Abstract
Objective
To evaluate whether the type of on-site care a trauma patient receives affects outcome.
Summary Background Data
The controversy regarding the prehospital care of trauma patients between Advanced Life Support (ALS) and Basic Life Support (BLS) is ongoing. Due to this unresolved controversy, as well as historical, cultural, and political factors, there are significant variations with respect to the type of prehospital care available for trauma patients.
Methods
This prospective cohort study compared three types of prehospital trauma care systems: Montreal, where physicians provide ALS (MD-ALS); Toronto, where paramedics provide ALS (PMD-ALS); and Quebec City, where emergency medical technicians provide BLS only (EMT-BLS). The study took advantage of this variation to evaluate the association between the type of on-site care and mortality in patients with major life-threatening injuries. All patients were treated at highly specialized tertiary (level I) trauma hospitals. The main outcome measure was death as a result of injury. Follow-up was to hospital discharge.
Results
The overall mortality rates by type of on-site personnel were physicians 35%, paramedics 24%, and EMTs 18%. For patients with major but survivable trauma, the overall mortality rates were physicians 32%, paramedics 28%, and EMTs 26%. The overall mortality rate of patients receiving only BLS at the scene was 18% compared to 29% for patients receiving ALS. For the subgroup of patients with major but survivable injuries, the mortality rates were 30% for ALS and 26% for BLS. The adjusted increased risk for mortality in patients receiving ALS at the scene was 21%.
Conclusions
In urban centers with highly specialized level I trauma centers, there is no benefit in having on-site ALS for the prehospital management of trauma patients.
In the Western world, trauma is the leading cause of death for individuals under 45 years of age, and it remains the fourth leading cause of death for all ages combined. 1,2 In 1994, 8,687 people died following accidents in Canada. 3 Approximately four times as many patients suffer severe disability related to accidents each year.
Prehospital care for trauma patients is provided by emergency medical personnel using either Basic Life Support (BLS) or Advanced Life Support (ALS) techniques. BLS (or “scoop and run”) consists of noninvasive interventions such as wound dressing, immobilization, fracture splinting, oxygen administration, and noninvasive cardiopulmonary resuscitation. ALS encompasses all of these BLS techniques in addition to invasive procedures, including intubation, initiation of IV access with fluid replacement, administration of medications, and in rare cases application of pneumatic antishock garments (PASG). The rationale for the use of on-site ALS in trauma is that these interventions will reduce the rate of physiologic and hemodynamic deterioration, thus stabilizing the patient before arrival at the hospital. It is expected that this will result in increased chances of survival. The paradox is that on-site ALS increases the amount of time that is spent on the scene and hence increases the delay to definitive in-hospital care. To date, the controversy between the “scoop and run” versus “stay and stabilize” approach to prehospital trauma care remains unresolved and has been the subject of a limited number of studies, most of which were based on small numbers of selected patients. Studies supporting ALS have failed to show an association between on-site ALS and increased survival among patients with major trauma. 4–14 Studies supporting BLS have shown higher survival rates for patients treated using the “scoop and run” approach compared to those treated using on-site ALS. 15–30 The validity of these studies is often compromised due to the lack of control for confounding variables and appropriate comparison groups.
A 1992 study by Schmidt et al. 31 compared trauma patients with equivalent Injury Severity Scores (ISS) transported by helicopter in Germany to patients transported by helicopter in the United States. In Germany, patients received treatment by a paramedic and a trauma surgeon and in the United States by a paramedic and a nurse. They found that the German patients received significantly more advanced interventions, including IV fluids, endotracheal intubations, and thoracic decompressions, than the American group. This led to a decrease in early mortality and improved outcome compared to patients in the Major Trauma Outcome Study (MTOS).
In addition to increasing prehospital delays, the argument against “stay and stabilize” is strengthened because none of the specific ALS interventions has been proven to be beneficial for the prehospital management of severely injured patients. The rationale for using on-site IV line placement and fluid infusion is that it will control hemodynamic deterioration. The amount of fluid infused, however, cannot compensate for the blood lost in a severely bleeding patient; for such cases the definitive treatment is surgery. 8,19,20 The time required to start an IV on the scene is a matter of debate: certain authors report minimal times between 2 and 4 minutes, 10,32–36 while others show times of 12 minutes or more. 18,37 There are no controlled studies evaluating the impact of IV placement on patient outcome.
