Abstract
Methanol intoxication produces toxic injury to the retina and optic nerve, resulting in blindness. The toxic metabolite in methanol intoxication is formic acid, a mitochondrial toxin known to inhibit the essential mitochondrial enzyme, cytochrome oxidase. Photobiomodulation by red to near-IR radiation has been demonstrated to enhance mitochondrial activity and promote cell survival in vitro by stimulation of cytochrome oxidase activity. The present studies were undertaken to test the hypothesis that exposure to monochromatic red radiation from light-emitting diode (LED) arrays would protect the retina against the toxic actions of methanol-derived formic acid in a rodent model of methanol toxicity. Using the electroretinogram as a sensitive indicator of retinal function, we demonstrated that three brief (2 min, 24 s) 670-nm LED treatments (4 J/cm2), delivered at 5, 25, and 50 h of methanol intoxication, attenuated the retinotoxic effects of methanol-derived formate. Our studies document a significant recovery of rod- and cone-mediated function in LED-treated, methanol-intoxicated rats. We further show that LED treatment protected the retina from the histopathologic changes induced by methanol-derived formate. These findings provide a link between the actions of monochromatic red to near-IR light on mitochondrial oxidative metabolism in vitro and retinoprotection in vivo. They also suggest that photobiomodulation may enhance recovery from retinal injury and other ocular diseases in which mitochondrial dysfunction is postulated to play a role.
Decrements in mitochondrial function have been postulated to be involved in the pathogenesis of numerous retinal and optic nerve diseases, including age-related macular degeneration, diabetic retinopathy, and Leber's hereditary optic neuropathy (1–3). Decrements in mitochondrial function have also been postulated to be involved in the pathogenesis in methanol intoxication (4–7). Methanol intoxication produces toxic injury to the retina and optic nerve, frequently resulting in blindness. A toxic exposure to methanol typically results in the development of formic acidemia, metabolic acidosis, visual toxicity, coma, and, in extreme cases, death (8, 9). Visual disturbances generally develop between 18 and 48 h after methanol ingestion and range from misty or blurred vision to complete blindness. Both acute and chronic methanol exposure have been shown to produce retinal dysfunction and optic nerve damage clinically (8–10) and in experimental animal models (11–14).
Formic acid is the toxic metabolite responsible for the retinal and optic nerve toxicity produced in methanol intoxication (4–7, 15). Formic acid is a mitochondrial toxin that inhibits cytochrome c oxidase, the terminal enzyme of the mitochondrial electron transport chain of all eukaryotes (16, 17). Cytochrome oxidase is an important energy-generating enzyme critical for the proper functioning of almost all cells, especially those of highly oxidative organs, including the retina and brain (18). Previous studies in our laboratory have established a rodent model of methanol-induced visual toxicity and documented formate-induced mitochondrial dysfunction and retinal photoreceptor toxicity in this animal model (6, 7, 12, 13).
Photobiomodulation by light in the red to near-IR range (630–1,000 nm) using low-energy lasers or light-emitting diode (LED) arrays has been shown to accelerate wound healing, improve recovery from ischemic injury in the heart, and attenuate degeneration in the injured optic nerve (19–24). At the cellular level, photoirradiation at low fluences can generate significant biological effects, including cellular proliferation, collagen synthesis, and the release of growth factors from cells (22, 25, 26). Our previous studies have demonstrated that LED photoirradiation at 670 nm (4 J/cm2) stimulates cellular proliferation in cultured cells and significantly improves wound healing in genetically diabetic mice (19, 24). Despite its widespread clinical application, the mechanisms responsible for the beneficial actions of photobiomodulation have not been elucidated. Mitochondrial cytochromes have been postulated as photoacceptors for red to near-IR light energy and reactive oxygen species have been advanced as potential mediators of the biological effects of this light (25, 27).
We hypothesize that the therapeutic effects of red to near-IR light result, in part, from the stimulation of cellular events associated with increases in cytochrome c oxidase activity. In support of this hypothesis, we have recently demonstrated in primary neuronal cells that LED photobiomodulation (670 nm at 4 J/cm2) reverses the reduction in cytochrome oxidase activity produced by the blockade of voltage–dependent sodium channel function by tetrodotoxin (28). The present studies extended these investigations to an in vivo system to determine whether 670-nm LED treatment would improve retinal function in an animal model of methanol-induced mitochondrial dysfunction.
Using the electroretinogram (ERG) as a sensitive indicator of retinal function, we demonstrated that three brief (2 min, 24 s) 670-nm LED treatments (4 J/cm2) delivered 5, 25, and 50 h after the initial dose of methanol attenuated the retinotoxic effects of methanol-derived formate. Our studies demonstrate a significant recovery of rod- and M-cone-mediated retinal function as well as a significant recovery of UV-cone-mediated function in LED-treated rats. We further show that LED treatment protected the retina from methanol-induced histopathology. The present study provides evidence that 670-nm LED treatment promotes the recovery of retinal function and protects the retina against the cytotoxic actions of the mitochondrial toxin, formic acid. Our findings are consistent with the hypothesis that LED photobiomodulation at 670 nm improves mitochondrial respiratory chain function and promotes cellular survival in vivo. They also suggest that photobiomodulation may enhance recovery from retinal injury and other ocular diseases in which mitochondrial dysfunction is postulated to play a role.
