Abstract
Mexican Americans are the largest subgroup of Hispanics, the largest minority population in the United States. Stroke is the leading cause of disability and third leading cause of death. The authors compared stroke incidence among Mexican Americans and non-Hispanic Whites in a population-based study. Stroke cases were ascertained in Nueces County, Texas, utilizing concomitant active and passive surveillance. Cases were validated on the basis of source documentation by board-certified neurologists masked to subjects’ ethnicity. From January 2000 to December 2002, 2,350 cerebrovascular events occurred. Of the completed strokes, 53% were in Mexican Americans. The crude cumulative incidence was 168/10,000 in Mexican Americans and 136/ 10,000 in non-Hispanic Whites. Mexican Americans had a higher cumulative incidence for ischemic stroke (ages 45–59 years: risk ratio = 2.04, 95% confidence interval: 1.55, 2.69; ages 60–74 years: risk ratio = 1.58, 95% confidence interval: 1.31, 1.91; ages ≥75 years: risk ratio = 1.12, 95% confidence interval: 0.94, 1.32). Intracerebral hemorrhage was more common in Mexican Americans (age-adjusted risk ratio = 1.63, 95% confidence interval: 1.24, 2.16). The subarachnoid hemorrhage age-adjusted risk ratio was 1.57 (95% confidence interval: 0.86, 2.89). Mexican Americans experience a substantially greater ischemic stroke and intracerebral hemorrhage incidence compared with non-Hispanic Whites. As the Mexican-American population grows and ages, measures to target this population for stroke prevention are critical.
Keywords: cerebral hemorrhage, cerebrovascular accident, ethnic groups, Hispanic Americans, ischemic attack, transient, Mexican Americans, population surveillance, subarachnoid hemorrhage
Abbreviation: BASIC, Brain Attack Surveillance in Corpus Christi
Hispanic Americans are now the largest minority population in the United States (1). Mexican Americans are by far the largest subgroup of Hispanic Americans. There are no existing data regarding the cerebrovascular disease burden faced by Mexican Americans, and estimates regarding the impact of stroke on the nation are therefore limited. Cerebrovascular disease is the leading cause of adult disability and third leading cause of death in the United States (2). Direct and indirect expenditures approach 50 billion dollars annually (3). The Mexican-American population is among the country’s fastest growing groups (1). As this currently youthful population ages, stroke will become even more important. Efforts to target populations for health care interventions must begin with accurate estimates of disease occurrence.
Social and biologic risk factors are associated with stroke to a similar extent in Mexican Americans and non-Hispanic Whites (4). The higher prevalence of diabetes mellitus (5), lower socioecononmic status (6), and limited access to quality health care (7) found in Mexican Americans would predict more stroke in Mexican Americans relative to non-Hispanic Whites. However, vital statistics suggest that non-Hispanic Whites actually experience more stroke mortality, particularly at older ages when stroke is most common (8). Vital statistics data may greatly underestimate ethnic-specific stroke mortality as a result of improper coding of ethnicity on the death certificate (9). The most accurate estimates of disease burden are made through population-based ascertainment of stroke cases with reliable definitions of ethnicity and case status.
The Brain Attack Surveillance in Corpus Christi (BASIC) Project is a population-based stroke surveillance effort in a nonimmigrant biethnic community in southeast Texas. We present here cumulative stroke incidence among Mexican Americans and non-Hispanic Whites in this representative US community.
MATERIALS AND METHODS
The methodology of the BASIC Project was previously reported (10, 11). Briefly, a combination of active and passive surveillance was used to ensure complete case capture of all cerebrovascular cases in residents of Nueces County, Texas, who were more than 44 years of age. The project took place between January 2000 and December 2002. Nueces County has a population of 313,645 with 56 percent Mexican American and 38 percent non-Hispanic White (1). Over 95 percent of the county’s population resides within the city of Corpus Christi. Nueces County is over 150 miles from San Antonio and Houston, and it serves as the regional referral area for the sparsely populated surrounding counties. This affords complete case capture for initial contact of acute medical conditions including stroke. Nueces County is not an immigrant community. The majority of Mexican Americans there are second- and third-generation US citizens.
Abstractors underwent a rigorous training and certification process, and several quality assurance mechanisms were imposed. Cases were screened from emergency department and inpatient sources by manually searching visit and admission logs for a set of previously validated screening diagnostic codes (12). The abstractors routinely canvassed intensive care units and hospital floors searching for in-house strokes or those not ascertained through the screening logs. This hot pursuit was supplemented by review of hospital passive listings of International Classification of Diseases, Ninth Revision, discharge codes for stroke (codes 430–438, excluding codes 433.x0 and 434.x0 (x = 1–9), 437.0, 437.2, 437.3, 437.4, 437.5, 437.7, 437.8, and 438).
