the regulatory protein were created according to the manufacturer's protocol and maintained under hygromycin selection. The cell lines were then transiently transformed for inducible expression with plasmids pGeneV5His-C-EGFP, pGeneV5His-C-2BC-EGFP, or pGeneV5His-C-2BC/L-EGFP and induced 24 h posttransfection with 10−8 M mifepristone. Cell viability was measured by using the trypan blue assay described above.
Protein interaction analysis by yeast two-hybrid system.
The 2BC proteins of RV16 and RV16/L were amplified from pRV16.11 and pUCRV16/L, respectively, by using PCR with restriction enzyme-linked primers and then cloned into the yeast vectors pGBKT7 and pACT2 (Clontech). The plasmids were introduced by transformation into the yeast strain YGH1 and selected on SC-Trp-Leu plates. Screens were carried out initially by testing for β-galactosidase activity by using a filter lift assay; three colonies were picked and grown to an optical density at 600 nm (OD600) of ∼0.5. One OD600 unit was collected and resuspended in 50 μl of Y-PER (Pierce) and then incubated at 30°C for 3 min. Next, 200 μl of o-nitrophenyl-β-d-galactopyranoside (ONPG) diluted in dimethylformamide (4 mg/ml) was added, and the samples were placed at 30°C until a yellow color was observable. Then, 500 μl of 1 M NaCO3 was added to stop the reaction, and the samples were placed on ice until the end of the time period (360 min). All samples were clarified by centrifugation, and the OD420 value was determined. This value was converted to Miller units by dividing it by the time in minutes until the yellow color appeared (or by 360 min if no color appeared) and multiplying the value by 103.
RESULTS
Major group HRV16 grows in mouse cells.
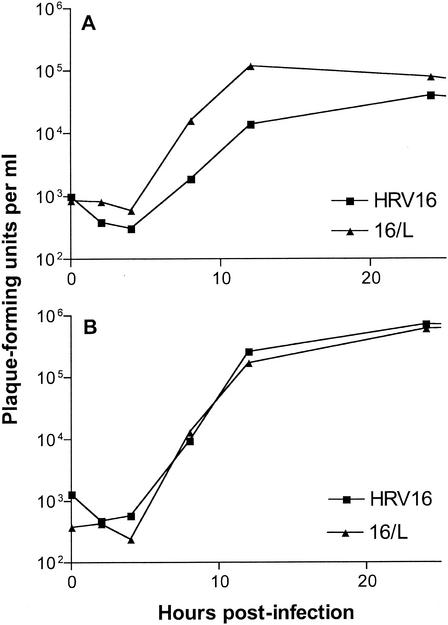
To determine whether mouse cells are permissive for replication of a major group rhinovirus, viral RNA was transcribed in vitro from HRV16 DNA and introduced into mouse L and 3T3 cells by transfection. Both cell lines supported viral replication, producing ca. 103 PFU/ml at 3 days posttransfection. These cell lines are not susceptible to infection with major group HRVs because they do not express ICAM-1, the receptor for cell entry. For this reason, cell lines stably expressing human ICAM-1 were isolated and used for subsequent experiments. These cells are susceptible to infection with HRV16, but the cells do not develop total cytopathic effect, and the amount of virus released after one cycle of growth was lower than in HeLa cells (Fig. 1A). Infection of HeLa cells with HRV16, in contrast, led to total cytopathic effect and a yield of 105 to 106 PFU/ml (Fig. 1B).
FIG. 1.
One-step growth analysis. At the indicated times postinfection, cells were scraped into the medium, virus was released by freeze-thawing, and the virus titer was determined by plaque assay on HeLa cells. (A) Growth of HRV16 and 16/L in ICAM-L cells infected with 10 PFU/cell; (B) growth of HRV16 and 16/L in HeLa cells infected with 10 PFU/cell.
Isolation of HRV16 mutant with improved growth in ICAM-L cells.
To improve the replication of HRV16 in mouse cells, the virus was serially passaged between HeLa and ICAM-L cells, an approach previously used to adapt rhinovirus 2 for growth in mouse cells (51). After 35 alternate passages, a virus was isolated (16/L) that causes total cytopathic effect on ICAM-L cells. In a one-step growth experiment in ICAM-L cells, 16/L displayed faster kinetics of replication and increased yields compared to wild-type HRV16 (Fig. 1A). In HeLa cells, the two viruses replicated with similar kinetics and to equal titers (Fig. 1B).
Improved growth of 16/L in mouse cells maps to the viral 2C protein.
