Abstract
Objectives. Although local-level chronic disease and risk factor data are not typically available, they are valuable for guiding public health interventions and policies. To present a case for disaggregated community-level health data, we conducted a study exploring the relevance of such data to research on health disparities.
Methods. We designed a population-based health survey to gather information on many health measures, 13 of which are presented here. Interviews were conducted with 1699 adults (18–75 years) in 6 Chicago community areas between September 2002 and April 2003.
Results. Statistically significant variations in health measures were found between the 6 communities themselves (108 of 195 pairwise comparisons were significant) and between the communities and Chicago as a whole (35 of 54 comparisons were significant).
Conclusions. The local-level variations in health revealed in this study emphasize that geographic and racial/ethnic health disparities are still prominent in Chicago and shed light on the limitations of existing city- and regional-level data.
Until recently, local-level public health data have not been routinely collected and thus are not readily avalable. Existing data that can be geocoded to the county, city, or community level are derived from traditional surveillance systems (e.g., vital records and communicable disease registries), and provide information on small-area trends and variances in mortality,2,3 measures related to birth outcomes,4 and infectious diseases.5 However, they offer little local information on the determinants of morbidity and mortality.6,7 Such information is derived from health surveys, often conducted at the national (e.g., National Health Interview Survey [NHIS]) and state (e.g., Behavioral Risk Factor Surveillance System [BRFSS]) levels. Although these data are essential in terms of national public health policies and health monitoring, they are typically not available at the local level.
Social epidemiologists and public health practitioners have responded to this growing need for local health data.8–10 For instance, Northridge et al., gathering data at the local level, found that the smoking prevalence rate in Harlem (42%) was notably different from the rate in New York State as a whole (25%) and the rate among non-Hispanic Blacks residing in the state (25%).11 Others have conducted health surveys designed to gather these important data at the county (e.g., Los Angeles County Health Survey12 and Seattle–King County Survey13), city (e.g., New York City Health and Nutrition Examination Survey14), and community or neighborhood (e.g., New York City health disparities report15 and New York City Community Health Survey16) levels. Even the Centers for Disease Control and Prevention, which conducts state-based health surveys (i.e., BRFSS surveys), has recognized the importance of local-level data, designing the Selected Metropolitan/Micropolitan Area Risk Trends Project to mathematically estimate health-related prevalence proportions in smaller geographic areas.17,18
As urban settings become increasingly diverse and certain populations are disproportionately affected by disease,19,20 variations in the health status of these smaller geographic areas may be substantial,2 and such variations must be considered if true advances in disease prevention and control are to be achieved.8–10,21–23 To explore such differences, we conducted a household survey in 6 diverse communities of Chicago to examine health profile differences.
METHODS
Community Areas
Chicago is divided into 77 officially designated community areas that are often used as a basis for describing the city’s health conditions, delivering health care services, and implementing community-based interventions.24 Figure 1 ▶ shows the 6 community areas selected for this survey, and Table 1 ▶ presents some of their demographic and socioeconomic characteristics.
FIGURE 1—
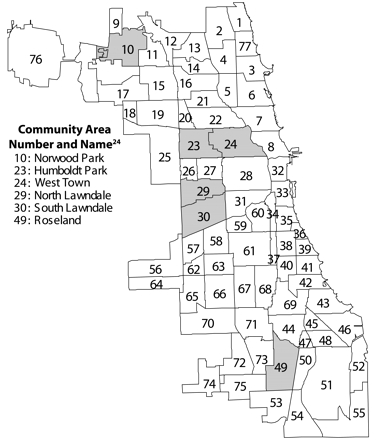
Six of Chicago’s 77 community areas.
TABLE 1—
Demographic Characteristics of 6 Chicago Community Areas Compared With Chicago Overall and the United States: Improving Community Health Survey, 2002–2003
| Humboldt Park | North Lawndale | Norwood Park | Roseland | South Lawndale | West Town | Chicago | United States | |
| Total population | 65 836 | 41 768 | 37 669 | 52 723 | 91 071 | 87 435 | 2 896 016 | 281 421 906 |
| Race/ethnicity, % | ||||||||
| Non-Hispanic Black | 47 | 94 | 1 | 98 | 13 | 9 | 36 | 12 |
| Non-Hispanic White | 3 | 1 | 88 | 1 | 4 | 39 | 31 | 69 |
| Hispanic | 48 | 5 | 6 | 1 | 83 | 47 | 26 | 13 |
| Mexican | 24 | 3 | 3 | 0 | 76 | 25 | 18 | 7 |
| Puerto Rican | 18 | 0 | 0 | 0 | 1 | 16 | 4 | 1 |
| Median household income, $ | 28 728 | 18 342 | 53 402 | 38 237 | 32 320 | 38 915 | 38 625 | 41 994 |
| High-school diploma, %a | 50 | 60 | 83 | 77 | 37 | 70 | 72 | 80 |
| Unemployment rate, %b | 18 | 26 | 3 | 17 | 12 | 7 | 10 | 6 |
| Individual poverty rate, %c | 31 | 45 | 4 | 18 | 27 | 21 | 20 | 12 |
Note. Data for Chicago and the United States were derived from the 2000 census.
