Abstract
Absorption, pharmacokinetics, distribution, metabolism, and excretion of [14C]ribavirin were studied in rats (30 mg/kg of body weight) and cynomolgus monkeys (10 mg/kg) after intravenous (i.v.) and oral administration. The oral absorption and bioavailability were 83 and 59%, respectively, in rats and 87 and 55%, respectively, in monkeys. After i.v. administration, the elimination half-life (t[1/2]) was 9.9 h in rats and 130 h in monkeys and the total body clearance was 2,600 ml/h/kg in rats and 224 ml/h/kg in monkeys. The apparent volume of distribution was 11.4 liter/kg in rats and 29.4 liter/kg in monkeys. There was extensive distribution of drug-derived radioactivity into red blood cells and extensive metabolism of ribavirin in rats and a lesser degree of metabolism in monkeys. Excretion of total radioactivity in urine from rats accounted for 84% of the i.v. dose and 83% of the oral dose, whereas that from monkeys accounted for 47% of the i.v. dose and 67% of the oral dose. Several metabolites were observed in plasma and urine from both species. The amount of unchanged ribavirin in urine from both species was quite small after either i.v. or oral administration.
Ribavirin (1-β-d-ribofuranosyl-1,2,4-triazole-3-carboxamide)is a purine nucleoside analog with broad-spectrum activity against a variety of DNA and RNA viral infections (6, 8). In combination with alpha interferon (IFN-α), the clinical efficacy of this drug in the treatment of chronic hepatitis C virus infection has been shown by many studies. The in vivo activity of ribavirin can be ascribed to at least two distinct groups of activities, namely, direct and indirect antiviral effects (13). The direct antiviral effect of ribavirin is attributed to its intracellular metabolites, including the mono-, di-, and triphosphorylated forms of ribavirin (7). Ribavirin may also elicit indirect antiviral effects by promoting T-cell-mediated immunity or by affecting the intracellular GTP concentration through inhibition of the host enzyme IMP dehydrogenase (IMPDH), thereby depleting the intracellular GTP pool available for viral replication (9-12).
Red blood cell and plasma levels of radioactivity and recovery of urinary radioactivity after intravenous (i.v.) and intramuscular (i.m.) dosing of [14C]ribavirin have been studied in rats (1, 2). A similar study was also conducted with rhesus monkeys after i.v. dosing of [14C]ribavirin (2). However, no oral dosing studies based on [14C]ribavirin have been conducted. Miller et al. (4) reported the distribution of radioactivity and composition of metabolites in serum, urine, and various tissues in rats after i.v. and oral dosing of [3H]ribavirin. However, concentrations of ribavirin were not determined in these studies and no pharmacokinetic parameters were reported. Thus, the absorption and bioavailability and various pharmacokinetic parameters of ribavirin after oral administration have not been evaluated in animal studies.
The objectives of this study were to determine the absorption, bioavailability, pharmacokinetics, distribution, metabolism, and excretion of ribavirin in rats and monkeys.
MATERIALS AND METHODS
Compound.
The compound, [5-14C]ribavirin, was synthesized using [14C]butyrate as the precursor. The labeled nucleoside was extensively purified by column chromatography and repetitive recrystallization. The chemical identity and purity were verified by mass spectrometry and proton magnetic resonance spectrometry. The radiopurity (>98%) was confirmed by high-performance liquid chromatography (HPLC), coupled with radioflow detection.
Drug administration and sample collection in rats.
After overnight fasting, six male Sprague-Dawley rats received an i.v. dose of 30 mg of [14C]ribavirin/kg of body weight through a tail vein by a percutaneous catheter and six rats received an oral dose of 30 mg/kg (75 μCi per rat) via oral gavage. Serial blood samples from three rats in each dosing route were collected directly into heparinized Vacutainer tubes and immediately centrifuged to separate plasma and red blood cells (RBC). In a separate study, urine and fecal samples from three rats in each dosing route were also collected in metabolic cages for analysis.
Drug administration and sample collection in cynomolgus monkeys.
