Abstract
The clinical presentation of myocarditis is variable and often mimics myocardial infarction. The diagnosis of acute myocarditis is frequently empiric, and is made on the basis of the clinical presentation, electrocardiographic changes, elevated cardiac enzymes, and lack of epicardial coronary artery disease. To date, the only widely available method for the diagnosis of myocarditis is myocardial biopsy. This procedure, although very specific, has limited sensitivity and substantial procedural morbidity and mortality rates. We present the case of a young woman who presented with chest pain and dramatic anteroseptal ST-segment elevation on electrocardiography. The diagnosis of acute myocarditis was eventually confirmed with use of cardiac magnetic resonance imaging.
Key words: Chest pain, coronary angiography, electrocardiography, gadolinium DTPA, magnetic resonance imaging, myocardial infarction/diagnosis, myocarditis/diagnosis/etiology, virus diseases/complications
The clinical presentation of patients with myocarditis is variable, ranging from fatigue to fulminant congestive heart failure and sudden death. Associated pericardial inflammation often causes precordial chest discom-fort and, together with diffuse electrocardiographic (ECG) changes, can mimic an acute coronary syndrome.1,2 The diagnosis of myocarditis is often empiric and is made on the basis of clinical presentation, ECG changes, elevated cardiac enzymes, and lack of epicardial coronary artery disease. We present a case of focal myocarditis in a patient who presented with chest pain and impressive anteroseptal ST-segment elevation on electrocardiography, mimicking an acute myocardial infarction.
Case Report
A 22-year-old woman with no relevant medical history presented at the emergency department of our institution with severe, substernal, crushing chest pain of 45 minutes' duration. The patient had not had radiation of the arm or neck but did report radiation of the back. She perceived no change in the quality of pain with position or on inspiration. Within the past week, she had experienced shortness of breath, diaphoresis, nausea, and vomiting. There was no current or past use of cocaine or other stimulants. She had no history of chest wall trauma. She reported having a gastrointestinal illness involving emesis and diarrhea the week before she developed the chest discomfort. She was afebrile. Her initial heart rate was 66 beats/min; blood pressure, 106/64 mmHg; and respiratory rate, 24 breaths/min with an oxygen saturation of 99% on room air.
The physical examination in the emergency room was notable for the absence of jugular venous distention, and regular heart rhythm with a physiologic, split 2nd heart sound and no audible murmur, gallop, or rub. She had clear lungs and no peripheral edema. A chest radiograph also revealed clear lungs with a normal-sized cardiac silhouette. The initial ECG revealed sinus rhythm with occasional premature ventricular beats and 1-mm down-sloping ST elevation in leads V1 and V2 (Fig. 1A). She was given aspirin and intravenous morphine, and her pain resolved. A repeat ECG revealed normalization of the ST-segment elevation with biphasic T waves in leads V1 and V2. A chest computed tomographic scan excluded the presence of aortic dissection or pulmonary embolus.
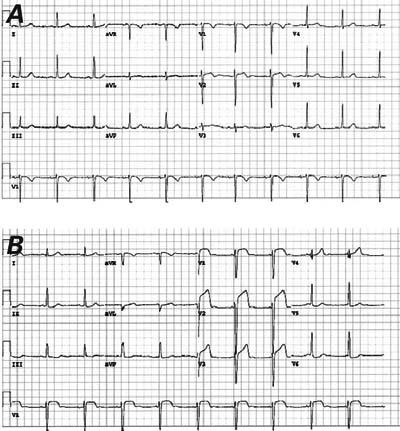
Fig. 1 A) Presenting electrocardiogram during chest pain demonstrates 0.5- to 1-mm ST-segment elevation in leads V1 and V2 with a biphasic T wave in lead V2. B) During recurrent chest pain, up to 8-mm ST elevation is seen in leads V1 through V3, with nonspecific changes in the inferolateral leads. Note the absence of ST elevation in leads V4 through V6.