Cases that screened positive for potential stroke diagnostic codes were reviewed for eligibility criteria (aged ≥45 years, Nueces County residence). All eligible cases were fully abstracted and source documentation was copied. Study neurologists validated cases using source documentation, blinded to ethnicity, on the basis of previously published international criteria (13, 14). Mexican-American and non-Hispanic White subjects considered for validation were equally likely to have received head computed tomography or magnetic resonance imaging (Mexican Americans: 94.8 percent; non-Hispanic Whites: 93.7 percent; p = 0.22) (15). Stroke was defined as the acute onset (from minutes to hours) of a focal neurologic deficit specifically attributable to a cerebrovascular distribution that persists for greater than 24 hours (except in cases of sudden death or if the development of symptoms is interrupted by a surgical or interventional procedure) and not attributable to another disease process (seizure, brain tumor, hypoglycemia, metabolic encephalopathy, or hysteria). A diagnosis of transient ischemic attack was the same except that symptoms abated within 24 hours. The diagnosis of intracerebral hemorrhage or subarachnoid hemorhage required the clinical symptoms mentioned above and neuroimaging that demonstrated a spontaneous focal collection of blood in either the parenchyma/ventricle (intracerebral hemorrhage) or subarachnoid space (subarachnoid hemorrhage). A spinal fluid definition of subarachnoid hemorrhage, including xanthochromia and/ or greater than 1,000 red blood cells per cubic millimeter without a decrement from first to last tubes of greater than 25 percent (16), was accepted. To determine initial stroke severity, we retrospectively abstracted the National Institutes of Health Stroke Scale from the chart in accordance with the validated method of Willams et al. (17).
Two thirds of the validated cases were randomly selected to participate in a structured patient interview. The interview contained questions regarding risk factors, medications that patients were taking prior to their stroke, access to care, and race/ethnicity. The BASIC Project interview identifies race and ethnicity in a manner similar to that of the 2000 US Census with a question about race and then a separate question about ethnicity. Patients recording their ethnicity “of Hispanic origin” were also asked the country of origin of their parents and their grandparents. Since race/ethnicity data obtained from the interview were available for only a random sample of subjects, race/ethnicity was also obtained from the medical record for all patients. The use of medical record race/ethnicity for this study was validated by the subject’s interview data by comparing self-reported and medical record-abstracted race/ethnicity. From a total of 1,194 interviews of 580 Mexican Americans, 546 non-Hispanic Whites, and 68 Blacks, we observed 97 percent agreement (kappa = 0.94) between self-report and medical record for race/ethnicity classification.
An out-of-hospital sampling frame was used to estimate nonhospitalized stroke and transient ischemic attack cases. A random sample from primary care physicians, nursing homes, and neurologists in Nueces County was obtained, with neurologists being oversampled. The following available population of primary care physicians (n = 167), nursing homes (n = 12), and neurologists (n = 11) yielded a sample of 47 primary care physicians, four nursing homes, and 11 neurologists.
This project was approved by the institutional review boards of the University of Michigan and the University of Texas at Houston, the Corpus Christi/Nueces County Health District, and all hospitals.
Regarding statistical analysis, age-specific 36-month cumulative incidence was calculated by ethnicity and stroke type (ischemic stroke, intracerebral hemorrhage, subarachnoid hemorrhage, and transient ischemic attack). Ethnic classification of Mexican American or non-Hispanic White was determined from the medical record for the numerators for the incidence calculations. From the interview data regarding family ancestry, it was determined that only 1 percent of subjects reported ancestry other than Mexican. From this information, we determined that it would be appropriate to classify our Hispanic stroke cases as Mexican American.
The denominators for the incidence calculations were the 2000 US Census estimates using 5- and 15-year age categories (1). The denominators for non-Hispanic Whites were derived from individuals reporting the single race group White and an ethnicity of non-Hispanic origin. This method may have led to an underestimation of the non-Hispanic White population, as individuals who reported two- or three-race combinations were not included; however, these categories represent only 3.7 percent of Texas residents. The denominators for Mexican Americans were derived from individuals who reported an ethnicity of Hispanic origin regardless of race. Less than 1 percent of subjects residing in Nueces County who identified their ethnicity as Hispanic on the 2000 US Census identified their race as other than White. Further, among the Hispanics in Nueces County included in the 2000 US Census, only 1.2 percent identified an ancestral origin from a country other than Mexico (1 percent identified Spain and 0.2 percent identified Central or South America). These data support our designation of the census population data into non-Hispanic White and Mexican American for the population of Nueces County, Texas, and they demonstrate that definitions in the numerators correspond to definitions in the denominators for the incidence calculations.