aAmong those 25 years or older.
b Percentage of resident civilians older than 16 years who did not have a job and were actively seeking work.
cPercentage of residents with annual incomes below the federally defined poverty level in 1999.
We selected these community areas for various social and political reasons, but our primary interest was their role in shaping local policies and developing community interventions. We selected North Lawndale and South Lawndale because we are affiliated with the Sinai Health System, which serves these communities (Figure 1 ▶). The population of North Lawndale is almost entirely Black, and the median household income is $18 000; South Lawndale is predominantly Mexican, with a median household income of $32 000.
The contiguous communities of West Town and Humboldt Park, located west of downtown Chicago, are interesting in an epidemiological sense in that they are both facing transitions related to urban development. In addition, they are home to energetic and dedicated community-based organizations that were eager to use the data gathered here to implement changes. The population of West Town is one-half White, one-quarter Mexican, and one-quarter Puerto Rican, whereas that of Humboldt Park is one-half Black, one-quarter Mexican, and one-quarter Puerto Rican. Finally, we selected Roseland, a predominantly Black community on the south side, and Norwood Park, a predominantly White community on the north side, because they represented 2 geographically and racially disparate communities.
According to 2000 US census data, median household incomes in the 6 study communities ranged from $18000 to $53 000, compared with $39000 for Chicago and $42 000 for the United States as a whole. Overall, the communities were reflective of different geographic areas but were not selected to be representative of the city of Chicago.
Sample
The sample was composed of adults living in households situated in each of the 6 community areas. We employed a 3-stage probability sampling design to ensure community representation.25 First, we selected 15 census blocks from each community area using probability proportional to size sampling,26 meaning that the blocks in each community area were selected in a manner proportionate to the number of individuals 18 years or older who lived on these blocks according to the 2000 US census. Second, we randomly selected households from each block. Third, a screener enumerated all household members and identified a random adult respondent using the Troldahl–Carter–Bryant methodology.27 Eligibility was limited to selected individuals between the ages of 18 and 75 years who resided in one of the targeted community areas, were physically and mentally able to answer the interview questions in English or Spanish, and provided consent to participate.
Survey Instrument
Data were obtained from the Sinai Health System’s Improving Community Health Survey, which was developed by a survey design committee composed of 6 representatives of community-based organizations from the participating community areas, 3 representatives of local Chicago health agencies, and 4 representatives of the Sinai Health System. The committee met every other week from January through March 2002 to develop the survey. The survey instrument then underwent extensive review and pretesting between April and August 2002. Topics and primary research questions were selected according to the needs and interests of community representatives. Whenever possible, questions were worded in a manner identical to questions used in existing health surveys (e.g., BRFSS, NHIS) so that appropriate comparison data would be available.
A certified translator translated the instrument and all supporting materials into Spanish. When available, translated questions from existing health surveys were used. Appropriate modifications of the Spanish instrument were made as a result of cognitive interviews in Spanish and pretest interviews conducted with native Spanish speakers to ensure accurate comprehension of the translated questions. After several iterations over a 5-month period, the final adult instrument was reviewed and approved by the survey design committee and a questionnaire review committee from the Survey Research Laboratory at the University of Illinois at Chicago, the organization subcontracted to implement the survey.
Data Collection
The survey was administered face to face in respondents’ homes from September 2002 through April 2003. Interviewers were hired and trained by the Survey Research Laboratory, which has been involved in conducting a number of such household surveys. Interviewers were either members of or culturally familiar with the communities surveyed. Interviewers underwent 21 hours of formal training, and roughly one third were native Spanish speakers or bilingual.
Community leaders from the survey design committee sent an advance letter to households selected for the survey. Interviewers made at least 12 attempts to screen and interview the randomly selected adult from each household at different times of the day and different days of the week. Most (85%) of the interviews, which were approximately 1 hour in duration, were conducted during evening and weekend hours. Interviewees received a health information packet (in Spanish or English) along with $40 for their time.
