Abstract
There is an interest in the use of high thoracic epidural anesthesia in cardiac surgery, because experimental and clinical studies have suggested that central neuroaxial blockade attenuates the response to surgical stress and improves myocardial metabolism and perioperative analgesia—thus enabling earlier extubation and a smoother postoperative course.
Matters of major concern in the adoption of high thoracic epidural anesthesia in cardiac surgery are neurologic injury secondary to neuroaxial hematoma and hypotension secondary to sympatholysis. The risk associated with possible neuraxial hematoma caused by high thoracic epidural anesthesia has been thoroughly investigated and largely discounted, but scant attention has been devoted to the onset of hypotensive episodes in the same setting. We analyzed the hypotensive episodes that occurred in a series of 144 patients who underwent on-pump cardiac surgery procedures. Among the patient variables that we tested in a multivariate logistic-regression model, only female sex was found to be significantly correlated with hypotension.
In order to decrease the incidence and severity of hypotensive episodes resulting from anesthetic blockade, anesthesiologists need to monitor, with special care, women patients who are under high thoracic epidural anesthesia. Further studies are needed in order to determine why women undergoing open heart surgery under high thoracic epidural anesthesia are at a relatively greater risk of hypotension.
Key words: Analgesia, epidural; anesthesia, epidural; blood pressure; cardiac surgical procedures; heart/innervation; hypotension/chemically induced; sympathetic nervous system/drug effects; vascular resistance/drug effects
There is an interest in the use of high thoracic epidural anesthesia (HTEA) in cardiac surgery, because experimental1–5 and clinical6–21 studies have suggested that central neuroaxial blockade—which has reversible sympatholytic effects—has the capability to attenuate the response to surgical stress and to improve both myocardial metabolism and perioperative analgesia. These beneficial effects have been proved to enable earlier extubation and a smoother postoperative course.
Despite these advantages, epidural anesthesia has not gained widespread acceptance in cardiac surgery because of concerns regarding the potential development of such sequelae as spinal cord injury (associated with neuroaxial hematoma), epidural infection, and hypotension (secondary to sympatholysis induced by anesthetic blockade).
Various aspects of the hazard of epidural hematoma have been thoroughly investigated,11,22–27 and the risk has been held to be negligible—nothing that would contraindicate the use of HTEA in selected patients.11 Infection may be prevented by the meticulous use of aseptic techniques.27 The hypotension that can ensue when HTEA is implemented28–31 has received scant attention to date.
In this retrospective study, we recorded and analyzed all hypotensive episodes and attempted to find any statistically significant correlation between the development of hypotension and a number of patient variables. These included age, sex, weight, height, body mass index (BMI), ejection fraction, reoperation, history of myocardial infarction, history of hypertension, use of vasoactive drugs, peripheral artery disease, and surgical procedure.
Patients and Methods
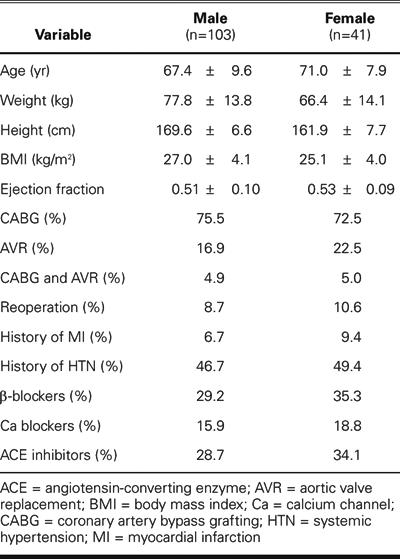
The study population consisted of 144 consecutive patients (103 men and 41 women). Their mean age was 68.4 years (range, 42–88 years). Their chief clinical characteristics are shown in Table I. From 1 April 2004 through 31 January 2005, the patients underwent—as isolated or combined procedures—coronary artery bypass grafting or aortic valve replacement for moderate-to-severe stenosis, under HTEA combined with general anesthesia.
Table I. Patients' Characteristics by Sex
In order to join the HTEA group, patients had to qualify for elective surgery and to have the following coagulation test results: activated partial thromboplastin time <45 seconds (normal, 25–30 s), PT-INR value <1.4, and platelet count greater than 80,000 plt/mm3 (normal, 150,000–400,000 plt/mm3). Among the exclusion criteria were the administration of ticlopidine within 15 days before surgery and the administration of platelet glycoprotein IIb/IIIa inhibitors. In common with previous investigators,22–26 we did not consider treatment with low-molecular-weight heparin and aspirin below the dosage of 160 mg/day to be contraindications to the procedure. Patients with significant aortic insufficiency were also excluded from the study in order to avoid introducing further variables that could influence hemodynamic response to the procedure.
