Abstract
In order to determine the temporal pattern of weaning from mechanical ventilation for patients undergoing prolonged mechanical ventilation after cardiac surgery, we performed a retrospective review of 21 patients' weaning courses at our long-term acute care hospital. Using multiple regression analysis of an estimate of individual patients' percentage of mechanical ventilator support per day (%MVSD), we determined that 14 of 21 patients (67%) showed a statistically significant quadratic or cubic relationship between time and %MVSD. These patients showed little or no improvement in their ventilator dependence until a point in time when, abruptly, they began to make rapid progress (a “wean turning point”), after which they progressed to discontinuation of mechanical ventilation in a relatively short period of time. The other 7 patients appeared to have a similar weaning pattern, although the data were not statistically significant.
Most patients in the study group weaned from the ventilator through a specific temporal pattern that is newly described herein. Data analysis suggested that the mechanism for the development of a wean turning point was improvement of pulmonary mechanics rather than improvement in gas exchange or respiratory load. Although these observations need to be confirmed by a prospective trial, they may have implications for weaning cardiac surgery patients from prolonged mechanical ventilation, and possibly for weaning a broader group of patients who require prolonged mechanical ventilation.
Key words: Cardiac surgical procedures; postoperative care; postoperative complications; prolonged mechanical ventilation; respiration, artificial; retrospective studies; ventilator weaning/methods/statistics & numerical data
Advances in anesthesia and surgical techniques over the past several years have allowed most patients undergoing cardiac surgery to be weaned from mechanical ventilation (MV) within a few hours after surgery.1 By recent estimates, however, approximately 5% of cardiac surgery patients still require postoperative prolonged mechanical ventilation (PMV), of 7 or more days' duration.2–4 The need for PMV support in this group of patients arises from various complications in the perioperative period, often in conjunction with underlying, preoperative conditions.3–8 The mortality rate for such patients currently ranges from 15% to 45%9,10 and contrasts starkly with the generally excellent outcomes of patients after cardiac surgery. Interestingly, survivors of PMV after cardiac surgery are almost always eventually weaned from MV and generally enjoy a good quality of life after discharge from the hospital.2,10
Mechanical ventilation itself, independent of the cause for its use, is associated with a high rate of complications, the most notable of which is ventilator-associated lung injury and pneumonia.11 Therefore, a major focus of MV investigation in recent years has been to develop ways to wean and remove patients from ventilators as rapidly as possible. In fact, a number of highly effective strategies for shortening the duration of MV in patients with acute respiratory failure have been developed,12 which have significantly lowered mortality rates and lessened the complications for these patients.13 However, progress in weaning patients from PMV—whether it is associated with medical or surgical causes—has been lagging, possibly due to the relative lack of study of this specific process and patient population.14 The current, prevailing weaning strategy for the PMV population comes largely from expert, consensus opinion and consists of slow-paced, prolonged weaning, characterized by gradual, stepwise reductions of MV support, often in the setting of a long-term acute care hospital (LTAC) specializing in this process.12
Our experience, however, with cardiac surgery patients who require PMV has suggested that their temporal weaning pattern may be neither one of stepwise decrements nor one of a slow, gradual decline in the need for ventilator support. Rather, we have observed that patients seem to make little initial progress in weaning until a point in time when weaning abruptly becomes rapid, leading to discontinuation of MV in a relatively short period of time. We have found no good description in the literature of the PMV weaning course over time, either for cardiac surgery patients or for other, noncardiac surgery patients. Identifying a temporal pattern of the weaning course may suggest ways to improve the efficacy and efficiency of weaning cardiac surgery patients from PMV and, therefore, improve outcomes and costs in this group.
We conducted a retrospective review of the ventilator courses of a group of patients who required PMV after cardiac surgery. These patients were transferred to an LTAC for weaning and were eventually removed successfully from MV. Specifically, we evaluated the change in level of MV support over time and tried to determine whether there was an identifiable wean turning point after which the weaning progress became rapid.
Patients and Methods
We retrospectively reviewed the hospital courses of consecutive patients admitted to Kindred Hospital Houston from December 1997 through December 2001. (Kindred Hospital Houston is an LTAC that serves as a regional weaning center.) We included patients who had undergone cardiac surgery and required PMV. Study patients were transferred from St. Luke's Episcopal Hospital and the Texas Heart Institute, Houston, Texas (SLEH/THI), a tertiary acute care facility specializing in cardiovascular disease. Patients were excluded from analysis if they had to be transferred back to SLEH/THI, could not be weaned from MV, or died.
