The United Kingdom has seen rapid rises in immigration of minorities culturally and linguistically different from the majority population. The 2001 census showed that ethnic minority groups comprised about 7.9% of the population of the United Kingdom, with people of Indian, Pakistani, or Bangladeshi origin comprising about 3.6%.1 Similar to the initiatives to decrease health care disparities in the United States, the Department of Health in England has given priority to equity in health care provision, with a focus on minority ethnic groups.2 Researchers in both the U.S. and the UK have voiced concerns about whether ethnic groups should be considered homogeneous, and how this might affect comparisons with majority groups and the planning of health care interventions.”3
Although in many respects ethnic minority groups often have similar levels of morbidity and mortality as the ethnic majority population, there are some key differences. For example, diabetes is more common in South Asians and coronary heart disease is moderately more common in South Asian groups, particularly those of Pakistani and Bangladeshi origins.4 Furthermore, the extent to which health services adequately respond to the health care needs and preferences of minority ethnic group patients is variable.4
As health care organizations develop health care services for ethnic minority populations, they need to understand whether separate ethnic minority groups can be considered as part of a larger homogeneous group. For example, some data suggest that the distribution of cardiovascular risk factors is not uniform among South Asian subgroups.5 Thus, for planning purposes, are South Asians similar enough that the Indian, Pakistani, and Bangladeshi communities can be collapsed into a single entity?
One characteristic that may be particularly important in planning health care policy and interventions for ethnic minority groups is sensitivity to language differences with the majority group. Ethnic minorities’ inability to speak the majority group’s language can be a significant barrier to care and may affect providers’ ability to recognize disease. Studies focusing on Hispanics in the United States have shown that lack of English language skill and use is a barrier to care.6–9 Language and foreign birth have been used as proxies for acculturation, a multidimensional process in which individuals whose primary learning has been in one culture adapt to reflect the host culture.10–12
Little investigation of within-group differences among South Asian immigrants to England has been undertaken, especially in light of the potential role of English language skills in the prevalence and recognition of diabetes and hypertension. The purpose of this study was to examine language skills among foreign-born South Asians in England and the prevalence of diagnosed diabetes and hypertension and undetected elevated blood glucose and high blood pressure in a nationally representative sample.
METHODS
The data used for this study were from the 1999 Health Survey for England (HSE), an annual survey based on a nationally representative, probability sampling design for England. Although the HSE is conducted annually, each year the survey has a unique focus. The focus may be on disease entities (e.g., cardiovascular disease in the 2003 HSE) or on special populations (e.g., the elderly in the 2000 HSE and children and young people in the 2002 HSE). The 1999 HSE was focused on ethnic minority health because the general population surveys did not include sufficient minority participation to make distinctions regarding different minority groups. In the 1999 survey, minorities were oversampled but appropriate weights were included to make population estimates.
This study focused on foreign-born South Asian (Indian, Pakistani, and Bangladeshi) adults (≥18 years of age). This group was selected for several reasons. First, we wanted to focus on an immigrant minority population with potential language difficulties because of issues that might be unique to them. Second, by performing within-group analyses focusing on language skill among minority immigrants and detection of disease, we could investigate differences within minority groups as well as investigating a barrier to care that is potentially addressable through common interventions. Thus, native-born minorities or immigrants from countries with English as the predominant language were not included in the study (e.g., Great Britain-born South Asians, Black Caribbeans, Irish). We considered analyzing one additional group in the HSE, foreign-born Chinese. Unfortunately, the sample size of this group was too small to be analyzed with an appropriate degree of reliability.
Although interviews were conducted in respondents’ language of choice, an item asking the respondent to self-assess spoken English language ability was included. The response categories were “very well,” “fairly well,” “slightly,” or “not at all.” We classified high language acculturation as individuals who assessed their ability to speak English as very or fairly well. Low language ability was defined as individuals who assessed their ability to speak English as slightly or not at all.