In all patients, preoperative medical therapy, including transcutaneously administered nitrates, was given until the day of surgery, with the exception of diuretics and aspirin, which were discontinued 48 hours before surgery. Informed consent was obtained from each patient.
The surgical risk in this series was assessed by the Parsonnet score.32 Fifteen patients out of 144 had peripheral artery disease and were in stages IIa, IIb, or III of the Fontaine's classification33 or had undergone previous arterial surgery or endovascular procedures.
One hour before being taken to the operating room, patients were injected intramuscularly with atropine (10 μg/kg), fentanyl (1 μg/kg), and droperidol (0.35 mg/kg). The patients were then transferred to the waiting area of the operating room, where peripheral venous access was established and electrocardiographic (ECG) monitoring (Marquette Solar® 8000 M, GE Medical Systems; Bradford, UK) was initiated in leads II and V5. An epidural 19-gauge catheter (Flex Tip Plus®, Arrow International; Reading, Pa) was inserted at the level of the T3–T4 intervertebral space and advanced 4 cm in the attempt to reach the T1 vertebral body. A test dose of 2 mL of 2% lidocaine was administered in order to exclude subarachnoid displacement of the catheter. Arterial blood pressure was monitored via a cannula (Marquette Solar 8000 M) placed in the radial artery.
After 2 hours of observation in the waiting area, during which the patient was monitored for the development of neurologic complications, 7 mL/kg of crystalloid solution was given over 20 minutes; then 0.5% bupivacaine (0.15 mg/cm body length) and alfentanil (6 μg/cm body length) were slowly delivered through the epidural catheter. The extent of neural blockage was checked by a pinprick. Patients were then taken to the operating room, where general anesthesia was induced intravenously with alfentanil (6 μg/kg), propofol (1–1.5 mg/kg), and vecuronium (0.1 mg/kg) and maintained with an infusion of propofol (3–5 mg/kg/h) and a bolus dose of vecuronium (0.02 mg/kg) every 20 minutes. Continuous infusion of bupivacaine (0.06 mg/cm body length/h) and alfentanil (3 μg/cm body length/h) was administered through the epidural catheter and continued until 48 hours after the end of the operation.
Arterial blood pressure was continuously monitored throughout the procedure. Hypotension—defined as a 30% decrease in mean arterial pressure in comparison with basal levels, or as a mean absolute blood pressure value ≤60 mmHg for ≥5 minutes28,29—was treated with a continuous infusion of noradrenaline at an initial dose of 0.01 μg/kg/min until basal levels were restored. A 300-IU/kg dose of heparin was given immediately before the arterial cannula was inserted into the aorta, and subsequent doses were administered in bolus in order to maintain an activated coagulation time >450 seconds. Moderate hypothermia was induced (32 °C) during cardiopulmonary bypass. After discontinuation of cardiopulmonary bypass, protamine sulfate was administered at a dose of 1 mg/100 IU of heparin. After the operation, the patients were transferred to the intensive care unit. Vasoconstrictors were not required in any of the patients during the postoperative period.
Neurologic assessment was performed on the patients upon their awakening and after extubation. Neurologic signs and symptoms (radicular pain, paresthesia, and temporary or permanent paralysis) were continuously monitored until discharge from the intensive care unit. No additional analgesic drugs were required during the postoperative period.
Statistical Analysis
Using an explorative-descriptive method, χ2 tests were performed to evaluate the relationship between patients' descriptive and clinical variables and the onset of hypotension. A multivariate logistic-regression analysis was applied to the results of the bivariate statistical analyses in order to estimate the independent contribution of each predictor to the explanation of the hypotensive outcome. The presence or absence of hypotension constituted the binary response variable in the logistic-regression model, whereas the predictors were sex, BMI, and chronic treatment with calcium channel blockers. The discriminative power of the logistic regression model was checked with a receiver operating characteristic (ROC) curve. The 2-sided alpha level for statistical testing was 0.05. All analyses were performed using SPSS statistical software (version 12.0, SPSS Inc.; Chicago, Ill).
