Abstract
Objectives
We sought to determine whether literacy mediates the relationship between education and glycemic control among diabetes patients.
Methods
We measured educational attainment, literacy using the Short Test of Functional Health Literacy in Adults (s-TOFHLA), and glycemic control (HbA1c) in 395 diabetes patients at a U.S. public hospital. We performed path analysis to compare two competing models to explain glycemic control. The direct effects model estimated how education was related to HbA1c; the mediational model estimated the strength of the direct relationship when the additional pathway from education to literacy to HbA1c was added.
Results
Both the model with a direct effect of education on HbA1c and the model with literacy as a mediator were supported by good fit to observed data. The mediational model, however, was a significant improvement, with the additional path from literacy to HbA1c reducing the discrepancy from observed data (p<0.01). After including this path, the direct relationship between education and HbA1c fell to a non-significant threshold.
Conclusions
In a low-income population with diabetes, literacy mediated the relationship between education and glycemic control. This finding has important implications for both education and health policy.
While the association between education and health is well established and is robust across health conditions and outcomes,1–6 the paths by which education influences health require further elucidation. There are a number of competing theories regarding mediators in this relationship, including, but not limited to (1) work, economic, and environmental conditions; (2) social-psychological resources; and (3) health behaviors.7,8 Notably, relatively little attention has been paid to how educational differences can affect health through interactions with the health care system. In this context, literacy may be particularly important. Recently, researchers and policymakers have highlighted the gap between the literacy demands placed on individuals in the health care context and individuals’ capacity to optimally function in these settings, or “health literacy.”9–11 With the demonstration of the wide variation in literacy skills in industrialized nations,12,13 some have suggested that this variation might explain some of the disparities in health attributed to socioeconomic status, including educational attainment.14–16 While literacy may be an important explanatory variable in the relationship between education and health, this hypothesis has not been formally tested. Were literacy a mediator in the relationship between education and health, the implications for both education policy and health policy would be significant.17
“Health literacy” has been defined as a measure of an individuals’ ability to perform basic reading and numerical tasks required to optimally function in the health care environment,18 and more broadly as the degree to which individuals have the capacity to obtain, process, and understand basic health information and services needed to make appropriate health decisions.9,19 Current measures of health literacy are highly correlated with standard measures of general literacy.20–22 Inadequate literacy has been found to be associated with demographic characteristics and markers of socioeconomic status, such as older age, non-White race/ethnicity, immigrant status, and lower educational attainment and income.9,12,23 While literacy has been shown to be a robust determinant of health in developing nations,24 its influence may not be limited to non-industrialized countries. Studies in the U.S. have demonstrated that literacy is independently associated with self-rated health,25,26 risk of hospitalization,27 knowledge of self-management practices,28,29 and metabolic control in adult-onset (type 2) diabetes.30
To assess whether literacy can explain the relationship between education and health outcomes, we studied an ethnically diverse population of patients with type 2 diabetes cared for in a public health system. We selected diabetes for a number of reasons. First, from a research perspective, diabetes is unique in having a readily available laboratory test of glycemic (blood sugar) control (HbA1c), an intermediate outcome that strongly influences health trajectory in diabetes and a standard measure in clinical practice.31,32 Second, because diabetes self-management demands require active participation by patients, interactive communication with health providers, and successful navigation of the health care system,33 diabetes is an ideal model for identifying mediators between education and health in the chronic disease context.34 Third, the association between education and diabetes outcomes is consistent across a number of outcomes, including self-management practices,34,35 glycemic control, diabetes complications,36,37 and mortality.38,39 Finally, because the educational gradient in diabetes prevalence is well established,40,41 examining mediators between education and diabetes-specific outcomes could have significant public health implications.2,17
METHODS
Study sample
Details regarding the study participants, recruitment procedures, and interview process have been previously described.30,42 Study participants were recruited in 2000 from two primary care clinics at San Francisco General Hospital (SFGH), the public hospital for the City and County of San Francisco. A high proportion of individuals cared for at SFGH have incomes below the federal poverty level, are first-generation immigrants to the United States, and are publicly insured or uninsured. SFGH primary care clinic patients receive care from University of California, San Francisco (UCSF) attending faculty and residents. Clinics have diabetes educators available for individual consultation with patients. At the time of the study, there was no systematic diabetes disease management system in place.
