SYNPOSIS
In January 2005, the U.S. Centers for Disease Control and Prevention hosted a national consultation of scientists, public health officials, and community service providers to address growing concerns about the association of methamphetamine use and sexual risk behavior for HIV/STD infection, which is well documented among men who have sex with men. The purpose of the consultation was to review a representation of the current state of the science and practice on the topic in order to reduce the situational link of methamphetamine use and sexual risk. A set of suggestions for future research and programs were developed by the participants. This article provides a summary of content and recommendations from the consultation, and not an exhaustive review of the literature.
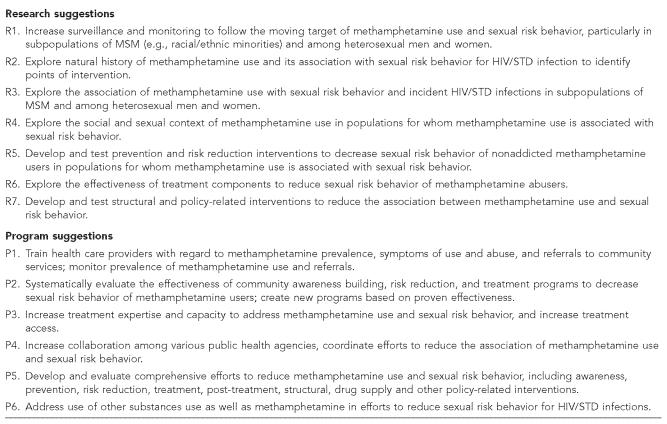
On January 13 and 14, 2005, the U.S. Centers for Disease Control and Prevention (CDC) hosted a national consultation of scientists, public health officials, and community service providers to address growing public health concerns regarding the association of methamphetamine use and sexual risk behavior for HIV/STD infection. The consult was intended to provide a representative, albeit not exhaustive, review of current science and practice up to that time, and focused largely on men who have sex with men (MSM) because of the well-documented association between methamphetamine use and sexual risk behavior in those populations. What follows is a summary of the consult, including a list of research and program suggestions (Figure) developed by the participants.
Figure.
Research and program suggestions from the CDC consultation on methamphetamine use and sexual risk behavior for HIV/STD infection
BACKGROUND
Waves of increased methamphetamine use have been observed in the United States after World War II, during the 1960s and 1970s, and, currently, since the 1980s.1 By the early 1990s, methamphetamine use was increasingly prevalent in the western United States, and it has gradually moved to the Midwest and East.2 Small lab manufacturing of methamphetamine has also increased, particularly in rural and suburban regions.3 In many areas of the country, methamphetamine is notably or increasingly associated with arrests and treatment admissions.4
Methamphetamine is a Schedule II drug and a central nervous system stimulant with a high potential for addiction. Chemically-similar, amphetamines are legally available for treatment of narcolepsy, obesity, and attention deficit disorder.5 Cognitive changes in the orbitofrontal cortex of methamphetamine abusers are similar to those of cocaine and other substance abusers, and possibly underlie loss of control and compulsive behavior.6 However, methamphetamine use also has distinct, long-lasting cognitive effects such as sensitization.7 Physical effects of methamphetamine use include increased heart rate and blood pressure, decreased appetite, increased alertness and restlessness, inability to sleep, talkativeness, teeth grinding, hyperthermia, convulsion, and death.5 Usage over time can cause effects such as irritability, aggressiveness, paranoia, and hallucinations.5,8 Enhanced sensitization in studies of rats suggest that methamphetamine use can increase sexual behavior.9,10 Methamphetamine use may cause impotence at the same time it increases libido and decreases inhibitions, which could lead to use of medication for erectile dysfunction by men (e.g., sildenafil) or increased receptive anal sex among MSM. Some of the effects of methamphetamine may be partly functional, including increased energy, mood enhancement, weight loss, and heightened sexual sensitivity and pleasure.3 These factors should be considered when developing interventions.
PREVALENCE OF METHAMPHETAMINE USE
Prevalence of methamphetamine use by MSM varies according to sampling method and behavioral assessment window. A 2001 study11 found that 15% of MSM in San Francisco used methamphetamine during their most recent anal sex episode in the prior three months, which was third only to the prevalence of alcohol and marijuana use. Suggesting a geographical difference at the time, a 2000–01 baseline study of HIV-positive MSM found a higher prevalence of three-month methamphetamine use for participants in San Francisco (18%) compared to New York (7%; p<0.001). (Personal communication, David Purcell, CDC, October 24, 2005). Preliminary data from the 2004 CDC National HIV Behavioral Surveillance of MSM suggest that overall a higher percentage of methamphetamine users (50.4%) were white compared to non-users (43.5%; p<0.05), (Personal communication, Amy Drake, CDC, October 24, 2004). Further analyses of methamphetamine use data are needed to examine potential race/ethnicity and other demographic differences nationally and by region.