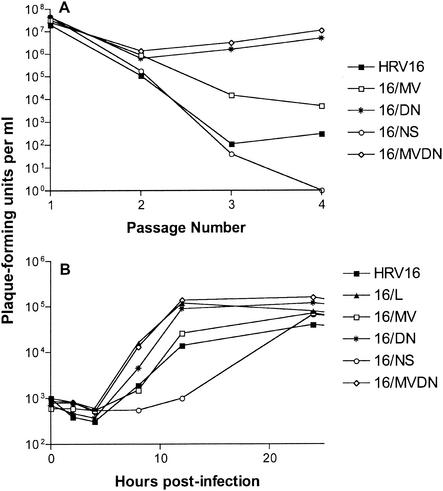
A full-length DNA copy of the 16/L genome was prepared from viral RNA, and RNA transcripts produced from the cloned DNA were infectious. The complete nucleotide sequences of 16/L DNA and of its parent wild-type HRV16 revealed three mutations in the genome of 16/L that lead to coding changes: one in the 2B protein, N26S, and two in the 2C protein, M121V and D266N. To determine which mutation was responsible for the improved growth of 16/L, each change was introduced singly into the wild-type DNA (16/MV, 16/DN, and 16/NS). In addition, both 2C mutations were placed together in a wild-type background (16/MVDN). RNA transcripts from each DNA were introduced into HeLa cells to produce high-titer virus stocks. When viruses were then passed three times on ICAM-L cells, only 16/DN and 16/MVDN produced high titers (Fig. 2A). Titers of 16/MV were slightly higher than HRV16, whereas the 2B mutation (16/NS) alone had no effect on the ability of HRV16 to grow in ICAM-L cells.
FIG. 2.
(A) Serial passage of rhinoviruses in mouse cells. Viral RNAs produced by in vitro transcription were introduced into HeLa cells by transfection (passage 1), and the viruses produced were serially passaged in ICAM-L cells (passages 2 to 4). Virus titers were quantified by plaque assay in HeLa cells after each passage. (B) One-step growth analysis of rhinoviruses on ICAM-L cells infected with 10 PFU/cell.
The results of one-step growth analysis in ICAM-L cells show that the replication kinetics and yield of 16/L, 16/DN, and 16/MVDN were almost identical (Fig. 2B). The replication of 16/MV resembled that of HRV16, and 16/NS lagged behind all of the others. In HeLa cells, all viruses replicated with equal kinetics (data not shown), indicating that the mutations conferred a specific adaptation to mouse cells. These results suggest that two amino acid changes in 2C are responsible for the improved growth of 16/L in ICAM-L cells.
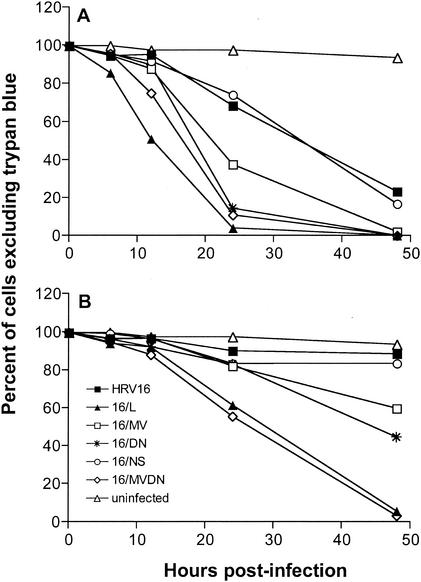
Virus 16/L kills ICAM-L cells.
To determine which mutation was responsible for the ability of virus 16/L to cause a cytopathic effect, a trypan blue exclusion assay was used to measure the viability of infected cells. At 24 h postinfection at a multiplicity of infection of 10, 16/L killed 97% of ICAM-L cells, whereas HRV16 killed only 32% (Fig. 3A). Viruses 16/MVDN and 16/DN caused nearly as much cytopathic effect as 16/L at this time point, but the kinetics of cell killing were slower. Although 16/MV causes significantly more cell death than either HRV16 or 16/NS, the cytopathic effects were less pronounced than with 16/DN or 16/MVDN, and 16/NS and HRV16 killed cells at nearly identical rates. By 48 h postinfection, viruses 16/L, 16/MVDN, and 16/DN caused a total cytopathic effect, whereas neither 16/NS or HRV16 killed more than 80% of infected cells.
FIG. 3.
Trypan blue exclusion assay. ICAM-L cells were infected with the indicated viruses with 10 (A) or 1 (B) PFU/cell. At the indicated times after infection, cells were assayed for exclusion of trypan blue. Cells excluding trypan blue are viable and are expressed as a percentage of the total cells in each sample at each time point.
At a multiplicity of infection of 1, the differences in cell killing between the viruses are more dramatic (Fig. 3B). Both 16/L and 16/MVDN cause total cytopathic effect by 48 h postinfection. Viruses with individual mutations have a hierarchy of cell-killing abilities: virus 16/DN is the most cytopathic, 16/MV kills slightly fewer cells, and 16/NS kills cells at rates close to that of HRV16. These findings are in agreement with the results of growth curve analysis and indicate that both changes in 2C contribute to the increased cytopathic effect seen in 16/L infection of mouse cells.