Results of initial cardiac enzyme tests revealed a troponin I of 29.5 ng/mL (normal, <0.4 ng/mL), creatine kinase (CK) of 272 U/L (normal, 20–150 U/L), and CK-MB isoenzyme fraction of 32.8 ng/mL (normal, <5.0 ng/mL) with a relative index of 12.1 (normal, <2.5). Echocardiography performed in the emergency department showed mild global hypokinesis of the left ventricle, with an ejection fraction of 0.45 and disproportionate septal hypokinesis. There was no evidence of pericardial thickening or effusion. The patient was given oral metoprolol and intravenous heparin and was transferred to the cardiac care unit, where she had a recurrence of her chest pain associated with dramatic anteroseptal ST elevation (Fig. 1B). The chest pain persisted despite sublingual and intravenous nitroglycerin administration, and she was taken urgently to the cardiac catheterization laboratory. She was found to have normal epicardial coronary arteries with minimal luminal irregularities (Fig. 2). The left ventricular end-diastolic pressure was 14 mmHg. Her chest pain resolved spontaneously after cardiac catheterization. The CK and CK-MB levels peaked on the 2nd day of hospitalization at 3,692 U/L and 459 ng/mL, respectively. Cardiac magnetic resonance imaging (MRI) showed hypokinesis of the basal septum and a corresponding large area of mid-myocardial delayed enhancement with sparing of the subendocardial tissue (Fig. 3). By the 4th day of hospitalization, the ST segments had normalized on ECG. The patient was discharged on β-blocker therapy in good condition, without recurrence of pain. Six months later, she remained asymptomatic, and β-blockers were discontinued. She had resumed all normal activities.

Fig. 2 Left coronary angiogram in a right anterior oblique-caudal projection shows no significant coronary artery disease.
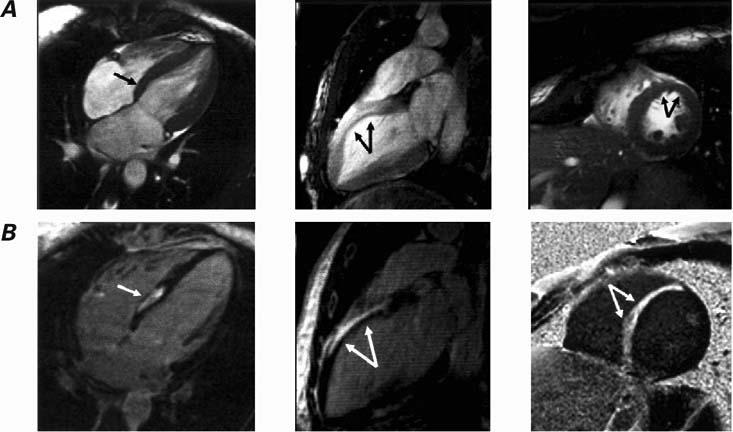
Fig. 3 A) Four-chamber, long-axis and short-axis end-systolic frames from a cine magnetic resonance image (MRI) acquisition show decreased systolic wall thickening in the basal septum and anterior wall (arrows). The long-axis-view cine sequence was obtained several minutes after gadolinium DTPA administration. B) Inversion recovery MRIs in multiple planes obtained 15 minutes after gadolinium DTPA administration show delayed enhancement in the basal septum and anterior wall. Note the “mid-myocardial” position of the area of enhancement, with sparing of the subendocardial region (arrows)—a typical finding in myocarditis.
Discussion
In patients who have chest pain with elevated myocardial enzymes and the absence of coronary artery disease, myocarditis is often the leading diagnosis. In this patient, young age and an apparent preceding viral illness supported a diagnosis of myocarditis; however, the localized dramatic anteroseptal ST-segment elevation raised the possibility of an acute coronary syndrome. Currently, the only widely available method for the definitive diagnosis of myocarditis is endomyocardial biopsy. This technique has limited sensitivity with an estimated range of 43% to 64%, with an overall complication rate of 6% and a 0.4% risk of death due to perforation.3,4 Radiolabeled antimyosin antibody has been used to identify myocarditis; however, this method identifies myocardial necrosis from any cause, including myocardial infarction, and is therefore nonspecific. In 1 report,5 radiolabeled antimyosin antibody scintigraphy was combined with rest thallium imaging to differentiate myocarditis from acute myocardial infarction, with a sensitivity of 67% and specificity of 63%.5 The authors relied on diffuse myocardial uptake or antimyosin uptake that was inconsistent with coronary anatomy and without a matched thallium defect, which is a method that may not always apply to focal myocarditis.