Results
Anesthesia that made use of HTEA was adopted in 144 patients. Although the expected mean mortality rate for our study population predicted by the Parsonnet score32 was 5%, no deaths occurred in this series. Of the 144 patients who were submitted to HTEA, 25 developed hypotension during the 30-min interval after the administration of bupivacaine and alfentanil into the epidural space. Table II shows the relationships between patient variables and onset of hypotension.
Table II. Patients' Characteristics and Clinical Presentation*
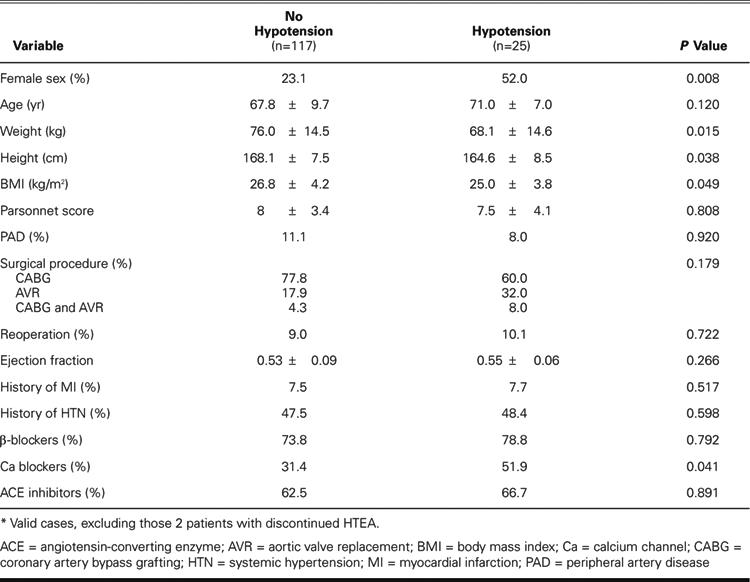
Of the 106 patients who underwent isolated coronary bypass grafting, 15 developed hypotension. This occurred in 7 of the 77 men and in 8 of the 29 women belonging to this group. In the group undergoing isolated aortic valve replacement, 8 patients out of 29 developed hypotension (5 out of 20 men and 3 out of 9 women). Of the 7 patients (5 men and 2 women) who underwent combined underwent coronary artery bypass grafting and aortic valve replacement, both women presented hypotension. A statistically significant correlation was found between hypotension and female sex (P=0.008) (Table II).
As could be expected, hypotension was more frequent among patients with isolated aortic valve stenosis and aortic stenosis associated with coronary artery disease than among those with coronary artery disease alone, albeit with values that were not statistically significant.
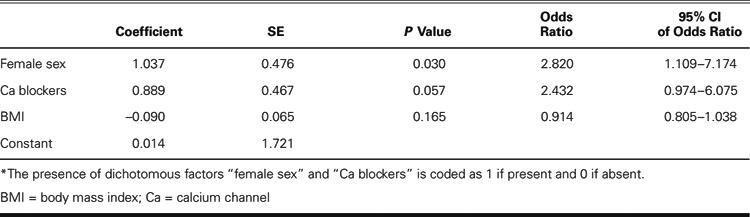
Bivariate statistical analysis demonstrated, in addition to female sex, a significant correlation between hypotension and BMI (P=0.049) and with the preoperative use of calcium channel blockers (P=0.041). When these 3 factors were analyzed in a multivariate logistic regression model, only female sex was found to be statistically correlated with hypotension (P=0.030), with an odds ratio of 2.82 (95% confidence interval, 1.109–7.174) (Table III).
TABLE III. Results of the Logistic Regression Analysis*
The area under the ROC curve was 0.74, with a 95% confidence interval of 0.63–0.84 (Fig. 1)
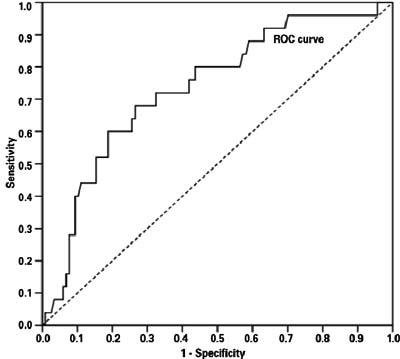
Fig. 1 Receiver operating characteristic (ROC) curve of the logistic regression model. The area under the ROC curve was 0.74, with a 95% confidence interval of 0.63–0.84.