Potential study participants were identified from the hospital’s administrative and clinical computerized database. Patients were eligible if they had visited one of the two primary care clinics in the prior 12 months, had at least one visit to a primary care physician in the prior six months, and had a recorded hemoglobin A1c (HbA1c) in the database. Participation was restricted to individuals older than 30 years, who spoke either English or Spanish fluently, and had type 2 diabetes as determined by a billing ICD-9 code of 250.XX.43 Patients with a diagnosis of end-stage renal disease, psychotic disorder, dementia, or blindness were excluded because these conditions can interfere with accurate literacy measurement.20
Between June and December 2000, bilingual research assistants approached all eligible patients who attended a clinic appointment. Individuals were offered $5.00 to participate in a study of diabetes and doctor/patient communication. Informed consent was obtained from participants by explaining the study verbally and handing out an informed consent statement written at a fifth-grade reading level. Individuals who agreed to participate were tested with a pocket vision screener to ensure that their corrected visual acuity was better than 20/100. Those with acceptable vision completed a measure of literacy and were administered the study questionnaire in either English or Spanish. The protocol was approved by the UCSF Human Subjects Committee.
Measures
Background information
Data collection involved oral administration of a 45-minute questionnaire that included socio-demographic information, including age, gender, race/ethnicity, marital status, employment, and health insurance status. Educational attainment was assessed by asking patients to choose their highest educational level completed from the following choices: 8th grade or less; some high school; high school graduate or GED; some college or technical school; and college graduate or graduate degree. For our analyses, patients were grouped into one of three education categories: less than high school graduate, high school graduate or GED, and technical school or college attendance or graduation. While our original sample included 408 subjects, there were too few (n=13) with graduate or professional degrees to examine them as a unique level, and due to insufficient power, these subjects were excluded, leaving a sample of 395 patients. Questions queried how well individuals speak and read English. While all subjects spoke either English or Spanish fluently, we categorized patients who answered “no English,” or “more Spanish [or preferred language] than English” to both questions as speaking a primary language other than English.44 We also administered an eight-item social-support inventory adapted from the Diabetes Care Profile45 that asks subjects to rate the extent to which family or friends support their diabetes self-care.
Literacy
Participants completed, in English or Spanish, the Short Test of Functional Health Literacy in Adults (s-TOFHLA), a reliable, validated measure of literacy in the health care context.20,46 The abbreviated s-TOFHLA is a 36-item timed reading comprehension test that uses the modified Cloze procedure;47 every fifth to seventh word in a passage is omitted, requiring individuals to select the likely word from four multiple-choice options. The measure includes two health care passages written in 14-point type. One passage involves instructions for preparing an upper gastrointestinal tract radiograph series (Gunning-Fog Index readability grade 4.3)48 and the other is a portion of the “Rights and Responsibilities” section from a Medicaid application (Gunning-Fog Index readability grade 10.4).49 Participants received a score ranging from 0 to 36, with higher values representing greater literacy.
Health outcomes
We obtained each subject’s most recent HbA1c value from the SFGH database. HbA1c, a measure of patients’ glycemic control over an approximately three-month period, has been demonstrated to be a robust indicator of health status, as well as a predictor of health care utilization, costs, and disease trajectory.2,50,51 Ninety-eight percent of HbA1c values were obtained within 12 months before the patient interview. SFGH uses ion-exchange chromatography52 to measure HbA1c. To correct for the non-normal distribution of HbA1c data, analyses incorporated log-transformed HbA1c values.