Similarly, the effectiveness of on-site intubation in improving outcome of severely injured patients has not been adequately evaluated. The rationale for on-scene intubation is that this intervention will maintain airway patency and oxygenation. 38 As with IV placement, the argument against intubation is that it causes significant delays to definitive in-hospital care. Unlike IV placement, however, there is some agreement that in certain severely injured and unconscious patients, intubation should be initiated at the scene or en route to the hospital. 7,19,38
The only ALS intervention subjected to evaluation by randomized controlled trials is PASG. A series of such studies failed to demonstrate any benefit and in some cases showed an increase in adverse outcome rates associated with the use of this apparatus. 39–41
The unresolved controversy regarding the on-site management of trauma patients is reflected in the regional variation of prehospital patient management protocols. This variation is observed profoundly in Canada, where the type of on-site care available to trauma patients ranges from BLS provided by emergency medical technician (EMTs) to physician-provided ALS. The type of prehospital care available to trauma patients is determined by regional policies that are dictated by local political, cultural, and economic factors as well as the influential opinion of local experts.
The purpose of the present study was to compare the effectiveness of three different approaches for the prehospital management of severely injured patients. The study assessed the relative effectiveness of a BLS-only approach, a physician-based ALS approach (MD-ALS), and a paramedic-based ALS system (PMD-ALS) used in three different Canadian cities.
Prehospital trauma care in Montreal is coordinated by Urgences-Santé, a nonprofit government agency under the aegis of the local health board. In this system, EMTs and physicians are used for the prehospital management of trauma patients, but only physicians are permitted to perform ALS. The protocol in effect at Urgences-Santé is aimed at limiting the request of a physician to cases of severe trauma. Before 1993, approximately 75% of the major trauma patients were treated at the scene by a physician. In 1994, this was reduced to 40%, in 1995 it was 30%, but since then it has been increased to 50%. The lack of availability of physicians to answer all of the requests creates a random fluctuation in which patients with severe injuries may receive on-site care by a physician with ALS available, or by an EMT applying the “scoop and run” approach.
Prehospital care in Quebec City is provided exclusively by EMTs administering BLS techniques only.
Prehospital care in Toronto is provided by EMTs who provide BLS and paramedics who are capable of performing ALS. Between 1984 and 1995 ambulance crews consisted of either two EMTs or two paramedics. Since that time, a two-tiered response algorithm was introduced in which the first responders were EMTs (BLS crew) followed by paramedics (ALS crews) who took over the care of the patient. To increase ALS coverage, in 1995, “split crews” were implemented. The ALS split crew consists of a fully certified paramedic and a level II paramedic who is not permitted to administer medications, initiate intravenous access, or perform endotracheal intubation. With this increased coverage, approximately 48% of the major trauma cases have on-site ALS available. The treatment performed by the paramedics (ALS crews) is subject to “off-line” control by written protocols and less frequently “on-line” control. BLS crews adhere to the “scoop and run” approach.
The objectives of the current study were threefold:
To compare the effectiveness of three different prehospital trauma care systems—one with only EMTs providing BLS and adhering to the “scoop and run” approach), one with paramedics available to provide on-site ALS (PMD-ALS), and the third with physicians available to provide on-site ALS (MD-ALS)—in reducing trauma-related mortality.
To evaluate and compare the effectiveness of three different types of on-site management (EMT-BLS, PMD-ALS, and MD-ALS) in reducing trauma-related mortality.
To evaluate and compare the effectiveness of two different types of on-site care (ALS and BLS) in reducing trauma-related mortality.
METHODS
This observational study was based on three cohorts of patients treated for severe injuries between January 1, 1993, and December 31, 1997, in three Canadian cities (Montreal, Quebec City, and Toronto). The three cohorts were exposed to different prehospital trauma care, but all received in-hospital care at designated level I tertiary trauma centers. The type of on-site care provided depended on the prehospital system in place in the respective city and the availability of ALS personnel within the city.
The study sample from each site was identified from patients who were treated for severe injury at one of the four tertiary trauma centers in the three cities: the Montreal General Hospital and Hôpital Sacré-Coeur in Montreal, Hôpital Enfant-Jésus in Québec City, and Sunnybrook Health Sciences Trauma Center in Toronto. To identify patients with major trauma, the following inclusion criteria were applied: death as a result of the injury, hospitalization for more than 3 days, treatment in an intensive care unit, surgery requiring admission, or an ISS of more than 12.
The outcome measure for the present study was mortality, defined as death as a result of the injury. The cohorts were followed up to discharge from the trauma centers. The exposure or independent variable used was dependant on the objective addressed. For the first objective, the independent variable was the city, which defined the type of prehospital services available as EMTs only (Quebec City), PMD-ALS (Toronto), and MD-ALS (Montreal). For the second objective the exposure variable described the type of on-site crew managing the patient as EMT, PMD, or MD. Finally, the exposure variable for the third objective described the type of on-site care received by the patient as ALS or BLS.