Mechanical Ventilation and Weaning Procedures. All patients were ventilated via tracheostomy tube with Puritan Bennett 7200® Mechanical Ventilators (Puritan Bennett, Inc., a Tyco Healthcare company; Pleasanton, Calif). Volume-cycled modes were set to deliver a decelerating ramp flow pattern (the standard method to deliver air flow through a ventilator, consisting of a high flow rate at the outset of the delivered breath and gradually lessened flow over the remainder of the breath), with a peak inspiratory flow rate of 60 L/min (range, 50–100 L/min). The tidal volume was set between 5 and 10 mL/kg of lean body weight and adjusted to keep the peak inspiratory pressure less than 35 cm H2O. The fraction of inspired oxygen (FiO2) was adjusted to the lowest value producing a blood oxygen saturation of at least 92%. Positive pressure breaths from the ventilator were triggered by negative airway pressure with a sensitivity usually set at 2 cm H2O (range, 0.4–2.0 cm H2O).
No specific weaning protocol was applied to these patients. Weaning, however, generally proceeded according to physicians' orders that allowed respiratory therapists to decrease MV support to the lowest level at which patients did not demonstrate fatigue-pattern breathing (respiratory rate, >30 breaths/min; use of accessory muscles; or complaints of respiratory distress). Weaning was stopped when patients developed fatigue, had an oxygen saturation of less than 90%, or developed an uncontrolled major medical complication. Complications included acute change in mental status, exacerbation of chronic obstructive pulmonary disease, nosocomial infections, bronchitis or pneumonia with voluminous secretions, pulmonary embolism, noncardiogenic pulmonary edema, renal failure, exacerbation of congestive heart failure, hemodynamically significant arrhythmias, unstable angina, profound electrolyte disturbances, sepsis, acute gastrointestinal bleeding, or severe anemia (hematocrit, <25%). Weaning was initiated during the day, and patients generally rested at night on higher levels of MV support until they were judged ready to be completely off the ventilator. During the weaning course, all patients received physical therapy 1 or 2 times per day and bedside pulmonary rehabilitation.
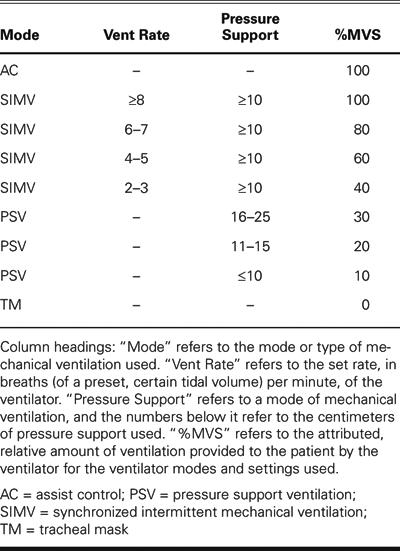
Study Design. The weaning course of the study population was analyzed by assigning a percentage of MV support (%MVS) per day (%MVSD) to each patient's hospital stay in the LTAC until the patient was completely weaned from the ventilator. The components of %MVS are described in Table I. The %MVSD was derived using the following formula: %MVSD = [Number of hours at a particular level of MV support during the day × Percentage of MV support (%MVS) over that time]/24 hours. For example, a patient might spend 8 hours at night on the assist control mode (AC) of ventilation at a respiratory rate of 10 breaths/min (in other words, the ventilator breathes almost completely for the patient). Then the patient has a morning pressure support ventilation (PSV) trial of 10 cm H2O for 6 hours. (PSV is a mode of ventilation whereby the patient initiates breaths, but receives more or less pressure support from the ventilator. At a support level of 10 cm H2O, the patient usually does most of the work of breathing.) This period is followed by a tracheal mask trial for 6 hours (during this trial, the patient is removed from the ventilator and given only humidified air, to allow the patient to breathe completely on his or her own). The patient is then placed on synchronized intermittent mandatory ventilation (SIMV) with a respiratory rate of 4 breaths/min and a PSV of 10 cm H2O for the remainder of the day (4 hours). (SIMV with PSV is a mixed mode of MV whereby the patient receives some mandatory breaths but also can breathe on his or her own, with some PSV between those mandatory breaths.) In this case, then, the %MVSD would be [(8 hours × 100 %MVS) + (6 hours × 10 %MVS) + (6 hours × 0 %MVS) + (4 hours × 60 %MVS)]/24 hours = 46%.