Methods
Materials.
LED arrays (8 × 10 cm) were obtained from Quantum Devices (Barneveld, WI). Methanol (HPLC grade) obtained from Sigma was diluted in sterile saline and administered as a 25% (wt/vol) solution. Thiobutabarbitol sodium salt (Inactin) was purchased from Research Biochemicals (Natick, MA). Atropine sulfate was obtained from AmVet Pharmaceuticals (Fort Collins, CO). Hydroxypropyl methylcellulose (2.5%) drops were acquired from IOLAB Pharmaceuticals, Claremont, CA. Atropine sulfate ophthalmic solution drops were purchased from Phoenix Pharmaceutical (St. Joseph, MO). All other chemicals were reagent grade or better.
Animals.
Male Long-Evans rats (Harlan–Sprague–Dawley), which weighed 250–350 g, were used throughout these experiments. All animals were supplied with food and water ad libitum and maintained on a 12-h light/dark schedule in a temperature- and humidity-controlled environment. Animals were handled in accordance with the Guide for the Care and Use of Laboratory Animals as adopted and promulgated by the National Institutes of Health.
Methanol-Intoxication Protocol.
Animals were randomly assigned to one of four treatment groups: (i) untreated control, (ii) LED-treated control, (iii) methanol-intoxicated, and (iv) LED-treated, methanol-intoxicated rats. Rats were placed in a thermostatically controlled Plexiglas chamber (22 × 55 × 22 cm; maintained at 22–23°C) and exposed to a mixture of N2O/O2 (1:1; flow rate 2 liters/min) for the duration of the experiment. N2O/O2 exposure produces a transient state of tetrahydrofolate deficiency in the rat, resulting in formate accumulation after methanol administration (12). In the present studies, methanol [25% (wt/vol) methanol in saline] was administered i.p. to N2O/O2-treated rats at an initial dose of 4 g/kg, followed by supplemental doses of 1.5 g/kg at 24 and 48 h. This methanol intoxication protocol has been shown to produce a state of prolonged formic acidemia with formate concentrations between 5 and 8 mM in methanol-intoxicated rats, resulting in visual dysfunction (6, 7). Moreover, similar concentrations of blood formate over similar time periods have been shown to produce ocular toxicity experimentally in monkeys and have been associated with visual toxicity in human methanol intoxication (8, 9, 11). Formate concentrations were determined from tail vein blood samples by fluorometric analysis as described (6, 7, 13).
LED Treatment.
GaAlAs LED arrays of 670-nm wavelength (LED bandwidth 25–30 nm at 50% power) were obtained from Quantum Devices. Rats were placed in a Plexiglas restraint device (12.7 × 9 × 7.6 cm). The LED array was positioned directly over the animal at a distance of 1 inch, exposing the entire body. Treatment consisted of irradiation at 670 nm for 2 min and 24 s, resulting in a power intensity of 28 mW/cm2 and an energy density of 4 J/cm2 at 5, 25, and 50 h after the initial dose of methanol. These stimulation parameters (670 nm at energy density of 4 J/cm2) had been demonstrated to be beneficial for wound healing and to stimulate cellular proliferation and cytochrome oxidase activity in cultured visual neurons (19, 28).
ERG Procedures and Analyses.
ERG experiments were performed as described (6, 7). The light stimulation apparatus consisted of a three-beam optical system. All three beams were derived from tungsten-halide lamps (50 W, 12 V). Beam intensity was controlled by using neutral density step filters. ERG recordings were differentially amplified and computer-averaged. The amplified signal was processed through a two-stage active narrow bandpass filter (the half voltage of this filter was 0.2 times the center frequency). To ensure that any transients in the response that occur at the onset of the stimulus pulses were not included in the average, the initiation of signal averaging was delayed by a preset number of stimulus cycles (typically a minimum of 20). The resulting ERG is an extremely noise-free, single-cycle, sinusoidal waveform. The averaged responses were measured (peak-to-trough amplitude) from a calibrated digital oscilloscope display.
Before ERG analysis, ophthalmoscopic examination confirmed that all eyes were free of lenticular opacities or other gross anomalies. Rats were anesthetized with thiobutabarbitol sodium salt (100 mg/kg, i.p.), positioned in a Kopf stereotaxic apparatus, and placed on a heating pad to maintain core body temperature at 37°C. Atropine sulfate (0.05 mg/kg, s.c.) was administered to inhibit respiratory-tract secretions. The pupil of the eye to be tested was dilated by topical application of 1% atropine sulfate. Methylcellulose was topically applied as a lubricant and to enhance electrical conduction. A circular silver, wire recording electrode was positioned on the cornea, a reference electrode was placed above the eye, and a ground electrode was placed on the tongue. Recordings were obtained under ambient light conditions from cool white fluorescent room lights ≈100 cd/m2 at the rat's eye. Flickering stimuli (light/dark ratio = 0.25:0.75) were presented. Responses to 60 successive flashes were averaged for each stimulus condition. At each test wavelength, a minimum of four stimulus intensities spaced at intervals of 0.3 log unit were presented. The stimulus intensity yielding a 5-μV criterion response was determined by extrapolating between the two intensity points that bracketed the 5-μV response for each animal. All sensitivity measures were made in triplicate.