Statistical Analysis
Between-group differences with respect to categorical variables were evaluated for statistical significance with the chi-square statistic. For continuous variables, one-way analysis of variance was used to evaluate the significance of between-group differences. For all estimates 95% confidence intervals were calculated. Between-group differences with respect to mortality rates were described by the relative risk using Quebec City, EMT-BLS, or BLS as the baseline, depending on the specific analysis conducted. For each estimate of the relative risk, 95% confidence intervals were used to assess precision and statistical significance.
Logistic regression models were used to produce adjusted estimates of the relative risk for each one of the exposure variables studied. The logistic regression model was developed by first including all of the following variables as predictors of death: age (years); gender; body region injured (yes/no): head/neck, face, thorax, abdomen, extremities; mechanism of injury (yes/no): motor vehicle collision, fall, firearm, stabbing, blunt object, sharp object (accidental), other; ISS; and penetrating trauma. A backwards selection process was used to identify those variables that were the strongest independent predictors of mortality. A significance level of 15% was set as the minimum for the variable to be kept in the final model. The variables maintained in the model by this backwards selection procedure defined the basic logistic regression models that were used in the final analyses.
RESULTS
A total of 9,405 patients were included in the study. Table 1 shows that 5,096 (54% of the patients in the study sample) were from Montreal, 2,530 (27%) were from Toronto, and 1,779 (19%) were from Quebec City. The reason that there are approximately twice as many patients from Montreal is explained by the fact that two trauma centers participated from this region.
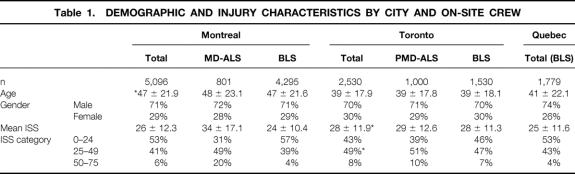
Table 1. DEMOGRAPHIC AND INJURY CHARACTERISTICS BY CITY AND ON-SITE CREW
Montreal had 801 (16%) patients who received on-site ALS by a physician, while 1,000 (40%) of the Toronto patients received ALS by a paramedic at the scene. None of the patients from Quebec City received on-site ALS. In total, 1,801 (19%) patients received on-site ALS and 7,604 (81%) received BLS only at the scene. Of the 1,801 patients receiving ALS at the scene, 801 (44%) were treated by a physician and 1,000 (56%) were treated by a paramedic.
The data in Table 1 describe the demographic and injury characteristics of the study sample. The overall mean age of the sample was 44 years, and 72% of patients were male. Compared to Quebec City and Toronto, the Montreal patients had a significantly higher mean age (P < .001). Although the proportion of male patients was slightly higher in Quebec City, this difference was not statistically significant.
The overall mean ISS was 26, with 43% of patients having an ISS between 25 and 49 and 6% having an ISS over 49. The mean ISS of the Toronto patient cohort was 28 compared to 26 for Montreal and 25 for Quebec City. This difference was statistically significant (P < .001). The Toronto cohort had a significantly higher proportion of patients with an ISS between 25 and 49 compared to the patients from Montreal and Quebec City (P < .001).
Most of the patients (57%) were injured in motor vehicle accidents; 28% were injured in falls. Injuries due to firearms, stabbing, blunt object, sharp object, or other causes comprised approximately 15% of the remaining injuries, with blunt objects and firearms representing 5% and 3% of the total, respectively. The proportion of patients injured in motor vehicle collisions was significantly higher in Toronto (74%) compared to Montreal (50%) and Quebec City (54%) (P < .001). The proportion of patients injured in falls was significantly lower in Toronto (12%) compared to Montreal (33%) and Quebec City (33%) (P < .001). All other mechanisms of injury were statistically similar between cities.
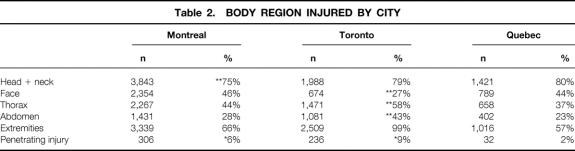
Most patients had at least one injury to the head or the extremities. The proportion of patients with injuries to the head was significantly lower for Montreal (P < .01). The proportion of patients with facial injuries was significantly lower in Toronto (P < .01). The Toronto patients had significantly higher rates of thoracic and abdominal injuries (P < .01). The proportion of patients with penetrating injuries was significantly higher in Toronto, followed by Montreal and lowest in Quebec (P = .01) (Table 2).