The survey was administered via computer-assisted personal interviewing techniques to reduce the potential for errors related to data entry or skip patterns. Ten percent of each interviewer’s work was validated at random for quality assurance purposes. The goal of conducting at least 300 face-to-face interviews in each community area was met in 5 of the 6 communities. Only 190 interviews were completed in Norwood Park, the predominantly White community area with the highest median household income.
Response Rate
Interviews were attempted at 4888 households. Of the original list of addresses derived from census data, only 89.5% were occupied. We were able to make contact in the case of 76.3% of these households, and 76.5% of households successfully contacted cooperated with the screening. A total of 1953 eligible individuals were contacted, of whom 1699 (87%) agreed to participate and completed the survey.
The overall response rate, based on a conservative calculation procedure outlined by the American Association for Public Opinion Research,28 was 43.2%. In this procedure, all originally sampled buildings and households were included in the denominator.29 That is, unoccupied housing, households that no longer existed, and households where interviewers were not able to locate residents were included, in addition to individuals who refused to participate.
Measures
The Sinai Improving Community Health Survey adult module contained 469 questions focusing on various health conditions and risk factors. Whenever possible, questions were worded exactly as they are in BRFSS surveys to facilitate comparisons with Chicago and national data. The 13 measures analyzed for this study focused on health conditions, health behaviors, and health care access.
Health conditions.
We asked respondents whether they had ever been diagnosed with high blood pressure, arthritis, asthma, depression, or diabetes by a doctor, nurse, or other health professional. In addition, as a means of determining the prevalence of obesity within each community, we used individuals’ self-reported height and weight to calculate their body mass index.
Health behaviors.
We also asked about physical activity and smoking. Respondents were asked how many times a week they engaged in moderate activities for at least 30 minutes at a time. We calculated the percentages who engaged in such activities at least 5 times a week (in accord with the guidelines of the Centers for Disease Control and Prevention). Consistent with the Chicago BRFSS survey, we defined current smokers as those who responded yes to the questions “Have you smoked at least 100 cigarettes in your entire life?” and “Do you currently smoke cigarettes?”
Health care access.
We asked a series of questions designed to determine health care coverage and access to health care services. Respondents were asked whether they currently had any type of health insurance or medical coverage. Also, they were asked whether, at any point during the preceding 12 months, they needed but did not obtain dental care because they could not afford it. They were asked the same question about prescription medications. Both of these latter questions were identical to questions asked in the NHIS.
In addition, we asked about cancer screening. Women were asked “Have you ever had a mammogram or breast x-ray?” and “How long has it been since you had your last mammogram?” We analyzed the proportion of women age 40 years or older who had a mammogram in the past year. Also, all respondents were asked “Have you ever had a sigmoidoscopy or colonoscopy?” and “How long ago did you have one of these tests?” We assessed the percentages of adults 50 years or older who had undergone one of these tests.
Statistical Analysis
The 2000 US population was used as the standard in directly age-adjusting health condition prevalence proportions to be consistent with comparison data. The sampling weights used in our analysis accounted for differential probabilities of selection and post-stratification so that the sample would resemble the distribution of each community area’s population according to the 2000 census. For each measure, we assessed differences in community area pairwise prevalence rates using z tests for proportions. We examined 15 comparisons for each measure (e.g., South Lawndale vs North Lawndale, South Lawndale vs Norwood Park) in terms of their statistical significance.
In addition, we compared prevalence rates for each community area measure with rates for Chicago as a whole and evaluated statistical significance at the .05 α level. Although we conducted a number of significance tests, we did not adjust the overall significance level (e.g., via a Bonferroni inequality calculation) because we viewed this analysis as exploratory and did not examine any formal hypotheses regarding community differences. We analyzed the data using Stata, version 8.0, to account for sampling design effects.30
RESULTS
Table 2 ▶ presents the data for the 13 health conditions, health behaviors, and health care access measures assessed in our analyses. Most of the differences in these measures between the community areas themselves and between the community areas and Chicago as a whole were statistically significant. For example, the percentage of people reporting that they had been diagnosed with high blood pressure ranged from 17% in South Lawndale to 41% in North Lawndale, and 13 of the 15 pairwise comparisons made between the different community areas were statistically significant. Furthermore, high blood pressure prevalence rates in 5 of the 6 community areas were statistically different from the overall Chicago rate of 23%.
