Abstract
Francisella tularensis is a highly infectious, facultative intracellular bacterium which causes epidemics of tularemia in both humans and mammals at regular intervals. The natural reservoir of the bacterium is largely unknown, although it has been speculated that protozoa may harbor it. To test this hypothesis, Acanthamoeba castellanii was cocultured with a strain of F. tularensis engineered to produce green fluorescent protein (GFP) in a nutrient-rich medium. GFP fluorescence within A. castellanii was then monitored by flow cytometry and fluorescence microscopy. In addition, extracellular bacteria were distinguished from intracellular bacteria by targeting with monoclonal antibodies. Electron microscopy was used to determine the intracellular location of F. tularensis in A. castellanii, and viable counts were obtained for both extracellular and intracellular bacteria. The results showed that many F. tularensis cells were located intracellularly in A. castellanii cells. The bacteria multiplied within intracellular vacuoles and eventually killed many of the host cells. F. tularensis was found in intact trophozoites, excreted vesicles, and cysts. Furthermore, F. tularensis grew faster in cocultures with A. castellanii than it did when grown alone in the same medium. This increase in growth was accompanied by a decrease in the number of A. castellanii cells. The interaction between F. tularensis and amoebae demonstrated in this study indicates that ubiquitous protozoa might be an important environmental reservoir for F. tularensis.
Francisella tularensis, a gram-negative, nonsporulating, nonmotile, and capsulated coccobacillus, is a facultative intracellular bacterium which causes tularemia in humans and animals (37). Inoculation or inhalation of as few as 10 F. tularensis organisms may cause disease in humans (35, 36), and because of its high virulence and contagiousness, the bacterium is considered a possible bioterrorism agent (7). It has been isolated from approximately 250 wildlife species (37), but its principal natural reservoir is largely unknown, although studies have shown that the organism may persist for more than a year in water or mud (30).
Virtually nothing is known about the virulence mechanisms of F. tularensis or about how it survives within host cells. Even the avirulent live vaccine strain (LVS), which has been used as a human vaccine (34), is strongly pathogenic for certain animals and causes a lethal infection in mice that is indistinguishable from human disease (8). It has been shown that LVS is very well adapted to the intracellular environment of macrophages, survives in phagosomes (3, 13), and exerts a cytopathogenic effect on murine macrophages (3a, 5, 13) Furthermore, it has been found that LVS localizes within an acidic vesicle, which facilitates its iron uptake (11), and that LVS releases an acid phosphatase that inhibits the respiratory burst in neutrophils (33). Recently, it has also been demonstrated that infection with the LVS strain induces apoptosis in murine macrophages (24).
Free-living amoebae such as Acanthamoeba species are commonly found in natural aquatic systems (25). As a part of biofilms in aquatic environments, free-living amoebae and bacteria are involved in complex interactions. Francisella species are also known to be connected with natural water systems (18, 30), and it is well known that Acanthamoeba species are environmental hosts of several intracellular pathogens, such as Legionella, Chlamydia, and Mycobacterium (2, 26, 38, 39). Legionella cells interact with their protozoan hosts and mammalian cells in a similar way. The known genetic factors required by Legionella to infect protozoa are also required for the infection process in mammalian cells (16, 17). Previous studies of the interaction between F. tularensis and Acanthamoeba castellanii have shown that growth of F. tularensis is enhanced in media preconditioned by amoebae (15). Here, we have tested the hypothesis that protozoa may comprise a significant environmental reservoir for F. tularensis.
MATERIALS AND METHODS
Microorganisms and plasmid construction.
A. castellanii (ATCC 30234) was obtained from the American Type Culture Collection (ATCC), Manassas, Va., and F. tularensis LVS (type B) was obtained from the U.S. Army Medical Research Institute of Infectious Diseases, Fort Detrick, Md. F. tularensis LVS carrying a destabilized form of green fluorescent protein (GFP) was constructed as follows. First, the promoter for GroEL from F. tularensis LVS (9) was amplified by PCR, cloned into the SmaI-PstI sites upstream of the chloramphenicol acetyltransferase (CAT) gene in pKK214 (23, 29), and then introduced into F. tularensis LVS by cryotransformation (31). The resulting plasmid was designated pKK214CAT and was used as the basic construct in the present work. A mutant form (M2) of wild-type GFP (6) was amplified by PCR and cloned into the PstI-EcoRI sites of the pKK214CAT plasmid under the control of the GroEL promoter. Because the EcoRI site is inside the CAT gene, this procedure led to the partial removal of the CAT gene. The resulting plasmid was designated pKK214GFP. Next, a destabilized variant (ASV) of GFP (Clontech, Palo Alto, Calif.) was amplified by PCR and cut with Bsp1407I-EcoRI, and the resulting Bsp1407I-EcoRI fragment was cloned into pKK214GFP cut with the same enzymes. This resulted in substitution of the C-terminal part of GFP (M2 form) for the destabilized C-terminal form (ASV), which contains sequences encoding protease targets responsible for the rapid degradation of the expressed protein. This construct was designated pKK214GFP/ASV. To determine the half-life of this GFP/ASV construction in F. tularensis LVS, samples containing 2.0 × 109 CFU/ml were inactivated by treatment with 250 μg of gentamicin (Sigma, St. Louis, Mo.) per ml for 1 h at room temperature in darkness. After confirming that the cells were unable to grow, as determined by viable counts, following this treatment, viable count and flow cytometry analyses were carried out in parallel for 7 days. No growth on modified Thayer-Martin agar was observed, and the fluorescence gradually decreased.