Methamphetamine use in the general population is relatively low compared to use in some populations of MSM. Data from the Monitoring the Future study indicate that there are no increasing trends in methamphetamine use in a general population of 12th graders, with an annual prevalence of 4.7% in 1999 to 3.6% in 2002.12 However, other data show recent increases in methamphetamine-related arrests and in treatment and emergency room admissions overall.13,14 Any of these methamphetamine use findings could change in the future if use continues to expand; additional data are needed to more thoroughly assess and monitor national and regional trends in methamphetamine use.
ASSOCIATION BETWEEN METHAMPHETAMINE USE AND SEXUAL RISK BEHAVIOR
Methamphetamine use is associated with sexual risk behavior; this is well documented among MSM in studies with various windows of behavioral assessment (e.g., three and 12 months, and most recent sexual encounter).11,15,16 Methamphetamine use is consistently associated with unprotected anal sex among MSM, particularly unprotected receptive anal sex (URA). For example, among HIV-positive MSM, methamphetamine users were more than twice as likely than non-users to report URA with a partner whose HIV serostatus was negative or unknown, and more than four times as likely to report the behavior with HIV-positive partners in the past three months.11 More specifically, HIV-positive or HIV-negative MSM who used methamphetamine immediately before or during anal sex were twice as likely as MSM who did not use methamphetamine to report URA during that encounter;12 alternatively, Viagra use was associated with unprotected insertive anal sex.
Some evidence suggests that methamphetamine use may also be associated with unprotected vaginal sex and with a higher number of sex partners in the past 12 months among heterosexual men and women who are not injection drug users (IDUs) attending HIV testing centers in California in 1994–95 (males: 4.5 partners for meth users versus 2.9 partners for non-users [p<0.0001]; females: 4.5 versus 2.4 partners, respectively [p<0.0001]).17 However, there was an even larger difference in number of sex partners for gay meth users (13.6) compared to non-users (6.9; p<0.0001).17 Other studies have found relatively high rates of sexual risk behavior among heterosexual IDUs who use methamphetamine.18
HIV-positive MSM may be more likely than HIV-negative MSM to use methamphetamine,12 and some MSM methamphetamine users may be more likely than other methamphetamine users to use it during sex.17 A study of HIV-positive MSM who use methamphetamine19 found that the most frequently self-reported motivation for using methamphetamine was to enhance sexual pleasure (reported by nearly 90%). Yet, a study of HIV-negative heterosexual (male and female) methamphetamine users20 did not find sexual pleasure to be a self-reported motivator. An assessment of Latino gay men also showed that sexual enhancement was a primary reason for methamphetamine use.21 Thus, existing data indicate a solid link between methamphetamine use and sexual risk among MSM and perhaps among heterosexual men and women. More research is needed on differences between heterosexuals and MSM and on differences among heterosexuals by gender.
ASSOCIATION BETWEEN METHAMPHETAMINE USE AND STD INFECTION AMONG MSM
Not surprisingly, the link between methamphetamine use and sexual risk is also related to STD infection. STD clinic data for MSM in San Francisco showed that increased risk for early syphilis infection was associated with methamphetamine use (especially when combined with Viagra) in the past four weeks.22 Increased risk for early syphilis was also seen for MSM who were not white in race/ethnicity, were HIV infected, had met sex partners on the Internet, and reported stronger identification and behavioral affiliation with gay communities. Another analysis of the same data showed that methamphetamine use was associated with HIV infection, syphilis infection, coinfection with two or more STDs, age under 35 years, depression, and use of more than one substance.22 A nested case-control study of MSM recruited on the Internet found men who had used methamphetamine in the prior six months were twice as likely as those who had not to report an STD infection during the same six-month period.23
CONTEXTS OF METHAMPHETAMINE USE AND SEXUAL RISK BEHAVIOR AMONG MSM
A study of methamphetamine users in Seattle during the 1990s revealed five primary subgroups or contexts of MSM methamphetamine use: party circuits, bathhouses or sex clubs, transgender circles, youth circles (club or street scene), and self-medicating HIV-positive men (often depressed, homeless, and IDU).24 In another study, a greater proportion of MSM who attended circuit parties (weekend-long series of dance parties) in the prior year reported methamphetamine use than did MSM who had not attended a circuit party.25 Further, among MSM who had attended circuit parties, more of them reported use of methamphetamine and other substances during circuit party weekends than during weekends they attended dance clubs or other weekends, particularly when the parties were away from their town of residence (San Francisco).16 Men who used methamphetamine during circuit party weekends were more than twice as likely (versus men who did not) to have unprotected anal sex during that weekend with a partner whose HIV status was unknown or different from theirs.