Statistical analyses
We employed path analysis to empirically investigate if literacy might act as a factor mediating the relationship between educational level and glycemic control. An extension of more familiar multiple regression approaches, path analysis utilizes structural equation modeling techniques with measured variables.53 Investigators first specify models based on expected relationships between variables and then compare the extent to which observed relationships between variables “fit” those that would be expected based on the model. This approach considers how much of the variation in the data can be explained by expected relationships in the model and how this finding compares to what one would find using a model based on chance relationships between variables. Path analysis is a powerful analytic tool permitting the simultaneous estimation of both direct and indirect influences on outcomes,53 enabling comparison of the explanatory power of competing models and observation of mediational effects by examining changes in the strength of variable relationships across models. For our purposes, we were interested in exploring whether including literacy as a potential mediator in the model reduces the initial education/health relationship and reduces uncertainty in the model.
Path analysis generates estimated path coefficients, or standardized linear regression coefficients, reflecting standardized effect size values based on the variance accounted for by the specific relationship between variables within the model. Specifically, standardized path estimates reflect the extent to which a one standard deviation unit change in a predictor variable is associated with the corresponding standard deviation change for an outcome variable. Significance is determined by dividing the estimates by their standard estimates and using a t-test. Path analysis was conducted using LISREL 8.54 software.54
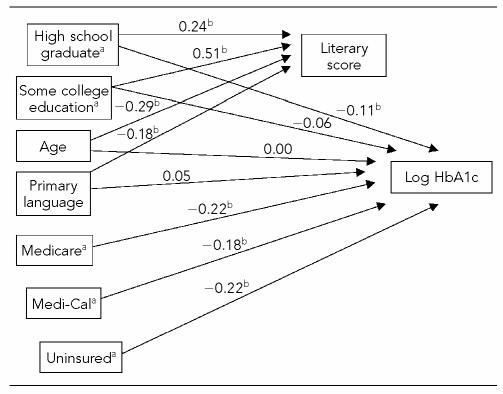
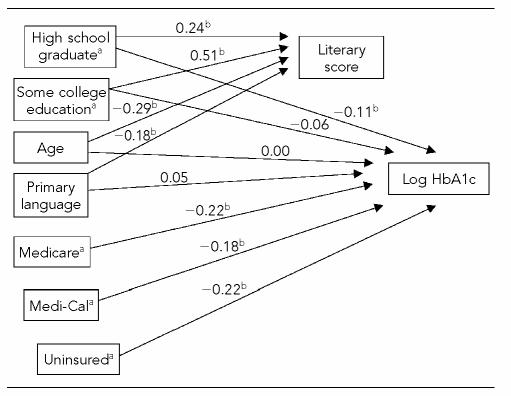
Our analyses compared two competing models—a direct effects model and a mediational model—to explain patients’ glycemic control (levels of HbA1c). The direct effects model estimated how measured educational attainment was related to HbA1c (Figure 1; note that in this model, there is no line [path] to allow expression of any relationship between literacy scores and HbA1c). The mediational model estimated the strength of the direct relationship between educational attainment and HbA1c when the additional pathway from literacy to HbA1c was added into the model (Figure 2; note that in this model, there is a line [path] to allow expression of a relationship between literacy scores and HbA1c).
Figure 1.
Path analytic model testing the direct effect of educational attainment levels on log-transformed HbA1c values in low-income adults with diabetes
a Categorical variables with more than two levels include a referent group. For education, the referent group is those having less education than a high school diploma. For insurance, the referent group is having private insurance.
b Indicates statistical significance based on t-test p values <0.05. Values shown represent standardized path estimates such that a one standard deviation unit change in a predictor variable is associated with the corresponding path value proportion of a standard deviation change for either literacy score or log HbA1c.
Figure 2.
Path analytic model testing the mediational effect of educational attainment levels on log-transformed HbA1c values via literacy among low-income adults with diabetes
a Categorical variables with more than two levels include a referent group. For education, the referent group is those having less education than a high school diploma. For insurance, the referent group is having private insurance.
b Indicates statistical significance based on t-test p values <0.05. Values shown represent standardized path estimates such that a one standard deviation unit change in a predictor variable is associated with the corresponding path value proportion of a standard deviation change for either literacy score or log HbA1c.