Culture media and growth conditions.
A. castellanii was grown without shaking at 30°C to a final concentration of 106/ml in ATCC medium no. 712 (ATCC). Modified Thayer-Martin agar plates containing 36 g of GC base medium (Difco Laboratories, Detroit, Mich.) per liter, 10 g of hemoglobin (Difco) per liter, 10 mg of IsoVitaleX (BBL Microbiology Systems, Cockeysville, Md.) per liter, and 10 mg of tetracycline (Sigma) per liter were used for viable counts and growth of F. tularensis LVS/GFP/ASV. After the inoculum was spread as serial dilutions, the agar plates were incubated at 37°C in 5% CO2 for at least 2 days if not otherwise stated. Cocultures of F. tularensis LVS/GFP/ASV and A. castellanii were incubated in Falcon tissue culture flasks (75 cm2) filled with 50 ml of ATCC medium 712 containing 20 μg of tetracycline per ml and an initial concentration of 105 A. castellanii cells and 106 F. tularensis cells per ml. Control flasks with the microorganisms cultured separately were prepared in the same way and with the same initial concentrations. The flasks were incubated at 30°C without shaking. Samples were withdrawn regularly for electron microscopy, flow cytometry, and fluorescence microscopy analysis and to obtain viable counts.
Flow cytometry analysis.
The flow cytometer (FACSort; Becton Dickinson Immuno Systems, San Jose, Calif.), equipped with an argon laser giving a 488-nm primary emission line, was calibrated with unlabeled and labeled beads (Becton Dickinson) and FACSComp software (Becton Dickinson). Unlabeled cells were adjusted for forward scatter (relative size), side scatter (relative granularity), FL1 (green color), FL2 (red color), and FL3 (deep red color). The measuring time per sample was 15 to 50 s, with a medium flow rate of 60 μl/min. From each sample 10,000 events were registered, and data were analyzed with Cell Quest software (Becton Dickinson). Samples (3 ml) of cell suspension from the coculture flasks were centrifuged for 10 min at 300 × g in a model TJ6 centrifuge (Beckman Instruments, Palo Alto, Calif.) and washed six times with FacsWash solution (Becton Dickinson) prior to the analyses.
Microscopy analysis.
A. castellanii cells were counted in a Bürker counting chamber (Merck Eurolab, Stockholm, Sweden) under a light microscope (Leica Microscopy Systems, Heerburgg, Switzerland), while the abundance and distribution of F. tularensis LVS/GFP/ASV were analyzed by fluorescence microscopy (Leica Microscopy Systems). Prior to analysis, using an oil immersion lens and a green filter, 2-ml samples of cell suspension from the coculture flask were centrifuged for 10 min at 300 × g in a Beckman model TJ6 centrifuge, and the resulting pellets were washed six times with FacsWash solution.
Antibody labeling of extracellular F. tularensis LVS/GFP/ASV was performed by adding 10 μl of biotin-labeled antibodies, specific for F. tularensis LVS (German Armed Forces Medical Academy, Munich, Germany), to 1-ml samples of cell suspension from coculture flasks. The samples were incubated for 20 min at room temperature, washed, reincubated for 20 min with 10 μl of R-phycoerythrin-conjugated Streptoavidin (DAKO, Glostrup, Denmark), washed again, and examined under the fluorescence microscope.
For electron microscopy, 2-ml samples of cell suspension from the coculture flasks were centrifuged for 10 min at 300 × g in a Beckman model TJ6 centrifuge, and the resulting pellets were washed six times with FacsWash solution. Each pellet of infected amoebae was fixed with 2.5% glutaraldehyde in 0.1 M sodium cacodylate buffer (pH 7.3) for 2 h at room temperature. The samples were then washed twice in the same buffer and fixed in 1% reduced osmium tetroxide for 1 h. The specimens were centrifuged into pellets, which were embedded in a 2% solution of agarose at 45°C. The solidified agarose containing the amoebae was cut into small cubes, which were dehydrated in graded acetone and embedded in an Epon-Araldite mixture. Ultrathin sections were stained with uranyl acetate and lead citrate and examined with a transmission electron microscope (EM 900; Carl Zeiss, Oberkochen, Germany).