Table I. Percentage of Mechanical Ventilator Support (%MVS)
For each patient, the %MVSD was analyzed over time, measured in days. In addition, dynamic lung compliance (Cp) was calculated each day as a rough measure of respiratory load. (Cp was defined as tidal volume/[peak inspiratory pressure – positive end expiratory pressure] and inversely related to the difficulty of inflating the lung; that is, the lower the Cp, the easier it is and the less work it takes to inflate the lung.) The mean daily FiO2 was used as a rough marker of gas exchange. The relationship of these data to the daily %MVD for each patient was also analyzed.
Statistical Analysis. The relationship between %MVSD and time was analyzed for each patient individually by multiple regression analysis, using the patient's LTAC day number (total number of days spent at the LTAC to that point) as the predictor of %MVSD. In a separate analysis, the value of %MVSD was raised to the 1st, 2nd, and 3rd powers to determine whether the relationship was linear, quadratic (in geometric terms, curvilinear), or cubic (geometrically, curvilinear with 2 curves or bicurvilinear). Two-tailed Pearson correlations between FiO2 and %MVSD, and between Cp and %MVSD, were calculated to determine whether there were relationships between crude measures of gas exchange or respiratory load and the weaning process. P values of less than 0.05 were considered to be statistically significant. The statistical program package was SPSS version 10 (SPSS Inc.; Chicago, Ill).
Results
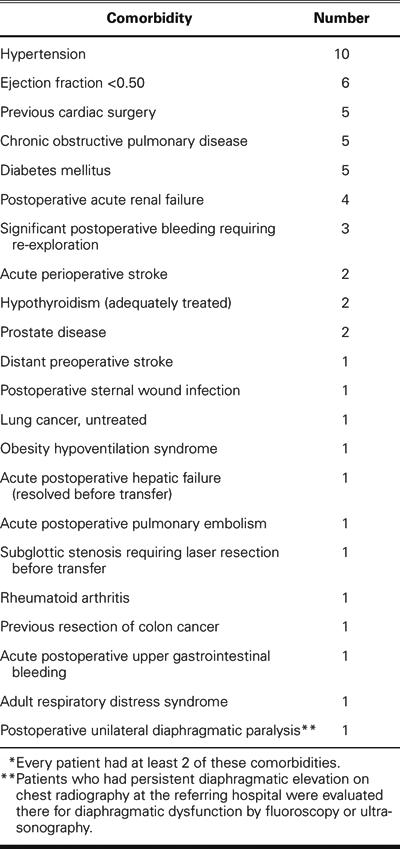
During the study period, a total of 33 consecutive patients who required PMV after cardiac surgery were transferred to Kindred Hospital Houston from SLEH/THI. Four patients, still on MV, were transferred back to SLEH/THI for complications requiring medical-center-level care (two for tracheal stenosis, one for an acute alteration in mental status, and one for sternal wound infection). One patient on MV was transferred to an LTAC that was closer to the patient's home. Seven patients died of complications at Kindred Hospital. The remaining 21 patients met our inclusion criteria, and their data were analyzed. Fifteen of these patients were weaned from MV and discharged home, and six were transferred to a rehabilitation hospital or a skilled nursing facility after weaning. There were 12 men and 9 women (age range, 40–89 years; mean, 71 ± 13 years;). Fourteen patients had undergone coronary artery bypass grafting (CABG); 2 patients, aortic valve replacement (AVR); 2 patients, mitral valve replacement (MVR); 2 patients, CABG and AVR; and 1 patient, CABG and MVR. The mean time on MV before LTAC admission was 35 ± 14 days (range, 9–61 days). The most frequently seen comorbidities were hypertension (10); ejection fraction of less than 0.50 (6); prior cardiac surgery (5); chronic obstructive pulmonary disease (5); and diabetes mellitus (5). All comorbidities are presented in Table II. Every patient had at least 2 comorbidities.
Table II. Comorbidities in 21 Patients on Prolonged Mechanical Ventilation*
The mean %MVSD upon admission was 86.5% ± 21.3% (range, 30%–100%) with 13 of 21 (62%) having a %MVSD of 100%. The mean Cp was 0.026 ± 0.011 L/cm H2O (range, 0.01–0.051 L/cm H2O), and the mean FiO2 was 0.37 ± 0.07 (range, 0.30–0.60). The mean time to discontinuation of MV was 24.0 ± 16.4 days (range, 5–77 days).