No patient presented clinical signs suggestive of epidural hematoma or neuraxial injury. Two procedures were discontinued because of accidental injection of the anesthetic solution into the intrathecal space. In these 2 patients, computed tomographic scanning of the cervical segment showed dislocation of the epidural catheter into the subarachnoid space. Both patients required endotracheal intubation and mechanical ventilation. One of them was extubated after 1 hour, and the operation was postponed until the next day. In the other patient, the unstable cardiac condition contraindicated postponement of the operation, which was performed immediately under total intravenous anesthesia. Neither patient experienced neurologic sequelae, and both were discharged from the hospital on the 7th postoperative day.
Discussion
Epidural anesthesia in cardiac surgery has gained interest because of the potential advantages the technique can offer, including improved analgesia,6,7 attenuation of response to surgical stress,8–11 improved distribution of coronary blood flow,12–17 reduced oxygen demand,13,17 improved postoperative respiratory function,18–21 faster recovery of awareness, and establishment of spontaneous ventilation.21
The risk of neuraxial hematoma, generally regarded as the most serious complication of peridural anesthesia, has been thoroughly investigated.11,22–26 In particular, a statistical calculation of the risk of paraplegia secondary to hematoma formation in the cardiac surgical population who underwent HTEA—carried out using data from all relevant small studies published prior to 2000—showed that the risk varied between a minimum 1:150,000 and maximum of 1:1,500, with a 95% confidence interval.26 No patient in our series presented clinical signs suggestive of epidural hematoma or neuraxial injury.
Infection is an ever-present threat when invasive procedures are performed. The potentially serious consequences of an epidural infection, which include epidural and paraspinal abscesses, as well as meningitis, must be kept in mind when adopting HTEA.27 In our series, meticulous aseptic techniques were used, and, as an additional precautionary measure, we applied subcutaneous tunneling, cuffs, and bacterial filters. No epidural catheter infection was observed.
The patients in our series were easily extubated within a few hours after surgery; they could be mobilized early and were generally discharged from the intensive care unit within 12 hours after the intervention, thus confirming the experience reported in the literature.19–21
The hypotensive effect of HTEA and its possible consequences have received scant attention in the literature.29–31 In our series of patients, hypotension was observed in 25 out of 142 patients (17.6%) during the 30-min interval after the administration of bupivacaine and alfentanil into the epidural space. This occurrence was easily corrected by administering a low dose of vasoconstrictors, without untoward effects or complications.
The association between hypotension and HTEA was tested against a number of patient variables: age, weight, height, BMI, sex, peripheral artery disease, ejection fraction, history of myocardial infarction, history of hypertension, type of surgical procedure, reoperation, and chronic treatment with calcium channel blockers, β-blockers, and angiotensin-converting enzyme (ACE) inhibitors.
Bivariate statistical analysis has demonstrated a significant correlation between hypotension and female sex, BMI, and the preoperative use of calcium channel blockers. When these 3 factors were analyzed with a logistic regression model, only female sex was found to be a significant predictor of hypotension. In contrast with previously reported findings,31 no relationship was found between peripheral artery disease and the development of hypotension in this group of patients.
The results of the present study cannot account for why women experienced hypotension more frequently than men. Presumably, additional variables (such as unrecognized thyroid disease and hormonal profile) will need to be included in a larger sample of patients in order to elucidate this finding.
Conclusions
In our study, HTEA was proved safe when applied to selected patients and when precise guidelines were followed. In our series, no deaths occurred and no neurologic sequelae were observed. Hypotension secondary to sympatholysis induced by anesthetic blockade arises more frequently in women than in men. In order to decrease the incidence and severity of hypotensive episodes resulting from anesthetic blockade, anesthesiologists need to monitor, with special care, women who are under high thoracic epidural anesthesia. Such hypotension is easily corrected by the administration of a low dose of vasoconstrictors. Further studies are needed in order to determine why women undergoing open heart surgery under HTEA are at a relatively greater risk of hypotension.
Acknowledgment
The authors wish to thank Deborah Ciullo for her secretarial assistance.