TABLE 2—
Prevalence of Selected Health Conditions, Health Behaviors, and Measures of Health Care Access Among Adults in 6 Chicago Community Areas, 2002–2003
| Prevalence (95% CI) | ||||||||
| No. of Significant Pairwise Comparisonsa | Humboldt Park | North Lawndale | Norwood Park | Roseland | South Lawndale | West Town | Chicago | |
| Health conditions | ||||||||
| High blood pressure | 13 | 35b (32.6, 37.2) | 41b (37.8, 44.6) | 26 (23.6, 28.6) | 39b (36.2, 40.7) | 17b (12.7, 20.5) | 28b (24.7, 31.2) | 23 (20.6, 25.2) |
| Arthritis | 9 | 23 (20.0, 25.8) | 25b (22.6, 26.8) | 18 (16.1, 19.8) | 25b (22.4, 26.8) | 10b (7.8, 11.2) | 27b (24.0, 29.6) | 20 (17.9, 21.7) |
| Asthma | 11 | 17b (14.8, 19.3) | 18b (15.7, 19.9) | 12 (10.4, 14.3) | 13 (10.8, 15.1) | 1b (0.6, 1.2) | 21b (17.9, 23.4) | 11 (10.2, 12.4) |
| Depression | 12 | 21 (18.8, 22.6) | 15 (13.2, 17.1) | 9 (7.2, 9.8) | 13 (11.1, 13.9) | 21 (18.1, 23.3) | 23 (19.9, 26.6) | . . . |
| Diabetes | 11 | 16b (13.3, 18.5) | 10b (8.1, 12.4) | 4b (3.5, 5.2) | 12b (10.0, 13.1) | 6 (3.8, 7.3) | 14b (11.4, 16.0) | 7 (6.6, 8.4) |
| Obese (body mass index ≥ 30 kg/m2) | 9 | 36b (33.3, 39.5) | 41b (37.6, 44.9) | 20 (18.3, 22.6) | 38b (35.5, 40.3) | 37b (31.3, 42.8) | 31b (27.4, 34.8) | 22 (20.0, 23.2) |
| Health behaviors | ||||||||
| Engages in 30 min of moderate activity 5 times per week | 7 | 34 (28.9, 38.8) | 30 (26.0, 33.6) | 30 (22.3, 37.4) | 27 (22.6, 31.0) | 15b (7.7, 21.6) | 36 (30.1, 41.4) | 30 (25.4, 35.7) |
| Current smoker | 8 | 35b (26.8, 43.4) | 39b (33.7, 44.8) | 18b (15.7, 21.2) | 33b (24.9, 41.6) | 20 (15.0, 25.3) | 32b (25.4, 38.1) | 24 (21.6, 28.9) |
| Health care access | ||||||||
| Currently insured (adults 18–64 y) | 11 | 61b (53.6, 69.1) | 61b (52.0, 69.1) | 93b (88.7, 97.5) | 70 (62.6, 76.9) | 46b (30.2, 61.0) | 73 (68.4, 77.9) | 73 (69.6, 77.4) |
| Did not obtain needed dental care in past year | 5 | 33 (29.5, 36.5) | 28 (21.8, 34.8) | 9 (6.4, 12.0) | 30 (21.8, 39.2) | 25 (13.1, 36.5) | 34 (26.4, 41.4) | . . . |
| Did not obtain needed prescription medications in past year | 9 | 23 (18.7, 27.1) | 24 (18.2, 29.9) | 4 (2.2, 6.2) | 15 (9.2, 20.9) | 12 (7.1, 16.5) | 18 (11.9, 23.8) | . . . |
| Mammogram in past year (women ≥ 40 y) | 3 | 56 (35.2, 76.1) | 65 (52.9, 76.6) | 65 (52.6, 77.9) | 61 (52.2, 69.7) | 38b (28.2, 47.5) | 47b (31.4, 63.5) | 67 (46.6, 74.0) |
| Colonoscopy/Sigmoidoscopy in past year (adults ≥ 50 y) | 0 | 16 (7.2, 25.1) | 13 (4.8, 20.8) | 18 (9.1, 27.2) | 25 (12.6, 36.6) | 14 (0.0, 27.8) | 16 (5.2, 27.4) | . . . |
Note. CI = confidence interval. Pairwise comparisons were made between community areas themselves and between community areas and Chicago as a whole. Health conditions prevalence data were age-adjusted to the 2000 census standard population.
aOut of a possible 15 between-community comparisons.
bSignificantly different (P < .05) from overall Chicago rate.