Several other variables related to socioeconomic status expected to influence HbA1c and/or literacy were also included in each of the models. Both the direct effects and the mediational models included relationships between health insurance and HbA1c because insurance is a powerful enabler of access to diabetes health care providers and medications.55 Individual income was not included in the model because there was insufficient variation among this low-income sample and because it likely represents an endogenous variable. The relationships of individual age and immigration status both to literacy and to HbA1c were also controlled because they might serve as confounding explanatory mechanisms. All exogenous variables were permitted to correlate with one another in the model.
Analyses tested the extent to which the direct effects model fit the observed data. Specifically, the observed covariance matrix detailing relationships among variables was compared to what would have been expected given the set of interrelationships depicted in the hypothesized model. After estimating fit for the direct effects model, this process was repeated to investigate the fit of the mediating model to the data. In path analyses, models that explain the observed data well have few discrepancies between expected and observed covariances, resulting in low, non-significant, chi-square values. To compare the overall fit observed between the two competing models, a chi-square difference test was conducted to evaluate if, given the degrees of freedom used for each model, the mediational model results in significantly lower chi-square values (i.e., better fit to observed data) than the direct effects model. We hypothesized that, while both models might adequately fit the observed data, the mediational model would provide greater explanatory power and attenuate the direct relationship between education and glycemic control when compared to the results of the direct effects model.
To gain a more complete understanding of relationships between variables and to perform sensitivity analyses, we also tested alternative models. These included a model in which literacy completely mediated the relationship between education and glycemic control (i.e., no path was included from education directly to HbA1c) and a model in which we included race/ethnicity and social support variables.56
RESULTS
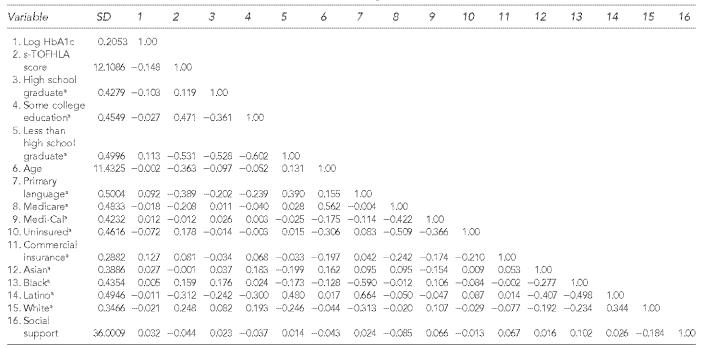
Study patients represented a low-income population and were racially and ethnically diverse (Figure 3). Most were publicly insured or had no health insurance. Patients had educational attainment that ranged from less than a high school graduate (47%), high school graduate or GED (24%), and some college or technical school (29%). The mean score on the s-TOFHLA was 21 out of 36, and the mean HbA1c was 8.5%. The correlation matrix and the standard deviations used for path analyses are shown in Table 1.
Figure 3.