Dependent variables
Diabetes/previously diagnosed diabetes
A diagnosis of diabetes was assessed by an item asking if a doctor had ever told the respondent that he or she has diabetes. This categorization has been used in previous studies.13,14
Undetected elevated blood glucose
Among individuals who have not been previously diagnosed with diabetes, elevated glycosylated hemoglobin (HbA1c) seems to indicate substantial risk for diabetes. Since HbA1c is a function of blood glucose and diabetes is defined as elevated blood glucose, HbA1c is a good indicator of diabetes.15 The use of HbA1c as a method of screening for diabetes has shown significant utility and may produce a conservative estimate of the prevalence of diabetes.16,17 Hanson et al. showed that fasting plasma glucose and HbA1c are similar in predictive ability for the detection of non-insulin-dependent diabetes mellitus (NIDDM) as defined by WHO criteria.18 Further, the Diabetes Control and Complications Trial Research Group (DCCT) suggests that HbA1c can be considered as a simple diagnostic test for NIDDM.19 Following Rohlfing’s work15 and the Diabetes UK standard that normal HbA1c is <6.1%,20 we define elevated blood glucose as HbA1C greater than 6.1%.
Hypertension/previously diagnosed hypertension
A diagnosis of hypertension was based on a question asking if a doctor had ever told the respondent that he or she has high blood pressure, excluding during pregnancy.
Undetected elevated blood pressure
Among individuals who denied being told by a doctor that they had high blood pressure, current high blood pressure was assessed. Blood pressure was calculated using the following protocol: three readings of systolic and diastolic blood pressure were collected at one-minute intervals in the right upper arm. Mean systolic blood pressure greater than 140 mm Hg or diastolic blood pressure greater than 90 mm Hg was considered elevated.21
Control variables
The HSE measured language use and a number of variables that might affect the relationship between prevalence and recognition of disease among ethnic minorities. These include age, gender, education, and body mass index (BMI). Because the study was limited to foreign-born adults, education was assessed as having reported an achieved qualification or not. BMI was derived from height and weight measurements (kg/m2) collected in the physical examination. BMI was classified as <25 for normal or underweight, 25–29.9 for overweight, and ≥30, which corresponds with a classification of obesity.22
Analysis plan
Our analysis incorporated the sample weights recommended for ethnic group analyses based on their probability of selection. Chi-square analyses were used for bivariate comparisons between language and diabetes and hypertension prevalence and undetected risk. Logistic regression models were computed for language and the diabetes and hypertension measures while controlling for age, sex, education, and BMI.
RESULTS
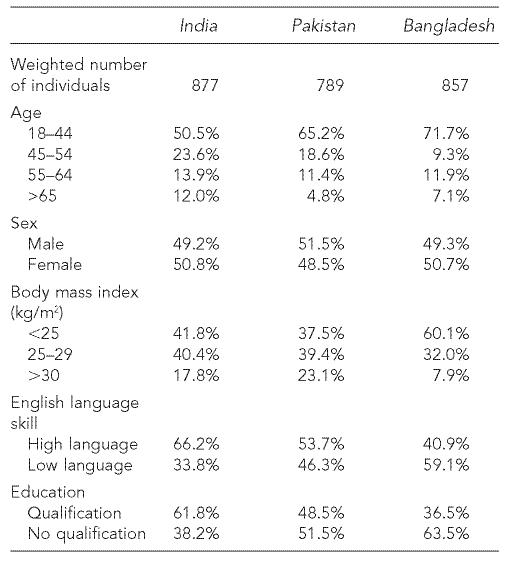
The characteristics of the three South Asian groups are shown in Table 1. Bangladeshis were generally younger, had lower self-assessed language skills in English, and had lower BMI than the other two groups.
Table 1.
Demographic characteristics of foreign-born South Asian adults
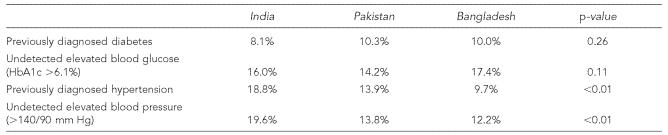
Table 2 indicates a high prevalence of diagnosed diabetes among each of the South Asian groups with no significant difference between the groups. The 1999 HSE does not include the general population prevalence of diabetes but these can be obtained from the 1998 HSE. The English white population prevalence of physician-diagnosed diabetes among individuals 18 and older from the 1998 HSE was 2.8%. Undetected elevated blood glucose levels were also substantial, with prevalence estimates for Indians double that of diagnosed diabetes.
Table 2.