The numerators were calculated by identifying an individual’s first event captured by the BASIC Project. Events were then summed by ethnicity and age categories for each stroke type. The age-specific, 36-month cumulative incidence for first-ever ischemic stroke only was also calculated by ethnicity. Cumulative incidence was first calculated using data from inpatient sources only. Data collected from the out-of-hospital sample during the last 24 months of the 36-month surveillance were then used to estimate the total number of strokes that occurred out of hospital and were used to adjust the number of ischemic strokes and transient ischemic attacks identified by the BASIC Project during 36 months of surveillance.
Risk ratios and 95 percent confidence intervals comparing Mexican Americans and non-Hispanic Whites were calculated to examine ethnic differences in cumulative incidence. To test for interactions between ethnicity and age on risk of stroke, we performed Breslow-Day tests of homogeneity. When there was no significant age-ethnicity interaction, age-adjusted risk ratios and 95 percent confidence intervals comparing Mexican Americans and non-Hispanic Whites were calculated using the Mantel-Haenszel method. The BASIC Project was designed to detect a minimum incidence risk ratio of 1.20 for overall stroke attack rates comparing Mexican Americans and non-Hispanic Whites, assuming 80 percent power and a 0.05 level of significance based on a two-sided hypothesis. The study was also sufficiently powered to study ethnic differences in ischemic stroke incidence. Age categories were prespecified before the study started as 45–59, 60–74, and 75 or more years.
In a secondary analysis, we compared the proportion of Mexican-American and non-Hispanic White ischemic stroke patients who were taking medication for known personal stroke risk factors. Z tests for binomial proportions were used to test for significant differences between ethnicities. SAS version 8.02 software (SAS Institute, Inc., Cary, North Carolina) was used for analyses.
RESULTS
Abstractors screened a total of 14,212 cases. Of these cases, 2,955 met the criteria and were referred to the neurologist for validation. There were a total of 2,550 validated cases of cerebrovascular disease during the study time period. Of these, 162 cases were excluded since they were not Mexican American or non-Hispanic White. Twenty-four cases with unknown stroke type were excluded, leaving 2,364 eligible cases. Of these 2,364 cases, an additional 14 out-of-hospital cases were excluded because they were submitted by physicians not sampled as part of the BASIC Project, leaving 2,350 cases for analysis. When an individual had more than one event captured by the BASIC Project, all events that occurred after the first one were excluded (n = 256), leaving 2,094 independent cases (i.e., one case per unique individual) eligible for the final analysis. Of these 2,094 independent cases, 69 were ascertained from the out-of-hospital sample, and 2,025 were ascertained from the inhospital sources.
Table 1 presents the age- and race/ethnic-specific cumulative incidence for completed cerebrovascular events (first-ever and recurrent completed ischemic stroke + intracerebral hemorrhage + subarachnoid hemorrhage). Of the completed cerebrovascular events, 53 percent occurred in Mexican Americans. The risk increased with advancing age and was higher in Mexican Americans compared with non-Hispanic Whites at each age group, although not statistically different for the group aged 75 or more years. There was a significant age-ethnicity interaction for total completed cerebrovascular events. The median National Institutes of Health Stroke Scale for completed cerebrovascular events did not differ by ethnicity (non-Hispanic White: 4 (interquartile range: 2–9) and Mexican American: 4 (interquartile range: 2–8)).
TABLE 1.
Age- and ethnic-specific cumulative incidence of total completed cerebrovascular events (first-ever and recurrent ischemic stroke, intracerebral hemorrhage, subarachnoid hemorrhage), Nueces County, Texas, January 2000–December 2002
| Total first-ever and recurrent ischemic stroke, intracerebral hemorrhage, and subarachnoid hemorrhage* |
||||||||
|---|---|---|---|---|---|---|---|---|
| Age (years) | Mexican-American cases | Mexican-American denominator | Cumulative incidence/ 10,000 | Non-Hispanic White cases | Non-Hispanic White denominator | Cumulative incidence/ 10,000 | Mexican-American/non-Hispanic White risk ratio | 95% confidence interval |
| 45–59 | 201 | 26,462 | 76 | 91 | 25,127 | 36 | 2.10 | 1.64, 2.69 |
| 60–74 | 298 | 13,331 | 224 | 216 | 15,411 | 140 | 1.59 | 1.34, 1.90 |
| ≥75 | 268 | 5,727 | 468 | 366 | 8,969 | 408 | 1.15 | 0.98, 1.34 |
| >45 | 767 | 45,520 | 168 | 673 | 49,507 | 136 | 1.24 | 1.12, 1.37 |
Breslow-Day test for homogeneity across age strata: p < 0.001.