Characteristics of study patients (N=395)
SD = standard deviation
s-TOFHLA = Short Test of Functional Health Literacy in Adults
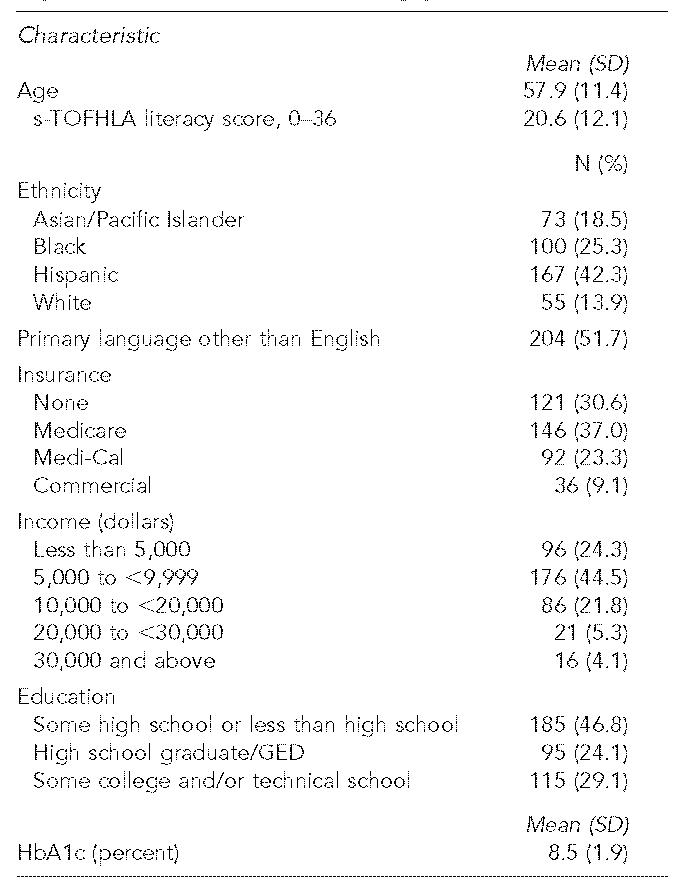
Table 1.
Correlation matrix and standard deviations used in analyses
Dummy coded variables where 1=presence of characteristic and 0=lack of characteristic
SD = standard deviation
s-TOFHLA = Short Test of Functional Health Literacy in Adults
Direct effects model
The conceptual model displaying a direct effect of educational attainment levels on HbA1c was supported (Figure 1; note the absence of a path from literacy to HbA1c). The normal theory least squares chi-square for the overall model (degrees of freedom [DF]=32, n=395) was 19.62 (p=0.96), indicating that the model fit the data well. There was no statistically significant discrepancy between the covariance matrix observed from the sample and the estimated matrix based on the conceptual model of relationships between variables. Other indicators of model fit also supported the effectiveness of this conceptual model. The root mean square error of approximation (RMSEA)57 was 0.0, suggesting exact model fit.58 The adjusted goodness of fit index (AGFI) and comparative fit index (CFI) also were 0.99 and 1.0 respectively, further supporting a close model fit.
Figure 1 shows the estimated path coefficients, reflecting standardized effect size values based on the variance accounted for by the specific relationship between variables within the model. In this model, path coefficient estimates revealed significant relationships between educational attainment and HbA1c, particularly at lower educational levels. Individuals with a high school degree had statistically significantly better glycemic control than those with less education. While a similar relationship was observed for individuals with some college education, the strength of the association did not reach significance. These effects were noted despite the inclusion of other variables related to socioeconomic status, including age, immigration status, and type of health insurance. Because the standardized path estimates shown in Figure 1 do not lend themselves to clinical interpretation, we calculated non-standardized estimates with raw HbA1c as the outcome. Compared to less than a high school education, completion of high school and college education was associated with an absolute difference in HbA1c of –0.45 and –0.22, respectively.
Mediational effects model
The mediational effects model (Figure 2) included literacy as a mediator between educational attainment and HbA1c levels, with an additional path to estimate the relationship between literacy and HbA1c. The same potentially confounding variables related to demographic and socioeconomic status (age, immigrant status, and health insurance type) included in the direct effects model remained in the mediational effects model. The conceptual model with literacy mediating the relationship of educational attainment on HbA1c also was supported by good fit to observed data. The normal theory least squares chi-square for the overall model (df=31, n=395) was 12.22 (p=0.999), indicating the model fit the data well. Other indicators also supported the effectiveness of model fit (RMSEA<.0001, AGFI=0.99, CFI=1.0).