Two experimental protocols were used to evaluate retinal function (1).
15-Hz/510-nm ERG response.
ERGs were recorded in response to a 15-Hz flickering light at a wavelength of 510 nm over a 3-log unit range of light intensity. For these studies, the unattenuated stimulus (log relative retinal illumination = 0) had an irradiance of 25 μW distributed over the 70° patch of illuminated retina. This can be calculated to produce retinal illumination equivalent to ≈104 scotopic trolands. These recording conditions disadvantage rods; however, because at least 97% of rat photoreceptors are rods and ERGs are recorded at luminance intensities ranging from 101 to 104 scotopic trolands, it is likely that the responses to the 15-Hz/510-nm light are drawn from both rods and medium wavelength cones (M-cones) (6, 7, 29).
25-Hz/UV ERG response.
UV-sensitive cone responses were elicited by a 25-Hz flickering UV light (380-nm cutoff) in the presence of an intense chromatic adapting light (445 μW) that eliminated responses mediated by rods and M-cones (29). The 25-Hz/UV ERG responses were recorded over a 1.5-log unit range of light intensity. For these studies, the unattenuated stimulus (log relative retinal illumination = 0) had an irradiance of 25 μW distributed over the 70° patch of illuminated retina. This can be calculated to produce retinal illumination equivalent to about 104 scotopic trolands in the rat eye.
Histopathologic Analysis.
Retinal tissue was prepared for histology as described (6, 7). Thick sections (1 μ) for light microscopy were stained with toluidine blue; thin sections for electron microscopy were stained for uranyl acetate-lead citrate (6, 7).
Statistical Analysis.
All values are expressed as means ± SEM. A one-way ANOVA with Bonferroni's test was used to determine whether any significant differences existed among groups for blood formate concentrations. For ERG studies, a two-way ANOVA was performed. In all cases, the minimum level of significance was taken as P < 0.05.
Results
Blood Formate Accumulation in Methanol-Intoxicated Rats Is Not Altered by 670-nm LED Treatment.
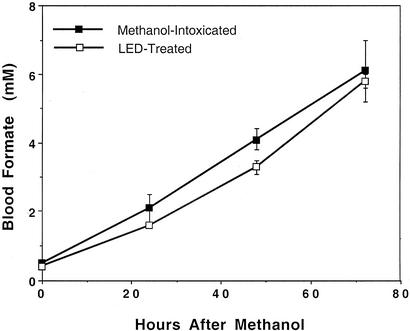
Formic acid is the toxic metabolite responsible for the retinal and optic nerve toxicity produced in methanol intoxication (5, 8, 12, 15). Linear increases in blood formate concentrations were observed in both methanol-intoxicated and LED-treated, methanol-intoxicated rats during the 72-h intoxication period (Fig. 1). In both treatment groups, blood formate concentrations increased 10-fold from endogenous concentrations of 0.5–0.6 mM before methanol administration to nearly 6 mM after 72 h of intoxication. The rate of formate accumulation and blood formate concentrations did not differ between the two treatment groups, indicating that LED treatment did not alter methanol or formate toxicokinetics. Similar increases in blood formate have been shown to disrupt retinal function in methanol-intoxicated rats (6, 7) and have been associated with visual toxicity in human methanol intoxication (8, 9).
Figure 1.
Photobiomodulation does not alter blood formate concentrations in methanol-intoxicated rats. Blood formate concentrations were determined before methanol administration and at 24-h intervals after methanol administration for 72 h. Shown are the mean values ± SEM from six rats in each experimental group. Blood formate concentrations did not differ between the methanol-intoxicated and LED-treated, methanol–intoxicated groups (P > 0.05).
Methanol-Induced Retinal Dysfunction Is Attenuated by 670-nm LED Treatment.
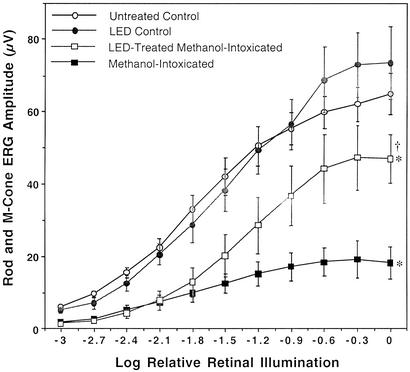
After 72 h of methanol intoxication, the function of rods and M-cones was assessed by recording the retinal response to a 15-Hz flickering light at wavelength of 510 nm (6, 7) (Fig. 2). In the untreated control group, 15-Hz/510-nm ERG amplitude increased linearly over the 3-log unit range of retinal illumination intensities, achieving a maximal amplitude of 65 ± 5 μV at maximal retinal illumination [0 log relative retinal illumination (LRRI) equivalent to 104 scotopic trolands]. A similar ERG response profile was observed in LED control animals. In both control groups a consistent 5-μV criterion threshold response was obtained at −3.0 ± 0.1 LRRI. In agreement with our previous studies, methanol intoxication produced a profound decrease in retinal sensitivity to light coupled with an attenuation of maximal ERG response amplitude (6, 7). The light intensity required to elicit a threshold (5 μV) 15-Hz/510-nm ERG response was increased by 0.6 log units to −2.4 ± 0.1 LRRI in methanol-intoxicated rats relative to control animals. In addition, the amplitudes of the flicker ERG responses were significantly attenuated at all luminance intensities, achieving a maximal amplitude of 18 ± 5 μV, ≈28% of the maximum control response. These changes are indicative of a severe deficit in retinal function and are consistent with formate-induced inhibition of photoreceptor oxidative metabolism (6, 7, 30–32). LED treatment significantly improved rod- and M-cone-mediated ERG responses in methanol-intoxicated rats. At lower luminance intensities (<1.5 LRRI), LED treatment had no effect on ERG response; however, at luminance intensities >1.5 LRRI, ERG responses were significantly greater in LED-treated rats compared with methanol-intoxicated animals. The maximal rod and M-cone in LED-treated rats was 47 ± 8 μV, 72% of the maximal control response. These data are indicative of a partial recovery of rod and M-cone function by LED photobiomodulation in methanol-intoxicated rats.