Although from a statistical standpoint independence of events is important (data presented in table 1), from a public health resource utilization perspective, it is also useful to investigate all completed cerebrovascular events (first-ever and recurrent completed ischemic stroke + intracerebral hemorrhage + subarachnoid hemorrhage) in the study population. When all events were considered, including multiple events per individual (n = 1,616), the cumulative incidence for completed cerebrovascular events is 193/10,000 in Mexican Americans and 149/10,000 in non-Hispanic Whites. In comparison with the data shown in table 1, these data suggest that several individuals experienced multiple events during the study time period. In this study population, 1,373 individuals (92 percent) experienced one completed cerebrovascular event, 95 (6 percent) experienced two events, 15 (1 percent) experienced three events, and two (0.1 percent) experienced four events during the study time period.
Table 2 shows the cumulative incidence for first-ever and recurrent ischemic stroke. Sixty-eight percent were first-ever ischemic stroke and 32 percent were recurrent ischemic stroke. Mexican Americans had a higher incidence at younger ages, but the risk converges with advancing age. There was a significant age-ethnicity interaction. The age-ethnicity interaction precluded age adjustment. Table 2 also demonstrates cumulative incidence for first-ever ischemic stroke. Mexican Americans between 45 and 59 years of age had almost double the risk of first stroke compared with non-Hispanic Whites. This difference approached zero when ethnic comparisons were made in those aged 75 or more years. This significant age-ethnicity interaction again precluded age adjustment.
TABLE 2.
Age- and ethnic-specific cumulative incidence for first-ever and recurrent stroke and transient ischemic attack, Nueces County, Texas, January 2000–December 2002
| Age (years) | Mexican-American cases | Mexican-American denominator | Cumulative incidence/ 10,000 | Non-Hispanic White cases | Non-Hispanic White denominator | Cumulative incidence/10,000 | Mexican-American/non-Hispanic White risk ratio | 95% confidence Interval | |
|---|---|---|---|---|---|---|---|---|---|
| Total first-ever and recurrent ischemic stroke* | |||||||||
| 45–59 | 157 | 26,462 | 59 | 73 | 25,127 | 29 | 2.04 | 1.55, 2.69 | |
| 60–74 | 250 | 13,331 | 188 | 183 | 15,411 | 119 | 1.58 | 1.31, 1.91 | |
| ≥75 | 219 | 5,727 | 382 | 307 | 8,969 | 342 | 1.12 | 0.94, 1.32 | |
| >45 | 626 | 45,520 | 138 | 563 | 49,507 | 114 | 1.21 | 1.08, 1.35 | |
| Total first-ever ischemic stroke* | |||||||||
| 45–59 | 116 | 26,462 | 44 | 58 | 25,127 | 23 | 1.90 | 1.39, 2.60 | |
| 60–74 | 171 | 13,331 | 128 | 122 | 15,411 | 79 | 1.62 | 1.29, 2.04 | |
| ≥75 | 137 | 5,727 | 239 | 210 | 8,969 | 234 | 1.02 | 0.83, 1.26 | |
| >45 | 424 | 45,520 | 93 | 390 | 49,507 | 79 | 1.18 | 1.03, 1.36 | |
| Total first-ever and recurrent intracerebral hemorrhage | |||||||||
| 45–59 | 31 | 26,462 | 12 | 10 | 25,127 | 4 | 2.94 | 1.44, 6.00 | |
| 60–74 | 40 | 13,331 | 30 | 29 | 15,411 | 19 | 1.59 | 0.99, 2.57 | |
| ≥75 | 45 | 5,727 | 79 | 53 | 8,969 | 59 | 1.33 | 0.89, 1.98 | |
| >45 | 116 | 45,520 | 25 | 92 | 49,507 | 19 | 1.37 | 1.04, 1.80 | |
| Age-adjusted risk ratio | 1.63 | 1.24, 2.16 | |||||||
| Total first-ever and recurrent subarachnoid hemorrhage | |||||||||
| 45–59 | 13 | 26,462 | 5 | 8 | 25,127 | 3 | 1.54 | 0.64, 3.72 | |
| 60–74 | 8 | 13,331 | 6 | 4 | 15,411 | 3 | 2.31 | 0.70, 7.68 | |
| ≥75 | 4 | 5,727 | 7 | 6 | 8,969 | 7 | 1.04 | 0.29, 3.70 | |
| >45 | 25 | 45,520 | 5 | 18 | 49,507 | 4 | 1.51 | 0.82, 2.77 | |
| Age-adjusted risk ratio | 1.57 | 0.86, 2.89 | |||||||
| Total first-ever and recurrent transient ischemic attack* | |||||||||
| 45–59 | 72 | 26,462 | 27 | 35 | 25,127 | 14 | 1.95 | 1.30, 2.92 | |
| 60–74 | 106 | 13,331 | 80 | 105 | 15,411 | 68 | 1.17 | 0.89, 1.53 | |
| ≥75 | 103 | 5,727 | 180 | 164 | 8,969 | 183 | 0.98 | 0.77, 1.26 | |
| >45 | 281 | 45,520 | 62 | 304 | 49,507 | 61 | 1.01 | 0.86, 1.18 | |
Breslow-Day test for homogeneity across age strata: p < 0.001.