Analysis of viable F. tularensis within A. castellanii.
Samples (3 ml) of cell suspensions from coculture flasks were centrifuged for 10 min at 300 × g in a Beckman model TJ6 centrifuge and washed six times with FacsWash solution to minimize extracellular F. tularensis contamination. The pellets were resuspended in 500 μl of FacsWash solution and incubated with 250 μg of gentamicin per ml for 1 h at room temperature. Next, the samples were centrifuged for 10 min at 300 × g in a Beckman model TJ6 centrifuge, and 100-μl portions of the supernatant were spread on modified Thayer-Martin agar plates. Each pellet was diluted twofold with 0.5% sodium deoxycholate and incubated for 5 min at room temperature, after which series of 10-fold dilutions from 101 to 104 were prepared and spread on modified Thayer-Martin agar.
RESULTS
GFP fluorescence from F. tularensis in A. castellanii.
Prior to the analyses of GFP fluorescence from F. tularensis in A. castellanii, we determined the half-life of the destabilized form (ASV) of the GFP expressed in F. tularensis LVS/GFP/ASV. The half-life was found to be approximately 34 h. This ensured that viable cells were measured, since dying cells would show lower fluorescence intensity with time.
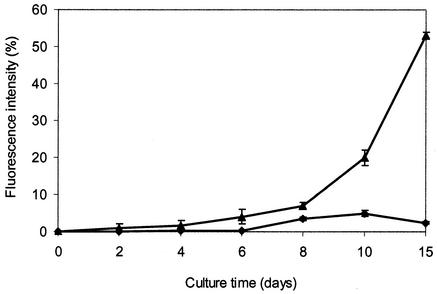
Flow cytometer analysis of samples taken from the flasks containing both F. tularensis LVS/GFP/ASV and A. castellanii showed that the fluorescence intensity increased with time in the A. castellanii population, from 0% at day 0 to 54% at day 15 (Fig. 1).
FIG. 1.
Changes in GFP fluorescence over time in cell populations of A. castellanii infected with F. tularensis LVS/GFP/ASV (triangles) and autofluorescence from A. castellanii (squares), measured by flow cytometry. Mean values from two independent experiments are shown (t test, P < 0.05). Bars show averages of the absolute deviations of data points from their mean.
Intracellular location of F. tularensis in A. castellanii.
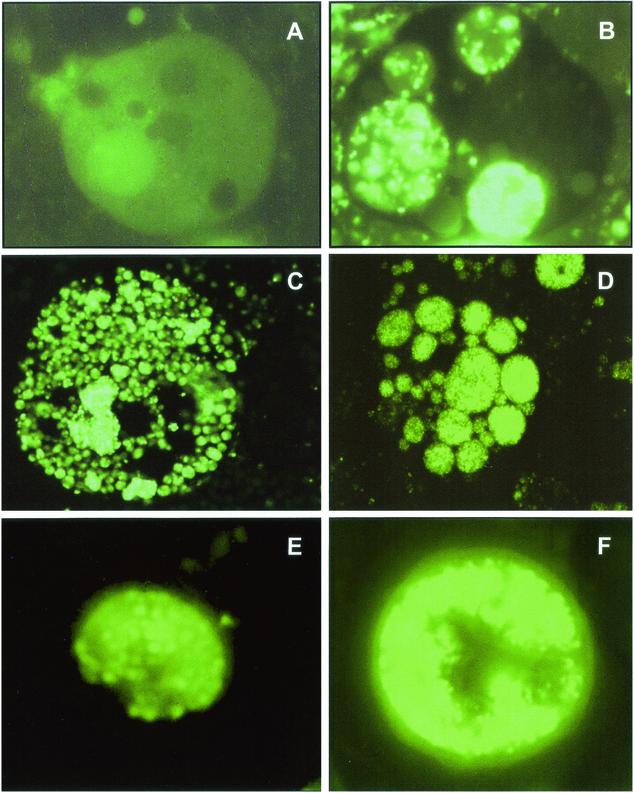
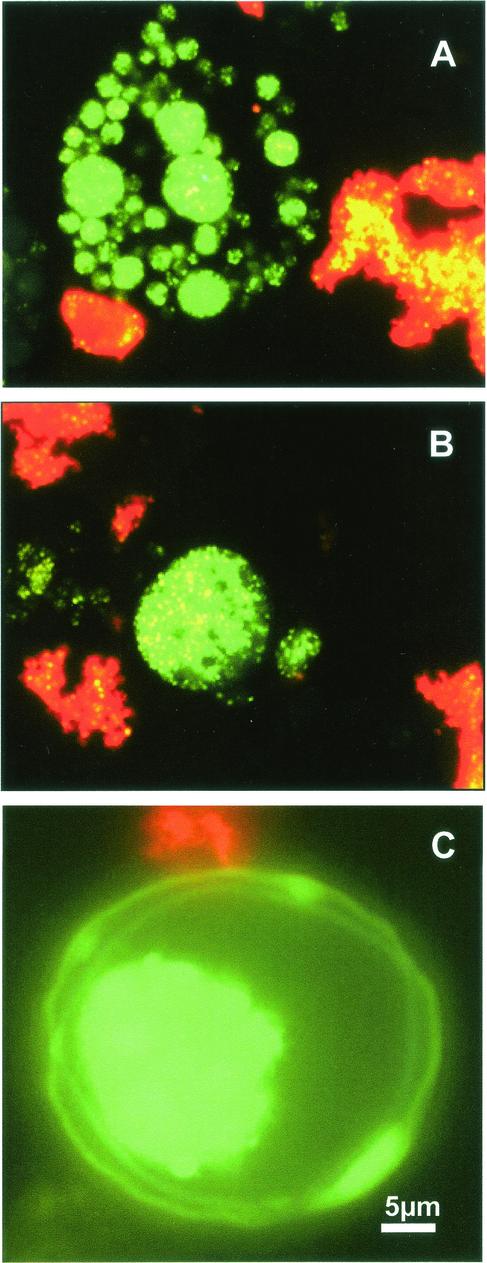