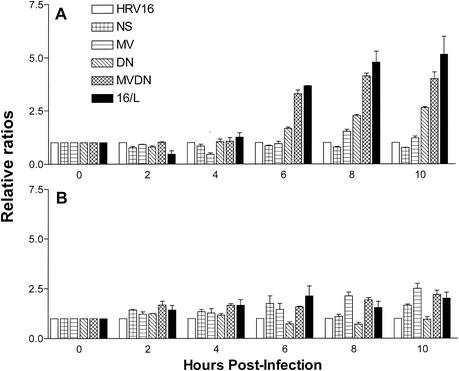
Higher levels of positive-strand viral RNA are produced in 16/L-infected ICAM-L cells than in HRV16-infected cells.
To determine whether the increased titers of virus 16/L in ICAM-L cells were reflective of increased RNA production, total cell RNA was isolated at different times after infection and analyzed by slot blot analysis with hybridization probes specific for positive- or negative-strand RNA. In infected ICAM-L cells, 16/L RNA levels are more than five times that of HRV16, and both mutations in 2C appeared to contribute to the increased RNA levels (Fig. 4A). Most of the viruses also showed increased RNA production in HeLa cells, but these increases were modest compared to the effect in ICAM-L cells (Fig. 4B). Relative levels of negative-sense RNA production mirrored positive-sense RNA production in both cell lines and for all viruses (data not shown).
FIG. 4.
Positive-strand viral RNA production. ICAM-L cells (A) or HeLa cells (B) were infected with virus at 10 PFU/cell. At the indicated times after infection, total RNA was extracted and immobilized on a membrane. Plus-strand viral RNA was detected by hybridization with a 32P-labeled RNA probe. RNA levels were quantified by using a PhosphorImager and ImageQuant software. At each time point, viral RNA levels were normalized to levels at time zero and to amounts of wild-type HRV16 RNA.
Expression of 2BC/L protein is not responsible for the increased cytopathic effect in 16/L infected cells.
In infected cells, the precursor of 2C, the 2BC protein, is present and functionally distinct from 2C. To determine whether protein 2BC from 16/L (2BC/L) was responsible for increased cytopathic effect during infection of mouse cells, the protein and its wild-type counterpart were expressed in mouse cells independently of viral infection. Because antibody to HRV16 2BC is not available, the proteins were fused to EGFP for detection in an inducible system. The expression of 2BC or 2BC/L was quantitated by flow cytometry, and cell death was measured by using the trypan blue exclusion assay. The results indicate that both EGFP-2BC and EGFP-2BC/L, but not EGFP alone, are toxic to ICAM-L cells at equal levels (data not shown). Therefore, production of 2BC/L protein is not the sole cause of the increased levels of cytopathic effect observed in 16/L infection of ICAM-L cells.
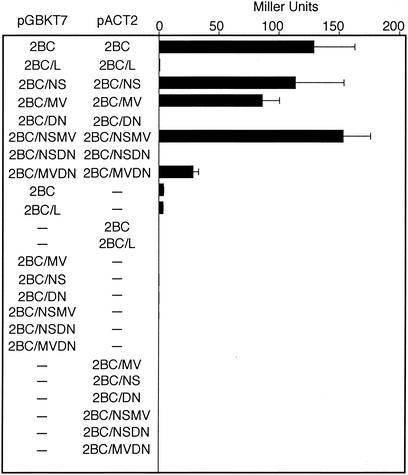
Dimerization of 2BC, but not 2BC/L, in a yeast two-hybrid system.
Poliovirus 2B and 2BC proteins form homomultimers when assayed in vitro or in the yeast two-hybrid system (13). Coxsackievirus B3 2B and 2BC proteins also form homomultimers in mammalian cells when assayed by a two-hybrid system or by fluorescence resonance energy transfer microscopy (15, 47). However, there is no evidence for the dimerization of coxsackievirus or poliovirus 2C protein. It was of interest to determine whether 2BC of HRV16 dimerizes and whether changes in 2BC/L affect the protein-protein interaction. When assayed in the yeast two-hybrid system, HRV16 2BC protein forms homodimers, whereas 2BC/L does not (Fig. 5). To determine which amino acid change(s) is responsible for the inability of 2BC/L to dimerize in yeast, the mutations were introduced singly and in pairs into pGBKT7-2BC and pACT-2BC. The single-amino-acid change in protein 2C from aspartic acid to asparagine (D266N) is sufficient to block dimerization of the 2BC protein (Fig. 5). 2BC proteins containing the single-amino-acid changes M121V or N26S or both M121V and N26S together are able to form dimers. No dimerization was observed of protein 2BC containing both D266N and N26S. Surprisingly, reduced levels of dimerization were observed with 2BC protein with M121V and D266N. Homodimers of 2BC and 2BC/L proteins produced from plasmids were not detected by immunoprecipitation from either HeLa or ICAM-L cells (data not shown). The functional relevance of 2BC homodimerization is under investigation.