After overnight fasting, four cynomolgus monkeys received an i.v. dose bolus (10 mg/kg) through a temporary percutaneous catheter in a saphenous vein or an oral dose of 10 mg of [14C]ribavirin/kg (0.5 mCi per monkey) via oral gavage with a 2-week washout period. Serial blood samples were collected directly in heparinized Vacutainer tubes and immediately centrifuged to separate plasma and RBC. Urine and fecal samples were also collected from each monkey for analysis.
Measurement of radioactivity.
The radioactivity in plasma (0.5 ml) and urine (0.2 ml) was measured directly using an Ultima Gold XR scintillation cocktail and a liquid scintillation counter (model 1900TR; Packard Instrument Company, Meriden, Conn.). Feces and RBC were combusted in a sample oxidizer (model 306; Packard Instrument Company), and the resulting [14C]CO2 was trapped in a mixture of Perma Fluor E+ and Carbo-Sorb followed by liquid scintillation counting. Using an external standard and an instrument-stored quench curve generated from a series of sealed quenched standards, scintillation count data were automatically corrected for counting efficiency.
Liquid chromatography-tandem mass spectrometry method for the determination of ribavirin in plasma.
The method involved the addition of an internal standard (acyclovir), protein precipitation with acetonitrile, solvent evaporation, reconstitution of residue, and an Inertsil silica column separation, followed by tandem mass spectrometry detection. Using positive electrospray ionization, a Perkin-Elmer Sciex API 3000 apparatus (Applied Biosystems, Foster City, Calif.) in the multiple-reaction monitoring mode was used to monitor the 245-to-113 and 259-to-128 transitions for ribavirin and the internal standard. The limit of quantitation was 10 ng/ml, with a relative standard deviation (SD) of <3% and a deviation of mean from the theoretical of <4%. Linear regression of the concentration data (range, 10 to 5,000 ng/ml) yielded a correlation coefficient of >0.999. The overall precision was <3, <4, and <6% relative SD (n = 8) for the 30-, 1,500-, and 3,500-ng/ml QC samples, respectively. The accuracy, expressed as deviation of mean from the theoretical, was not more than 9% for the intraday and interday means.
HPLC procedure for studying the metabolic profiles of ribavirin in plasma, urine, and RBC.
Plasma, urine, or RBC were mixed with an equal volume of acetonitrile. The mixtures were centrifuged, and the supernatant was injected into the HPLC apparatus coupled with a radioactivity detector (β-Ram model 2; IN/US Systems, Inc., Tampa, Fla.). The HPLC apparatus (model SCL 10VP; Shimadzu, Columbia, Md.) was equipped with a 4.6-mm by 110-cm Amide-80 column (TSK; Tosohaas, Montgomeryville, Pa.). The column was eluted with a solvent mixture, consisting of 95% organic mobile phase (acetonitrile) and 10% aqueous phase (25 mM ammonium acetate), and adjusted to a flow rate of 1.2 ml/min. Immediately after the injection, the solvent mixture was switched to 70% organic phase and 30% aqueous phase.
Pharmacokinetic analysis.
Using noncompartmental methods (Win Nonlin-2; Pharsight Corp., Mountain View, Calif.), concentrations of radioactivity and ribavirin in plasma and RBC were used to determine the pharmacokinetic parameters. The maximum concentration of the drug in serum (Cmax) and the time to maximum concentration of the drug in serum (Tmax) were observed values. The area under the concentration-time curve (AUC) to the last quantifiable sampling time (tf) [AUC (tf)] was computed using the linear trapezoidal rule. The AUC to infinity, AUC (I), was calculated as the sum of AUC (tf) and the quotient of the last measurable concentration (Ctf) and the elimination rate constant (K). The K was estimated as the negative slope of the regression of the log concentration versus time. Half-life (t[1/2]) was calculated by dividing the constant 0.693 by K. The apparent total body clearance (CL) was calculated as the ratio of the dose to AUC (I). The volume of distribution (V) was calculated as the ratio of total CL to K.
RESULTS
Concentrations of ribavirin in rat plasma.
After intravenous administration (30 mg/kg of body weight), the disposition kinetics of ribavirin were biphasic with an elimination t[1/2] of 9.9 h. The mean V was 11.4 liter/kg, and the mean CL of ribavirin was 2,600 ml/h/kg. After oral administration (30 mg/kg), ribavirin was rapidly absorbed, with a Tmax of 1 h and a Cmax of 0.433 μg/ml. The elimination t[1/2] was 8.1 h, which is similar to that obtained after intravenous dosing. By comparing the AUC (I) obtained after oral dosing to that obtained after intravenous dosing, the absolute bioavailability was calculated to be 27.1% (Table 1).