Individual path estimates (Figure 2; note the presence of a path from literacy to HbA1c) showed a statistically significant relationship between literacy and HbA1c such that individuals with higher literacy had better glycemic control. This effect was independent of education or the other control variables. In addition, when literacy was modeled as a mediator, direct relationships between educational attainment levels and HbA1c were attenuated, with the previously significant association of high school graduate with HbA1c becoming non-significant. To enable clinical interpretation, we calculated non-standardized path estimates with raw HbA1c as the outcome. Comparing the extremes of literacy scores demonstrated a difference in HbA1c value of –0.88. In this mediated model, compared to less than a high school education, completion of high school and college education was associated with a non-significant absolute difference in HbA1c of –0.28 and 0.11, respectively.
Model comparisons
Since both the direct effects model and the mediational model displayed effective overall model fit, we used a chi-square difference test to compare the extent to which the observed data fit each of these nested conceptual models. The mediational model was a significant improvement over the direct effects model, with the additional path from literacy to HbA1c reducing the discrepancy from the observed data (chi-square difference test=7.40, df=1, p< .01).
Alternative model considerations
Although initial conceptual models fit the observed data effectively without modifications, alternative models were tested to gain a more complete understanding of relationships between variables. We tested an alternative model in which relationships between educational levels and HbA1c were fully mediated through literacy. In this model, there were no direct paths from education to HbA1c, but the path from literacy to HbA1c was included. Consistent with previous models,56 age, immigration status, and type of health insurance continued to be included in this analysis. Overall, this full mediational model also fit the data well (chi-square [df=33, n=395]=14.95, p=0.997; RMSEA= 0.0, AGFI=0.99, CFI=1.0). The path from literacy to HbA1c retained a significant relationship such that higher levels of literacy resulted in lower HbA1c levels (better glycemic control). A chi-square difference test revealed that use of this more parsimonious model relying on full mediation did not result in significantly greater discrepancies from the observed data than the partial mediation model shown in Figure 2 (chi-square difference=2.73, df=2, p=0.26). However, like the model in Figure 2, the full mediational model significantly reduced discrepancies from the observed data when compared with the direct effects model in Figure 1 (chi-square difference=4.67, df=1, p =0.03). In sum, the inclusion of the path from literacy to HbA1c was critical for improving model fit. When the literacy/HbA1c path was in the model, the inclusion of a direct path from educational attainment to HbA1c did not result in significantly better model fit.
Alternative models that included race/ethnicity, dummy coded for each type, models that coded ethnicity dichotomously as white/non-white, and models that included social support as a continuous variable were also tested. In each case, paths between educational attainment levels, literacy, and HbA1c did not vary in significance or direction from the results presented herein. Likewise, model comparisons yielded similar findings about the fit of conceptual models. For parsimony, results presented here have excluded race/ethnicity and social support variables.
DISCUSSION
To our knowledge, this study is the first to examine the extent to which literacy may be a mediator in the relationship between education and health outcomes. Similar to others,36 we found that educational attainment was associated with better glycemic control, particularly when comparing the two lower strata of education (less than high school graduate vs. high school graduate). The differences observed were both statistically and clinically significant. We also demonstrated that the inclusion of literacy as a mediator attenuated the direct effects of education on glycemic control to non-significant levels, while the path between literacy and glycemic control was both statistically and clinically significant. Furthermore, comparison of model fits demonstrated that the adoption of a mediational model resulted in significant improvement over the direct effects model. These results suggest that in a population of low-income, ethnically diverse patients with diabetes, literacy at least partially mediates the observed relationship between education and glycemic control.