Samples taken from cocultures of F. tularensis LVS/GFP/ASV and A. castellanii showed an increase in the numbers of intracellular bacteria with time (Fig. 2). Moreover, different stages of infection were observed, including growth in intracellular-membrane-limited vacuoles, release of vesicles, and cysts containing bacteria. Samples taken at day 18 from the coculture were mixed with R-phycoerythrin-labeled antibodies specific for F. tularensis, and the antibody-directed staining was visualized by fluorescence microscopy. The results showed that GFP-labeled bacteria within A. castellanii were not accessible to the antibodies and hence exhibited green fluorescence. In contrast, extracellular bacteria were bound by the antibodies and thus exhibited red fluorescence. This demonstrated that many of the F. tularensis cells were located intracellularly (Fig. 3). The fluorescence microscopy also showed that F. tularensis-infected amoebae disintegrated as vesicles inside them filled with F. tularensis and that bacteria occurred within cysts (Fig. 2 and 3).
FIG. 2.
Fluorescence microscopy analysis. (A) A. castellanii trophozoite without intracellular F. tularensis (day 0). (B) Intact A. castellanii with Francisella-filled vacuoles (day 10). (C) Disintegrating A. castellanii filled with F. tularensis LVS/GFP/ASV (day 15). (D) Francisella-filled vesicles, enclosed within the cell membrane of a dead A. castellanii trophozoite (day 18). (E) Francisella-filled vesicle (day 18). (F) A. castellanii cyst containing F. tularensis LVS/GFP/ASV inside the double wall (day 40).
FIG. 3.
Differentiation between extracellular and intracellular F. tularensis by use of monoclonal antibodies. Viable intracellular F. tularensis LVS/GFP/AVS cells expressing GFP appear green, while extracellular F. tularensis cells appear red after treatment with labeled antibodies specific for F. tularensis. (A) Disintegrating A. castellanii trophozoite containing Francisella-filled vesicles (day 18). (B) Individual vesicle containing viable F. tularensis GFP/LVS/ASV (day 18). (C) A. castellanii cyst containing viable F. tularensis inside the cyst double wall (day 40).
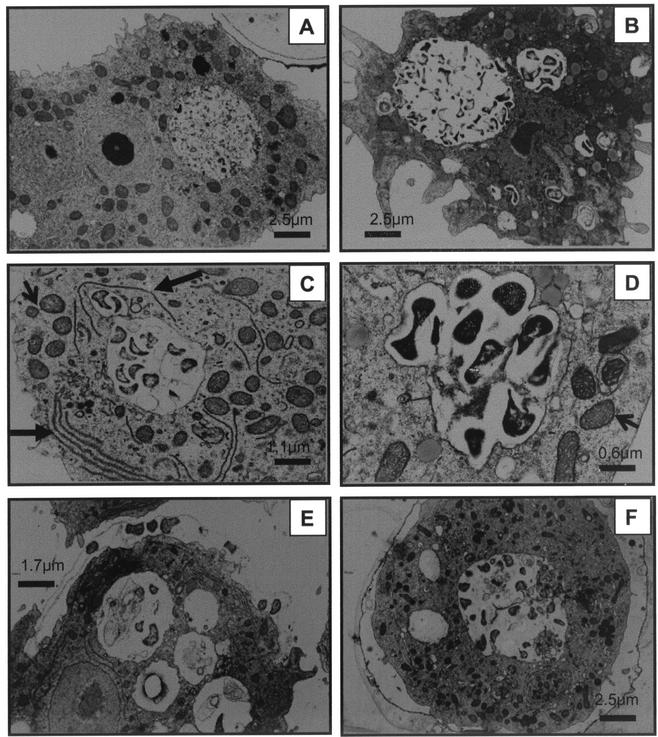
Electron micrographs confirmed that many F. tularensis cells were located within vacuoles in A. castellanii (Fig. 4). The vacuoles containing bacteria seemed to attract amoebal organelles such as mitochondria and rough endoplasmic reticulum (Fig. 4C and D) As shown in Fig. 4E, F. tularensis cells could be seen lining up between an emerging double wall, which is a sign of encystation. However, another outcome was also observed in some cases (Fig. 2F, 3C, and 4F), in which all the bacteria seemed to be located inside the double wall of the cyst.