FIG. 5.
Homodimerization of 2BC proteins containing single or multiple amino acid changes determined by yeast two-hybrid assay. Plasmids pACT and pGBKT7 either alone or containing genes encoding the indicated proteins were introduced into yeast strain YGH1 by cotransformation. Empty vectors are designated by dashes (—). Interaction of the fusion proteins was quantified by using the Miller assay.
DISCUSSION
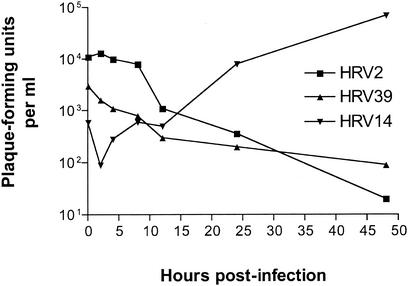
The presence or absence of an appropriate receptor on the cell surface determines whether the cell is susceptible to virus infection. Mouse cell lines are not susceptible to infection by major group HRVs because the viral receptor, ICAM-1, is absent from the cell surface. It was believed that mouse cells are not permissive to infection with HRVs because the cells lack intracellular molecules required for virus replication (50, 51). Although mouse cells are not susceptible to HRV16, replication occurred, to our surprise, after transfection of wild-type viral RNA. The block to subsequent replication cycles was overcome by expression of the viral receptor, ICAM-1, on the mouse cell surface. The ability of rhinoviruses to grow in mouse cells was found to be serotype specific, since the cells are not permissive for either minor-group HRV2 or major-group HRV39 but did allow replication of major-group viruses HRV16 and HRV14 (Fig. 6).
FIG. 6.
One-step growth analysis of HRV2, HRV39, and HRV14 in ICAM-L cells infected at 10 PFU/cell. At the indicated times postinfection, cells were scraped into the medium, virus was released by freeze-thawing, and the virus titer was determined by plaque assay on HeLa cells.
To improve the replication of HRV16 in mouse cells, the virus was alternately passaged between HeLa cells and ICAM-L cells. The variant obtained in this manner, 16/L, causes more extensive cytopathic effect in mouse cells and produces higher levels of infectious virus and viral RNA. The adaptation is specific for mouse cells, since HRV16 and 16/L produce similar amounts of virus and viral RNA in infected HeLa cells. There are three coding differences between HRV16 and 16/L: one in protein 2B and two in protein 2C. The adaptation phenotype maps to two amino acid changes in the 2C protein, M121V and D266N. The amino acid change in protein 2B, N26S, appears to be extraneous.
Much of our knowledge about the functions of proteins 2B, 2C, and 2BC has come from studies on cells infected with picornaviruses related to rhinovirus, such as poliovirus, coxsackievirus, and hepatitis A virus, and by expression of recombinant forms of the proteins. The expression of protein 2B or 2BC causes permeabilization of cellular membranes and triggers release of intracellular calcium from the endoplasmic reticulum (2, 21, 43, 46). Expression of protein 2B disturbs intracellular calcium levels by disrupting the endoplasmic reticulum membrane, and it has been proposed that such alterations could lead to plasma membrane lesions and virus release (46). Protein 2B might act as a viroporin, a viral protein that alters the permeability of cell membranes, and aggregates at membrane surfaces to produce small tetrameric pores (1). The 2B protein associates with cellular membranes via its two hydrophobic domains. Deletion of either domain reduces membrane association, and removal of both abrogates membrane association to a large extent (14). Picornavirus infection also leads to the inhibition of cellular protein trafficking, and this effect maps to both the 2B and the 3A proteins of picornaviruses (16). This inhibition can be induced in yeast or mammalian cells by the expression of proteins 2B or 3A (6).
One of the most dramatic alterations that occurs in picornavirus-infected cells is the extensive rearrangement of intracellular membranes. Viral RNA replication occurs on the outer surface of double-membraned vesicles derived initially from the endoplasmic reticulum and, later in infection, from the Golgi (12, 39, 42). Expression of 2BC protein in yeast and mammalian cells leads to membrane rearrangement (5), and the membrane proliferation activity maps to the 2C portion of the protein (6). However, the vesicles induced by 2C expression are less similar to those observed during viral infection than are vesicles induced by 2BC expression (3, 12). Viral RNA replication occurs in the center of a tightly packed rosette of vesicles that protects the nascent RNA and viral proteins. The 2C protein has both RNA- and membrane-binding motifs (4, 17, 18, 35, 44) and has been proposed to act as an anchor for RNA, tethering it to the inner surface of the rosette and allowing genomic replication to proceed (10). Protein 2C is also likely to contribute to the formation and maintenance of the rosette structure.