Table 2 presents comparative data for intracerebral hemorrhage as well. Young Mexican Americans aged 45–59 years had a threefold increased risk of intracerebral hemorrhage compared with non-Hispanic Whites. The age-adjusted risk ratio was 1.63 (95 percent confidence interval: 1.24, 2.16). Table 2 further presents the data for subarachnoid hemorrhage. While the risk ratios were similar to those found for ischemic stroke and intracerebral hemorrhage, the events were few and the confidence intervals overlapped unity. The age-adjusted risk ratio was 1.57 (95 percent confidence interval: 0.86, 2.89). Transient ischemic attack was experienced by 585 subjects in the hospital setting (table 2). Mexican Americans aged 45–59 years were almost twice as likely to experience a transient ischemic attack as were non-Hispanic Whites. However, at older ages there were no significant differences. A significant age-ethnicity interaction was also found for risk of transient ischemic attack.
To further evaluate if the lower risk ratios seen in the older age groups were due to the more youthful age distribution of Mexican Americans compared with non-Hispanic Whites, we reanalyzed table 2 (first-ever and recurrent ischemic stroke) by 5-year age groups. This is shown graphically in figure 1. Indeed, the group aged 80–84 years still showed an elevated risk for Mexican Americans. The group aged 85 or more years was not reported because of the different age distributions of the two ethnicities after the age of 85 years.
FIGURE 1.
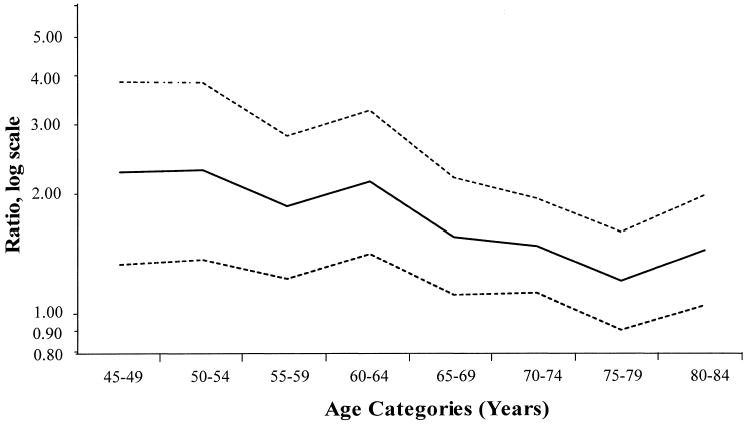
Natural log of first-ever and recurrent ischemic stroke cumulative incidence risk ratios with 95% confidence intervals by 5-year age categories (Mexican Americans/non-Hispanic Whites), Nueces County, Texas, January 2000–December 2002.
Table 3 shows the in-hospital cases plus the out-of-hospital cases. The out-of-hospital sample included 69 cases, of which 27 were ischemic strokes and 42 were transient ischemic attacks. These were inflated in table 3 on the basis of the sampling scheme to 168 cases (71 ischemic stroke and 97 transient ischemic attack) to reflect the numbers for the total population. Out-of-hospital strokes accounted for 5.6 percent of all first-ever and recurrent ischemic strokes (5.3 percent in Mexican Americans and 6.0 percent in non-Hispanic Whites) and 14.2 percent of transient ischemic attacks (14.1 percent in Mexican Americans and 14.4 percent in non-Hispanic Whites).
TABLE 3.