Cardiac MRI can noninvasively detect myocardial edema and myocyte damage. Myocarditis shows a characteristic pattern of contrast enhancement, which originates primarily from the epicardium, sparing the subendocardial layer.6,7 In contrast, myocardial infarction typically shows subendocardial enhancement on MRI.6,7 In a study by Mahrholdt and colleagues,6 MRI was evaluated in the diagnosis of acute myocarditis and compared with endomyocardial biopsy as the gold standard. Those authors showed histopathologic evidence of active myocarditis in more than 90% of biopsy specimens taken from areas of gadolinium DTPA enhancement (19 of 22 patients).6 Biopsies taken from areas without gadolinium enhancement showed active myocarditis in only 1 of 7 patients.6 In addition, serial MRI imaging has shown that myocarditis often begins focally and becomes more diffuse over time.8
The MRI in our patient was classic for myocarditis, with mid-myocardial enhancement of the septum, which spared the subendocardium and corresponded to the ECG changes, and wall-motion abnormality (Fig. 3). The other possible diagnosis in this case was acute coronary spasm causing an acute ST-elevation myocardial infarction. Superimposed coronary artery spasm in addition to acute myocarditis is difficult to exclude; but it was unlikely, considering the localized ECG findings in leads V1 through V3 without extension to the anterolateral precordial leads in a patient with a large territory supplied by the left anterior descending artery. The MRI findings were also inconsistent with myocardial infarction, because the MRI did not demonstrate endomyocardial enhancement—the pattern found in myocardial infarction. Ergonovine stimulation was not performed in the catheterization laboratory, because we did not consider it safe, given the cardiac enzyme evidence of ongoing myocardial necrosis.
In summary, a patient with focal myocarditis may present with chest pain and dramatic localized ST- segment elevation. A history of a preceding viral illness is an important clue to the correct diagnosis. Cardiac MRI is useful in differentiating myocardial ischemia, infarction, or spasm from acute myocarditis.
Footnotes
Address for reprints: Edward P. Gerstenfeld, MD, 9 Founders Pavilion, 3400 Spruce Street, Philadelphia, PA 19104. E-mail: edward.gerstenfeld@uphs.upenn.edu
References
- 1.Dec GW Jr, Waldman H, Southern J, Fallon JT, Hutter AM Jr, Palacios I. Viral myocarditis mimicking acute myocardial infarction. J Am Coll Cardiol 1992;20:85–9. [DOI] [PubMed]
- 2.Miklozek CL, Crumpacker CS, Royal HD, Come PC, Sullivan JL, Abelmann WH. Myocarditis presenting as acute myocardial infarction. Am Heart J 1988;115:768–76. [DOI] [PubMed]
- 3.Chow LH, Radio SJ, Sears TD, McManus BM. Insensitivity of right ventricular endomyocardial biopsy in the diagnosis of myocarditis. J Am Coll Cardiol 1989;14:915–20. [DOI] [PubMed]
- 4.Deckers JW, Hare JM, Baughman KL. Complications of transvenous right ventricular endomyocardial biopsy in adult patients with cardiomyopathy: a seven-year survey of 546 consecutive diagnostic procedures in a tertiary referral center. J Am Coll Cardiol 1992;19:43–7. [DOI] [PubMed]
- 5.Sarda L, Colin P, Boccara F, Daou D, Lebtahi R, Faraggi M, et al. Myocarditis in patients with clinical presentation of myocardial infarction and normal coronary angiograms. J Am Coll Cardiol 2001;37:786–92. [DOI] [PubMed]
- 6.Mahrholdt H, Goedecke C, Wagner A, Meinhardt G, Athanasiadis A, Vogelsberg H, et al. Cardiovascular magnetic resonance assessment of human myocarditis: a comparison to histology and molecular pathology. Circulation 2004; 109:1250–8. [DOI] [PubMed]
- 7.Laissy JP, Messin B, Varenne O, Iung B, Karila-Cohen D, Schouman-Claeys E, Steg PG. MRI of acute myocarditis: a comprehensive approach based on various imaging sequences. Chest 2002;122:1638–48. [DOI] [PubMed]
- 8.Friedrich MG, Strohm O, Schulz-Menger J, Marciniak H, Luft FC, Dietz R. Contrast media-enhanced magnetic resonance imaging visualizes myocardial changes in the course of viral myocarditis. Circulation 1998;97:1802–9. [DOI] [PubMed]