Regarding partner interactions, methamphetamine-addicted, HIV-positive MSM tended to report a sense of obligation to disclose their HIV status if they engaged in a sexual behavior perceived to carry greater risk for HIV transmission.26 However, many of these HIV-positive participants did not disclose their serostatus but believed that they protected the health of their sex partners by avoiding high-risk sexual behaviors; of note, perceptions of high-risk sex varied dramatically for both HIV-positive and HIV-negative participants.
METHAMPHETAMINE AWARENESS AND PREVENTION
Several examples of community awareness campaigns or prevention efforts were presented at the consultation; however, little or no evidence was reported on the effectiveness of these programs. Evaluation of existing programs is essential to determine whether or not prevention activities are effective. Community representatives stated, anecdotally, that task forces have been useful in systematically addressing methamphetamine use. These coalitions often include drug treatment and HIV/STD prevention service providers; policy makers; public health and law enforcement officials; representatives of business, civic, and faith-serving agencies; other non-government organizations; and community members. Consult participants recommended (1) assessing the unique situation in a given community before acting; (2) evaluating realistic and worthwhile “success” outcomes; (3) using methods (whenever possible) that have been assessed and found to be effective; (4) working to change behavioral norms that accept or encourage methamphetamine use and sexual risk behavior; (5) training health providers, policy makers, law enforcement, and other community leaders; (6) being sensitive to racial/ethnic and sexual orientation diversity; (7) collaborating with representatives of target populations; and (8) using programs that are flexible and can be customized to the needs of a particular population or setting.
METHAMPHETAMINE TREATMENT
Drug treatment for MSM who use methamphetamine can dramatically reduce sexual risk behavior as well as methamphetamine use,27,28 although no particular treatment approach has been found to be more effective than another. Drug treatment should be a part of a comprehensive community effort to reduce sexual risk behavior. Because the majority of drug users are not enrolled in an inpatient setting at any one time, communities should explore the use of less intensive resources, such as outpatient treatment, 12-step groups, community forums, and general support groups.
The following suggestions were offered based on experiences of existing community-based drug treatment programs: (1) meet the users “where they are” (i.e., some will be seeking abstinence while others will not); (2) assess the degree of methamphetamine use, abuse, dependence, or addiction; (3) provide a comprehensive set of options varying from outreach-based harm reduction to residential treatment; (4) focus on both sex- and drug-related risk behaviors; (5) address use of other substances in addition to methamphetamine; and (6) develop collaborative relationships between community providers and research institutions.
POLICY APPROACHES
National, state, and local agencies have pursued policy-related actions in response to the burgeoning methamphetamine problem. Policies to control methamphetamine production have had important, if temporary, effects in reducing methamphetamine-related abuse, hospitalizations, and arrests.13,14 Some communities have considered policies for sex venues where methamphetamine users with high levels of sexual risk behavior may be more likely to come into contact with non-users or people at lower risk. These venues include bathhouses, sex clubs, circuit parties, and Internet sites. Such policies include reducing hours of operation, and development and enforcement of drug-free venues.
On November 19, 2004, the National Coalition of STD Directors presented testimony to the CDC/HRSA federal Advisory Committee on HIV and STD Prevention and Treatment advocating four action steps: (1) increase availability of drug treatment slots; (2) evaluate and adapt current prevention efforts; (3) adopt and scale up contingency management (e.g., vouchers that can be exchanged for goods and services following drug-free urine samples); and (4) convene a national task force to address networks of methamphetamine manufacturing and distribution to MSM.
FINAL COMMENT
Methamphetamine use and sexual risk behavior are public health issues in the United States. Methamphetamine use and risk for HIV/STD infection can occur together and are a concern for communities of MSM and potentially other populations, although more surveillance and research are needed. This may also be the case in other industrialized countries that have seen recent increases in STDs among MSM. National, state, and local organizations should continue to work together to develop comprehensive and balanced approaches that effectively prevent or reduce methamphetamine and other drug use and sexual risk behavior in our communities.
