Abstract
Entrapment of catheter components during cardiologic interventions is rare but can cause life-threatening complications and the need for emergency cardiac surgery. We report our surgical series of patients who have experienced entrapped guidewires, Rotablator Systems, and stents after cardiologic interventions.
Nine patients were referred for emergency surgery after entrapment of catheter remnants and ensuing acute ischemia. Guidewire fragments persisted in the left anterior descending coronary artery (2 patients) and in the right coronary artery (1 patient); Rotablator Systems lodged in the right coronary artery (2 patients); and stents were entrapped in the left anterior descending coronary artery (3 patients) and in the ramus circumflexus (1 patient).
Patients were referred for surgical therapy within 132 ± 30 min of device entrapment. Surgical procedures included coronary artery bypass grafting and removal of Rotablators or guidewires. Entrapped stents were left in situ, and additional coronary artery bypass grafting was performed. All patients survived. There were no signs of perioperative myocardial infarction.
We conclude that surgical strategy has to be individualized in patients with entrapped catheter remnants. The removal of entrapped stents or small fragments of catheter components seems not to be mandatory, if these are contained within small, chronically occluded coronary vessels or within a distal segment.
Key words: Angioplasty, transluminal, percutaneous coronary/adverse effects; coronary thrombosis/prevention & control; coronary vessels; device removal; emergencies; equipment failure; foreign bodies/surgery; heart catheterization; iatrogenic disease; intraoperative complications; myocardial revascularization; prosthesis failure; stents/adverse effects
Entrapment of catheter remnants (guidewire, stent, Rotablator) in coronary arteries is a rare but serious complication of percutaneous coronary intervention, with hazardous potential for the patient. Retrieval of these remnants from the coronary circulation with various interventional devices is a readily available and technically familiar approach that has a relatively high success rate.1
Despite this, up to 15% to 20% of patients with failed percutaneous retrieval of misplaced catheter remnants are referred to emergent cardiac surgery, which still carries a significant perioperative risk.2,3 Stent embolization or misplacement has been reported in 0.3% to 1.2% of percutaneous transluminal coronary angioplasty (PTCA) interventions.1,2,4 The incidence of guidewire or Rotablator (Rotablator© Rotational Atherectomy System, Boston Scientific; Natick, Mass) entrapment is difficult to determine, as there are only scattered case reports to go by.5,6 The optimal surgical management and outcome for these last patients remain unknown. Herein, we report our surgical experience and approach with patients who experience entrapment of catheter remnants.
Patients and Methods
From January 1998 through December 2003, 9 patients (6 women and 3 men; mean age, 71.4 ± 6.2 years) were referred for emergency cardiosurgical therapy at our institution after cardiologic intervention resulting in entrapment of catheter remnants. The clinical data on the patients are presented in Table I.
Table I. Patients and Clinical Data
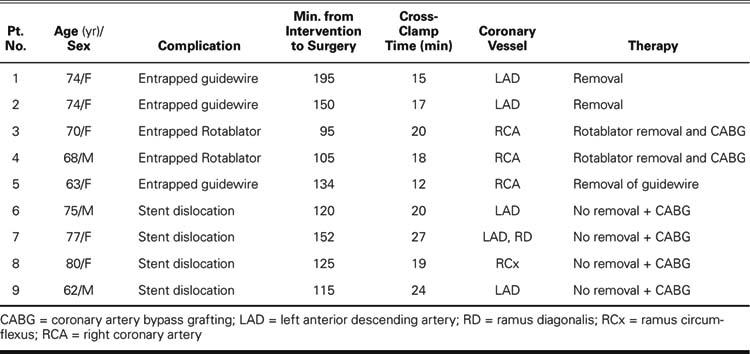
Guidewires rested in the left anterior descending coronary artery (LAD) (2 patients) and in the right coronary artery (RCA) (1 patient). Stents were entrapped in the LAD (3 patients) and in the ramus circumflexus (RCx) (1 patient). In 2 patients, a Rotablator System lodged in the RCA, which is illustrated in Figure 1. In 1 patient, a stent was entrapped between the LAD and the 1st diagonal branch, with secondary perforation of the LAD. The indication for operation in all patients was acute ischemia (ST elevation) as shown by electrocardiography after frustrated attempts at retrieval per catheter.

Fig. 1 Rotablato© tip perforating the right coronary artery (*).
Results
Patients were referred for surgical therapy within 132 ± 30 min of the device entrapment. Cardiopulmonary bypass was performed under normothermia, and myocardial protection was provided with antegrade blood cardioplegia. The mean cross-clamp time was 19.1 ± 4.5 min.