FIG. 4.
Electron microscopy analysis. (A) A. castellanii trophozoite without intracellular F. tularensis (day 0). (B) A. castellanii trophozoite with Francisella-filled vacuoles (day 9). (C and D) Recruitment of mitochondria (short arrows) and rough endoplasmic reticulum (long arrows) to the vacuole containing bacteria. (E) A. castellanii trophozoite undergoing encystation with F. tularensis cells lined up between the two layers of the emerging double wall (day 16). (F) A. castellanii cyst containing F. tularensis on the inside of the double wall (day 16).
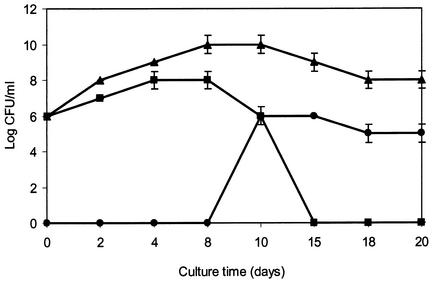
Growth of cocultures of F. tularensis LVS/GFP/ASV and A. castellanii.
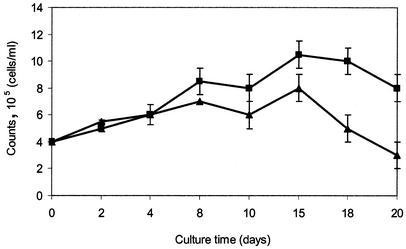
Viable counts of extracellular F. tularensis LVS/GFP/ASV increased in the presence of A. castellanii from 2 × 106 CFU/ml at day 0 to 2 × 109 CFU/ml at day 15. In contrast, viable counts of F. tularensis LVS/GFP/ASV cultured alone decreased from 2 × 106 CFU/ml at day 0 to nondetectable levels at day 15 (Fig. 5). Differences between the numbers of A. castellanii cells in cultures with or without F. tularensis LVS/GFP/ASV were also apparent. The total counts, according to Bürker chamber determinations, showed that the numbers of A. castellanii cells increased from 4 × 105 cells/ml at day 0 to 8 × 105 cells/ml at day 20 when cultured alone and decreased from 4 × 105 cells/ml at day 0 to 3 × 105 cells/ml at day 20 when cocultured with F. tularensis LVS/GFP/ASV (Fig. 6).
FIG. 5.
Viable counts of F. tularensis cultured alone (squares), F. tularensis cocultured with A. castellanii (triangles), and intracellular F. tularensis (circles). Mean values from two independent experiments are shown (t test, P < 0.05). Bars show averages of the absolute deviations of data points from their mean.
FIG. 6.
Counts of A. castellanii cultured with F. tularensis (triangles) and without F. tularensis (squares) over time. Mean values from two independent experiments are shown (t test, P < 0.05). Bars show averages of the absolute deviations of data points from their mean.
The viability of the F. tularensis cells within A. castellanii was analyzed by taking viable counts of the bacteria after gentamicin treatment to kill extracellular bacteria followed by deoxycholate treatment of the A. castellanii cells to release the intracellular bacteria. No bacteria were recovered from gentamicin-treated medium, but in A. castellanii cells, an increase in F. tularensis LVS/GFP/ASV viable counts was observed over time, from 0 cells/ml at days 0, 2, 4, and 8 to 2 × 106 cells/ml at day 15 (Fig. 5).
DISCUSSION
F. tularensis is a highly infectious and facultative intracellular bacterium that causes various types of tularemia in mammals (18). It has been considered a potential biological weapon and possible bioterrorism agent (7), so its survival in nature is of interest from an epidemiological perspective. The main reservoir of the bacterium is not known, but it has been shown that other intracellular bacteria, such as Legionella, Mycobacterium, and Chlamydia, utilize protozoa as natural reservoirs (2, 26, 38). In this context, it has been shown that growth of F. tularensis is enhanced in media preconditioned by A. castellanii (15). It has also been speculated that F. tularensis may persist in A. castellanii (4).