The research and program suggestions generated from the CDC consultation provide only a general framework. Scientists and evaluators need to address the large gaps in knowledge that currently exist, and funding agencies should come together to accomplish this goal. Health officials and program specialists, with the help of scientists, should take what is known from research and evaluation and use it to implement effective community programs. The challenge for communities is to determine how best to allocate limited resources among prevention, treatment, and policy activities to achieve maximum epidemiological benefit.
Acknowledgments
The authors thank Rob Janssen, MD, and John Douglas, MD, for their support of this consultation at CDC, and Lynne Stockton for her editing assistance. Sincere appreciation goes to each of the speakers for their important contributions to the CDC methamphetamine consultation: Lynda Erinoff, PhD, William Wong, MD, Rafael Diaz, PhD, Don Des Jarlais, PhD, Steven Tierney, EdD, Steve Shoptaw, PhD, Richard Rawson, PhD, Peter Staley, Joel Kaufman, PhD, Cathy Reback, PhD, Sabina Hirshfield, PhD, Michael Siever, PhD, Dan Wohlfieler, Blake Harrison, and Cornelius Baker. The authors also extend their gratitude to the consult chairpersons and rapporteurs, the more than 100 consult participants, Jacques Normand, PhD, and Lynda Erinoff, PhD, with the National Institute on Drug Abuse and Andrew Forsyth, PhD, with the National Institute on Mental Health, and all others in the field for their continued involvement in addressing this important public health issue.
REFERENCES
- 1.Narconon Arrowhead. History of methamphetamine and amphetamine timeline. [cited 2005 Oct 20]. Available from: URL: http://www.methamphetamineaddiction.com/methamphetamine_timeline.html.
- 2.National Institute on Drug Abuse. Methamphetamine abuse and addiction. [cited 2005 Oct 20]. Available from: URL: http://www.drugabuse.gov/researchreports/methamph/methamph.html.
- 3.Nodeworks Encyclopedia. Methamphetamine. [cited 2005 Dec 19]. Available from: URL: http://pedia.noteworks.com/M/ME/MET/Methamphetamine.
- 4.National Institute on Drug Abuse. NIDA InfoFacts: methamphetamine. [cited 2005 Oct 20]. Available from: URL: http://www.nida.nih.gov/infofacts/methamphetamine.html.
- 5.Hanson G, Venturelli PJ. Drugs and society. Boston: Jones – Bartlett; 1998. [Google Scholar]
- 6.Volkow ND, Chang L, Wang GJ, Fowler JS, Ding YS, Sedler M, et al. Low level of brain dopamine D2 receptors in methamphetamine abusers: association with metabolism in the orbitofrontal cortex. Am J Psychiatry. 2001;158:2015–21. doi: 10.1176/appi.ajp.158.12.2015. [DOI] [PubMed] [Google Scholar]
- 7.Wang GJ, Volkow ND, Chiang L, Miller E, Sedler M, Hitzemann R, et al. Partial recovery of brain metabolism in methamphetamine abusers after protracted abstinence. Am J Psychiatry. 2004;161:242–8. doi: 10.1176/appi.ajp.161.2.242. [DOI] [PubMed] [Google Scholar]
- 8.Comer SD, Hart CL, Ward AS, Haney M, Foltin RW, Fischman MW. Effects of repeated oral methamphetamine administration in humans. Psychopharmicology (Berl) 2001;155:397–404. doi: 10.1007/s002130100727. [DOI] [PubMed] [Google Scholar]
- 9.Robinson TE, Berridge KC. Addiction. Annual Rev Psychol. 2003;54:25–53. doi: 10.1146/annurev.psych.54.101601.145237. [DOI] [PubMed] [Google Scholar]
- 10.Fiorino DF, Phillips AG. Facilitation of sexual behavior in male rats following d-amphetamine-induced behavioral sensitization. Psychopharmicology (Berl) 1999;142:200–8. doi: 10.1007/s002130050880. [DOI] [PubMed] [Google Scholar]
- 11.Mansergh G, Shouse RL, Marks G, Guzman R, Rader M, Buchbinder S, et al. Sex Transm Infect. 2005. Methamphetamine and sildenafil (Viagra) use are linked to unprotected receptive and insertive anal sex, respectively, in a sample of men who have sex with men. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Monitoring the Future study. [cited 2005 Jan 10]. Available from: URL: http://www.monitoringthefuture.org.