TABLE 1.
Mean (SD) pharmacokinetic parameters of ribavirin in rats and monleys after i.v. and oral administration of [14C]ribavirin
| Analyte (parameter) | Unit | Rat (n = 3)
|
Monkey (n = 4)
|
||
|---|---|---|---|---|---|
| i.v. | Oral | i.v. | Orala | ||
| Plasma ribavirin | |||||
| Cmax | μg/ml | 20.5 (3.5) | 0.433 (0.093) | 12.5 (2.5) | 0.29 |
| Tmax | h | 0 | 1 | 0 | 1.5 |
| AUC (I) | μg × h/ml | 11.2 (0.4) | 3.04 (0.49) | 45.5 (6.3) | 13.10 |
| AUC (tf) | μg × h/ml | 11.0 (0.4) | 2.48 (161) | 33.1 (5.5) | 7.92 |
| Bioavailability | % | NAb | 27.1 | NA | 28.2 |
| t1/2 | h | 9.9 (2.9) | 8.1 (5.1) | 130 (7) | 18.8 |
| CI | ml/h/kg | 2,600 (118) | 10,200 (1,670) | 224 (27) | 80.3 |
| V | liter/kg | 11.4 (3.43) | NCc | 29.4 (3.97) | NC |
| Plasma radioactivity | |||||
| Cmax | μg/ml | 22.6 (1.4) | 4.86 (1.51) | 14.8 (1.9) | 2.96 |
| Tmax | h | 0.0833 | 2 | 0.083 | 6 |
| AUC (tf) | μg × h/ml | 39.3 (3.1) | 31.9 (5.1) | 47.7 (10.5) | 43.5 |
| t1/2 | h | 0.4 | NC | 114 (24.1) | 64.4 |
| Absorption | % | NA | 81.2 | NA | 91.2 |
| Plasma ribavirin/plasma radioactivity | |||||
| Cmax | None | 0.91 | 0.09 | 0.84 | 0.10 |
| AUC (tf) | None | 0.28 | 0.08 | 0.69 | 0.18 |
| RBC radioactivity | |||||
| Cmax | μg/ml | 22.5 (1.8) | 4.90 (0.90) | 41.8 (5.2) | 10.5 |
| Tmax | h | 0 | 2 | 36 | 24 |
| AUC (tf) | μg × h/ml | 115 (17) | 60.4 (16.7) | 5,880 (792) | 1,450 |
| t1/2 | h | 14.8 (1.1) | NC | NC | NC |
| RBC radioactivity/plasma radioactivity | |||||
| AUC (tf) | 2.93 | 1.89 | 123 | 33 | |
| Excretion of radioactivity | |||||
| Urine | % of dose | 87.7 (2.02) | 86.7 (3.35) | 47.3 (6.90) | 71.6 |
| Feces | % of dose | 1.41 (0.91) | 17.6 (3.40) | 0.80 (0.07) | 8.50 |
| Total | % of dose | 97.6 (0.96) | 2.57 (0.32) | 55.8 (6.30) | 90.5 |
| Absorption | % | NA | 80.9 | NA | 79.1 |
Two monkeys had significant carryover from previous i.v. dosing and were not included in the calculation of the mean.
NA, not applicable.
NC, not calculated.
Radioactivity levels in rat plasma and RBC.
The radioactivity concentration at 5 min after i.v. administration of [14C]ribavirin was approximately 22.6 and 22.4 μg eq/ml in plasma and RBC, respectively. However, the radioactivity declined, with a t[1/2]α of 0.4 h in both plasma and RBC and a t[1/2]β of 2.30 h in plasma and 5.83 h in RBC. As a result, the radioactivity AUC (tf) in RBC (115 μg eq · h/ml) was 2.9-fold higher than that in plasma (39 μg eq · h/ml), indicating significant association of ribavirin with rat RBC. After oral administration, the radioactivity AUC (tf) in RBC (60 μg eq · h/ml) was 1.9-fold higher than that in plasma (32 μg · h/ml). By comparing the plasma radioactivity AUC (tf) obtained after oral dosing to that after i.v. dosing, the absorption was estimated to be 81.2% (Table 1).