We determined that 14 of 21 patients (67%) showed a statistically significant quadratic or cubic relationship between time and %MVSD. Of these, 12 patients demonstrated a significant negative quadratic relationship between time and %MVSD (a curvilinear relationship with a period of downward bend). (See Figure 1.) The initial %MVSD of these 12 patients was 81.6% ± 24.1%. They made little initial progress in weaning from the ventilator. In fact, their %MVSDs increased over the 1st few days of their hospital course. However, on day 12.4 ± 6.9, the %MVSD of 92.2% ± 8.8% began to decrease dramatically. The patients weaned rapidly for 3.1 ± 2.2 days, and their %MVSDs dropped 65.1% ± 16.8% before the weaning progress slowed. They were eventually liberated from mechanical ventilation 10.4 ± 5.6 days after the wean turning point (WTP). The other 2 patients (of this group of 14) showed only a significant negative cubic relationship between time and %MVSD (a curvilinear relationship with 2 downward curves [bicurvilinear] and a plateau between the 2 curves). The temporal wean curve for one of these patients is shown in Figure 2. Their initial ventilator courses were linear, followed by a WTP, but the %MVSD decline did not continue until the discontinuation of mechanical ventilation. Instead, the weaning progress stabilized for several days at a lower level of %MVSD, before dropping again linearly to the point of ventilator liberation. Four patients (in this same group of 14) demonstrated both a significant negative quadratic relationship and a significant negative cubic relationship between time and %MVSD.
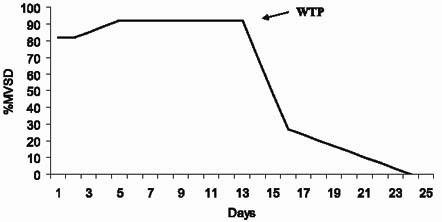
Fig. 1 Data from 12 of our 21 patients revealed a significant quadratic—that is, curvilinear—relationship between time and the percentage of mechanical ventilation support per day (%MVSD). Their ventilator courses were initially linear, until a point in time—the wean turning point (WTP)—when the %MVSD curve turned sharply downward, representing a period of rapid weaning that ended in liberation from MV.
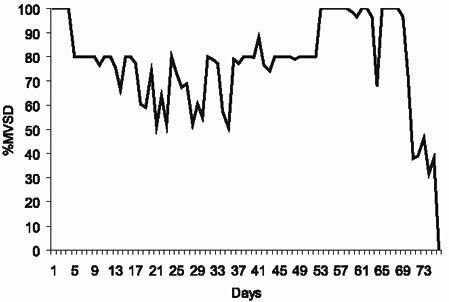
Fig. 2 The wean curve of a patient whose relationship between time and the percentage of mechanical ventilation support per day (%MVSD) conformed significantly only to a negative cubic regression, or curvilinear with 2 curves. This patient experienced a wean turning point (WTP) on day 64 of the hospital course, followed by a relatively brief weaning plateau (5 days) before a 2nd rapid weaning phase led to the discontinuation of mechanical ventilation.
The other 7 patients (33%) who weaned from PMV had data that displayed a negative linear relationship between time and %MVSD (as time advanced, the %MVSD declined linearly). In all of these patients, we also found a quadratic, curvilinear relationship, but analysis of the data points for these curves showed P values greater than 0.05. Figure 3 shows the curve of 1 such patient. In summary, in 14 of 21 patients (67%) who weaned from the ventilator, therefore, we found a statistically significant negative curvilinear or bicurvilinear relationship between time and %MVSD—in other words, a WTP. The curves of the other 7 patients who weaned followed this pattern, but those data were not strong enough to produce a statistically significant WTP.
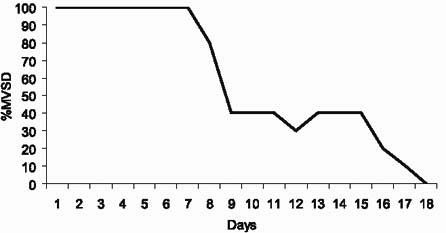
Fig. 3 The wean curve of a patient shows a significant linear relationship between time and the percentage of mechanical ventilation support per day (%MVSD). Although the data also demonstrated a quadratic (curvilinear) relationship between time and %MVSD—a wean turning point (WTP) at day 8 of the hospital course—the relationship did not reach statistical significance.