Figure 2.
Photobiomodulation improves rod and M-cone ERG response in methanol-intoxicated rats. Rod and M-cone (15 Hz/510 nm) ERG analysis was performed after 72 h of methanol intoxication. Shown are the mean values ± SEM from six rats in the untreated control, methanol-intoxicated, and LED-treated, methanol-intoxicated experimental groups and four rats from the LED control group. ERG responses in methanol-intoxicated and LED-treated, methanol-intoxicated rats were significantly lower than those measured in control rats (*, P < 0.001). ERG responses in LED-treated, methanol-intoxicated rats were significantly greater than those measured in methanol-intoxicated rats (†, P < 0.001).
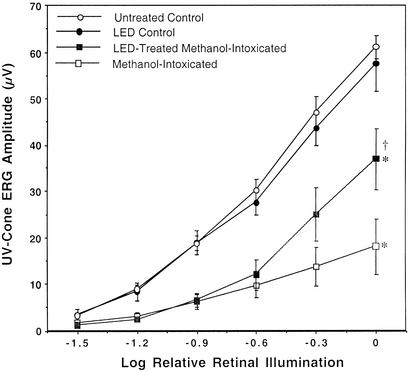
The function of UV-sensitive cones was examined by recording the retinal response to a 25-Hz flickering UV light (380-nm cutoff) in the presence of an intense chromatic adapting light. These conditions have been shown to isolate the UV-cone response in the rat retina (29). The effects of methanol intoxication and LED light treatment on UV-cone ERG responses are shown in Fig. 3. In untreated control animals the UV-cone-mediated ERG amplitude increased linearly from a 5-μV threshold value (−1.4 ± 0.03 LRRI) to a maximal value of 56 ± 3 μV over the 1.5-log unit range of retinal illumination used in these studies. LED-treated control animals exhibited a similar ERG response profile to that observed in untreated control animals. In methanol-intoxicated rats, the UV-cone ERG response was profoundly attenuated consistent with our previous studies (6, 7). The light intensity required to elicit a 5-μV response was increased by 0.5 log units to 0.9 ± 0.08 LRRI in intoxicated animals, and the maximal response amplitude was reduced to 18 ± 6 μV, 30% of the maximum control response. Similar to what we observed in the rod and M-cone ERG studies, LED treatment had no effect on UV-cone ERG response at lower luminance intensities, but significantly improved ERG response at higher luminance intensities. The maximal UV-cone ERG response in LED-treated rats was 37 ± 7 μV, 61% of the control response indicative of a partial recovery of UV-cone function by LED photobiomodulation.
Figure 3.
Photobiomodulation improves UV-cone ERG response in methanol-intoxicated rats. UV-cone (25 Hz/380 nm) ERG analysis was performed after 72 h of methanol intoxication. Shown are the mean values ± SEM from six rats in the control, methanol-intoxicated, and LED-treated, methanol-intoxicated experimental groups and four rats from the LED control group. UV-cone ERG responses were recorded from the same animals in which the rod and M-cone responses were recorded. ERG responses in methanol-intoxicated and LED-treated, methanol-intoxicated rats were significantly lower than those measured in control rats (*, P < 0.001). ERG responses in LED-treated, methanol-intoxicated rats were significantly greater than those measured in methanol-intoxicated rats (†, P < 0.05).
Methanol-Induced Retinal Histopathology Is Prevented by 670-nm LED Treatment.