Table 2. BODY REGION INJURED BY CITY
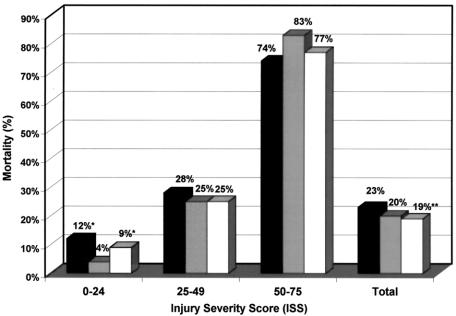
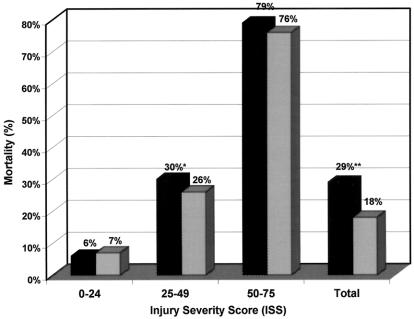
The overall mortality rates for Montreal, Toronto, and Quebec City were 23%, 20%, and 19% (Fig. 1). The mortality rate for Quebec City was significantly lower compared to Montreal and Toronto (P < .001). For patients with mild to moderate injury severity (ISS 1–24), there was a significant trend of lower mortality in Toronto followed by Quebec City, with Montreal having the highest rate (P = .001). There were no statistically significant differences between the three cities with respect to the mortality rates for patients with major (ISS 25–49) or fatal (ISS 50–79) injury severity.
Figure 1. Mortality by city stratified by Injury Severity Score (ISS). ▪, Montreal;, Toronto; □, Quebec. *P = .001, **P < .01.
Table 3 summarizes the demographic and injury characteristics of the patients by the type of crew that was present at the scene. These data show that 7,604 patients received on-site care by a BLS crew, 801 were treated by a physician at the scene, and 1,000 were treated by a paramedic. Both physicians and paramedics were capable of providing ALS at the site. The patients treated by paramedics were younger compared to those treated by a BLS crew and by physicians (P = .001). The proportion of male patients was just over 70% for all three groups.
Table 3. DEMOGRAPHIC AND INJURY CHARACTERISTICS BY ON-SITE CREW
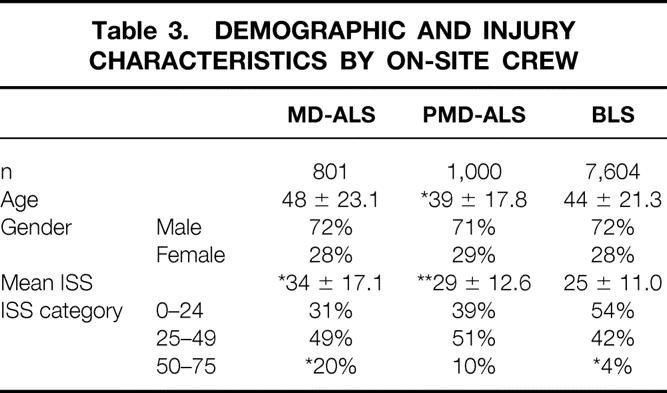
The mean ISS was significantly higher for the patients treated by a physician at the scene compared to the other two groups (P = .001). In addition, the mean ISS of the patients treated by paramedics was higher than that of the patients treated by an EMT crew (P = .01). The ISS distribution shows that a significantly higher proportion of the patients treated by a physician had an ISS between 50 and 75, while the proportion of patients with an ISS between 24 and 49 was significantly lower for the patients treated by a BLS crew (P = .001). A significantly higher proportion of patients injured in motor vehicle collisions were treated by paramedics (72%) compared to physicians (52%) and EMTs (56%) (P = .001) and a lower proportion injured in falls (PMD 11%, MD-ALS 52%, BLS 29%) (P = .001). Other mechanisms of injury were statistically similar between groups.
Concerning body regions injured, the prevalence of injuries to the head or neck regions was not different between the three groups. However, the proportion of patients with injuries to the face was lower for the patients treated by paramedics (PMD 27%, MD 44%, BLS 42%), while significantly more patients in this group had injuries to the thorax (PMD 59%, MD 49%, BLS 45%) and abdomen (PMD 45%, MD 32%, BLS 29%)(P = .001). Finally, the incidence of penetrating injuries was higher in the patients treated by paramedics (PMD 12%, MD 7%, BLS 5%) (P = .001).