Previously diagnosed diabetes and hypertension and elevated risk markers among foreign-born South Asian adults
UK-born South Asians included in the 1999 HSE were relatively young, with few over age 44 (<5 individuals in the HSE). Consequently, a comparison of UK-born vs. foreign-born individuals 18 and older would therefore be inappropriate for diabetes and hypertension, diseases that tend to appear in later life. However, the UK-born South Asian individuals aged 18–44 have significantly lower prevalence of diagnosed disease and undetected elevated glucose and blood pressure than their 18–44 year-old foreign-born counterparts. UK-born adults had a prevalence rate of 0.8% for diagnosed diabetes, while the foreign-born individuals had a prevalence of 2.5% (p=0.008). The prevalence of undetected elevated glucose was 7.2% for the UK-born individuals and 11.5% for those foreign born (p=0.03). Similarly, the UK-born South Asians had a diagnosed prevalence of hypertension of 3.1% vs. 6.0% for the foreign-born individuals (p=0.003). The prevalence of undetected elevated blood pressure was 4.8% for the UK born and 8.7% for the foreign born (p=0.02).
The prevalence of diagnosed hypertension varied significantly between the ethnic groups. The prevalence of diagnosed hypertension, as opposed to diagnosed diabetes, was closer to general population estimates, with all of the South Asian groups having lower prevalence. The English white population prevalence of physician-diagnosed hypertension from the 1998 HSE was 20.4%. Undetected elevated blood pressure also differed between the groups but accounted for a substantial burden of illness. The frequency of both diagnosed diabetes and diagnosed hypertension in the same individual was relatively similar, with Indians having a prevalence of 4.0%, Pakistanis having a prevalence of 4.2%, and Bangladeshis having a prevalence of 3.8%. This compared to the 1998 English white adult population prevalence of 1.5% for individuals having been diagnosed with both conditions.
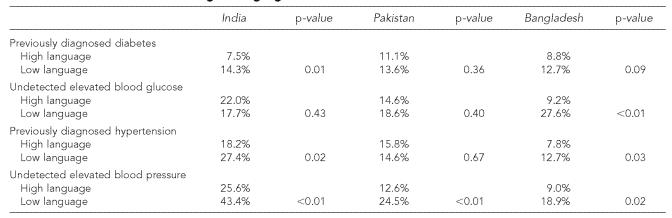
Table 3 shows that in unadjusted analyses, English language skill is associated with having diagnosed disease as well as undetected high-risk conditions. The general trend is that the greater the ethnic minority group’s language skill in English, the lower the prevalence of disease. However, there are individual differences among the ethnic groups that may be masked by collapsing different South Asian groups into one category. For diagnosed diabetes, only one of the three ethnic groups (Indians) demonstrates a statistically significant relationship. When all South Asians are grouped together, a significant relationship is observed, with the prevalence of diagnosed diabetes being 9.1% for individuals with high language skill and 13.3% for individuals with low language skill (p=0.01). In contrast, when considered individually, only one of the three ethnic groups (Bangladeshis) demonstrates a relationship between language and undetected elevated blood glucose. When all South Asians are collapsed into one category, no significant relationship is observed between the prevalence of undetected elevated blood glucose and language skill: 17.0% of individuals with high English language skill and 22.4% of individuals with low English language skill showed undetected elevated blood glucose levels.
Table 3.
Relationship between previously diagnosed diabetes and hypertension and elevated risk markers with English language skill
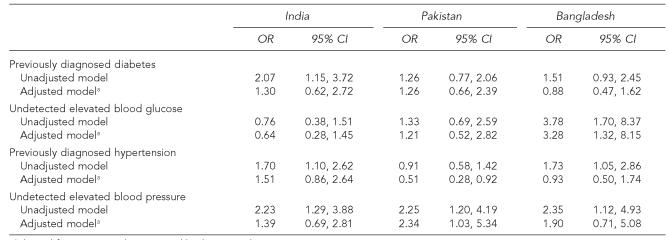
The results shown in Table 4 indicate that for certain conditions, language is associated with disease burden even after controlling for potential confounders. Although diagnosed diabetes and hypertension have some ethnic-specific relationships with language in unadjusted analyses, these are no longer significant in adjusted analyses. However, in adjusted analyses, language was significantly associated with undetected elevated blood glucose among Bangladeshis and undetected elevated blood pressure among Pakistanis.