The 2 entrapped Rotablator Systems were retrieved through an aortotomy, and coronary artery bypass grafting (CABG) was performed. All patients (n=4) with an entrapped stent received CABG surgery alone, without stent removal. The 3 entrapped guidewires were completely removed, with the exception of a small wire fragment in the distal RCA. In that case, CABG was not performed due to the small diameter of the vessel. In the event of LAD bypass, the left internal mammary artery (LIMA) was used in all patients.
The survival rate was 100%. No perioperative complications were observed. There were no signs of perioperative myocardial infarction as indicated by clinical chemistry (CK >10 μmol/L/sec, with a CK-MB proportion >10%) or by electrocardiographic changes (new Q waves, ST elevation, or R-wave depression). All patients received a combination of aspirin and clopidogrel for 9 months postoperatively and were observed at 3-month intervals during the 1st postoperative year.
The 1-year follow-up was uneventful for all patients; in particular, no patient required further reintervention for angina or signs of ischemia.
Discussion
Patients with catheter remnants that were entrapped during PTCA remain a particular challenge, because little is known about the incidence and clinical outcome.2,7 In addition, no guidelines exist for optimal surgical management. This complication is life-threatening because it can lead to myocardial ischemia, infarction, or lethal arrhythmia due to intracoronary thrombosis. Studies using intravascular ultrasound have shown that incompletely expanded stents are frequently associated with acute or subacute stent thrombosis.8,9
The primary therapeutic option is interventional retrieval by means of specialized harvesting devices.10 In the event of failed interventional retrieval and persistent signs of ischemia, patients should be urgently referred to surgery.
The success of surgery in this circumstance is determined primarily by the clinical status of the patient before the operation. For patients in cardiogenic shock, the risk of death remains 20% to 50%.11–13 Additional risk factors depend upon the duration, extent, and location of ischemia. In the event of preoperative myocardial ischemia, the risk of perioperative infarction is 40% to 70%—but that risk drops to 2% to 4% in cases without preoperative myocardial ischemia.3
In our series, all patients had signs of ischemia, yet there was no perioperative myocardial infarction. The successful outcome for these patients was due, we believe, to a clear recognition of the problem and a short interval between failed intervention and emergency operation. Other groups14,15 have shown that patients who have a perioperative infarction experience significantly more delay between failed PTCA and emergency operation than do patients who have no infarction.
Intraoperative decisions about removing or leaving in situ the catheter remnants or stents should depend upon the location and size of the fragment, and the size of the coronary artery. In addition, the surgeon should consider the risk of further traumatizing the affected coronary artery by forcefully removing the foreign body. Despite their thrombogenicity, catheter remnants or stents need not be removed unless they protrude into the ascending aorta, which creates a risk of thrombotic embolization to cerebral and other peripheral vessels. Embolization of the wire itself is a low risk, because it usually is firmly fixed within the coronary artery. Small fragments of wire or misplaced stents may be left within the coronary artery without adverse sequelae, especially if they are contained within small, chronically occluded coronary vessels or within a distal part of the vessel.16,17
This complication is both uncommon and subject to reporting bias. The literature on surgical intervention for entrapped stents is sparse, and the commonly proposed therapy is obligatory removal of the foreign body from the coronary circulation.18–21 However, our clinical data show that removal of entrapped stents seems not to be obligatory. Early surgical intervention, including rapid CABG surgery to the supplied myocardium, is essential to a low mortality rate in this high-risk group. Finally, medical liability should be considered in cases of entrapped catheter components. Patients should receive detailed explanation of the risks of a remnant, even after a successful interventional procedure.