Footnotes
Address for reprints: Stefano Casalino MD, Clinica San Gaudenzio, Via Bottini 3, 28100 Novara, Italy. E-mail: casalino63@libero.it
Dr. Stelian is on fellowship from the “C.C. Iliescu” Institute, Bucharest, Romania
References
- 1.Klassen GA, Bramwell RS, Bromage PR, Zborowska-Sluis DT. Effect of acute sympathectomy by epidural anesthesia on the canine coronary circulation. Anesthesiology 1980; 52:8–15. [DOI] [PubMed]
- 2.Flatley KA, DeFily DV, Thomas JX Jr. Effects of cardiac sympathetic nerve stimulation during adrenergic blockade on infarct size in anesthetized dogs. J Cardiovasc Pharmacol 1985;7:673–9. [DOI] [PubMed]
- 3.Davis RF, DeBoer LW, Maroko PR. Thoracic epidural anesthesia reduces myocardial infarct size after coronary artery occlusion in dogs. Anesth Analg 1986;65:711–7. [PubMed]
- 4.Blomberg S, Ricksten SE. Thoracic epidural anaesthesia decreases the incidence of ventricular arrhythmias during acute myocardial ischaemia in the anaesthetized rat. Acta Anaesthesiol Scand 1988;32:173–8. [DOI] [PubMed]
- 5.Rolf N, Van de Velde M, Wouters PF, Mollhoff T, Weber TP, Van Aken HK. Thoracic epidural anesthesia improves functional recovery from myocardial stunning in conscious dogs. Anesth Analg 1996;83:935–40. [DOI] [PubMed]
- 6.Scott NB, Turfrey DJ, Ray DA, Nzewi O, Sutcliffe NP, Lal AB, et al. A prospective randomized study of the potential benefits of thoracic epidural anesthesia and analgesia in patients undergoing coronary artery bypass grafting. Anesth Analg 2001;93:528–35. [DOI] [PubMed]
- 7.Ho SC, Royse CF, Royse AG, Penberthy A, McRae R. Persistent pain after cardiac surgery: an audit of high thoracic epidural and primary opioid analgesia therapies. Anesth Analg 2002;95:820–3. [DOI] [PubMed]
- 8.Stenseth R, Bjella L, Berg EM, Christensen O, Levang OW, Gisvold SE. Thoracic epidural analgesia in aortocoronary bypass surgery. II: Effects on the endocrine metabolic response. Acta Anaesthesiol Scand 1994;38:834–9. [DOI] [PubMed]
- 9.Liem TH, Booij LH, Gielen MJ, Hasenbos MA, van Egmond J. Coronary artery bypass grafting using two different anesthetic techniques: Part 3: Adrenergic responses. J Cardiothorac Vasc Anesth 1992;6:162–7. [DOI] [PubMed]
- 10.Kirno K, Friberg P, Grzegorczyk A, Milocco I, Ricksten SE, Lundin S. Thoracic epidural anesthesia during coronary artery bypass surgery: effects on cardiac sympathetic activity, myocardial blood flow and metabolism, and central hemodynamics. Anesth Analg 1994;79:1075–81. [PubMed]
- 11.Williams J. Thoracic epidural anesthesia for cardiac surgery. Can J Anesth 2002;49(Suppl 1):7R.
- 12.Loick HM, Schmidt C, Van Aken H, Junker R, Erren M, Berendes E, et al. High thoracic epidural anesthesia, but not clonidine, attenuates the perioperative stress response via sympatholysis and reduces the release of troponin T in patients undergoing coronary artery bypass grafting. Anesth Analg 1999;88:701–9. [DOI] [PubMed]
- 13.Olausson K, Magnusdottir H, Lurje L, Wennerblom B, Emanuelsson H, Ricksten SE. Anti-ischemic and anti-anginal effects of thoracic epidural anesthesia versus those of conventional medical therapy in the treatment of severe refractory unstable angina pectoris. Circulation 1997;96:2178–82. [DOI] [PubMed]
- 14.Stenseth R, Berg EM, Bjella L, Christensen O, Levang OW, Gisvold SE. Effects of thoracic epidural analgesia on coronary hemodynamics and myocardial metabolism in coronary artery bypass surgery. J Cardiothorac Vasc Anesth 1995;9:503–9. [DOI] [PubMed]
- 15.Blomberg S, Emanuelsson H, Ricksten SE. Thoracic epidural anesthesia and central hemodynamics in patients with unstable angina pectoris. Anesth Analg 1989;69:558–62. [PubMed]