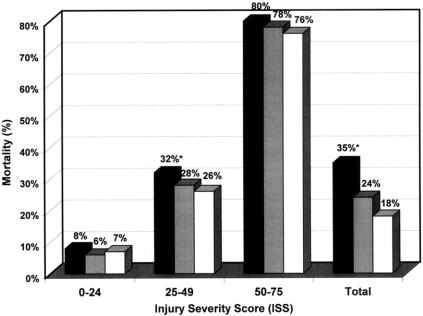
The overall mortality rate was significantly higher for the patients treated by a physician at the scene (P = .001). However, for the subgroup of patients with an ISS between 1 and 24, the mortality rate was low and not different for the three groups. For the patients with an ISS between 25 and 49, the mortality rate for the MD-ALS group was 32% compared to 28% for the PMD-ALS group and 26% for the BLS group. The difference between the MD-ALS and the other two groups was statistically significant (P = .001) (Fig. 2).
Figure 2. Mortality by on-site crew. ▪, Montreal;, Toronto; □, Quebec; BLS, Basic Life Support; MD-ALS, physician-provided Advanced Life Support; PMD-ALS, paramedic-provided Advanced Life Support. *P = .001.
Table 4 summarizes the demographic information and ISS of the patients depending on whether ALS or BLS care was administered on site. For these two groups, the mean age and proportion of male patients were similar, but the mean ISS was significantly higher for the ALS patients (P = .001). The ISS distribution showed that the ALS group had a significantly higher proportion of patients with an ISS between 24 and 49 and between 50 and 75 (P = .001). The ALS group had a significantly lower proportion of patients injured in falls (n = 379 [21%]) compared to the BLS group (n = 2,214 [29%]) (P = .001), but the other mechanisms were similar between ALS and BLS. The prevalence of injuries to the head was similar for the two groups (P = .37), although the proportion of patients with injuries to the thorax (ALS 55%, BLS 45%), abdomen (ALS 39%, BLS 29%), and extremities (ALS 88%, BLS 70%) was higher in the ALS group (P = .001). The proportion of ALS patients with penetrating injuries was twice that of the BLS patients (ALS 10%, BLS 5%). This difference was statistically significant (P = .001).
Table 4. DEMOGRAPHIC AND INJURY CHARACTERISTICS BY ON-SITE CARE
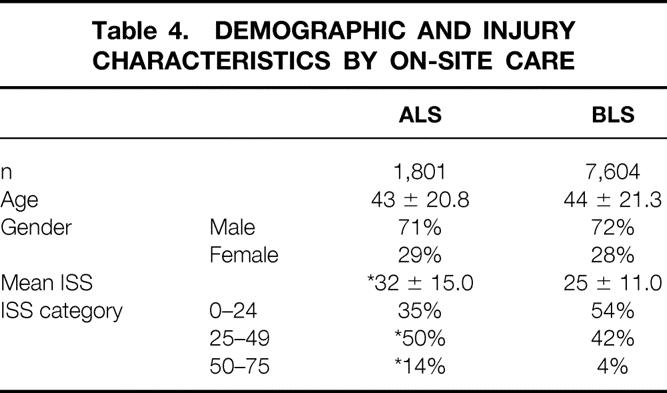
The overall mortality rate was 29% for the ALS group and 18% for the BLS group. The crude odds ratio was 1.86 (95% confidence limits 1.65–2.09). These data show a significant increase in the risk of dying associated with on-site ALS (P = .001) (Fig. 3). Stratification by ISS categories showed that for patients with minor to moderate injury (ISS 1–24), the mortality rates for the ALS and BLS groups were similar. For the patients with an ISS between 24 and 49, the mortality for the ALS group was 30% compared to 26% for the BLS group. The odds ratio for this stratum was 1.23 (95% confidence limits 1.04–1.45). This difference and odds ratio were statistically significant (P = .01).
Figure 3. Mortality by on-site care. ▪, Advanced Life Support (ALS);, Basic Life Support (BLS). *P = .01, **P = .001.
The final logistic regression model was derived by the backward selection process and included the following variables as covariates: age, body region injured, mechanism of injury, and ISS. The first logistic regression model (Table 5) tested the adjusted association between city and the odds of dying. This analysis showed that the adjusted odds of dying in Quebec City were 20% lower compared to Montreal; this was statistically significant (P = .01). The odds ratio for Toronto versus Quebec City indicated a 14% increase in the risk of dying for Toronto; this was not statistically significant. Compared to Toronto, the odds of dying in Montreal were 27% greater (P = .003).