Age- and ethnic-specific cumulative incidence adjusted to add the out-of-hospital cases to the in-hospital cases of ischemic stroke and transient ischemic attack, Nueces County, Texas, January 2000–December 2002
| Age (years) | Mexican-American cases* | Mexican-American denominator | Cumulative incidence/10,000 | Non-Hispanic White cases* | Non-Hispanic White denominator | Cumulative incidence/10,000 | Mexican-American/non-Hispanic White risk ratio | 95% confidence interval |
|---|---|---|---|---|---|---|---|---|
| Ischemic stroke | ||||||||
| 45–59 | 159 | 26,462 | 60 | 73 | 25,127 | 29 | 2.07 | 1.57, 2.73 |
| 60–74 | 269 | 13,331 | 202 | 207 | 15,411 | 134 | 1.50 | 1.26, 1.80 |
| ≥75 | 233 | 5,727 | 407 | 319 | 8,969 | 356 | 1.14 | 0.97, 1.35 |
| >45 | 661 | 45,520 | 145 | 599 | 49,507 | 121 | 1.20 | 1.08, 1.34 |
| Transient ischemic attack | ||||||||
| 45–59 | 86 | 26,462 | 32 | 47 | 25,127 | 19 | 1.74 | 1.22, 2.48 |
| 60–74 | 128 | 13,331 | 96 | 127 | 15,411 | 82 | 1.17 | 0.91, 1.49 |
| ≥75 | 113 | 5,727 | 197 | 181 | 8,969 | 202 | 0.98 | 0.77, 1.23 |
| >45 | 327 | 45,520 | 72 | 355 | 49,507 | 72 | 1.00 | 0.86, 1.16 |
Number of cases reflects 69 out-of-hospital cases (27 ischemic stroke and 42 transient ischemic attack) inflated based on the sampling scheme to 168 cases (71 ischemic stroke and 97 transient ischemic attack) to reflect numbers for the total population.
Table 4 shows the results of the secondary analysis examining consumption of medication for individuals’ personal stroke risk factors. Stroke patients were asked to report consumption of medications before the index stroke event. Of the subjects with a prior history of stroke who were known to have diabetes, 85–89 percent were taking medications to treat that condition, but only 67–75 percent were taking antiplatelet or antithrombotic medication at the time their stroke event was captured by the BASIC Project. There were no ethnic differences, but the numbers were small. Of those with no prior history of stroke, only about one third were taking antiplatelet or antithrombotic medication at the time their stroke event was captured by the BASIC Project. This is to be expected, since these medications have only been established as secondary stroke prevention drugs.
TABLE 4.
Proportion of patients taking stroke prevention medication before their index stroke event of those reporting a personal stroke risk factor, among a random sample of interviewed Mexican-American and non-Hispanic White ischemic stroke cases, Brain Attack Surveillance in Corpus Christi Project, January 2000–December 2002
| Mexican American
|
Non-Hispanic White
|
||||
|---|---|---|---|---|---|
| Risk factor | No. | % | No. | % | p value |
| Recurrent ischemic stroke cases (n = 181) | |||||
| Hypertension | 78 | 83 | 67 | 88 | 0.39 |
| Diabetes | 53 | 85 | 29 | 89 | 0.60 |
| Atrial fibrillation | 13 | 69 | 25 | 64 | 0.75 |
| High cholesterol | 45 | 60 | 43 | 58 | 0.85 |
| Heart disease | 43 | 72 | 41 | 80 | 0.39 |
| Stroke prevention* | 94 | 67 | 87 | 75 | 0.23 |
| First-ever ischemic stroke cases (n = 384) | |||||
| Hypertension | 137 | 88 | 123 | 83 | 0.25 |
| Diabetes | 93 | 92 | 53 | 91 | 0.84 |
| Atrial fibrillation | 21 | 67 | 27 | 78 | 0.40 |
| High cholesterol | 72 | 63 | 74 | 51 | 0.14 |
| Heart disease | 61 | 79 | 53 | 72 | 0.39 |
| Stroke prevention | 197 | 31 | 187 | 39 | 0.10 |
Warfarin, aspirin, ticlopidine, clopidogrel, or extended-release dipyridamole/aspirin.
DISCUSSION
The results of the BASIC Project clearly demonstrate an increased stroke incidence among Mexican Americans compared with non-Hispanic Whites in this representative southeast Texas community. Specifically, Mexican Americans have an increased incidence of intracerebral hemorrhage and subarachnoid hemorrhage compared with non-Hispanic Whites adjusted for age, as well as an increased incidence of ischemic stroke and transient ischemic attack at younger ages compared with non-Hispanic Whites. This is the first report to quantify the relative differences in stroke between these two important components of the US population. Efforts to reduce the stroke burden in Mexican Americans may target both conventional and nonconventional stroke risk factors (4). Mexican Americans have a high prevalence of diabetes mellitus, but the prevalences of hypertension and hyperlipidemia are comparable with those in non-Hispanic Whites (5, 16). Since it was previously shown that the prevalence of diabetes mellitus differs by just 6 percent in this community, it is likely that this explains only a small part of the stroke-related health disparity (18).