Footnotes
Address for reprints: Konstantin Alexiou, MD, Department of Cardiac Surgery, Heart Center Dresden Ltd., Technical University of Dresden, Fetscherstr. 76, D-01307 Dresden, Germany. E-mail: M.Weber@herzzentrum-dresden.com
References
- 1.Eggebrecht H, Haude M, von Birgelen C, Oldenburg O, Baumgart D, Herrmann J, et al. Nonsurgical retrieval of embolized coronary stents. Catheter Cardiovasc Interv 2000; 51:432–40. [DOI] [PubMed]
- 2.Kozman H, Wiseman AH, Cook JR. Long-term outcome following coronary stent embolization or misdeployment. Am J Cardiol 2001;88:630–4. [DOI] [PubMed]
- 3.Reidemeister JC, Wolfhard U. Direct coronary bypass operation in complicated coronary dissection [in German]. Z Kardiol 1996;85 Suppl 1:67–72. [PubMed]
- 4.Nikolsky E, Gruberg L, Pechersky S, Kapeliovich M, Grenadier E, Amikam S, et al. Stent deployment failure: reasons, implications, and short- and long-term outcomes. Catheter Cardiovasc Interv 2003;59:324–8. [DOI] [PubMed]
- 5.Breisblatt WM. Inflated balloon entrapped in a calcified coronary stenosis. Cathet Cardiovasc Diagn 1993;29:224–8. [DOI] [PubMed]
- 6.Ellis SG, Ajluni S, Arnold AZ, Popma JJ, Bittl JA, Eigler NL, et al. Increased coronary perforation in the new device era. Incidence, classification, management, and outcome. Circulation 1994;90:2725–30. [DOI] [PubMed]
- 7.Cantor WJ, Lazzam C, Cohen EA, Bowman KA, Dolman S, Mackie K, et al. Failed coronary stent deployment. Am Heart J 1998;136:1088–95. [DOI] [PubMed]
- 8.Moussa I, Di Mario C, Reimers B, Akiyama T, Tobis J, Colombo A. Subacute stent thrombosis in the era of intravascular ultrasound-guided coronary stenting without anticoagulation: frequency, predictors and clinical outcome. J Am Coll Cardiol 1997;29:6–12. [DOI] [PubMed]
- 9.Colombo A, Hall P, Nakamura S, Almagor Y, Maiello L, Martini G, et al. Intracoronary stenting without anticoagulation accomplished with intravascular ultrasound guidance. Circulation 1995;91:1676–88. [DOI] [PubMed]
- 10.Elsner M, Zeiher AM. Perforation and rupture of coronary arteries [in German]. Herz 1998;23:311–8. [DOI] [PubMed]
- 11.Holmes DR Jr, Holubkov R, Vlietstra RE, Kelsey SF, Reeder GS, Dorros G, et al. Comparison of complications during percutaneous transluminal coronary angioplasty from 1977 to 1981 and from 1985 to 1986: the National Heart, Lung, and Blood Institute Percutaneous Transluminal Coronary Angioplasty Registry. J Am Coll Cardiol 1988;12:1149–55. [DOI] [PubMed]
- 12.Morris RJ, Kuretu ML, Grunewald KE, Samuels LE, Strong MD, Wechsler AS. Surgical treatment of interventional coronary angiographic accidents. Angiology 1999;50:789–95. [DOI] [PubMed]
- 13.Talley JD, Weintraub WS, Roubin GS, Douglas JS Jr, Anderson HV, Jones EL, et al. Failed elective percutaneous transluminal coronary angioplasty requiring coronary artery bypass surgery. In-hospital and late clinical outcome at 5 years. Circulation 1990;82:1203–13. [DOI] [PubMed]
- 14.Klepzig H Jr, Kober G, Satter P, Kaltenbach M. Analysis of 100 emergency aortocoronary bypass operations after percutaneous transluminal coronary angioplasty: which patients are at risk for large infarctions? Eur Heart J 1991; 12:946–51. [PubMed]
- 15.Reul GJ, Cooley DA, Hallman GL, Duncan JM, Livesay JJ, Frazier OH, et al. Coronary artery bypass for unsuccessful percutaneous transluminal coronary angioplasty. J Thorac Cardiovasc Surg 1984;88(5 Pt 1):685–94. [PubMed]
- 16.Hartzler GO, Rutherford BD, McConahay DR. Retained percutaneous transluminal coronary angioplasty equipment components and their management. Am J Cardiol 1987;60:1260–4. [DOI] [PubMed]
- 17.Sethi GK, Ferguson TB Jr, Miller G, Scott SM. Entrapment of broken guidewire in the left main coronary artery during percutaneous transluminal coronary angioplasty. Ann Thorac Surg 1989;47:455–7. [DOI] [PubMed]
- 18.Erez E, Herz I, Snir E, Raanani E, Menkes H, Vidne BA. Surgical removal of stent entrapped in proximal left coronary artery system. Ann Thorac Surg 1996;62:884–5. [PubMed]
- 19.Chang TM, Pellegrini D, Ostrovsky A, Marrangoni AG. Surgical management of entrapped percutaneous transluminal coronary angioplasty hardware. Tex Heart Inst J 2002; 29:329–32. [PMC free article] [PubMed]
- 20.Fukui T, Takanashi S, Mihara W, Ishikawa K, Hosoda Y. Coronary endarterectomy and stent removal after iatrogenic perforation. Ann Thorac Surg 2004;77:708–11. [DOI] [PubMed]
- 21.Shekar PS, Leacche M, Farnam KA, Hernandez CG, Couper GS, Byrne JG. Surgical management of complications of percutaneous coronary rotational atherectomy interventions. Ann Thorac Surg 2004;78:e81–2. [DOI] [PubMed]