For the 12 patients with a statistically significant quadratic pattern of weaning, the mean time to the WTP was 12.4 ± 6.9 days, and the mean %MVSD at the WTP was 92.2% ± 8.8% (range, 79%–100%). Of note, there were 4 patients whose %MVSD was less than 80% upon admission; all of these patients had an increase in %MVSD by the time of their WTP. Their time from the WTP to discontinuation of mechanical ventilation was 10.4 ± 5.6 days (range, 1–23 days), and most of the ventilator weaning occurred during the period immediately after the WTP, when a mean drop in the %MVSD of 65.1% ± 16.8% was accomplished in just 3.1 ± 2.2 days.
For the 2 patients whose wean curves conformed only to a cubic relationship, the onset of the WTP was very different. One patient's WTP occurred at day 1, but the weaning plateau was relatively long (12 days) before the 2nd rapid weaning phase of the wean curve. The other patient's WTP occurred much later, on day 64, but the weaning plateau was relatively brief (5 days) before the 2nd rapid weaning phase began (Fig. 2).
It is noteworthy that 6 patients (29%) had an initial drop of at least 30% in %MVSD that was not sustained. These %MVSDs increased to at least their initial level before the patients were weaned sufficiently to discontinue mechanical ventilation.
Only 5 patients (24%) had a significant positive correlation between FiO2 and %MVSD (as the FiO2 went down, so did the %MVSD). Six patients (29%) had a significant negative correlation between Cp and %MVSD (as Cp went up, %MVSD went down). The interval between the onset of the last medical complication and the WTP was 17.1 ± 11.5 days (range, 5–42 days), but there was no obvious relationship between the timing of the WTP and the last medical complication.
Discussion
In most of our patients who required PMV after cardiac surgery, weaning from the ventilator took place over time by a specific pattern that is newly described herein. The weaning course of our patients was not a slow, linear, or stepwise decrement of mechanical ventilator support, as is commonly assumed of PMV patients. Rather, weaning of these patients had a pattern of limited initial progress until a point in time—the WTP—when weaning became rapid and resulted in liberation from mechanical ventilation within a few days. This pattern was evident regardless of the duration of mechanical ventilation, or from what level of ventilator support the weaning had begun.
There are several major methodological problems inherent in the design of this retrospective, observational study. The pre-eminent one is the lack of a strict weaning protocol. In our study, respiratory therapists had strict protocols, generally agreed upon in the literature, for when to terminate the wean out of concern for the patient's safety or to avoid ventilatory muscle fatigue.15,16 However, the timing of the initiation of weaning was left to the judgment of the therapists and physicians. Such practice has been found in the acute care setting, at least under some circumstances, to unnecessarily delay the onset of weaning and add length to the MV course.17,18 Thus, it may be that our patients were not aggressively weaned until well after they were ready, and the rapid weaning progress after the WTP might have been because the patients were no longer held back from weaning. Therefore, the weaning pattern observed in our study, including the WTP, might have been the result of our weaning practice pattern rather than actual patient improvement over time. Even if this is true, however, the observation of a WTP is still important, because it is generally held that patients treated with PMV require a strategy of gradual MV withdrawal.12 Moreover, there are concerns, arising from some basic studies, that a high level of ventilator support for prolonged periods can, by itself, produce substantial diaphragmatic dysfunction, which may necessitate gradual MV withdrawal to allow muscle function recovery.19–22 However, our data suggest that even if patients are on a high level of MV for a prolonged time, they can still wean rapidly. This would be consistent with recent data from animal models indicating that PMV, depending upon how it is delivered, does not necessarily “addict” the patient to the ventilator and require gradual withdrawal.23
It is also worth pointing out that 29% of the study population made substantial weaning progress early in their course (%MVSD decreased by at least 30%) but were unable to sustain their gains. They eventually needed as much, or more, ventilator support than they were on when they arrived at the LTAC. (Figure 2 is a good example of this.) These patients, at least, were very likely held back from weaning, not by the physicians' or therapists' preferences, but by true inability to wean. Certainly, these patients did not make slow, linear weaning progress. Nevertheless, we cannot be certain whether our patients' weaning patterns accurately reflected the course of their ventilator dependence and the temporal pattern of improvement. So however provocative these data are, a prospective study of temporal weaning patterns, using a strict weaning protocol such as one recently published for PMV,17 will be needed to answer this question.