In a similar manner, and consistent with data on insurance coverage, Norwood Park residents were more likely than residents of other communities to obtain needed dental care and prescription medicines. Only 9% of these individuals, compared with 34% in West Town and 33% in Humboldt Park, had not obtained needed dental care in the previous 12 months because they could not afford it. Of the 15 pairwise comparisons made for this measure, 5 were statistically significant.
Similarly, 4% of Norwood Park residents, compared with 24% of North Lawndale and 23% of Humboldt Park residents, had not obtained needed prescription medicines in the previous 12 months because they could not afford them. In this case, 9 of 15 pairwise comparisons were significant. Chicago data were not available for either of these variables.
Of the total of 195 tests (15 pairwise comparisons for each of the 13 measures) examining differences between measures, 108 were statistically significant (10 would have expected by chance alone from the unadjusted significance levels used). Finally, of the 54 tests (9 measures with available Chicago data for each of the 6 community areas) involving comparisons with Chicago data, 35 were significant (3 would have been expected by chance).
DISCUSSION
The overarching question addressed in this analysis was whether there were substantial variations in the health measures assessed between the community areas themselves and between the community areas and Chicago as a whole. Our data indicate that considerable variations existed in both instances. However, it should be noted that our analyses were exploratory and that the sample size was not selected to detect a particular effect size. As such, it is possible that any differences we have described here as statistically significant may not be meaningful or important, but it is also possible that meaningful or important differences did not reach the level of statistical significance. The variations identified demonstrate that existing national and even state surveys may not reflect the health conditions of local (often diverse) communities and suggest that available Chicago data may be inadequate in terms of representing the health of the city’s 77 community areas.
Previous analyses of vital statistics and communicable disease registry data have revealed considerable variations in health among these Chicago communities as well.3 Our survey data supplement such information and further identify substantial differences in the current status and determinants of health among these populations. For instance, North Lawndale and South Lawndale are adjacent to one another, yet they have very different health profiles. To consider just 1 measure, 39% of the former community’s residents are smokers, compared with only 20% of those of the latter community. If data are examined in an aggregated fashion, contextual differences in the demographic and health profiles of specific communities will not be identified, leading to difficulties in identifying and mounting effective community-based public health and public policy programs.
Another example of the importance of community-level data can be found in comparisons of North Lawndale and Roseland. Although both are composed virtually entirely of African American residents, Roseland has a much higher median household income level ($38000), one that is similar to Chicago and national levels. North Lawndale’s median household income ($18000), in contrast, makes it one of the poorest of Chicago’s 77 community areas. Despite this substantial economic difference, Roseland’s residents exhibited statistically significant advantages on only 4 of the 13 health measures assessed in this study (asthma, depression, insurance, and access to prescription medicines). These similarities, as opposed to the much larger differences that one might expect on the basis of the 2 communities’ median household incomes, raise important questions about the relation between race and class.31–35 Again, such a provocative finding can be obtained only through disaggregation of data at the community level.
Although it is one of the largest cities in the United States and its population is diverse, Chicago—labeled in a seminal study as “hypersegregated”36 (i.e., segregated on many dimensions simultaneously)—has proven to be an ideal setting for small area studies. A strength of this study is that some of the community areas assessed were homogeneous, lending valuable information to assessments of racial and ethnic health disparities. In fact, recent reports37,38 based on health status indicators drawn solely from vital records and communicable disease registries have demonstrated substantial and even increasing Black–White disparities at the city level in Chicago. Our study adds to a more general picture of the city’s health conditions in that we examined disparities at the community area level and analyzed health measures not available in existing databases. The kinds of disaggregated data used in our investigation are necessary to fully appreciate and ultimately remedy disparities in communities such as those assessed here.
Although it is not surprising that individuals of lower socioeconomic status fare worse than those in better financial situations in terms of health measures, the extent of such inequities has rarely been documented. Researchers can use the present local-level data to continue to investigate how people’s place of residence may affect their health,39,40 how socioeconomic factors correlate with health risk factors,41 and how self-reported survey data combined with analyses of existing birth and death certificates can provide in-depth profiles of community health conditions.2,3,5,42,43
Methodological Considerations
It must be emphasized that the pairwise comparisons described in this article were not corrected for the multiple tests that were conducted, and overall significance may have been compromised. Thus, our results should be viewed as exploratory. In addition, implementing a survey such as this one, in some of Chicago’s most disenfranchised communities, presented significant challenges. For example, many of the randomly selected households no longer existed when interviewers returned after field enumeration and initial block listing. The large numbers of vacant lots and empty homes in low-income communities, along with the number of homes in which no one answered the door after repeated attempts by the interviewers, may have contributed to the relatively low response rate of 43%.