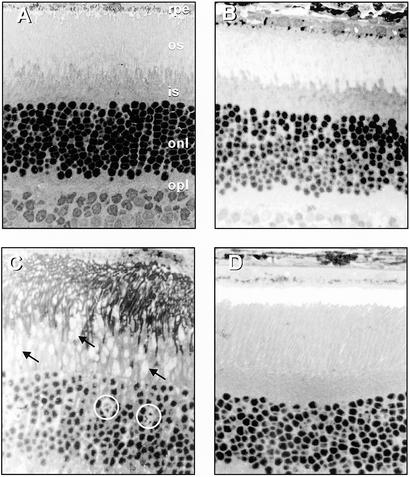
The architecture of the retina in methanol-intoxicated and LED-treated, methanol-intoxicated rats was evaluated by light and electron microscopy. These studies focused on the outer retina at the level of the photoreceptors based on our previous findings of outer retinal pathology and photoreceptor mitochondrial disruption after methanol intoxication (6, 7, 13). Fig. 4 illustrates outer retinal morphology in representative untreated control (Fig. 4A), LED control (Fig. 4B), methanol-intoxicated (Fig. 4C), and LED-treated, methanol-intoxicated (Fig. 4D) retinas. Pronounced histopathologic changes were apparent in the outer retina of methanol-intoxicated rats (Fig. 4C), including evidence of retinal edema, swelling of photoreceptor inner segments, and morphologic changes in photoreceptor nuclei. Retinal edema was evidenced by the spacing between the photoreceptor inner segments and by the spacing of the nuclei in the outer nuclear layer. Photoreceptor inner segments were profoundly swollen and enlarged, and photoreceptor nuclei in the outer nuclear layer appeared fragmented with irregularly stained chromatin. In contrast, LED-treated, methanol-intoxicated animals (Fig. 4D) exhibited retinal morphology that was indistinguishable from untreated control rats (Fig. 4A) and LED-treated control rats (Fig. 4B). In these animals outer retinal morphology was characterized by ordered photoreceptor inner segments with no evidence of vacuolization or swelling and the outer nuclear layer was compact with round and well-defined nuclei. The lack of retinal histopathology in LED-treated, methanol-intoxicated rats provides additional evidence of the retinoprotective actions of 670-nm LED treatment.
Figure 4.
Photobiomodulation protects retinal morphology in methanol-intoxicated rats. Outer retinal morphology in representative untreated control (A), LED control (B), methanol-intoxicated (C), and LED-treated, methanol-intoxicated (D) rats. Sections were taken from the posterior pole of the retina within two disk diameters of the optic nerve in any direction. (Toluidine blue, ×450.) (A) rpe, retinal pigment epithelium; os, photoreceptor outer segments; is, photoreceptor inner segments; onl, outer nuclear layer; opl, outer plexiform layer; ipl, inner plexiform layer. (B) The arrows indicate enlargement and swelling of the photoreceptor inner segments, and the circles indicate the fragmented appearance of photoreceptor nuclei. No histopathologic changes were apparent at the light microscopic level in the LED control or LED-treated, methanol-intoxicated groups.
The most obvious ultrastructural change observed in the outer retina of methanol-intoxicated rats was swelling and disruption of mitochondria in the inner segments of the photoreceptors. Some mitochondria were swollen and contained expanded cristae; other mitochondria were disrupted and showed no evidence of cristae (Fig. 5C). In contrast, mitochondria in the photoreceptor inner segments from LED-treated, methanol-intoxicated rats (Fig. 5D) exhibited normal morphology with well-defined cristae similar to inner segment mitochondrial morphology in untreated control rats (Fig. 5A) and LED-treated control rats (Fig. 5B). The absence of mitochondrial damage in photoreceptors of LED-treated, methanol-intoxicated rats strongly supports our hypothesis that 670-nm LED treatment preserved mitochondrial function.
Figure 5.
Photobiomodulation protects photoreceptor ultrastructure in methanol-intoxicated rats. Electron micrographs of the rod inner segment region in representative untreated control (A), LED control (B), methanol-intoxicated (C), and LED-treated, methanol-intoxicated (D) rats. The arrows indicate abnormal mitochondrial morphology in photoreceptor inner segments. Photoreceptor mitochondria from LED control or LED-treated, methanol-intoxicated rats exhibited normal morphology with well-defined cristae. (Magnifications: ×5,000.)
Discussion
Low-energy photon irradiation by light in the far-red to near-IR spectral range (630–1,000 nm) with low-energy lasers or LED arrays has been found to modulate various biological processes in cell culture and animal models (22–25). This phenomenon of photobiomodulation has been applied clinically in the treatment of soft tissue injuries and the acceleration of wound healing (19, 22). The mechanism of photobiomodulation by red to near-IR light at the cellular level has been ascribed to the activation of mitochondrial respiratory chain components, resulting in initiation of a signaling cascade that promotes cellular proliferation and cytoprotection (25, 27, 28). A comparison of the action spectrum for cellular proliferation after photoirradiation with the absorption spectrum of potential photoacceptors led Karu (25) to suggest that cytochrome oxidase is a primary photoreceptor of light in the red to near-IR region of the spectrum.
Recent studies conducted in primary neuronal cultures by our research group have shown that 670-nm LED photobiomodulation reversed the reduction in cytochrome oxidase activity produced by the blockade of voltage–dependent sodium channel function by tetrodotoxin and up-regulated cytochrome oxidase activity in normal neurons (28). The present studies extended these investigations to an in vivo system to determine whether 670-nm LED photobiomodulation would improve retinal function in an animal model of formate-induced mitochondrial dysfunction. Results of this study demonstrate the therapeutic benefit of photobiomodulation in the survival and functional recovery of the retina in vivo after acute injury by the mitochondrial toxin, formic acid generated in the course of methanol intoxication. We provide in vivo evidence that three brief postmethanol-intoxication treatments with 670-nm LED photoirradiation promotes the recovery of retinal function in rod and cone pathways and protects the retina from the histopathologic changes induced by methanol-derived formate. These findings provide a link between the actions of red to near-IR light on mitochondrial oxidative metabolism in vitro and retinoprotection in vivo.