- 13.Cunningham JK, Liu LM. Impacts of federal precursor chemical regulations on methamphetamine arrests. Addiction. 2005;100:479–88. doi: 10.1111/j.1360-0443.2005.01032.x. [DOI] [PubMed] [Google Scholar]
- 14.Cunningham JK, Liu LM. Impacts of federal ephedrine and pseudoephedrine regulations on methamphetamine-related hospital admissions. Addiction. 2003;98:1229–37. doi: 10.1046/j.1360-0443.2003.00450.x. [DOI] [PubMed] [Google Scholar]
- 15.Purcell DW, Moss S, Remien RH, Woods WJ, Parsons JT. Illicit substance use, sexual risk, and HIV-positive gay and bisexual men: differences by serostatus of casual partners. AIDS. 2005;19:S37–47. doi: 10.1097/01.aids.0000167350.00503.db. [DOI] [PubMed] [Google Scholar]
- 16.Colfax GN, Mansergh G, Guzman R, Vittinghoff E, Marks G, Rader M, et al. Drug use and sexual risk behavior among gay and bisexual men who attend circuit parties: a venue-based comparison. J Acquir Immune Defic Synd. 2001;28:373–9. doi: 10.1097/00126334-200112010-00011. [DOI] [PubMed] [Google Scholar]
- 17.Molitor F, Truax SR, Ruiz JD, Sun RK. Association of methamphetamine use during sex with risky sexual behaviors and HIV infection among non-injection drug users. West J Med. 1998;168(2):93–7. [PMC free article] [PubMed] [Google Scholar]
- 18.Des Jarlais D, Shimizu S. Methamphetamine injection among heterosexuals; Proceedings of the CDC Methamphetamine Consultation; Atlanta: GA; 2005. Jan 13, [Google Scholar]
- 19.Semple SJ, Patterson TL, Grant I. Motivations associated with methamphetamine use among HIV+ men who have sex with men. J Subst Abuse Treat. 2002;22(3):149–56. doi: 10.1016/s0740-5472(02)00223-4. [DOI] [PubMed] [Google Scholar]
- 20.Semple SJ, Patterson TL, Grant I. The context of sexual risk behavior among heterosexual methamphetamine users. Addict Behav. 2004;29:807–10. doi: 10.1016/j.addbeh.2004.02.013. [DOI] [PubMed] [Google Scholar]
- 21.Diaz RM, Heckert AL, Sanchez J. Reasons for stimulant use among Latino gay men in San Francisco: a comparison between methamphetamine and cocaine users. J Urban Health. 2005;82(1Suppl 1):i71–8. doi: 10.1093/jurban/jti026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wong W, Chaw JK, Kent CK, Klausner JD. Risk factors for early syphilis among gay and bisexual men seen in an STD clinic: San Francisco, 2002–2003. Sex Transm Dis. 2005;32:458–63. doi: 10.1097/01.olq.0000168280.34424.58. [DOI] [PubMed] [Google Scholar]
- 23.Hirshfield S, Remien RH, Walavalkar I, Chiasson MA. Crystal methamphetamine use predicts incident STD infection among men who have sex with men recruited online: a nested case-control study. J Med Internet Res. 2004;6(4):e41. doi: 10.2196/jmir.6.4.e41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gorman EM, Carroll RT. Substance abuse and HIV: considerations with regard to methamphetamines and other recreational drugs for nursing practice and research. J Assoc Nurses AIDS Care. 2000;11(2):51–62. doi: 10.1016/S1055-3290(06)60286-0. [DOI] [PubMed] [Google Scholar]
- 25.Mansergh G. Characteristics and behavior of MSM who attend circuit parties compared to MSM who do not: a three-study assessment. Proceedings of the National HIV Prevention Conference; Atlanta, GA. 2001. Aug 12-15, [Google Scholar]
- 26.Larkins S, Reback CJ, Shoptaw S, Veniegas R. Methamphetamine-dependent gay men's disclosure of their HIV status to sexual partners. AIDS Care. 2005;17:521–32. doi: 10.1080/09540120512331314321. [DOI] [PubMed] [Google Scholar]
- 27.Shoptaw S, Reback CJ, Peck JA, Yang X, Rotheram-Fuller E, Larkins S, et al. Behavioral treatment approaches for methamphetamine dependence and HIV-related sexual risk behaviors among urban gay and bisexual men. Drug Alcohol Depend. 2005;78:125–34. doi: 10.1016/j.drugalcdep.2004.10.004. [DOI] [PubMed] [Google Scholar]
- 28.Reback CJ, Larkins S, Shoptaw S. Changes in the meaning of sexual risk behaviors among gay and bisexual male methamphetamine abusers before and after drug treatment. AIDS Behav. 2004;8:87–98. doi: 10.1023/b:aibe.0000017528.39338.75. [DOI] [PubMed] [Google Scholar]