In the present study, we therefore aimed to study the interaction between F. tularensis and A. castellanii more thoroughly. The results show for the first time that F. tularensis can survive and grow within A. castellanii. The infection process begins when trophozoites engulf F. tularensis cells, which replicate and grow in vacuole structures inside the trophozoites. Thus, the infection process in amoebae shows a resemblance to Francisella infection in macrophages (3, 11). Our ultrastructural examinations showed that growth of F. tularensis in A. castellanii resulted in early changes in the amoebae, such as disappearance of the nucleus and condensation of the cytoplasm (Fig. 4). Moreover, cell organelles such as mitochondria and endoplasmic reticulum were recruited to the vacuoles containing bacteria (Fig. 4C and D). This phenomenon has also been observed in A. castellanii infected with Legionella (1). Infected trophozoites were found both intact, filled with vacuoles containing F. tularensis, and in the process of cytolysis, excreting vesicles containing F. tularensis. Some infected trophozoites were also seen undergoing encystation, with two observed sequences of events: in one F. tularensis was contained inside the double wall, while in the other F. tularensis cells lined up in the space between the layers of the double wall (Fig. 3 and 4), as previously described for Mycobacterium avium and Simkania negevensis (22, 38). Thus, taking the observations together, the infection cycle of F. tularensis in A. castellanii seems to display many features in common with Legionella infection in A. castellanii (17).
Viable counts of cocultured F. tularensis showed that the presence of A. castellanii enhanced its growth. This finding is in accordance with previous results (15) and is probably due to the F. tularensis using CO2 produced from live A. castellanii cells and nutrients derived from dead ones. In addition, intracellular F. tularensis may escape into the culture medium after lysis of the A. castellanii cells.
Counts of A. castellanii cells showed that there were 25% fewer cells when they were cocultured with F. tularensis than when they were grown alone, apparently because F. tularensis killed a substantial number of them. Furthermore, the increase of fluorescence inside A. castellanii cells with time showed that the number of F. tularensis per amoeba increased over time. Accordingly, the viable counts of F. tularensis released from A. castellanii by deoxycholate treatment also increased over time.
In this study the attenuated vaccine strain F. tularensis LVS was used. Compared to virulent strains of F. tularensis, this strain obviously is not highly virulent for humans. However, it is still highly virulent for mice and guinea pigs (34). The genetic change(s) that results in attenuation is unknown. It is possible that the LVS strain could have a toxic effect on the protozoan host that is different from that of fully virulent F. tularensis strains.
Many types of bacteria have been found in free-living amoebae, including Legionella spp., Burkholderia pickettii, Vibrio cholerae, Mycobacterium avium, and Listeria monocytogenes (17, 39). These bacteria are able to survive inside the protozoa as endosymbionts and to take advantage of the amoebae as vectors for their dissemination. However, Francisella shows no close relationship to these genera, being most closely related to arthropod parasites and symbionts, including Wolbachia persica, the Dermatocor andersoni symbiont, and Ornithodorous moubata symbiont B (10, 27, 28). Other related strains, outside the Francisellaceae, include members of the Pisciricketsiaceae, in particular the intracellular bacterium Piscirickettsia salmonis, which is a fish pathogen (37).
Francisella bacteria are commonly transmitted to vertebrates via bites by ticks or mosquitoes (18, 19). However, ticks may not comprise a natural reservoir for Francisella, since infected ticks show a high mortality rate and transovarial transmission remains dubious (12, 19, 20). Moreover, the bacterium has been isolated from about 250 wildlife species (18, 37), clearly demonstrating that F. tularensis should be considered a highly successful intracellular parasite with a very broad host range and ability to survive and spread in widely differing natural environments.
The ability of F. tularensis to survive in trophozoites of A. castellanii and cysts, as demonstrated in this study, may have implications for the mode of transmission of the microorganism. However, although we have shown preliminary evidence for the survival of F. tularensis in amoebal cysts, the potential for its survival under various types of adverse conditions in these cysts still needs to be systematically examined. The close connection of tularemia with water (30) and the isolation of the bacterium from water samples used for domestic purposes, as well as from natural water systems, as the causal agent of outbreaks of the disease (14, 20, 21, 32) support the hypothesis that amoebae may have a role in the natural transmission of F. tularensis.
Acknowledgments
This work has been supported through Swedish Defense Agency project number A4854.
The opinions expressed in this paper are those of the authors and do not reflect any official policy.
A. Sjöstedt is acknowledged for critical reading of the manuscript. Electron micrographs were skillfully prepared by V. Baranov, University of Umeå, and monoclonal antibody specific for F. tularensis was kindly provided by R. Grunow, German Armed Forces Medical Academy, Munich.