Low-energy laser irradiation has documented benefits in promoting the healing of hypoxic, ischemic, and infected wounds (19, 22). However, lasers have limitations in beam width, wavelength capabilities, and size of wounds that can be treated (19). Heat generated from the laser light can damage biological tissue, and the concentrated beam of laser light may accidentally damage the eye. LED arrays were developed for National Aeronautics and Space Administration manned space flight experiments. In comparison to lasers, the patented LED technology generates negligible amounts of heat, is clinically proven to be safe, and has achieved nonsignificant risk status for human trials by the Food and Drug Administration (19). The wavelength, power, and energy parameters used in the present study are based on their beneficial effects for wound healing in humans (19) and stimulation of CO activity in cultured neuronal cells (28).
The retinoprotective actions of 670-nm LED treatment in the present study are consistent with the actions of formate as a mitochondrial toxin and the actions of 670-nm light on cytochrome oxidase activity. Formate has been shown to reversibly inhibit cytochrome oxidase activity with an apparent inhibition constant between 5 and 30 mM (16, 17). Blood formate concentrations in methanol-intoxicated rats in the present study fall within this range and retinal formate concentrations closely parallel blood formate concentrations (12). The functional and morphologic alterations produced in the retina by methanol-derived formate are indicative of formate-induced inhibition of photoreceptor mitochondrial energy metabolism. Photoreceptors are the most metabolically active cells in the body, and the energy required for phototransduction is derived primarily from oxidative metabolism (33, 34). The loss of retinal sensitivity to light and attenuation of ERG response in methanol-intoxicated rats are indicative of formate-induced inhibition of photoreceptor oxidative energy metabolism and are similar to the actions of other metabolic poisons in the retina (6, 31, 32). The observed mitochondrial swelling and disruption in the photoreceptor inner segments in methanol-intoxicated rats are consistent with a disruption of ionic homeostasis secondary to inhibition of cytochrome oxidase. Moreover, similar morphologic alterations have been reported in the retinas of patients with mitochondrial diseases that inhibit electron transport (35–37).
In the present study, the increase in ERG response and the lack of damage to photoreceptor mitochondria in LED-treated, methanol-intoxicated rats are indicative of a biostimulatory effect of 670-nm light on photoreceptor bioenergetics. A growing body of evidence suggests that cytochrome oxidase is a key photoacceptor of light in the far-red to near-IR spectral range (25, 38–40). Cytochrome oxidase is an integral membrane protein that contains four redox active metal centers and has a strong absorbance in the far-red to near-IR spectral range detectable in vivo by near-IR spectroscopy (41–43). Moreover, 660–680 nm of irradiation has been shown to increase electron transfer in purified cytochrome oxidase (40), increase mitochondrial respiration and ATP synthesis in isolated mitochondria (39), and up-regulate cytochrome oxidase activity in cultured neuronal cells (28). An up-regulation of retinal cytochrome oxidase by LED treatment would effectively counteract the inhibitory actions of formate on retinal oxidative metabolism, thus improving retinal function. Although retinal function was improved in LED-treated rats, it was not restored to control response levels. At lower luminance intensities, LED treatment did not improve the ERG response in methanol-intoxicated rats, suggesting that the rate of activation of some components of phototransduction activation remained compromised by formate. Because the rate of activation of phototransduction depends on an adequate supply of GTP and ATP (30–32), it is possible that the formate-induced metabolic inhibition is only partly attenuated by our LED treatment protocol.
The prolonged effect of three brief LED treatments in mediating the retinoprotective actions in methanol intoxication suggests that 670-nm LED photostimulation induces a cascade of signaling events initiated by the initial absorption of light by cytochrome oxidase. These signaling events may include the activation of immediate early genes, transcription factors, cytochrome oxidase subunit gene expression, and a host of other enzymes and pathways related to increased oxidative metabolism (25, 28, 44). In addition to increased oxidative metabolism, red to near-IR light stimulation of mitochondrial electron transfer is known to increase the generation of reactive oxygen species (25). These mitochondrially generated reactive oxygen species may function as signaling molecules to provide communication between mitochondria and the cytosol and nucleus and thus play an important signaling role in the activation of retinoprotective processes after LED treatment (45).
The results of this study and others suggest that photobiomodulation with red to near-IR light augments recovery pathways promoting neuronal viability and restoring neuronal function after injury. Importantly, there was no evidence of damage to the normal retina after 670-nm LED treatment. Based on these findings, we suggest that photobiomodulation may represent an innovative and novel therapeutic approach for the treatment of retinal injury and the treatment of retinal diseases, including age-related macular degeneration, glaucoma, diabetic retinopathy, and Leber's hereditary optic neuropathy.