Access to care and acculturation are important nonconventional stroke risk factors in Mexican Americans. A recent study found that Hispanics were 12.7 percent less likely to receive the appropriate secondary stroke prevention drug compared with non-Hispanic Whites (19). We did not find similar results in the current study. However, a study in Nueces County found that the general population of Mexican Americans was less knowledgeable about stroke risk factors and felt less empowered to prevent stroke compared with the general population of non-Hispanic Whites (18). Mexican Americans were also less likely to say that they would call 9-1-1 when experiencing an acute stroke, thus limiting access for acute stroke therapy. However, in a case-control study comparing stroke patients with population-based controls, access-to-care variables were equally predictive of stroke in both Mexican Americans and non-Hispanic Whites (4). Although limitations in access to care may be associated with similar risk of stroke for individuals of both ethnic groups, it is possible that stroke-related health disparities are partially explained by the greater relative prevalence of limitations in access to quality health care in Mexican Americans compared with non-Hispanic Whites (7).
The role of genetics as an explanation for the ischemic stroke disparity between Mexican Americans and non-Hispanic Whites has not been addressed. Cavernous malformations, an important cause of intracerebral hemorrhage, were found to have an underlying genetic association with a mutation that clusters in Mexican-American families (20). Ischemic stroke is more likely polygenic and complex, but clues from studies of populations at high risk may be fruitful.
Other minority populations experience an excess stroke risk. African Americans, particularly at younger ages, suffer an excess burden (21, 22). In the predominantly Black Hispanic population of northern Manhattan (New York City), Hispanics are at greater risk of first stroke compared with non-Hispanic Whites. The interaction of age and race/ethnicity demonstrates a higher relative stroke burden for young minority populations compared with older minority populations when comparisons are made with non-Hispanic Whites.
In the current study, a significant interaction of age and ethnicity was demonstrated for ischemic stroke incidence. The etiology of this interaction is poorly understood. Competing mortality does not explain the finding (8), but cohort factors remain to be investigated. An interaction was not seen for intracerebral hemorrhage or subarachnoid hemorrhage, but a trend for an age-ethnicity interaction was seen for intracerebral hemorrhage.
Inclusion of out-of-hospital stroke cases accounted for 5.6 percent of all stroke cases and 14.2 percent of all transient ischemic attacks in the current study, emphasizing the importance of incorporating these measures in estimates of total stroke incidence. We expected higher out-of-hospital totals in non-Hispanic Whites compared with Mexican Americans because of greater access to outpatient services for non-Hispanic Whites. The differences, however, were minimal. These differences may be greater in immigrant communities.
This study provides population-based data from a multi-ethnic community. We must be cautious about generalizing these results, particularly to immigrant communities. Although every attempt was made to capture all events, there is the possibility of missing data. Direct neurologic examinations and neuroimaging review would have been the ideal way to validate cases, but these were impractical in a large population-based work. It is especially unlikely that the potential sources of bias would affect the direction of risk ratio estimates.
Stroke burden encompasses incidence, stroke severity, and outcome, including disability and mortality. This paper demonstrates clear incidence differences and does not suggest that Mexican Americans have less stroke severity. Additional research is needed to determine if differences in disability and mortality exist.
Mexican Americans are the largest component of the largest minority population in the United States. Their risk of stroke is substantially elevated compared with that of non-Hispanic Whites. As the Mexican-American population ages and continues its fast growth, the medical, social, and economic impacts of stroke will be felt throughout the United States. Efforts to specifically target Mexican Americans for stroke prevention and acute stroke therapy are indicated.
Acknowledgments
This study was funded by grant RO1 NS38916 from the National Institutes of Health.
References
- 1.US Census Bureau. United States Census 2000. Washington, DC: US Census Bureau, 2003. (http://www.census.gov/main/www/cen2000.html). (Accessed October 10, 2003).
- 2.American Stroke Association. Dallas, TX: American Heart Association, 2003. (http://www.strokeassociation.org). (Accessed October 10, 2003).