Protein 2C may also have a role in virion assembly. A temperature-sensitive poliovirus mutant with changes in the 2C protein is unable to release RNA from capsids at the nonpermissive temperature (23). Poliovirus mutants resistant to hydantoin, a drug that blocks virion assembly, have single amino acid changes in the 2C protein (48). However, no differences in the thermostability of HRV16 and 16/L virions were detected (data not shown), indicating that the changes in 2C are not likely to affect virion structure.
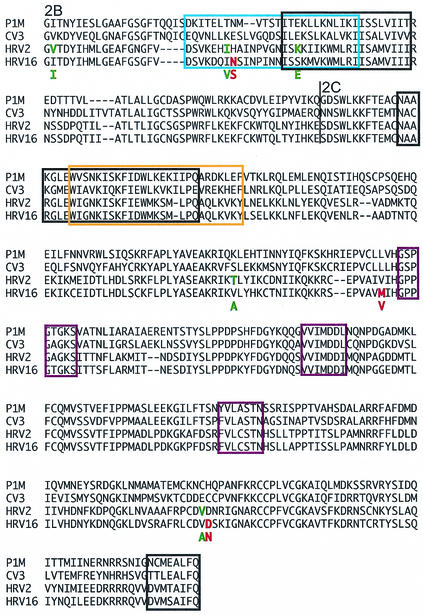
How do the changes in protein 2C enhance the replication and cytopathic effect of rhinovirus 16 in mouse cells? Amino acid changes in 2C crucial for the adaptation phenotype do not fall within nucleoside triphosphate binding motifs or domains important for binding RNA or membranes (Fig. 7). One possibility is that changes in 2BC are directly responsible for the enhanced cytopathic effect of 16/L. However, our results do not support this hypothesis: expression of the 2BC and 2BC/L proteins in mouse cells leads to comparable cytopathy. Alternatively, the increased cell killing of 16/L may simply be a consequence of its enhanced ability to replicate in mouse cells. How could changes in 2BC protein specifically improve replication in mouse cells? The 2BC/L protein might more efficiently induce the formation of membrane vesicles on which RNA synthesis occurs. Consistent with this hypothesis, more viral RNA is produced in mouse cells infected with 16/L than in cells infected with HRV16. Unfortunately, the mechanism by which 2BC induces membrane vesicles in cells is unknown. The 2B and 2BC proteins colocalize on vesicular membranes with COPII proteins of the anterograde transport system, which are involved in the budding of poliovirus-induced membrane vesicles from the endoplasmic reticulum (38). 2BC might exert its membrane-proliferating effects through direct or indirect interactions with COPII proteins or with other cell proteins involved in vesicle formation. Protein 2BC or 2C could have a reduced interaction with a murine ortholog of a human protein, leading to inefficient replication, and amino acid changes in 16/L might optimize this interaction. As a consequence, vesicle induction in mouse cells would improve and more viral RNA synthesis would occur, leading to enhanced viral replication.
FIG. 7.
Alignment of the 2BC proteins of poliovirus, coxsackievirus, HRV2, and HRV16. Most structure-function information on 2BC comes from studies on poliovirus and coxsackievirus, and these domains were extrapolated to the rhinovirus proteins. Proteins 2B and 2C are labeled, and the cleavage site between the two is marked with a line. Outlined in purple are nucleoside triphosphate-binding motifs (36, 45). RNA-binding regions are outlined in blue (35), and membrane-binding regions are outlined in black (14, 17, 18, 44). Regions binding both membranes and RNA are outlined in orange. In the HRV16 sequence, red letters indicate amino acids that have changed in the mouse-adapted strain. In the HRV2 sequence, green letters indicate amino acids that have changed in the mouse-adapted strain. The amino acid in the adapted strain is shown below the parental sequence.
Multimerization of picornavirus 2B and 2BC proteins has been demonstrated in yeast and in mammalian cells (13, 15, 47). Here we show that the D266N amino acid change, which by itself can significantly improve replication of HRV16 in mouse cells, prevents the dimerization of protein 2BC in yeast. Although we do not know whether HRV16 protein 2BC forms dimers in virus-infected cells, it is tempting to speculate that the lack of dimerization of 2BC/L is related to the improved growth of HRV16/L in mouse cells. This hypothesis is confounded by the observation that protein 2BC/MVDN does dimerize in yeast, albeit to a low level, and the growth of virus carrying these two mutations is comparable to that of 16/L. It is possible that the inability of protein 2BC/L to dimerize is unrelated to virus growth in any cell type but rather is a reflection of the conformational state of the protein. Conformational changes that are a result of the amino acid substitutions might confer an improved interaction with host cell protein required for replication.