A 2nd major methodological problem of the study is our use of the novel “%MVSD” as a measure of relative ventilator support. Current commercially available ventilators cannot accurately measure the ratio of machine-to-patient contribution with regard to the work of breathing.24,25 Therefore, for the purpose of analyzing our patients' ventilator use over time in a retrospective fashion, we created an arbitrary and admittedly crude method of estimating ventilatory support using ventilator settings, that is, the %MVS. In reality, the %MVS is a scale of ventilator settings from lower to higher, and our study is one of how the settings changed over time, as estimated by the %MVSD. We presumed that the settings accurately indicated the amount of, or need for, ventilator support. Nonetheless, when used consistently within individual patients' data sets, this metric should at least be sufficiently accurate to show how the ventilator settings changed over time, and hence be a helpful tool for tracking ventilator use and weaning. More specifically, the %MVSD was designed to help us to determine whether our patients' ventilator use over time could be accurately described by linear, quadratic, or cubic regression equations. To put it in geometric terms, each patient's %MVSD was plotted over time to see if the graph fit a linear, curvilinear, or bicurvilinear pattern. This enabled us to test the hypothesis that a WTP occurred: that the wean curve “turned the corner” in a statistically significant way and thereafter progressed more rapidly.
A 3rd notable methodological problem with our study is that of accounting for the effect of medical complications on the weaning course, which has received relatively little attention.26 The ways in which different complications affect respiratory load, pulmonary mechanics, or both, have not been clearly determined—at least not in the PMV population. Hence, there is no scoring system for the impact of complications on weaning. Our only analysis of the impact of complications involved those that are known to affect weaning. We looked for a temporal association between complications and each individual's WTP. None was obvious. Future studies are needed to evaluate this issue more carefully, focusing upon the impact of complications on respiratory load and ventilatory performance.
Interpreting our results was complicated by the fact that our patients were often ventilated with a greater level of support at night than during the day. Typically, during the day, patients were weaned to the lowest %MVS for the longest period of time tolerated. However, the level of support was often increased at night to guard against the development of respiratory muscle fatigue from the increased work of breathing during periods when patients were not monitored as closely, and to avoid, as much as possible, disrupted sleep.27 These variations in support may account, at least in part, for our observation that some of the patients (29% of the study group) weaned rapidly after the WTP but then demonstrated a slowing, or a plateau, of the weaning process before eventual discontinuation of MV. However, the practice of increasing nocturnal support should not have altered the initial curvilinear decline in ventilator support, meaning the occurrence of a WTP, in this group.
Perhaps one of the more salient observations of our study, if we assume that our patients weaned as rapidly as they could have, was the lack of a consistent relationship between weaning progress (as determined by the %MVSD) and measures of respiratory load or gas exchange. This suggests that the mechanism of weaning progress in our patients was an improvement either of ventilatory function, or of the performance characteristics of the chest wall or ventilatory muscles. Why pulmonary mechanics would abruptly improve, if indeed they did so, is unclear. One explanation might be the resolution of phrenic neuropathy associated with open-heart surgery.28 However, only 1 patient in the group was shown, with use of standard clinical tools, to have diaphragmatic dysfunction. Yet it is possible that other patients had subclinical alteration of diaphragmatic function, which can be subtle and require sophisticated electrophysiologic studies to detect. Ultimately, we think it unlikely that the entire group suffered from diaphragmatic palsy. Cardiac surgery is well documented, however, to cause decreased pulmonary function (as measured by spirometry) and impaired pulmonary mechanics—even in the absence of diaphragmatic dysfunction—for up to several months after surgery.29–31 The precise mechanism for these sequelae has not been delineated; but we believe that, in our patients, the eventual resolution of these impairments may have allowed the rapid weaning period observed. Other possible explanations of ventilatory improvement include resolution of neuropathy or myopathy associated with critical illness, achievement of adequate protein repletion, muscle reconditioning or adaptation, or other factors of MV weaning failure as yet not identified in the literature.
The possible implication of our results is that patients who require PMV after cardiac surgery, and potentially noncardiac PMV patients, may be capable of rapidly weaning from MV at some point in their course, regardless of the duration or level of MV support they have required. If that point could be identified with accuracy, by trials of spontaneous breathing or other means, PMV courses could conceivably be shortened by an appropriately aggressive weaning strategy from that point in time. Furthermore, if it can be established that a WTP occurs in post-cardiac surgery patients or in other PMV populations, investigation into the mechanism of its development may yield ways to hasten its occurrence. Earlier weaning from PMV may ultimately lead to improved outcomes in post-cardiac surgery patients, who historically have a poorer prognosis than do other surgical patients.