Also, there was notable variation in participation rates according to community area. In North Lawndale, the poorest of the areas assessed, the occupancy rate (percentage of occupied households) was 85%, whereas the refusal rate was 10%. In Norwood Park, the richest area assessed, the occupancy rate was 98% and the refusal rate was 35%. Thus, although many houses (about 15%) in North Lawndale were vacant or burned down, 90% of the potential participants located completed the survey. In Norwood Park, conversely, although most of the housing units were occupied, only 65% of those contacted agreed to participate in the survey. This was also one of the main reasons why we completed only 190 surveys in Norwood Park instead of the goal of 300. Our difficulties in this community were consistent with reports from the 2000 census, according to which Chicago’s more affluent communities had the highest refusal rates in the city.
Overall, 87% of the eligible respondents we were able to contact agreed to participate in and complete the survey. Factors that may have contributed to this relatively high participation rate included the $40 incentive offered, the partnerships established with community-based organizations, and the persistence of interviewers who, before defining a household as “nonresponding,” visited that household at least 12 times.
Overall, the demographic characteristics of the respondents (in terms of gender, age, and race/ethnicity) closely reflected the characteristics of their respective census blocks. Studies have shown that the health status of survey nonrespondents is usually worse than that of respondents.44,45 If this is the case, then our results for health conditions may represent underestimates, whereas our health access results may represent overestimates. It is unclear precisely how our response rate affected our findings, but this is one of the challenges presented by all population-based surveys.
Financial Considerations
Another consideration in conducting a survey such as this one is cost. How many of these communities could be regularly surveyed, and at what expense? Such issues will vary from city to city and state to state. The present survey cost approximately $60000 per community area to obtain a sample size that resulted in about 300 completed surveys. Not included in the cost were determining the appropriate questions to be asked, constructing the questionnaire, and analyzing the data. Whether such surveys are cost effective, and where funds might be found to support them, are political rather than epidemiological questions. However, notwithstanding the high value of local data, not every community needs a survey each year. Local health departments or health researchers may decide that communities or other small geographic areas could be satisfactorily surveyed once every 5 years, for example. Also, some communities may be so homogeneous that several could be combined into a single sampling unit.
Implications for Future Research
Variations in health measures identified at the local level shed light on the limitations of the existing city data often used in establishing public health policies and monitoring population health. The local-level information on these Chicago communities described here has never before been collected; however, such data are essential in identifying communities most at risk of poor health outcomes, exploring the determinants of such variations in health, and ultimately guiding community health programs and policies.10,22,23,46
With community area prevalence and risk factor data available, these Chicago communities are at a considerable advantage in developing effective community-based initiatives designed to improve the health of their residents. For instance, setting priorities and planning for improved health in South Lawndale may involve ensuring access to health care services, whereas in Humboldt Park the focus may be on diabetes outreach and management. In fact, survey findings have already been successful in guiding local foundations to invest in programs related to arthritis, weight loss, and asthma management in these Chicago communities.47
Finally, our findings can inform policymakers, community leaders, and researchers in their efforts to advocate for equitable distribution of resources, particularly in the context of widening health disparities in Chicago37,38 and other similar urban centers and in achieving Healthy People 2010 goals.48 Our survey data document, emphasize, and reinforce the fact that geographic and racial/ethnic health disparities are still prominent in Chicago, and thus, they offer opportunities for action and development of effective interventions and policies at the local level.
Acknowledgments
Generous funding for this project was provided by the Robert Wood Johnson Foundation (grant 043026) and the Chicago Community Trust (grant C2003-00844).
This project would not have been possible without the support, time, and dedication of the epidemiologists and researchers at the Sinai Urban Health Institute.
Human Participant Protection This study was approved by the institutional review boards of the Sinai Health System and the University of Illinois at Chicago. All participants provided written informed consent.
Peer Reviewed
Contributors A. M. Shah synthesized the analyses and led the writing. S. Whitman originated the study and supervised all aspects of its implementation. A. Silva completed the statistical analyses. All of the authors helped to conceptualize ideas, interpret findings, and review drafts of the article.
References
- 1.Shaping a Health Statistics Vision for the 21st Century. Washington, DC: US Dept of Health and Human Services; 2002.