Concentrations of ribavirin in monkey plasma.
After i.v. administration (10 mg/kg), the disposition kinetic of ribavirin was biphasic with an elimination t[1/2] of 130 h. The mean V was 29.4 liter/kg, and the mean CL of ribavirin was 224 ml/h/kg. After oral administration (10 mg/kg), ribavirin was absorbed with a Tmax of 1.5 h and a Cmax of 0.29 μg/ml. The elimination t[1/2] was 188 h. By comparing the AUC (I) obtained after oral dosing to that after i.v. dosing, the absolute bioavailability was calculated to be 29% (Table 1).
Radioactivity levels in monkey plasma and RBC.
The radioactivity concentration at 5 min after i.v. administration of [14C]ribavirin was 14.8 μg eq/ml in plasma and 41.8 μg eq/ml in RBC. Thereafter, the radioactivity declined, with a t[1/2] of 114 h in plasma and a t[1/2] of 316 h in RBC. Hence, the radioactivity AUC (tf) in RBC (5,830 μg eq · h/ml) was 123-fold higher than that for plasma (47.7 μg eq · h/ml). These data indicated a significant association of ribavirin to monkey RBC. After oral administration, the radioactivity AUC (tf) in RBC (1,450 μg eq · h/ml) was 33-fold higher than that in plasma (43.5 μg eq · h/ml) (Table 1). By comparing the plasma radioactivity AUC (tf) obtained after oral dosing to that obtained after i.v. dosing, the absorption was calculated to be more than 91.2%.
Urinary and fecal excretion of radioactivity in rats and monkeys.
Over a 96-h period, 87.7% of the i.v. dose and 86.7% of the oral dose were excreted in the urine (Table 1). In rat feces, 1.41% of the i.v. dose and 17.6% of the oral dose were excreted. These data demonstrated that biliary excretion did not play a significant role in the elimination of ribavirin in rats. The total recovery of radioactivity in urine and feces accounted for 97.6% of the i.v. dose and more than 100% of the oral dose.
Over a 168-h period, 47.3% of the i.v. dose and 71.6% of the oral dose were excreted in the urine. In monkey feces, 0.80% of the i.v. dose and 10.2% of the oral dose were excreted (Table 1). These data indicated that biliary excretion also played no significant role in the elimination of ribavirin in monkeys. The total recovery of radioactivity in urine and feces accounted for approximately 55.8% of the i.v. dose and 90.5% of the oral dose.
Metabolic profiles in plasma and urine of rats and monkeys.
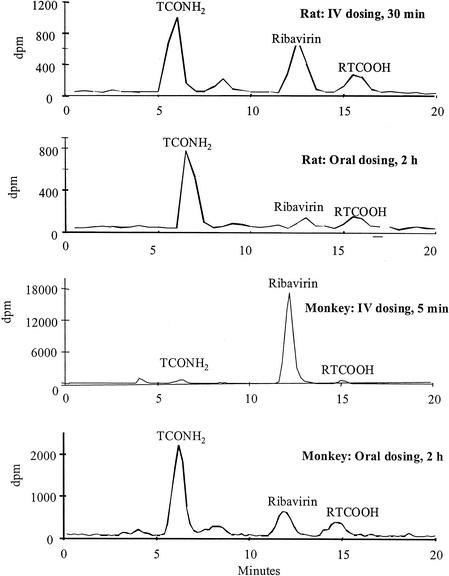
In rat plasma 30 min after i.v. dosing, ribavirin and TCONH2 are the two major radioactive peaks, with RTCOOH and unknown 1 as the minor metabolites detected (Fig. 1). However, at 2 h after oral dosing, TCONH2 is the only major radioactive peak, with small amounts of ribavirin and RTCOOH detected, indicating a significant role of first-pass effect in the liver.
FIG. 1.
Metabolic profiles in rat and monkey plasma after i.v. and oral administration of [14C]ribavirin. dpm, disintegrations per minute.