Conclusions
We showed that a group of patients who required prolonged mechanical ventilation after cardiac surgery weaned from the ventilator through a specific and newly described temporal pattern. These patients showed little weaning progress until a wean turning point when, abruptly, they began to make rapid progress leading to liberation from mechanical ventilation in a relatively short period of time. Furthermore, our data suggest that the mechanism for development of the wean turning point was the improvement of pulmonary mechanics rather than improvements in gas exchange or respiratory load. These observations pose questions, the further study of which may have practical implications for weaning post-cardiac patients, and possibly for a broader group of patients, who require prolonged mechanical ventilation.
Footnotes
Address for reprints: James P. Herlihy, MD, 6624 Fannin St., Suite 1730, Houston, TX 77030. E-mail: jph@houstonlungdocs.com
References
- 1.Liu LL, Gropper MA. Respiratory and hemodynamic management after cardiac surgery. Curr Treat Options Cardiovasc Med 2002;4:161–9. [DOI] [PubMed]
- 2.Pappalardo F, Franco A, Landoni G, Cardano P, Zangrillo A, Alfieri O. Long-term outcome and quality of life of patients requiring prolonged mechanical ventilation after cardiac surgery. Eur J Cardiothorac Surg 2004;25:548–52. [DOI] [PubMed]
- 3.Yende S, Wunderink R. Causes of prolonged mechanical ventilation after coronary artery bypass surgery. Chest 2002; 122:245–52. [DOI] [PubMed]
- 4.Kern H, Redlich U, Hotz H, von Heymann C, Grosse J, Konertz W, Kox WJ. Risk factors for prolonged ventilation after cardiac surgery using APACHE II, SAPS II, and TISS: comparison of three different models. Intensive Care Med 2001;27:407–15. [DOI] [PubMed]
- 5.Hammermeister KE, Burchfiel C, Johnson R, Grover FL. Identification of patients at greatest risk for developing major complications at cardiac surgery [published erratum appears in Circulation 1991;84:446]. Circulation 1990;82 (5 Suppl):IV380–9. [PubMed]
- 6.Kollef MH, Wragge T, Pasque C. Determinants of mortality and multiorgan dysfunction in cardiac surgery patients requiring prolonged mechanical ventilation. Chest 1995;107:1395–401. [DOI] [PubMed]
- 7.Thompson MJ, Elton RA, Mankad PA, Campanella C, Walker WS, Sang CT, Cameron EW. Prediction of requirement for, and outcome of, prolonged mechanical ventilation following cardiac surgery. Cardiovasc Surg 1997;5:37681. [DOI] [PubMed]
- 8.Dunning J, Au J, Kalkat M, Levine A. A validated rule for predicting patients who require prolonged ventilation post cardiac surgery. Eur J Cardiothorac Surg 2003;24:270–6. [DOI] [PubMed]
- 9.LoCicero J 3rd, McCann B, Massad M, Joob AW. Prolonged ventilatory support after open-heart surgery. Crit Care Med 1992;20:990–2. [DOI] [PubMed]
- 10.Engoren M, Buderer NF, Zacharias A. Long-term survival and health status after prolonged mechanical ventilation after cardiac surgery. Crit Care Med 2000;28:2742–9. [DOI] [PubMed]
- 11.MacIntyre NR. Evidence-based ventilator weaning and discontinuation. Respir Care 2004;49:830–6. [PubMed]
- 12.MacIntyre NR, Cook DJ, Ely EW Jr, Epstein SK, Fink JB, Heffner JE, et al. Evidence-based guidelines for weaning and discontinuing ventilatory support: a collective task force facilitated by the American College of Chest Physicians; the American Association of Respiratory Care; and the American College of Critical Care Medicine. Chest 2001;120(6 Suppl):375S-95S. [DOI] [PubMed]