- 2.Fang J, Bosworth W, Madhavan S, Cohen H, Alderman MH. Differential mortality in New York City (1988–1992), part two: excess mortality in the South Bronx. Bull N Y Acad Med. 1995;72:483–499. [PMC free article] [PubMed] [Google Scholar]
- 3.Whitman S, Silva A, Shah A, Ansell D. Diversity and disparity: GIS and small area analysis in six Chicago neighborhoods. J Med Syst. 2004;28:397–411. [DOI] [PubMed] [Google Scholar]
- 4.Krieger N, Chen JT, Waterman PD, Soobader MJ, Subramanian SV, Carson R. Choosing area based socioeconomic measures to monitor social inequalities in low birthweight and childhood lead poisoning: the Public Health Disparities Geocoding Project (US). J Epidemiol Community Health. 2003;57:186–199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Krieger N, Waterman PD, Chen JT, Soobader MJ, Subramanian S. Monitoring socioeconomic inequalities in sexually transmitted infections, tuberculosis, and violence: geocoding and choice of area-based socioeconomic measures—the Public Health Disparities Geocoding Project (US). Public Health Rep. 2003;118: 240–260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.McGinnis JM, Foege WH. Actual causes of death in the United States. JAMA. 1993;270:2207–2212. [PubMed] [Google Scholar]
- 7.Mokdad AH, Marks JS, Stroup DF, Gerberding JL. Actual causes of death in the United States, 2000. JAMA. 2004;29:1238–1245. [DOI] [PubMed] [Google Scholar]
- 8.Friedan TR. Asleep at the switch: local public health and chronic disease. Am J Public Health. 2004; 94:2059–2061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Simon PA, Wold CM, Cousineau MR, Fielding JE. Meeting the data needs of a local health department: the Los Angeles County Health Survey. Am J Public Health. 2001;91:1950–1952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fielding JE, Frieden TR. Local knowledge to enable local action. Am J Prev Med. 2004;27:183–184. [DOI] [PubMed] [Google Scholar]
- 11.Northridge ME, Morabia A, Ganz ML, et al. Contribution of smoking to excess mortality in Harlem. Am J Epidemiol. 1998;147:250–258. [DOI] [PubMed] [Google Scholar]
- 12.The Health of Angelenos: A Comprehensive Report of the Health of Residents of Los Angeles County. Los Angeles, Calif: Los Angeles County Dept of Health Services; 2000.
- 13.Seattle/King County Epidemiology, Planning, and Evaluation Unit. Communities Count 2000: social and health indicators across King County. Available at: http://www.metrokc.gov/health/reports/cc2k/cc2kintro.pdf. Accessed May 3, 2006.
- 14.New York City Dept of Health and Mental Hygiene. New York City Health and Nutrition Examination Survey (NYC HANES). Available at: http://www.nyc.gov/html/doh/html/hanes/hanes.html. Accessed May 3, 2006.
- 15.Karpati A, Kerker B, Mostashari F, et al. Health disparities in New York City. Available at: http://www.nyc.gov/html/doh/downloads/pdf/epi/disparities-2004.pdf. Accessed May 3, 2006.
- 16.New York City Dept of Health and Human Hygiene. New York City Community Health Survey 2002. Available at: http://www.nyc.gov/html/doh/html/survey/survey.shtml. Accessed May 3, 2006.
- 17.Centers for Disease Control and Prevention. SMART: selected metropolitan and micropolitan area risk trends. Available at: http://apps.nccd.cdc.gov/brfss-smart/index.asp. Accessed May 3, 2006.
- 18.Centers for Disease Control and Prevention. 2002 IL BRFSS SMART (selected metropolitan/micropolitan area risk trends for Illinois). Available at: http://apps.nccd.cdc.gov/brfss-smart/MMSAProjAreas.asp?state=IL. Accessed May 3, 2006.
- 19.Fullilove RE, Fullilove MT, Northridge ME, et al. Risk factors for excess mortality in Harlem: findings from the Harlem Household Survey. Am J Prev Med. 1999;16:S22–S28. [DOI] [PubMed] [Google Scholar]
- 20.Northridge ME, Meyer IH, Dunn L. Overlooked and underserved in Harlem: a population-based survey of adults with asthma. Environ Health Perspect. 2002; 110:S217–S220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Healthy Communities 2000: Model Standards. Guidelines for Community Attainment of the Year 2000 National Health Objectives. 3rd ed. Washington, DC: American Public Health Association; 1991.
- 22.Brownson RC, Bright FS. Chronic disease control in public health practice: looking back and moving forward. Public Health Rep. 2004;119:230–238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Howell EM, Pettit KL, Ormond BA, Kingsley GT. Using the National Neighborhood Indicators Partnership to improve public health. J Public Health Manage Pract. 2003;9:235–242. [DOI] [PubMed] [Google Scholar]
- 24.Chicago Fact Book Consortium. Local Community Fact Book: Chicago Metropolitan Area, 1990. Chicago, Ill: Academy Chicago Publishers; 1995.