REFERENCES
- 1.Abu Kwaik, Y., L. Y. Gao, B. J. Stone, C. Venkataraman, and O. S. Harb. 1998. Invasion of protozoa by Legionella pneumophila and its role in bacterial ecology and pathogenesis. Appl. Environ. Microbiol. 64:3127-3133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Amann, R., N. Springer, W. Schonhuber, W. Ludwig, E. N. Schmid, K. D. Muller, and R. Michel. 1997. Obligate intracellular bacterial parasites of Acanthamoeba related to Chlamydia spp. Appl. Environ. Microbiol. 63:115-121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Anthony, L. S. D., R. D. Burke, and F. E. Nano. 1991. Growth of Francisella spp. in rodent macrophages. Infect. Immun. 59:3291-3296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3a.Anthony, L. S. D., and P. A. L. Kongshavn. 1985. Host resistance to experimental murine tularemia. Fed. Proc. 44:528. [DOI] [PMC free article] [PubMed]
- 4.Berdal, B. P., R. Mehl, N. K. Meidell, A. Lorentzen-Styr, and O. Scheel. 1996. Field investigations of tularaemia in Norway. FEMS Immunol. Med. Microbiol. 13:191-195. [DOI] [PubMed] [Google Scholar]
- 5.Bhatnagar, N., E. Getachew, S. Straley, J. Williams, M. Meltzer, and A. Fortier. 1994. Reduced virulence of rifampicin-resistant mutants of Francisella tularensis. J. Infect. Dis. 170:841-847. [DOI] [PubMed] [Google Scholar]
- 6.Cormack, B. P., R. H. Valdivia, and S. Falkow. 1996. FACS-optimized mutants of the green fluorescent protein (GFP). Gene 173:333-338. [DOI] [PubMed] [Google Scholar]
- 7.Dennis, D. T., T. V. Inglesby, and D. A. Henderson. 2001. Tularemia as a biological weapon: medical and public health management. JAMA 285:2763-2773. [DOI] [PubMed] [Google Scholar]
- 8.Eigelsbach, H. T., and C. M. Down. 1961. Prophylactic effectiveness of live and killed tularemia vaccines. I. Production of vaccine and evaluation in the white mouse and guinea pig. J. Immunol. 87:415-425. [PubMed] [Google Scholar]
- 9.Ericsson, M., I. Golovliov, G. Sandstrom, A. Tarnvik, and A. Sjostedt. 1997. Characterization of the nucleotide sequence of the groE operon encoding heat shock proteins chaperone-60 and -10 of Francisella tularensis and determination of the T-cell response to the proteins in individuals vaccinated with F. tularensis. Infect. Immun. 65:1824-1829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Forsman, M., G. Sandstrom, and A. Sjostedt. 1994. Analysis of 16S ribosomal DNA sequences of Francisella strains and utilization for determination of the phylogeny of the genus and for identification of strains by PCR. Int. J. Syst. Bacteriol. 44:38-46. [DOI] [PubMed] [Google Scholar]
- 11.Fortier, A. H., D. A. Leiby, R. B. Narayanan, E. Asafoadjei, R. M. Crawford, C. A. Nancy, and M. S. Meltzer. 1995. Growth of Francisella tularensis LVS in macrophages: the acidic intracellular compartment provides essential iron required for growth. Infect. Immun. 63:1478-1483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Francis, E. 1937. Sources of infection and seasonal incidence of tularemia in man. Public Health Rep. 52:103-113. [Google Scholar]
- 13.Golovliov, I., M. Ericsson, G. Sandstrom, A. Tarnvik, and A. Sjostedt. 1997. Identification of proteins of Francisella tularensis induced during growth in macrophages and cloning of the gene encoding a prominently induced 23-kilodalton protein. Infect. Immun. 65:2183-2189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Greco, D., G. Allegrini, T. Tizzi, E. Ninu, A. Lamanna, and S. Luzi. 1987. A waterborne tularaemia outbreak. Eur. J. Epidemiol. 3:35-38. [DOI] [PubMed] [Google Scholar]
- 15.Gustafson, K. 1989. Growth and survival of four strains of Francisella tularensis in a rich medium preconditioned with Acanthamoeba palestinensis. Can. J. Microbiol. 35:1100-1104. [DOI] [PubMed] [Google Scholar]
- 16.Harb, O. S., and Y. Abu Kwaik. 2000. Interaction of Legionella pneumophila with protozoa provides lessons. ASM News 66:609-616. [Google Scholar]
- 17.Harb, O. S., L. Y. Gao, and Y. Abu Kwaik. 2000. From protozoa to mammalian cells: a new paradigm in the life cycle of intracellular bacteria. Environ. Microbiol. 2:251-265. [DOI] [PubMed] [Google Scholar]
- 18.Hopla, C. E. 1974. The ecology of tularemia. Adv. Vet. Sci. Comp. Med. 18:25-53. [PubMed] [Google Scholar]
- 19.Hubalek, Z., F. Treml, J. Halouzka, Z. Juricova, M. Hunady, and V. Janik. 1996. Frequent isolation of Francisella tularensis from Dermacentor reticulatus ticks in an enzootic focus of tularaemia. Med. Vet. Entomol. 10:241-246. [DOI] [PubMed] [Google Scholar]
- 20.Jellison, W. L. 1974. Tularaemia in North America 1930-1974. University of Montana, Missoula.