A variant of HRV2 (HRV2/L) that grows in mouse cells produces P2 proteins that migrate differently on protein gels compared to those of the parent virus (51). The nucleotide sequence of the P2 region of HRV2/L reveals three amino acid changes in 2B and two in 2C (Fig. 7). Whether or not these changes are responsible for the adaptation phenotype has not been determined. Notably, one substitution in 2B and one in 2C of HRV2/L are adjacent to amino acid alterations in 16/L. This observation suggests that the changes in HRV2/L are important for growth in mouse cells. Although we did not find a definitive role for the 2B change in adaptation of HRV16 to mouse cells, the presence of a change at the adjacent residue of HRV2/L suggests that it may serve an as-yet-unidentified function.
The findings reported here demonstrate that adaptation of rhinovirus to mouse cells is caused by amino acid changes in 2BC. This multifunctional protein influences membrane vesicle trafficking, membrane permeability, and viral RNA replication. Despite the numerous roles attributed to 2BC in infected cells, mechanistic details have not been revealed. An explanation of the functional basis for the adaptation phenotype will require an understanding of the mechanism of action of protein 2BC. Identification of cellular partners of 2BC and the study of how such protein-protein interactions direct its function will advance our understanding of viral replication and pathogenesis.
Acknowledgments
This work was supported by Public Health Service grant AI50754 from the National Institute of Allergy and Infectious Diseases.
We thank Wai-Ming Lee, University of Wisconsin, Madison, for an infectious DNA clone of HRV16; Bert Semler, University of California, Irvine, for an infectious DNA clone of HRV14; and the University of Newcastle for an ICAM-1 DNA clone.
REFERENCES
- 1.Agirre, A., A. Barco, L. Carrasco, and J. Nieva. 2002. Viroporin-mediated membrane permeabilization. J. Biol. Chem. 277:40434-40441. [DOI] [PubMed] [Google Scholar]
- 2.Aldabe, R., A. Barco, and L. Carrasco. 1996. Membrane permeabilization by poliovirus proteins 2B and 2BC. J. Biol. Chem. 271:23134-23137. [DOI] [PubMed] [Google Scholar]
- 3.Aldabe, R., and L. Carrasco. 1995. Induction of membrane proliferation by poliovirus proteins 2C and 2BC. Biochem. Biophys. Res. Commun. 206:64-76. [DOI] [PubMed] [Google Scholar]
- 4.Banerjee, R., A. Echeverri, and A. Dasgupta. 1997. Poliovirus-encoded 2C polypeptide specifically binds to the 3′-terminal sequences of viral negative-strand RNA. J. Virol. 71:9570-9578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Barco, A., and L. Carrasco. 1995. A human virus protein, poliovirus protein 2BC, induces membrane proliferation and blocks the exocytic pathway in the yeast Saccharomyces cerevisiae. EMBO J. 14:3349-3364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Barco, A., and L. Carrasco. 1998. Identification of regions of poliovirus 2BC protein that are involved in cytotoxicity. J. Virol. 72:3560-3570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Barton, D. J., E. P. Black, and J. B. Flanegan. 1995. Complete replication of poliovirus in vitro: preinitiation RNA replication complexes require soluble cellular factors for the synthesis of VPg-linked RNA. J. Virol. 69:5516-5527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Barton, D. J., and J. B. Flanegan. 1997. Synchronous replication of poliovirus RNA: initiation of negative-strand RNA synthesis requires the guanidine-inhibited activity of protein 2C. J. Virol. 71:8482-8489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bertino, J. S. 2002. Cost burden of viral respiratory infections: issues for formulary decision makers. Am. J. Med. 112(Suppl. 6A):42S-49S. [DOI] [PubMed]
- 10.Bienz, K., D. Egger, T. Pfister, and M. Troxler. 1992. Structural and functional characterization of the poliovirus replication complex. J. Virol. 66:2740-2747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bienz, K., D. Egger, M. Troxler, and L. Pasamontes. 1990. Structural organization of poliovirus RNA replication is mediated by viral proteins of the P2 genomic region. J. Virol. 64:1156-1163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cho, M. W., N. Teterina, D. Egger, K. Bienz, and E. Ehrenfeld. 1994. Membrane rearrangement and vesicle induction by recombinant poliovirus 2C and 2BC in human cells. Virology 202:129-145. [DOI] [PubMed] [Google Scholar]
- 13.Cuconati, A., W. Xiang, F. Lahser, T. Pfister, and E. Wimmer. 1998. A protein linkage map of the P2 nonstructural proteins of poliovirus. J. Virol. 72:1297-1307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.de Jong, A., E. Wessels, H. Dijkman, J. Galama, W. Melchers, H. Willems, and F. van Kuppeveld. 2003. Determinants for membrane association and permeabilization of the coxsackievirus 2B protein and the identification of the Golgi complex as the target organelle. J. Biol. Chem. 278:1012-1021. [DOI] [PubMed]