- 16.Kock M, Blomberg S, Emanuelsson H, Lomsky M, Stromblad SO, Ricksten SE. Thoracic epidural anesthesia improves global and regional left ventricular function during stress-induced myocardial ischemia in patients with coronary artery disease. Anesth Analg 1990;71:625–30. [DOI] [PubMed]
- 17.Blomberg S, Emanuelsson H, Kvist H, Lamm C, Ponten J, Waagstein F, Ricksten SE. Effects of thoracic epidural anesthesia on coronary arteries and arterioles in patients with coronary artery disease. Anesthesiology 1990;73:840–7. [DOI] [PubMed]
- 18.Liem TH, Hasenbos MA, Booij LH, Gielen MJ. Coronary artery bypass grafting using two different anesthetic techniques: Part 2: Postoperative outcome. J Cardiothorac Vasc Anesth 1992;6:156–61. [DOI] [PubMed]
- 19.Visser WA, Liem TH, Brouwer RM. High thoracic epidural anesthesia for coronary artery bypass graft surgery in a patient with severe obstructive lung disease. J Cardiothorac Vasc Anesth 2001;15:758–60. [DOI] [PubMed]
- 20.Tenling A, Joachimsson PO, Tyden H, Hedenstierna G. Thoracic epidural analgesia as an adjunct to general anaesthesia for cardiac surgery. Effects on pulmonary mechanics. Acta Anaesthesiol Scand 2000;44:1071–6. [DOI] [PubMed]
- 21.Stenseth R, Bjella L, Berg EM, Christensen O, Levang OW, Gisvold SE. Effects of thoracic epidural analgesia on pulmonary function after coronary artery bypass surgery. Eur J Cardiothorac Surg 1996;10:859–66. [DOI] [PubMed]
- 22.Horlocker TT, Wedel DJ, Schroeder DR, Rose SH, Elliott BA, McGregor DG, Wong GY. Preoperative antiplatelet therapy does not increase the risk of spinal hematoma associated with regional anesthesia. Anesth Analg 1995;80:303–9. [DOI] [PubMed]
- 23.Wheatley RG, Schug SA, Watson D. Safety and efficacy of postoperative epidural analgesia. Br J Anaesth 2001;87:47–61. [DOI] [PubMed]
- 24.Castellano JM, Durbin CG Jr. Epidural analgesia and cardiac surgery: worth the risk? Chest 2000;117:305–7. [DOI] [PubMed]
- 25.Ho AM, Chung DC, Joynt GM. Neuraxial blockade and hematoma in cardiac surgery: estimating the risk of a rare adverse event that has not (yet) occurred. Chest 2000;117:551–5. [DOI] [PubMed]
- 26.Sanchez R, Nygard E. Epidural anesthesia in cardiac surgery: is there an increased risk? J Cardiothorac Vasc Anesth 1998;12:170–3. [DOI] [PubMed]
- 27.Dawson S. Epidural catheter infections. J Hosp Infect 2001; 47:3–8. [DOI] [PubMed]
- 28.Buggy D, Higgins P, Moran C, O'Brien D, O'Donovan F, McCarroll M. Prevention of spinal anesthesia-induced hypotension in the elderly: comparison between preanesthetic administration of crystalloids, colloids, and no prehydration. Anesth Analg 1997;84:106–10. [DOI] [PubMed]
- 29.Buggy DJ, Power CK, Meeke R, O'Callaghan S, Moran C, O'Brien GT. Prevention of spinal anaesthesia-induced hypotension in the elderly: i.m. methoxamine or combined hetastarch and crystalloid. Br J Anaesth 1998;80:199–203. [DOI] [PubMed]
- 30.Hartmann B, Junger A, Klasen J, Benson M, Jost A, Banzhaf A, Hempelmann G. The incidence and risk factors for hypotension after spinal anesthesia induction: an analysis with automated data collection. Anesth Analg 2002;94:1521–9. [DOI] [PubMed]
- 31.Bromage PR. Epidural analgesia. Philadelphia; WB Saunders: 1978.
- 32.Gabrielle F, Roques F, Michel P, Bernard A, de Vicentis C, Roques X, et al. Is the Parsonnet's score a good predictive score of mortality in adult cardiac surgery: assessment by a French multicentre study. Eur J Cardiothorac Surg 1997; 11:406–14. [DOI] [PubMed]
- 33.Fontaine R, Kim M, Kieny R. Surgical treatment of peripheral circulation disorders [in German]. Helv Chir Acta 1954; 21:499–533. [PubMed]