- 13.Burns SM, Earven S, Fisher C, Lewis R, Merrell P, Schubart JR, et al. Implementation of an institutional program to improve clinical and financial outcomes of mechanically ventilated patients: one-year outcomes and lessons learned. Crit Care Med 2003;31:2752–63. [DOI] [PubMed]
- 14.Scheinhorn DJ, Chao DC, Stearn-Hassenpflug M. Liberation from prolonged mechanical ventilation. Crit Care Clin 2002;18:569–95. [DOI] [PubMed]
- 15.Hess D. Ventilator modes used in weaning. Chest 2001;120 (6 Suppl):474S-6S. [DOI] [PubMed]
- 16.Esteban A, Alia I, Tobin MJ, Gil A, Gordo F, Vallverdu I, et al. Effect of spontaneous breathing trial duration on outcome of attempts to discontinue mechanical ventilation. Spanish Lung Failure Collaborative Group. Am J Respir Crit Care Med 1999;159:512–8. [DOI] [PubMed]
- 17.Scheinhorn DJ, Chao DC, Stearn-Hassenpflug M, Wallace WA. Outcomes in post-ICU mechanical ventilation: a therapist-implemented weaning protocol. Chest 2001;119:236–42. [DOI] [PubMed]
- 18.Vitacca M, Vianello A, Colombo D, Clini E, Porta R, Bianchi L, et al. Comparison of two methods for weaning patients with chronic obstructive pulmonary disease requiring mechanical ventilation for more than 15 days. Am J Respir Crit Care Med 2001;164:225–30. [DOI] [PubMed]
- 19.Sassoon CS. Ventilator-associated diaphragmatic dysfunction. Am J Respir Crit Care Med 2002;166:1017–8. [DOI] [PubMed]
- 20.Yang L, Luo J, Bourdon J, Lin MC, Gottfried SB, Petrof BJ. Controlled mechanical ventilation leads to remodeling of the rat diaphragm. Am J Respir Crit Care Med 2002;166:1135–40. [DOI] [PubMed]
- 21.Sassoon CS, Caiozzo VJ, Manka A, Sieck GC. Altered diaphragm contractile properties with controlled mechanical ventilation. J Appl Physiol 2002;92:2585–95. [DOI] [PubMed]
- 22.Anzueto A, Peters JI, Tobin MJ, de los Santos R, Seidenfeld JJ, Moore G, et al. Effects of prolonged controlled mechanical ventilation on diaphragmatic function in healthy adult baboons. Crit Care Med 1997;25:1187–90. [DOI] [PubMed]
- 23.Sassoon CS, Zhu E, Caiozzo VJ. Assist-control mechanical ventilation attenuates ventilator-induced diaphragmatic dysfunction. Am J Respir Crit Care Med 2004;170:626–32. [DOI] [PubMed]
- 24.Marini JJ, Smith TC, Lamb VJ. External work output and force generation during synchronized intermittent mechanical ventilation. Effect of machine assistance on breathing effort. Am Rev Respir Dis 1988;138:1169–79. [DOI] [PubMed]
- 25.Weavind L, Shaw AD, Feeley TW. Monitoring ventilator weaning—predictors of success. J Clin Monitor Comput 2000;16:409–16. [DOI] [PubMed]
- 26.Mancebo J. Weaning from artificial ventilation. Monaldi Arch Chest Dis 1998;53:350–4. [PubMed]
- 27.Parthasarathy S, Tobin MJ. Effect of ventilator mode on sleep quality in critically ill patients. Am J Respir Crit Care Med 2002;166:1423–9. [DOI] [PubMed]
- 28.DeVita MA, Robinson LR, Rehder J, Hattler B, Cohen C. Incidence and natural history of phrenic neuropathy occurring during open heart surgery. Chest 1993;103:850–6. [DOI] [PubMed]
- 29.Ragnarsdottir M, KristjAnsdottir A, Ingvarsdottir I, Hannesson P, Torfason B, Cahalin L. Short-term changes in pulmonary function and respiratory movements after cardiac surgery via median sternotomy. Scand Cardiovasc J 2004; 38:46–52. [DOI] [PubMed]
- 30.Nicholson DJ, Kowalski SE, Hamilton GA, Meyers MP, Serrette C, Duke PC. Postoperative pulmonary function in coronary artery bypass graft surgery patients undergoing early tracheal extubation: a comparison between short-term mechanical ventilation and early extubation. J Cardiothorac Vasc Anesth 2002;16:27–31. [DOI] [PubMed]
- 31.Locke TJ, Griffiths TL, Mould H, Gibson GJ. Rib cage mechanics after median sternotomy. Thorax 1990;45:465–8. [DOI] [PMC free article] [PubMed]