- 15.de Jong, A. S., I. W. Schrama, P. H. Willems, J. M. Galama, W. J. Melchers, and F. J. van Kuppeveld. 2002. Multimerization reactions of coxsackievirus proteins 2B, 2C, and 2BC: a mammalian two-hybrid analysis. J. Gen. Virol. 83:783-793. [DOI] [PubMed] [Google Scholar]
- 16.Doedens, J. R., and K. Kirkegaard. 1995. Inhibition of cellular protein secretion by poliovirus proteins 2B and 3A. EMBO J. 14:894-907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Echeverri, A., R. Banerjee, and A. Dasgupta. 1998. Amino-terminal region of poliovirus 2C protein is sufficient for membrane binding. Virus Res. 54:217-223. [DOI] [PubMed] [Google Scholar]
- 18.Echeverri, A. C., and A. Dasgupta. 1995. Amino terminal regions of poliovirus 2C protein mediate membrane binding. Virology 208:540-553. [DOI] [PubMed] [Google Scholar]
- 19.Gern, J. E. 2002. Rhinovirus respiratory infections and asthma. Am. J. Med. 112(Suppl. 6A):19S-27S. [DOI] [PubMed]
- 20.Hall, L., and R. R. Rueckert. 1971. Infection of mouse fibroblasts by cardioviruses: premature uncoating and its prevention by elevated pH and magnesium chloride. Virology 43:152-165. [DOI] [PubMed] [Google Scholar]
- 21.Jecht, M., C. Probst, and V. Gauss-Muller. 1998. Membrane permeability induced by hepatitis A virus proteins 2B and 2BC and proteolytic processing of HAV 2BC. Virology 252:218-227. [DOI] [PubMed] [Google Scholar]
- 22.Johnston, S. L., P. K. Pattemore, G. Sanderson, S. Smith, F. Lampe, L. Josephs, P. Symington, S. O'Toole, S. H. Myint, D. A. Tyrrell, et al. 1995. Community study of role of viral infections in exacerbations of asthma in 9-11 year old children. BMJ 310:1225-1229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Li, J. P., and D. Baltimore. 1990. An intragenic revertant of a poliovirus 2C mutant has an uncoating defect. J. Virol. 64:1102-1107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Li, J. P., and D. Baltimore. 1988. Isolation of poliovirus 2C mutants defective in viral RNA synthesis. J. Virol. 62:4016-4021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lomax, N. B., and F. H. Yin. 1989. Evidence for the role of the P2 protein of human rhinovirus in its host range change. J. Virol. 63:2396-2399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.McIntosh, K. 1999. Closer to a cure for the common cold? JAMA 281:1844-1845. [DOI] [PubMed] [Google Scholar]
- 27.Mirzayan, C., and E. Wimmer. 1992. Genetic analysis of an NTP-binding motif in poliovirus polypeptide 2C. Virology 189:547-555. [DOI] [PubMed] [Google Scholar]
- 28.Nicholson, K. G., J. Kent, and D. C. Ireland. 1993. Respiratory viruses and exacerbations of asthma in adults. BMJ 307:982-986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ong, E. L., M. E. Ellis, A. K. Webb, K. R. Neal, M. Dodd, E. O. Caul, and S. Burgess. 1989. Infective respiratory exacerbations in young adults with cystic fibrosis: role of viruses and atypical microorganisms. Thorax 44:739-742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Pfister, T., and E. Wimmer. 1999. Characterization of the nucleoside triphosphatase activity of poliovirus protein 2C reveals a mechanism by which guanidine inhibits poliovirus replication. J. Biol. Chem. 274:6992-7001. [DOI] [PubMed] [Google Scholar]
- 31.Pincus, S. E., and E. Wimmer. 1986. Production of guanidine-resistant and -dependent poliovirus mutants from cloned cDNA: mutations in polypeptide 2C are directly responsible for altered guanidine sensitivity. J. Virol. 60:793-796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Pitkaranta, A., and F. G. Hayden. 1998. Rhinoviruses: important respiratory pathogens. Ann. Med. 30:529-537. [DOI] [PubMed] [Google Scholar]
- 33.Pribble, C. G., P. G. Black, J. A. Bosso, and R. B. Turner. 1990. Clinical manifestations of exacerbations of cystic fibrosis associated with nonbacterial infections. J. Pediatr. 117:200-204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Reithmayer, M., A. Reischl, L. Snyers, and D. Blaas. 2002. Species-specific receptor recognition by a minor-group human rhinovirus (HRV): HRV serotype 1A distinguishes between the murine and the human low-density lipoprotein receptor. J. Virol. 76:6957-6965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Rodriguez, P. L., and L. Carrasco. 1995. Poliovirus protein 2C contains two regions involved in RNA binding activity. J. Biol. Chem. 270:10105-10112. [DOI] [PubMed] [Google Scholar]
- 36.Rodriguez, P. L., and L. Carrasco. 1993. Poliovirus protein 2C has ATPase and GTPase activities. J. Biol. Chem. 268:8105-8110. [PubMed] [Google Scholar]
- 37.Rotbart, H. 1999. Medical impact of rhinovirus, p. 12. Annual report. Biota, Inc., Melbourne, Australia.