Table 4.
Unadjusted and adjusted likelihood of having diagnosed diabetes or hypertension or undetected risk for diabetes or hypertension by English language skills among foreign-born South Asians
Adjusted for age, sex, education, and body mass index
OR = odds ratio
CI = confidence interval
DISCUSSION
Our findings indicate that important differences exist among South Asian ethnic groups and that treating them as a homogenous group may be misleading and obscure differences between the subgroups. This supports previous work that has found heterogeneity in South Asian subgroups in blood pressure.23 In addition, proficiency in English seems to have an important association with the detection of disease. This is further suggested by the greater prevalence of detected and undetected disease among young foreign-born South Asian adults compared to those born in the UK. For ethnic groups that have language and cultural differences from the majority English-speaking population, ensuring cultural competence among providers seems to be warranted.
Our findings suggest a relationship between English language skill and diabetes and hypertension among South Asian groups. Health beliefs and practices are integrated into ethnic and cultural orientation,24–26 and include different explanatory models of illness.27,28 Patients’ understanding of symptoms and the need for detection of relatively insidious conditions including diabetes and hypertension is particularly important.29 Cultural practices and health beliefs play a role in a proper understanding of disease and appropriate health care usage. If these beliefs and knowledge are inconsistent with the prevailing culture, the minority group may be at greater risk for disease. Consequently, being able to convey appropriate information to patients and help them become more health literate is a crucial role for the physician, particularly with patients of low educational attainment, immigrants, and racial and ethnic minorities.30
These findings have implications for the care of the South Asian community in the United Kingdom. If the amount of diagnosed diabetes and the amount of undetected elevated blood glucose are combined to indicate the total diabetes burden in the foreign-born Bangladeshi population, 27% of adults are affected. Moreover, low English language skill was significantly associated with undetected elevated blood glucose among Bangladeshis. Focused policies on diabetes detection within South Asian communities may therefore be warranted.
There are several limitations to this study. The data are cross-sectional, which limits the ability to make inferences about causality. Consequently, we can only present associations between language and disease. Second, the present measures of undetected elevated blood glucose and elevated blood pressure do not conform to strict diagnostic criteria for undetected diabetes or hypertension. Nevertheless, from a public health perspective, they do indicate a high potential for disease. Third, the measure of English language skills included in the HSE was relatively crude. However, general assessments of language proficiency or language use have commonly been used in studies of acculturation and health.31,32
For countries such as the U.S. and the UK, where immigration of ethnic minority populations has increased rapidly in recent decades, awareness of language and cultural differences from the majority English-speaking population and ensuring cultural competence among providers seems to be warranted. The findings also have substantial implications beyond the UK and suggest that even within a “single” ethnic group, there are differences in disease prevalence and complications and access to health care. These differences are likely to be wider between ethnic groups but this remains to be tested in further research. Moreover, language barriers may be an important influence on health status and further research (both quantitative and qualitative) is needed to understand these barriers and how they might impact health status and access to health care.33
In conclusion, this study points to the importance of within-group differences among foreign-born South Asian adults in England. Health policy and planning initiatives should be aware of differences between ethnic communities that may previously have been considered a unified whole. Language as a barrier to health care for ethnic minorities requires that the health system focus on culturally sensitive health services and better outreach to minority groups.
Footnotes
This project was supported in part by grants 1R21DK66066A1 and 1R21DK067130 f rom the National Institute of Diabetes and Digestive and Kidney Diseases and by grant 1P30AG021677 from the National Institute on Aging.
REFERENCES
- 1.Office of National Statistics (UK) Population of the United Kingdom: by ethnic group. 2001. Apr, [cited 2005 Feb 20]. Available from: URL: http://www.statistics.gov.uk/CCI/nugget.asp?ID=455&Pos=4&ColRank=2&Rank=1000.