In monkey plasma 30 min after i.v. dosing, ribavirin is the only predominant radioactive peak, indicating a much lesser extent of metabolism in monkeys than in rats. At 2 h after oral dosing, TCONH2 is the only major radioactive peak, with smaller amounts of ribavirin, RTCOOH, and unknown metabolites detected, again indicating a significant first-pass effect in monkeys.
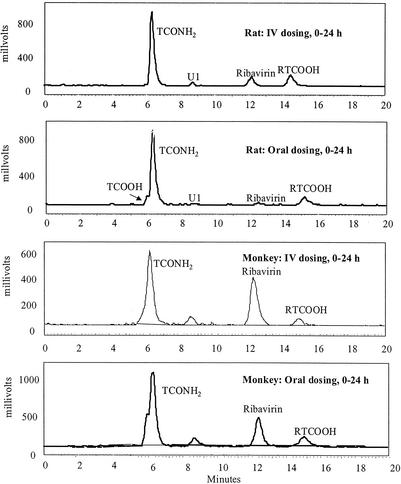
In rat urine after (0 to 24 h) either i.v. or oral dosing, TCONH2 is the only predominant radioactive peak, with very small amounts of ribavirin, RTCOOH, and TCOOH detected (Fig. 2). In monkey urine after (0 to 24 h) either i.v. or oral dosing, TCONH2 and ribavirin are the two major radioactive peaks (Fig. 2). These urinary metabolic data are in good agreement with the plasma metabolic data indicating that there is a much lesser extent of metabolism in monkey than in rats.
FIG. 2.
Metabolic profile in rat and monkey urine after i.v. and oral administration of [14C]ribavirin. U1, unknown 1.
DISCUSSION
It has been reported previously (1, 3, 4, 5) that ribavirin readily entered RBC and converted to phosphorylated derivatives, including ribavirin triphosphate (RTP). Due to the lack of dephosphorylation enzymes in RBC, RTP accumulated with time. As RTP resembles ATP from a structure perspective, it may competitively inhibit ATP-dependent energy utilization in RBC, leading to hemolytic anemia. The severity of anemia is the highest in cynomolgus monkeys, followed by humans, rats, and dogs. These observations are in agreement with the results reported here; i.e., the ratio of RBC radioactivity AUC to plasma radioactivity AUC was 1.89 in rats and 33 in monkeys after oral dosing.
Ribavirin was well absorbed in rats and monkeys. Based on the ratio of plasma radioactivity AUC obtained after oral dosing to that obtained after i.v. dosing, absorption was estimated to be 81.2% for rats and 91.2% for monkeys. This is in good agreement with the extent of absorption for rats (80.9%), but not for monkeys (79.1%), based on the percentage of radioactivity excreted in urine after oral dosing and corrected for the total recovery of radioactivity in urine, feces, and various tissues. Therefore, percentages of absorption for drugs with extensive distribution to RBC, such as ribavirin, should be estimated from the total urinary recovery after oral dosing, corrected for the total recovery in urine, feces, and various tissues.
The t[1/2] of ribavirin for rats (9.9 h) was much shorter than that for monkeys (130 h). On the contrary, total CL for rats (2,600 ml/h/kg of body weight) was much larger than that for monkeys (224 ml/h/kg). These data indicated that a higher extent of ribavirin metabolism occurred in rats than monkeys. This is further supported by a lower ratio of plasma ribavirin AUC to plasma radioactivity AUC after oral dosing for rats (0.08) than for monkeys (0.18). Ribavirin was metabolized primarily to TCONH2 by deribosylation, with a small amount of metabolite as RTCOOH through deamination. TCONH2 was the major radioactive component in rat and monkey urine after either i.v. or oral dosing and in rat and monkey plasma after oral dosing, with ribavirin and RTCOOH as the minor radioactive components. However, in monkey plasma after i.v. dosing, ribavirin was the only major radioactive component, whereas for rats, both ribavirin and TCONH2 were major radioactive components, again confirming that ribavirin was metabolized faster in rats than in monkeys. Ribavirin was excreted primarily into urine. Biliary excretion played an insignificant role, since fecal excretion of radioactivity accounted for only 1.4% of the i.v. dose in rats and only 0.8% of the i.v. dose in monkeys.