Acknowledgments
We thank Dr. Kurt Henry for helpful discussions and suggestions and Anna Fekete for excellent technical assistance. We also gratefully acknowledge the technical support of Quantum Devices, Inc., for providing the LED arrays for this project. This work was supported by Defense Advanced Research Projects Agency Grant N66001-01-1-8969 (to H.T.W.), National Institute of Environmental Health Sciences Grant ES06648 (to J.T.E.), National Eye Institute Core Grant P30-EY01931 (to J.T.E. and M.T.T.W.-R., Core Investigators), National Eye Institute Grants EY11396 (to J.T.E.) and EY05439 (to M.T.T.W.-R.), and the Bleser Foundation Endowed Professorship (to H.T.W.).
Abbreviations
- LED
light-emitting diode
- ERG
electroretinogram
- LRRI
log relative retinal illumination
Footnotes
This paper was submitted directly (Track II) to the PNAS office.
References
- 1.Rizzo J F. Neurology. 1995;45:11–16. doi: 10.1212/wnl.45.1.11. [DOI] [PubMed] [Google Scholar]
- 2.Baron M J, Johnson M A, Andrews R M, Clarke M P, Griffiths P G, Bristow E, He L P, Durham S, Turnbull D M. Invest Ophthalmol Visual Sci. 2001;42:3016–3022. [PubMed] [Google Scholar]
- 3.Carelli V, Ross-Cisneros F N, Sadun A A. Neurochem Int. 2002;40:573–584. doi: 10.1016/s0197-0186(01)00129-2. [DOI] [PubMed] [Google Scholar]
- 4.Hayreh M M, Hayreh S S, Baumbach G L, Cancilla P, Martin-Amat G, Tephly T R. In: Neurotoxicity of the Visual System. Merigan W, Weiss B, editors. New York: Raven; 1980. pp. 35–53. [Google Scholar]
- 5.Martin-Amat G, Tephly T R, McMartin K E, Makar A B, Hayreh M M, Hayreh S S, Baumbach G, Cancilla P. Arch Ophthalmol. 1977;95:1847–1850. doi: 10.1001/archopht.1977.04450100149021. [DOI] [PubMed] [Google Scholar]
- 6.Seme M T, Summerfelt P M, Henry M M, Neitz J, Eells J T. J Pharmacol Exp Ther. 1999;289:361–370. [PubMed] [Google Scholar]
- 7.Seme M T, Summerfelt P, Henry M M, Neitz J, Eells J T. Invest Ophthalmol Visual Sci. 2001;42:834–841. [PubMed] [Google Scholar]
- 8.Eells J T. In: Browning's Toxicity and Metabolism of Industrial Solvents: Alcohols and Esters. Thurman R G, Kaufmann F C, editors. IV. Amsterdam: Elsevier; 1992. pp. 3–15. [Google Scholar]
- 9.Kavet R, Nauss K. Crit Rev Toxicol. 1990;21:21–50. doi: 10.3109/10408449009089872. [DOI] [PubMed] [Google Scholar]
- 10.Sharpe J, Hostovsky M, Bilbao J, Rewcastle N B. Neurology. 1982;32:1093–1100. doi: 10.1212/wnl.32.10.1093. [DOI] [PubMed] [Google Scholar]
- 11.Ingemansson S O. Acta Ophthalmol. 1983;158,Suppl.:5–12. [PubMed] [Google Scholar]
- 12.Eells J T, Henry M M, Lewandowski M F, Seme M T, Murray T G. Neurotoxicology. 2000;21:321–330. [PubMed] [Google Scholar]
- 13.Murray T G, Burton T C, Rajani C, Lewandowski M F, Burke J M, Eells J T. Arch Ophthalmol. 1991;109:1012–1016. doi: 10.1001/archopht.1991.01080070124049. [DOI] [PubMed] [Google Scholar]
- 14.Lee E W, Garner C D, Terzo T S. Toxicol Appl Pharmacol. 1994;128:199–206. doi: 10.1006/taap.1994.1198. [DOI] [PubMed] [Google Scholar]
- 15.Martin-Amat G, McMartin K E, Hayreh S S, Hayreh M, Tephly T R. Toxicol Appl Pharmacol. 1978;45:201–208. doi: 10.1016/0041-008x(78)90040-6. [DOI] [PubMed] [Google Scholar]
- 16.Nicholls P. Biochem Biophys Res Commun. 1975;67:610–616. doi: 10.1016/0006-291x(75)90856-6. [DOI] [PubMed] [Google Scholar]
- 17.Nicholls P. Biochim Biophys Acta. 1976;430:13–29. doi: 10.1016/0005-2728(76)90218-8. [DOI] [PubMed] [Google Scholar]
- 18.Wong-Riley M T T. Trends Neurosci. 1989;12:94–101. doi: 10.1016/0166-2236(89)90165-3. [DOI] [PubMed] [Google Scholar]
- 19.Whelan H T, Smits R L, Buchmann E V, Whelan N T, Turner S G, Margolis D A, Cevenini V, Stinson H, Ignatius R, Martin T, et al. J Clin Laser Med Surg. 2001;19:305–314. doi: 10.1089/104454701753342758. [DOI] [PubMed] [Google Scholar]