Table 5. LOGISTIC REGRESSION ANALYSIS
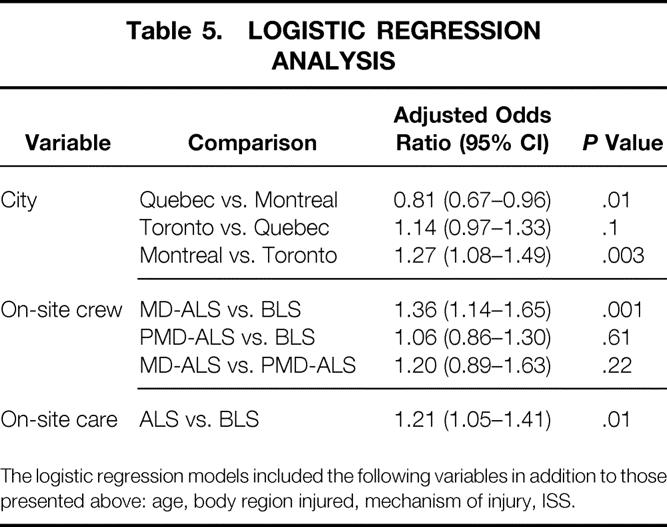
The logistic regression models included the following variables in addition to those presented above: age, body region injured, mechanism of injury, ISS.
The second logistic regression model tested the association between the on-site crew and the odds of dying. The results of this analysis showed that compared to being treated by an EMT, being treated by an MD at the scene was associated with a 36% increase in the adjusted odds of dying (P = .001). The odds ratio comparing physicians to paramedics was also elevated, indicating a 20% increase in the odds of dying; however, this did not reach statistical significance (P = .22). Finally, the odds ratio of paramedics versus EMTs showed a 6% increase in the odds of dying; this was not statistically significant (P = .61).
The third multiple logistic regression analysis compared on-site ALS to BLS only. This analysis showed that when patients received any type of ALS on the scene, the adjusted odds of dying increased significantly by 21% (P = .01).
The mean scene times for the three different types of on-site crews differed. MD-ALS crews had significantly longer mean scene time (24.9 minutes) compared to BLS crews (21.9 minutes) and PMD-ALS crews (19.3 minutes) (P = .01). The mean scene time for the PMD-ALS crew was significantly shorter compared to the BLS and the MD-ALS crews (P = .01).
To adjust for the effect of scene time on the association between the exposure variables and mortality, the logistic regression analyses were repeated with scene time included as a covariate in the models. The inclusion of scene time did not significantly change the odds ratio estimated (data not shown), although a longer scene time was significantly associated with an increased chance of dying in all models.
DISCUSSION
This observational study evaluated the association between three different types of prehospital care and mortality in patients with severe injuries. The study took advantage of the existing variations in prehospital trauma care between different regions of Canada. This variation reflects differences in local policies that result in inequality of care provided to trauma victims in Canada. The policies governing the type of prehospital care are determined at government and local health board levels and reflect an existing disagreement with respect to the prehospital management of patients with severe injuries.
The current study compared the mortality of patients with severe trauma who were ultimately treated for injuries at four level I, tertiary trauma centers in Montreal, Quebec City, and Toronto. The prehospital trauma care in these cities varies significantly, with physician-provided ALS in Montreal, paramedic-provided ALS in Toronto, and BLS only, provided by EMTs in Quebec City. The study was restricted to patients treated in designated tertiary, level I trauma centers to remove potential confounding factors related to differences in the level of hospital care provided to these patients.
The results of the study show that the use of on-site ALS, in general, does not provide any benefits in reducing mortality in patients with major trauma. This result is generalizable to patients injured in urban centers served by highly organized trauma care systems with access to a level I trauma center. The data from this study show that when physicians provide on-site ALS to trauma patients, the risk of mortality is significantly increased when compared to both EMT-provided BLS and paramedic-provided ALS. On-site ALS provided by paramedics was not associated with a reduction in mortality when compared to EMTs.
The results of this study are compatible with others in the literature that support the “scoop and run” approach for the prehospital management of trauma patients in an urban setting. The lack of effectiveness of ALS in general has often been attributed to the increased time required to perform ALS procedures at the scene. However, there is now a considerable body of evidence to suggest that certain ALS procedures, such as IV fluid replacement, may be harmful for patients with major trauma. 24,29,42,43 The increased risk of mortality associated with MD-ALS is probably due to the lack of standardized protocols and lack of specific training. The results of this study, in combination with the already existing evidence in the current literature, fail to support the use of ALS in the prehospital management of urban trauma patients. These conclusions may or may not apply to rural trauma patients. These results would suggest policy changes that minimize on-site care and restrict it to BLS procedures only. Resources should be allocated for the establishment of trauma care systems and networks that ensure rapid transport of major trauma patients to highly specialized trauma hospitals. In these systems, emphasis should be placed on minimizing on-scene time and establishing patient transfer corridors to decrease time to definitive in-hospital care and maximize efficiency of the healthcare resources.
Footnotes
Correspondence: John S. Sampalis, PhD, Montreal General Hospital, Department of Clinical Epidemiology, L10-520, 1650 Cedar Avenue, Montreal, Quebec, Canada.