REFERENCES
- 1.Catlin, D. H., R. Smith, and A. I. Samuels. 1980. 14C-ribavirin: distribution and pharmacokinetic studies in rats, baboon and man, p. 83-98. In R. A. Smith and W. Kirkpatrick (ed.), Ribavirin: a broad spectrum antiviral agent. Academic Press, New York, N.Y.
- 2.Ferrara, E. A., J. S. Oishi, R. W. Wannemacher, Jr., and E. L. Stephen. 1981. Plasma disappearance, urine excretion, and tissue distribution of ribavirin in rats and rhesus monkeys. Antimicrob. Agents Chemother. 19:1042-1049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Laskin, O. L., J. A. Longstreth, C. C. Hart, D. Scavuzzo, C. M. Kalman, J. D. Connor, and R. B. Roberts. 1987. Ribavirin disposition in high-risk patients for acquired immunodeficiency syndrome. Clin. Pharmacol. Ther. 41:546-555. [DOI] [PubMed] [Google Scholar]
- 4.Miller, J. P., L. J. Kigwana, D. G. Streeter, R. K. Robins, L. N. Simon, and J. Roboz. 1977. The relationship between the metabolism of ribavirin and its proposed mechanism of action. Ann. N. Y. Acad. Sci. 284:211-229. [DOI] [PubMed] [Google Scholar]
- 5.Page, T., and J. D. Conner. 1990. The metabolism of ribavirin in erythrocytes and nucleated cells. Intl. J. Biochem. 22:379-383. [DOI] [PubMed] [Google Scholar]
- 6.Sidwell, R. W., J. H. Huffman, G. P. Khare, L. B. Allen, J. T. Witkowski, and R. K. Robins. 1972. Broad-spectrum antiviral activity of virazole: 1-β-d-ribofuranosyl-1,2,4-triazole-3-carboxamide. Science 177:705-706. [DOI] [PubMed] [Google Scholar]
- 7.Smith, R. A. 1980. Mechanism of action of ribavirin, p. 99-118. In R. A. Smith and W. Kirkpatrick (ed.), Ribavirin: a broad spectrum antiviral agent. Academic Press, New York, N.Y.
- 8.Stephen, E. L., D. E. Jones, C. J. Peters, G. A. Eddy, P. S. Loizeaux, and P. B. Jahrling. 1980. Ribavirin treatment of Toga-, Arena-, and Bunyavirus infections in subhuman primates and other laboratory animal species. In R. A. Smith and W. Kirkpatrick (ed.), Ribavirin: a broad spectrum antiviral agent. Academic Press, New York, N.Y.
- 9.Streeter, D. G., J. T. Witkowski, G. P. Khare, R. W. Sidwell, R. J. Bauer, R. K. Robins, and L. N. Simon. 1973. Mechanism of action of 1-β-d-ribofuranosyl-1,2,4-triazole-3-carboxamide (virazole), a new broad-spectrum antiviral agent. Proc. Natl. Acad. Sci. USA 70:1174-1178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tam, R. C., B. P. Pai, J. Bard, C. Lim, D. R. Averett, U. T. Phan, and T. Milovanovic. 1999. Ribavirin polarizes human T cell responses towards a Type 1 cytokine profile. J. Hepatol. 30:376-382. [DOI] [PubMed] [Google Scholar]
- 11.Tam, R. C., C. Lim, J. Bard, and B. Pai. 1999. Contact hypersensitivity responses following ribavirin treatment in vivo are influenced by Type 1 cytokine polarization, regulation of IL-10 expression, and costimulatory signaling. J. Immunol. 163:3709-3717. [PubMed] [Google Scholar]
- 12.Tam, R. C., K. Ramasamy, J. Bard, B. Pai, C. Lim, and D. R. Averett. 2000. The ribavirin analogue ICN 17261 demonstrates reduced toxicity and antiviral effects with retention of both immunomodulatory activity and reduction of hepatitis-induced serum alanine aminotransferase levels. Antimicrob. Agents Chemother. 44:1276-1283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tam, R. C., J. Y. N. Lau, and Z. Hong. Mechanism of action of ribavirin in antiviral therapies. Antiviral Chem. Chemother., in press. [DOI] [PubMed]