- 2.Secretary of State for Health (UK) Putting people at the heart of public services. Cm 6268. London: Department of Health; 2004. The NHS improvement plan. [Google Scholar]
- Bloche MG. Race-based therapeutics. N Engl J Med. 2004;351:2035–7. doi: 10.1056/NEJMp048271. [DOI] [PubMed] [Google Scholar]
- 4.Gill PS, Kai J, Bhopal RS, Wild S. Health care needs assessment: black and minority ethnic groups. In: Raftery J, Stevens A, Mant J, editors. Health care needs assessment. 3rd series. Abingdon (UK): Radcliffe Medical Press; [cited 2006 Feb 20]. Available from: URL: http://hcna.radcliffe-oxford.com/bemgframe.htm. In press 2006. [Google Scholar]
- 5.Bhopal R, Unwin N, White M, Yallop J, Walker L, Alberti KG, et al. Heterogeneity of coronary heart disease risk factors in Indian, Pakistanis, Bangladeshi, and European origin populations: cross sectional study. BMJ. 1999;319:215–20. doi: 10.1136/bmj.319.7204.215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Karter AJ, Ferrara A, Darbinian JA, Ackerson LM, Selby JV. Self-monitoring of blood glucose: language and financial barriers in a managed care population with diabetes. Diabetes Care. 2000;23:477–83. doi: 10.2337/diacare.23.4.477. [DOI] [PubMed] [Google Scholar]
- 7.Fiscella K, Franks P, Doescher MP, Saver BG. Disparities in health care by race, ethnicity, and language among the insured: findings from a national sample. Medical Care. 2002;40:52–9. doi: 10.1097/00005650-200201000-00007. [DOI] [PubMed] [Google Scholar]
- 8.Schur CL, Albers LA. Language, sociodemographics, and health care use of Hispanic adults. J Health Care Poor Underserved. 1996;7:140–58. doi: 10.1353/hpu.2010.0024. [DOI] [PubMed] [Google Scholar]
- 9.Flores G, Fuentes-Afflick E, Barbot O, Carter-Pokras O, Claudio L, Lara M, et al. The health of Latino children: urgent priorities, unanswered questions, and a research agenda. JAMA. 2002;288:82–90. doi: 10.1001/jama.288.1.82. [published erratum appears in JAMA 2003;290:756] [DOI] [PubMed] [Google Scholar]
- 10.Mainous AG., 3rd Self-concept as an indicator of acculturation in Mexican Americans. Hispanic J Behavioral Sciences. 1989;11:178–89. [Google Scholar]
- 11.Griffith J. Relationship between acculturation and psychological impairment in adult Mexican Americans. Hispanic J Behavioral Sciences. 1983;5:431–59. [Google Scholar]
- 12.Nesdale D. Acculturation attitudes and the ethnic and host-country identification of immigrants. J Applied Social Psychol. 2002;32:1488–507. [Google Scholar]
- 13.Koopman RJ, Mainous AG, 3rd, Baker R, Gill JM, Gilbert GE. Continuity of care and recognition of diabetes, hypertension and hypercholesterolemia. Arch Intern Med. 2003;163:1357–61. doi: 10.1001/archinte.163.11.1357. [DOI] [PubMed] [Google Scholar]
- 14.Mainous AG, 3rd, Koopman RJ, Gill JM, Baker R, Pearson WS. The relationship between continuity of care and diabetes control: evidence from the Third National Health and Nutrition Examination Survey. Am J Public Health. 2004;94:66–70. doi: 10.2105/ajph.94.1.66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rohlfing CL, Little RR, Wiedmeyer HM, England JD, Madsen R, Harris MI, et al. Use of GHb (HbA1C) in screening for undiagnosed diabetes in the U.S. population. Diabetes Care. 2000;23:187–91. doi: 10.2337/diacare.23.2.187. [DOI] [PubMed] [Google Scholar]
- 16.Peters AL, Davidson MB, Schriger DL, Hasselblad V. A clinical approach for the diagnosis of diabetes mellitus: an analysis using glycosylated hemoglobin levels. JAMA. 1996;276:1246–52. [published erratum appears in JAMA 1997;277:1125] [PubMed] [Google Scholar]
- 17.Davidson MB, Schriger DL, Peters AL, Lorber B. Revisiting the oral glucose tolerance test criterion for the diagnosis of diabetes. J Gen Intern Med. 2000;15:551–5. doi: 10.1046/j.1525-1497.2000.08024.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hanson R, Nelson R, McCance D, Beart JA, Charles MA, Pettitt DJ, et al. Comparison of screening tests for non-insulin-dependent diabetes mellitus. Arch Intern Med. 1993;153:2133–40. [PubMed] [Google Scholar]