E-mail: mcsa@musica.mcgill.ca
Support provided by the NHRDP, Grant #6605-5264-001.
Accepted for publication March 27, 2002.
References
- 1.Health Reports. Canadian Centre for Health Information. Statistics Canada, Ottawa, 1989.
- 2.Mortality. Summary List of Causes, Vital Statistics. Health Division, Vital Statistics and Health Status Section, Statistics Canada, Ottawa, 1987–1990.
- 3.Health Reports. Statistics Canada. Vol. 7, No. 1, Cat. No. 82–003, 1995.
- 4.Hedges JR, Sacco WJ, Champion HR. An analysis of prehospital care of blunt trauma. J Trauma 1982; 22: 989–993. [DOI] [PubMed] [Google Scholar]
- 5.Aprahamian C, Thompson BM, Towne JB, et al. The effect of a paramedic system on mortality of major open intra-abdominal vascular trauma. J Trauma 1983; 23: 687–690. [DOI] [PubMed] [Google Scholar]
- 6.Potter D, Goldstein G, Fung SC. A controlled trial of prehospital advanced life support in trauma. Ann Emerg Med 1988; 17: 582–588. [DOI] [PubMed] [Google Scholar]
- 7.Bodai BI, Walton CB. Mistakes in treatment of accident cases before reaching hospital. Br J Accid Surg 1987; 18: 18–20. [DOI] [PubMed] [Google Scholar]
- 8.Trunkey DD, Siegel J, Baker SP, et al. Panel: Current status of trauma severity indices. J Trauma 1983; 23: 185–201. [PubMed] [Google Scholar]
- 9.Jacobs LM, Sinclair A, Beiser A, et al. Prehospital advanced life support: benefits in trauma. J Trauma 1984; 24: 8–13. [DOI] [PubMed] [Google Scholar]
- 10.Cwinn AA, Pons PT. On-scene management of trauma patients by paramedics. Ann Emerg Med 1988; 17: 189–190. [DOI] [PubMed] [Google Scholar]
- 11.Cwinn AA, Pons PT, Moore EE, et al. Prehospital advanced trauma life support for critical blunt trauma victims. Ann Emerg Med 1987; 16: 399–403. [DOI] [PubMed] [Google Scholar]
- 12.Winchell JW, Hoyt DB. Endotracheal intubation in the field improves survival in patients with severe head injury. Arch Surg 1997; 132: 592–597. [DOI] [PubMed] [Google Scholar]
- 13.Aprahamian C, Thompson BM, Towne JB, et al. The effect of a paramedic on mortality of major open intra-abdominal vascular trauma. J Trauma 1983; 23: 687–690. [DOI] [PubMed] [Google Scholar]
- 14.Fortner GS, Oreskovich MR, Copass MK, et al. The effects of prehospital trauma care on survival from a 50-meter fall. J Trauma 1983; 23: 976–981. [DOI] [PubMed] [Google Scholar]
- 15.Gervin AS, Fischer RP. The importance of prompt transport in salvage of patients with penetrating heart wounds. J Trauma 1982; 22: 443–448. [DOI] [PubMed] [Google Scholar]
- 16.Ivatury RR, Nallathambi MN, Roberge RJ, et al. Penetrating thoracic injuries: in-field stabilization vs. prompt transport. J Trauma 1987; 27: 1066–1073. [PubMed] [Google Scholar]
- 17.Cayten CG, Longmore W, Kuehl A, et al. Basic Life Support vs Advanced Life Support for urban trauma. AAST Abstract J Trauma 1984; 24: 651. [Google Scholar]
- 18.Smith JP, Boda BI, Hill AS, et al. Prehospital stabilization of critically injured patients: a failed concept. J Trauma 1985; 25: 65–70. [DOI] [PubMed] [Google Scholar]
- 19.Trunkey DD. Trauma. Sci Am 1983; 249: 28–35. [PubMed] [Google Scholar]
- 20.Gold CR. Prehospital advanced life support vs “scoop and run” in trauma management. Ann Emerg Med 1987; 16: 797–801. [DOI] [PubMed] [Google Scholar]
- 21.Sampalis JS, Lavoie A, Williams JL, et al. Standardized mortality ratio analysis on a sample of severely injured patients from a large Canadian city without regionalized trauma care. J Trauma 1992; 33: 205–212. [DOI] [PubMed] [Google Scholar]
- 22.Potter D, Goldstein G, Fung SC, et al. A controlled trial of prehospital advanced life support in trauma. Ann Emerg Med 1988; 17: 582–588. [DOI] [PubMed] [Google Scholar]
- 23.Cayten CG, Longmore W, Kuehl A, et al. BLS versus ALS in an urban setting [abstract]. Ann Emerg Med 1986; 15: 626–627. [Google Scholar]