- 25.Kish L. Survey Sampling. New York, NY: John Wiley & Sons Inc; 1965.
- 26.Sudman S. Applied Sampling. New York, NY: Academic Press Inc; 1976.
- 27.Troldahl V, Carter RE. Random selection of respondents within households in phone surveys. J Marketing Res. 1964;1:71–76. [Google Scholar]
- 28.Standard Definitions: Final Dispositions of Case Codes and Outcome Rates for Surveys. Ann Arbor, Mich: American Association for Public Opinion Research; 2000.
- 29.Johnson TP, Owens L. Survey response rate reporting in the professional literature. In: Proceedings of the 2003 American Statistical Association Conference, Section on Survey Research Methods. Alexandria, Va: American Statistical Association; 2004:127–133.
- 30.Stata Statistical Software, Version 8.0. College Station, Tex: Stata Corp; 2003.
- 31.Krieger N, Rowley DL, Hermann AA, Avery B, Phillips MT. Racism, sexism and social class: implications for studies of health, disease, and well being. Am J Prev Med. 1993;9(suppl 6):82–122. [PubMed] [Google Scholar]
- 32.Navarro V. Race or class versus race and class: mortality differentials in the United States. Lancet. 1990;336:1238–1240. [DOI] [PubMed] [Google Scholar]
- 33.Kaufman JS, Cooper RS. Seeking causal explanations in social epidemiology. Am J Epidemiol. 1999; 150:113–120. [DOI] [PubMed] [Google Scholar]
- 34.Muntaner C. Invited commentary: social mechanisms, race and social epidemiology. Am J Epidemiol. 1999;150:121–126. [DOI] [PubMed] [Google Scholar]
- 35.Ren XS, Amick BC, Williams DR. Racial/ethnic disparities in health: the interplay between discrimination and socioeconomic status. Ethn Dis. 1999;9: 151–165. [PubMed] [Google Scholar]
- 36.Massey DS, Denton NA. American Apartheid: Segregation and the Making of the Underclass. Cambridge, Mass: Harvard University Press; 1993.
- 37.Silva A, Whitman S, Margellos H, Ansell D. Evaluating Chicago’s success in reaching the Healthy People 2000 goal of reducing health disparities. Public Health Rep. 2001;116:484–494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Margellos H, Silva A, Whitman S. Comparison of health status indicators in Chicago: are black-white disparities worsening? Am J Public Health. 2004;94: 116–121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Acevedo-Garcia D, Lochner KA. Residential segregation and health. In: Kawachi I, Berkman LF, eds. Neighborhoods and Health. New York, NY: Oxford University Press Inc; 2003:265–287.
- 40.Diez Roux AV. The examination of neighborhood effects on health: conceptual and methodological issues related to the presence of multiple levels of organization. In: Kawachi I, Berkman LF, eds. Neighborhoods and Health. New York, NY: Oxford University Press Inc; 2003:45–64.
- 41.Barbeau EM, Krieger N, Soobader MJ. Working class matters: socioeconomic disadvantage, race/ethnicity, gender, and smoking in NHIS 2000. Am J Public Health. 2004;94:269–278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.O’Campo P. Invited commentary: advancing theory and methods for multilevel models of residential neighborhoods and health. Am J Epidemiol. 2003;157: 9–13. [DOI] [PubMed] [Google Scholar]
- 43.Kawachi I, Berkman LF, eds. Neighborhoods and Health. New York, NY: Oxford University Press Inc; 2003.
- 44.Shahar E, Folsom AR, Jackson R. The effect of nonresponse on prevalence estimates for a referent population: insights from a population-based cohort study. Ann Epidemiol. 1996;6:498–506. [DOI] [PubMed] [Google Scholar]
- 45.Cohen G, Duffy JC. Are nonrespondents to health surveys less healthy than respondents? J Off Stat. 2002;18:13–23. [Google Scholar]
- 46.Mostashari F, Kerker BD, Hajat A, Miller N, Frieden TR. Smoking practices in New York City: the use of a population-based survey to guide policymaking and programming. J Urban Health. 2005;82: 58–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Whitman S, Shah AM. Progress report to the Chicago Community Trust, May 2005. Available at: http://www.sinai.org/urban/publications.asp. Accessed May 3, 2006.
- 48.Healthy People 2010: Understanding and Improving Health. Washington, DC: US Dept of Health and Human Services; 2000.