- 19.Diabetes Control and Complications Trial Research Group. The relationship of glycemic exposure (HbA1c) to the risk of development and progression of retinopathy in the Diabetes Control and Complications Trial. Diabetes. 1995;44:968–83. [PubMed] [Google Scholar]
- 20.Diabetes UK. Second edition, revised. London: Diabetes UK; 2000. Recommendations for the management of diabetes in primary care. [Google Scholar]
- 21.Ramsay LE, Williams B, Johnston GD, MacGregor GA, Poston L, Potter JF, et al. British Hypertension Society guidelines for hypertension management 1999: summary. BMJ. 1999;319:630–5. doi: 10.1136/bmj.319.7210.630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.National Institutes of Health. Expert Panel on the Identification Evaluation and Treatment of Overweight and Obesity in Adults . Washington: National Institutes of Health; 1998. Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults: the evidence report. NIH Publication No. 98-4083. [PubMed] [Google Scholar]
- 23.Agyemang C, Bhopal RS. Is the blood pressure of South Asian adults in the UK higher or lower than that in European white adults? A review of cross-sectional data. J Hum Hypertens. 2002;16:739–51. doi: 10.1038/sj.jhh.1001488. [DOI] [PubMed] [Google Scholar]
- 24.Kleinman A, Eisenberg L, Good B. Culture, illness, and care: clinical lessons from anthropologic and cross-cultural research. Ann Intern Med. 1978;88:251–8. doi: 10.7326/0003-4819-88-2-251. [DOI] [PubMed] [Google Scholar]
- 25.Pachter LM. Culture and clinical care: folk illness beliefs and behaviors and their implications for health care delivery. JAMA. 1994;271:690–4. doi: 10.1001/jama.271.9.690. [DOI] [PubMed] [Google Scholar]
- 26.Fishman BM, Bobo L, Kosub K, Womeodu RJ. Cultural issues in serving minority populations: emphasis on Mexican Americans and African Americans. Am J Med Sci. 1993;306:160–6. doi: 10.1097/00000441-199309000-00006. [DOI] [PubMed] [Google Scholar]
- 27.Poss JE, Jezewski MA, Stuart AG. Home remedies for type 2 diabetes used by Mexican Americans in El Paso, Texas. Clin Nurs Res. 2003;12:304–23. doi: 10.1177/1054773803256872. [DOI] [PubMed] [Google Scholar]
- 28.Holt CL, Lukwago SN, Kreuter MW. Spirituality, breast cancer beliefs and mammography utilization among urban African American women. J Health Psychol. 2003;8:383–96. doi: 10.1177/13591053030083008. [DOI] [PubMed] [Google Scholar]
- 29.Schorling JB, Saunders JT. Is “sugar” the same as diabetes? A community-based study among rural African-Americans. Diabetes Care. 2000;23:330–4. doi: 10.2337/diacare.23.3.330. [DOI] [PubMed] [Google Scholar]
- 30.American Medical Association; Ad Hoc Committee on Health Literacy for the Council on Scientific Affairs. Health literacy: a report of the Council on Scientific Affairs. JAMA. 1999;281:552–7. [PubMed] [Google Scholar]
- 31.Adam MB, McGuire JK, Walsh M, Basta J, LeCroy C. Acculturation as a predictor of the onset of sexual intercourse among Hispanic and white teens. Arch Pediatr Adolesc Med. 2005;159:261–5. doi: 10.1001/archpedi.159.3.261. [DOI] [PubMed] [Google Scholar]
- 32.Himmelgreen DA, Perez-Escamilla R, Martinez D, Bretnall A, Eells B, Peng Y, et al. The longer you stay, the bigger you get: length of time and language use in the U.S. are associated with obesity in Puerto Rican women. Am J Phys Anthropol. 2004;125:90–6. doi: 10.1002/ajpa.10367. [DOI] [PubMed] [Google Scholar]
- 33.Greenhalgh T, Collard A, Begum N. Sharing stories: complex intervention for diabetes education in minority ethnic groups who do not speak English. BMJ. 2005;330:628. doi: 10.1136/bmj.330.7492.628. [DOI] [PMC free article] [PubMed] [Google Scholar]