- 24.Bickell WH, Wall MJ, Pepe PE, et al. Immediate versus delayed fluid resuscitation for hypotensive patients with penetrating torso injuries. N Engl J Med 1994; 331: 1105–1109. [DOI] [PubMed] [Google Scholar]
- 25.Martin RR, Bickell WH, Pepe PE, et al. Prospective evaluation of preoperative fluid resuscitation in hypotensive patients with penetrating truncal injury: a preliminary report. J Trauma 1992; 33: 354–362. [DOI] [PubMed] [Google Scholar]
- 26.Cayten CG, Murphy JG, Stahl WM. Basic life support versus advanced life support for injured patients with an injury severity score of 10 or more. J Trauma 1993; 35: 460–467. [DOI] [PubMed] [Google Scholar]
- 27.Murphy JG, Cayten CG, Stahl WM, et al. Dual response runs in prehospital trauma care. J Trauma 1993; 35: 356–362. [DOI] [PubMed] [Google Scholar]
- 28.Clevenger FW, Yarbrough DR, Reines HD. Resuscitative thoracotomy: the effect of field time on outcome. J Trauma 1988; 28: 441–445. [DOI] [PubMed] [Google Scholar]
- 29.Sampalis JS, Tamim H, Denis R, et al. Ineffectiveness of on-site intravenous lines: is pre-hospital time the culprit? J Trauma 1997; 43: 608–617. [DOI] [PubMed] [Google Scholar]
- 30.Demetriades D, Chan L, Cornwell E, et al. Paramedic vs private transportation of trauma patients. Arch Surg 1996; 131: 133–138. [DOI] [PubMed] [Google Scholar]
- 31.Schmidt U, Frame SB, Nerlich ML, et al. On-scene helicopter transport of patients with multiple injuries: comparison of a German and an American system. J Trauma 1992; 33: 548–555. [DOI] [PubMed] [Google Scholar]
- 32.Spaite DW, Valenzuela TD, Criss EA, et al. A prospective in-field comparison of intravenous line placement by urban and nonurban emergency medical personnel. Ann Emerg Med 1994; 24: 209–214. [DOI] [PubMed] [Google Scholar]
- 33.O’Gorman M, Trabulsy P, Pilcher DB. Zero-time pre-hospital IV. J Trauma 1989; 29: 84–86. [PubMed] [Google Scholar]
- 34.Feldman R. IV line placement: a time study for prehospital providers. J Emerg Med Serv 1986; 11: 43–45. [Google Scholar]
- 35.Pons PT, Moore EE, Cusick JM, et al. Prehospital venous access in an urban paramedic system: a prospective on-scene analysis. J Trauma 1988; 28: 1460–1463. [DOI] [PubMed] [Google Scholar]
- 36.Tsai A, Kallsen G. Epidemiology of pediatric prehospital care. Ann Emerg Med 1987; 16: 284–292. [DOI] [PubMed] [Google Scholar]
- 37.Pepe PE, Copass MK, Joyce TH. Prehospital endotracheal intubation: rationale for training emergency medical personnel. Ann Emerg Med 1985; 14: 1085–1092. [DOI] [PubMed] [Google Scholar]
- 38.Bickell WH, Pepe PE, Bailey ML, et al. Randomized trial of pneumatic garments in the prehospital management of penetrating abdominal injuries. Ann Emerg Med 1987; 16: 653–658. [DOI] [PubMed] [Google Scholar]
- 39.Bickell WH, Pepe PE, Wyatt CH, et al. Effect of antishock trousers on the trauma score: a prospective analysis in the urban setting. Ann Emerg Med 1985; 14: 218–222. [DOI] [PubMed] [Google Scholar]
- 40.Mattox KL, Bickell WH, Pepe PE, et al. Prospective randomized evaluation of antishock MAST in post-traumatic hypotension. J Trauma 1986; 26: 779–786. [DOI] [PubMed] [Google Scholar]
- 41.Bickell WH, Bruttig SP, Millnamow GA, et al. The detrimental effects of intravenous crystalloid after aortotomy in swine. Surgery 1991; 110: 529–536. [PubMed] [Google Scholar]
- 42.Kowalenko T, Stern S, Dronen S, et al. Improved outcome with hypotensive resuscitation of uncontrolled hemorrhagic shock in a swine model. J Trauma 1992; 33: 349–353. [PubMed] [Google Scholar]
- 43.Krausz MM, Bar-Ziv M, Rabinovici R, et al. “Scoop and run” or stabilize hemorrhagic shock with normal saline or small volume hypertonic saline? J Trauma 1992; 33: 6–10. [DOI] [PubMed] [Google Scholar]