- 3.Hickenbottom SL, Fendrick AM, Kutcher JS, et al. A national study of the quantity and cost of informal caregiving for the elderly with stroke. Neurology. 2002;58:1754–9. doi: 10.1212/wnl.58.12.1754. [DOI] [PubMed] [Google Scholar]
- 4.Smith MA, Risser JMH, Lisabeth LD, et al. Access to care, acculturation and risk factors for stroke in Mexican Americans: the Brain Attack Surveillance in Corpus Christi Project. Stroke. 2003;34:2671–5. doi: 10.1161/01.STR.0000096459.62826.1F. [DOI] [PubMed] [Google Scholar]
- 5.Sundquist J, Winkleby MA, Pudaric S. Cardiovascular disease risk factors among older black, Mexican-American, and white women and men: an analysis of NHANES III, 1988–1994. J Am Geriatr Soc. 2001;49:109–16. doi: 10.1046/j.1532-5415.2001.49030.x. [DOI] [PubMed] [Google Scholar]
- 6.Winkleby MA, Cubbin C. Influence of individual and neighbourhood socioeconomic status on mortality among black, Mexican-American, and white women and men in the United States. J Epidemiol Community Health. 2003;57:444–52. doi: 10.1136/jech.57.6.444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.He J, Muntner P, Chen J, et al. Factors associated with hypertension in the general population of the United States. Arch Intern Med. 2002;162:1051–8. doi: 10.1001/archinte.162.9.1051. [DOI] [PubMed] [Google Scholar]
- 8.Morgenstern LB, Spears WD, Goff DC, Jr, et al. African Americans and women have the highest stroke mortality in Texas. Stroke. 1997;28:15–18. doi: 10.1161/01.str.28.1.15. [DOI] [PubMed] [Google Scholar]
- 9.Poe GS, Powell-Griner E, McLaughlin JK, et al. Comparability of the death certificate and the 1986 National Mortality Follow-back Survey. Vital Health Stat. 1993;2(118):1–53. [PubMed] [Google Scholar]
- 10.Piriyawat P, Smajsova M, Smith MA, et al. Comparison of active and passive cerebrovascular surveillance: the Brain Attack Surveillance in Corpus Christi (BASIC) Study. Am J Epidemiol. 2002;156:1062–9. doi: 10.1093/aje/kwf152. [DOI] [PubMed] [Google Scholar]
- 11.Al-Wabil A, Cox MA, Moye LA, et al. Improving efficiency of stroke research: the Brain Attack Surveillance in Corpus Christi (BASIC) Study. J Clin Epidemiol. 2003;56:351–7. doi: 10.1016/s0895-4356(03)00005-2. [DOI] [PubMed] [Google Scholar]
- 12.Morgenstern LB, Wein TH, Smith MA, et al. Comparison of stroke hospitalization rates among Mexican Americans and non-Hispanic whites. Neurology. 2000;54:2000–2. doi: 10.1212/wnl.54.10.2000. [DOI] [PubMed] [Google Scholar]
- 13.Asplund K, Tuomilehto J, Stegmayr B, et al. Diagnostic criteria and quality control of the registration of stroke events in the MONICA project. Acta Med Scand Suppl. 1988;728:26–39. doi: 10.1111/j.0954-6820.1988.tb05550.x. [DOI] [PubMed] [Google Scholar]
- 14.Gillum R, Fortmann S, Prineas R, et al. International diagnostic criteria for acute myocardial infarction and acute stroke. Am Heart J. 1984;108:150–8. doi: 10.1016/0002-8703(84)90558-1. [DOI] [PubMed] [Google Scholar]
- 15.Smith MA, Risser JMH, Moye LA, et al. Designing multi-ethnic stroke studies: the Brain Attack Surveillance in Corpus Christi (BASIC) Project. Ethn Dis (in press). [PubMed]
- 16.Morgenstern LB, Luna-Gonzales H, Huber JC, Jr, et al. Worst headache and subarachnoid hemorrhage: prospective modern CT and spinal fluid analysis. Ann Emerg Med. 1998;32:297–304. [PubMed] [Google Scholar]
- 17.Williams LS, Yilmaz EY, Lopez-Yunez AM. Retrospective assessment of initial stroke severity with the NIH Stroke Scale. Stroke. 2000;31:858–62. doi: 10.1161/01.str.31.4.858. [DOI] [PubMed] [Google Scholar]
- 18.Morgenstern LB, Steffen-Batey L, Smith MA, et al. Barriers to stroke prevention and acute stroke treatment in Mexican Americans. Stroke. 2001;32:1360–4. doi: 10.1161/01.str.32.6.1360. [DOI] [PubMed] [Google Scholar]
- 19.Christian JB, Lapane KL, Toppa RS. Racial disparities in receipt of secondary stroke prevention agents among US nursing home residents. Stroke. 2003;34:2693–7. doi: 10.1161/01.STR.0000096993.90248.27. [DOI] [PubMed] [Google Scholar]
- 20.Sahoo T, Johnson EW, Thomas JW, et al. Mutations in the gene encoding KRIT1, a Krev-1/rap1a binding protein, cause cerebral cavernous malformations (CCM1) Hum Mol Genet. 1999;8:2325–33. doi: 10.1093/hmg/8.12.2325. [DOI] [PubMed] [Google Scholar]
- 21.Sacco RL, Boden-Albala B, Gan R, et al. Stroke incidence among White, Black, and Hispanic residents of an urban community: the Northern Manhattan Stroke Study. Am J Epidemiol. 1998;147:259–68. doi: 10.1093/oxfordjournals.aje.a009445. [DOI] [PubMed] [Google Scholar]
- 22.Kissela B, Schneider A, Kleindorfer D, et al. Stroke in a biracial population: the excess burden of stroke among Blacks. Stroke. 2004;35:426–31. doi: 10.1161/01.STR.0000110982.74967.39. [DOI] [PubMed] [Google Scholar]