- 38.Rust, R. C., L. Landmann, R. Gosert, B. L. Tang, W. Hong, H. P. Hauri, D. Egger, and K. Bienz. 2001. Cellular COPII proteins are involved in production of the vesicles that form the poliovirus replication complex. J. Virol. 75:9808-9818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Schlegel, A., T. H. Giddings, Jr., M. S. Ladinsky, and K. Kirkegaard. 1996. Cellular origin and ultrastructure of membranes induced during poliovirus infection. J. Virol. 70:6576-6588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Smith, M. B., and W. Feldman. 1993. Over-the-counter cold medications: a critical review of clinical trials between 1950 and 1991. JAMA 269:2258-2263. [DOI] [PubMed] [Google Scholar]
- 41.Stockl, J., H. Vetr, O. Majdic, G. Zlabinger, E. Kuechler, and W. Knapp. 1999. Human major group rhinoviruses downmodulate the accessory function of monocytes by inducing IL-10. J. Clin. Investig. 104:957-965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Suhy, D. A., T. H. Giddings, Jr., and K. Kirkegaard. 2000. Remodeling the endoplasmic reticulum by poliovirus infection and by individual viral proteins: an autophagy-like origin for virus-induced vesicles. J. Virol. 74:8953-8965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Summers, D. F., and J. V. Maizel, Jr. 1968. Evidence for large precursor proteins in poliovirus synthesis. Proc. Natl. Acad. Sci. USA 59:966-971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Teterina, N. L., A. E. Gorbalenya, D. Egger, K. Bienz, and E. Ehrenfeld. 1997. Poliovirus 2C protein determinants of membrane binding and rearrangements in mammalian cells. J. Virol. 71:8962-8972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Tolskaya, E. A., L. I. Romanova, M. S. Kolesnikova, A. P. Gmyl, A. E. Gorbalenya, and V. I. Agol. 1994. Genetic studies on the poliovirus 2C protein, an NTPase: a plausible mechanism of guanidine effect on the 2C function and evidence for the importance of 2C oligomerization. J. Mol. Biol. 236:1310-1323. [DOI] [PubMed] [Google Scholar]
- 46.van Kuppeveld, F. J., J. G. Hoenderop, R. L. Smeets, P. H. Willems, H. B. Dijkman, J. M. Galama, and W. J. Melchers. 1997. Coxsackievirus protein 2B modifies endoplasmic reticulum membrane and plasma membrane permeability and facilitates virus release. EMBO J. 16:3519-3532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.van Kuppeveld, F. J., W. J. Melchers, P. H. Willems, and T. W. Gadella, Jr. 2002. Homomultimerization of the coxsackievirus 2B protein in living cells visualized by fluorescence resonance energy transfer microscopy. J. Virol. 76:9446-9456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Vance, L. M., N. Moscufo, M. Chow, and B. A. Heinz. 1997. Poliovirus 2C region functions during encapsidation of viral RNA. J. Virol. 71:8759-8765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ward, M. A. 2002. Emergency department management of acute respiratory infections. Semin. Respir. Infect. 17:65-71. [DOI] [PubMed] [Google Scholar]
- 50.Yin, F. H., and N. B. Lomax. 1986. Establishment of a mouse model for human rhinovirus infection. J. Gen. Virol. 67(Pt. 11):2335-2340. [DOI] [PubMed] [Google Scholar]
- 51.Yin, F. H., and N. B. Lomax. 1983. Host range mutants of human rhinovirus in which nonstructural proteins are altered. J. Virol. 48:410-418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Zhu, Z., W. Tang, J. M. Gwaltney, Jr., Y. Wu, and J. A. Elias. 1997. Rhinovirus stimulation of interleukin-8 in vivo and in vitro: role of NF-κB. Am. J. Physiol. 273:L814-L824. [DOI] [PubMed] [Google Scholar]