- 20.Oron U, Yaakobi T, Oron A, Hayam G, Gepstein L, Rubin O, Wolf T, Ben Haim S. Lasers Surg Med. 2001;28:204–211. doi: 10.1002/lsm.1039. [DOI] [PubMed] [Google Scholar]
- 21.Assa E M, Rosner M, Belkin M, Solomon A, Schwartz M. Brain Res. 1989;476:205–212. doi: 10.1016/0006-8993(89)91240-7. [DOI] [PubMed] [Google Scholar]
- 22.Conlan M J, Rapley J W, Cobb C M. J Clin Periodont. 1996;23:492–496. doi: 10.1111/j.1600-051x.1996.tb00580.x. [DOI] [PubMed] [Google Scholar]
- 23.Yu W, Naim J O, Lanzafame R J. Lasers Surg Med. 1997;20:56–63. doi: 10.1002/(sici)1096-9101(1997)20:1<56::aid-lsm9>3.0.co;2-y. [DOI] [PubMed] [Google Scholar]
- 24.Sommer A P, Pinheiro A L, Mester A R, Franke R P, Whelan H T. J Clin Laser Med Surg. 2001;19:27–33. doi: 10.1089/104454701750066910. [DOI] [PubMed] [Google Scholar]
- 25.Karu T. J Photochem Photobiol. 1999;49:1–17. doi: 10.1016/S1011-1344(98)00219-X. [DOI] [PubMed] [Google Scholar]
- 26.Leung M C P, Lo S C L, Siu F K W, So K F. Lasers Surg Med. 2002;31:283–288. doi: 10.1002/lsm.10096. [DOI] [PubMed] [Google Scholar]
- 27.Grossman N, Schneid N, Reuveni H, Lubart R. Lasers Surg Med. 1998;22:212–218. doi: 10.1002/(sici)1096-9101(1998)22:4<212::aid-lsm5>3.0.co;2-s. [DOI] [PubMed] [Google Scholar]
- 28.Wong-Riley M T T, Bai X, Buchmann E, Whelan H T. NeuroReport. 2001;12:3033–3037. doi: 10.1097/00001756-200110080-00011. [DOI] [PubMed] [Google Scholar]
- 29.Jacobs G, Neitz J, Deegan J. Nature. 1991;353:655–656. doi: 10.1038/353655a0. [DOI] [PubMed] [Google Scholar]
- 30.Koskelainen A, Donner K, Kalamkarov G, Hemila S. Vision Res. 1994;34:983–994. doi: 10.1016/0042-6989(94)90002-7. [DOI] [PubMed] [Google Scholar]
- 31.Findl O, Hansen R, Fulton A. Invest Ophthalmol Visual Sci. 1995;36:1019–1026. [PubMed] [Google Scholar]
- 32.Fox D A, Katz L. Vision Res. 1992;32:249–255. doi: 10.1016/0042-6989(92)90134-5. [DOI] [PubMed] [Google Scholar]
- 33.Ames A, III, Li Y, Heher E C, Kimble C R. J Neurosci. 1992;12:840–853. doi: 10.1523/JNEUROSCI.12-03-00840.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ames A., III Can J Physiol Pharmacol. 1992;70:S158–S164. doi: 10.1139/y92-257. [DOI] [PubMed] [Google Scholar]
- 35.McKelvie P A, Morley J B, Byrne E, Marzuki S. J Neurol Sci. 1991;102:51–60. doi: 10.1016/0022-510x(91)90093-m. [DOI] [PubMed] [Google Scholar]
- 36.Rapp L M, Tolman B L, Dhindsa H S. Invest Ophthalmol Visual Sci. 1990;31:1186–1190. [PubMed] [Google Scholar]
- 37.Runge P, Calver D, Marshall J, Taylor D. Br J Ophthalmol. 1986;70:782–796. doi: 10.1136/bjo.70.10.782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Yu W, Naim J O, McGowan M, Ippolito K, Lanzafame R J. J Photochem Photobiol. 1997;66:866–871. doi: 10.1111/j.1751-1097.1997.tb03239.x. [DOI] [PubMed] [Google Scholar]
- 39.Passarella S, Casamassima E, Molinari S, Pastore D, Quagliariello E, Catalino I M, Cingolani A. FEBS Lett. 1984;175:95–99. doi: 10.1016/0014-5793(84)80577-3. [DOI] [PubMed] [Google Scholar]
- 40.Pastore D, Greco M, Passarella S. Int J Radiat Biol. 2000;76:863–870. doi: 10.1080/09553000050029020. [DOI] [PubMed] [Google Scholar]
- 41.Cooper C E, Springett R. Philos Trans R Soc London B. 1977;352:9–676. doi: 10.1098/rstb.1997.0048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Beauvoit B, Evans S M, Jenkins T W, Miller E E, Chance B. Anal Biochem. 1995;226:167–174. doi: 10.1006/abio.1995.1205. [DOI] [PubMed] [Google Scholar]
- 43.Beauvoit B, Kitai T, Chance B. Biophys J. 1994;67:2501–2510. doi: 10.1016/S0006-3495(94)80740-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Zhang C, Wong-Riley M. Eur J Neurosci. 2000;12:1013–1023. doi: 10.1046/j.1460-9568.2000.00997.x. [DOI] [PubMed] [Google Scholar]
- 45.Nemoto S, Takeda K, Yu Z X, Ferrans V J, Finkel T. Mol Cell Biol. 2000;20:7311–7318. doi: 10.1128/mcb.20.19.7311-7318.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]