- 21.Jellison, W. L., D. C. Epler, E. Kuhns, and G. M. Kohls. 1950. Tularaemia in man from a domestic rural water supply. Public Health Rep. 65:1219-1226. [PubMed] [Google Scholar]
- 22.Kahane, S., B. Dvoskin, M. Mathias, and M. G. Friedman. 2001. Infection of Acanthamoeba polyphaga with Simkania negevensis and S. negevensis survival within amoebal cysts. Appl. Environ. Microbiol. 67:4789-4795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kuoppa, K., A. Forsberg, and A. Norqvist. 2001. Construction of a reporter plasmid for screening in vivo promoter activity in Francisella tularensis. FEMS Microbiol. Lett. 205:77-81. [DOI] [PubMed] [Google Scholar]
- 24.Lai, X. H., I. Golovliov, and A. Sjostedt. 2001. Francisella tularensis induces cytopathogenicity and apoptosis in murine macrophages via a mechanism that requires intracellular bacterial multiplication. Infect. Immun. 69:4691-4694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Martinez, A. J., and G. S. Visvesvara. 1997. Free-living amphizoic and opportunistic amoebae. Brain Pathol. 7:583-598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Neumeister, B., S. Schoniger, M. Faigle, and K. Dietz. 1997. Multiplication of different Legionella species in Mono Mac 6 cells and in Acanthamoeba castellanii. Appl. Environ. Microbiol. 63:1219-1224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Niebylski, M. L., M. G. Peacock, E. R. Fischer, S. F. Porcella, and T. G. Schwan. 1997. Characterization of an endosymbiont infecting wood ticks, Dermacentor andersoni, as a member of the genus Francisella. Appl. Environ. Microbiol. 63:3933-3940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Noda, H., U. G. Munderloh, and T. J. Kurtti. 1997. Endosymbionts of ticks and their relationship to Wolbachia spp. and tick-borne pathogens of humans and animals. Appl Environ Microbiol. 63:3926-3932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Norqvist, A., K. Kuoppa, and G. Sandstrom. 1996. Construction of a shuttle vector for use in Francisella tularensis. FEMS Immunol. Med. Microbiol. 13:257-260. [DOI] [PubMed] [Google Scholar]
- 30.Parker, R. R., E. A. Steinhaus, G. M. Kohls, and W. L. Jellison. 1951. Contamination of natural waters and mud with Pasteurella tularensis and tularemia in beavers and muskrats in the north western United States. Natl. Inst. Health Bull. 193:1-61. [PubMed] [Google Scholar]
- 31.Pavlov, V. M., A. N. Mokrievich, and K. Volkovoy. 1996. Cryptic plasmid pFNL10 from Francisella novicida-like F6168: the base of plasmid vectors for Francisella tularensis. FEMS Immunol. Med. Microbiol. 13:253-256. [DOI] [PubMed] [Google Scholar]
- 32.Quan, S. F., A. G McManus, and H. von Fintel. 1956. Infectivity of tularemia applied to intact skin and ingested in drinking water. Science 123:942. [DOI] [PubMed] [Google Scholar]
- 33.Reilly, T. J., G. S. Baron, F. E. Nano, and M. S. Kuhlenschmidt. 1996. Characterization and sequencing of a respiratory burst-inhibiting acid phosphatase from Francisella tularensis. J. Biol. Chem. 271:10973-10983. [DOI] [PubMed] [Google Scholar]
- 34.Sandstrom, G. 1994. The tularaemia vaccine. J. Chem. Technol. Biotechnol. 59:315-320. [DOI] [PubMed] [Google Scholar]
- 35.Saslaw, S., H. T. Eigelsbach, H. E. Wilson, J. A. Prior, and S. Carhart. 1961. Tularaemia vaccine study. I. Intracutaneous challenge. Arch. Intern. Med. 107:689-701. [DOI] [PubMed] [Google Scholar]
- 36.Saslaw, S., H. T. Eigelsbach, J. A. Prior, H. E. Wilson, and S. Carhart. 1961. Tularaemia vaccine study. II. Respiratory challenge. Arch. Intern. Med. 107:702-714. [DOI] [PubMed] [Google Scholar]
- 37.Sjostedt, A. Family XVII. Francisellaceae, genus I. Francisella. In D. J. Brenner (ed.), Bergey's manual of systematic bacteriology, in press. Springer-Verlag, New York, N.Y.
- 38.Steinert, M., K. Birkness, E. White, B. Fields, and F. Quinn. 1998. Mycobacterium avium bacilli grow saprozoically in coculture with Acanthamoeba polyphaga and survive within cyst walls. Appl. Environ. Microbiol. 64:2256-2261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Winiecka-Krusnell, J., and E. Linder. 2001. Bacterial infections of free-living amoebae. Res. Microbiol. 152:613-619. [DOI] [PubMed] [Google Scholar]