Literacy could mediate the effects of education on glycemic control through a number of mechanisms. Individuals with inadequate literacy have been shown to have problems with both written and oral forms of communication in the clinical context.42,59–62 Since successful diabetes care involves interactive communication,63 participatory decision-making,64 and activation of patients with regard to self-care65 and goal-setting, those with inadequate literacy may be less prepared and poorly supported to care for their condition.28 In addition, given the self-management demands of contemporary diabetes care,66 individuals with inadequate literacy may find the diabetes self-care regimen overwhelming or unrealistic, particularly when the literacy demands intrinsic to navigating a complex health care system are also substantial.67 It is also possible that inadequate literacy is a marker for unmeasured factors at the individual level (such as personality, cognitive resources,34,68 sense of control, and socioeconomic status69) or at the neighborhood or community level (such as community empowerment or availability of goods and services that facilitate better health).70
There are a number of limitations to this study. First, the cross-sectional design does not allow us to infer that any associations were causal. In addition to unmeasured confounding, it is possible that the association between literacy and glycemic control is a consequence of reverse causation, e.g. that poor glycemic control leads to poor performance on tests of literacy71,72 and that inadequate literacy may itself reflect the trajectory of chronic disease.73 Second, we only modeled the relationships between education, literacy, and glycemic control—an intermediate health outcome. While we were underpowered to evaluate more distal outcomes, glycemic control is closely linked to symptom burden, self-rated health,74 long-term complication rates, and mortality among diabetics.32 Third, selecting a low-income population with diverse educational experiences and access to ongoing primary care necessitates that our findings be corroborated in other settings. Fourth, measures of educational attainment may have inconsistent reliability and validity across diverse populations, reflecting heterogeneous educational experiences,75 whereas literacy tests may more precisely reflect educational attainment. Finally, the lack of variation in income and access to care in our sample mitigated our ability to test the competing mediational effects of economic resources and access to care on glycemic control.1,76
Were our results to be replicated with other populations, in different settings, and across health conditions and outcomes, the implications for reducing health disparities related to the gradient in socioeconomic status would be great. Mediation suggests that education operates in part by improving literacy. From the perspective of national education policy, identifying a link between education and health that is mediated by an outcome for which the educational system is accountable may allow for more vigorous, multilateral support for investment in childhood and adult basic education. Improving the quality of the educational experience and ensuring equity in the degree to which educational systems assist individuals in attaining literacy skills could generate long-term public health dividends. Embedding literacy and health education instruction into education curricula may also prove beneficial.9,77 From the health policy perspective, as the expanding self-management66 and self-advocacy demands placed on individuals in complex, technology-oriented health systems require greater levels of oral, written, and computer literacy, our results could serve as a warning that educational disparities in chronic disease care may widen over time.9 On the other hand, our results suggest an opportunity may exist within health systems to reduce education-related disparities in outcomes by altering processes of care, tailoring health education, and simplifying navigation to better accommodate the literacy levels of the populations they serve. A small body of evidence suggests that such approaches could reduce or even eliminate education- and literacy-related disparities in the chronic disease context.33,34,78,79 It has been estimated that between one-third and one-half of individuals with type 2 diabetes have inadequate or marginal literacy skills.30,40 Future work should attempt to characterize those attributes of health systems and clinician-patient relationships that reduce literacy-related disparities and develop policy initiatives to more consistently embed such practices into health promotion activities and health care delivery.80
Acknowledgments
Dr. Schillinger was supported by a NIH Mentored Clinical Scientist Award K-23 RR16539-03. Electronic data were made available through the San Francisco General Hospital GCRC grant M01RR00083-42. Additional support was provided by NIMH training grant T32 MH 0l9391 (Dr Barton); R01 HD46113-01 (Dr. Karter), and the John D. and Catherine T. MacArthur Foundation Research Network on SES and Health (Dr. Adler).
REFERENCES
- 1.Backlund E, Sorlie PD, Johnson NJ. A comparison of the relationships of education and income with mortality: the National Longitudinal Mortality Study. Soc Sci Med. 1999;49:1373–84. doi: 10.1016/s0277-9536(99)00209-9. [DOI] [PubMed] [Google Scholar]
- 2.Sorlie PD, Backlund E, Keller JB. US mortality by economic, demographic, and social characteristics: the National Longitudinal Mortality Study. Am J Public Health. 1995;85:949–56. doi: 10.2105/ajph.85.7.949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Winkleby MA, Jatulis DE, Frank E, Fortmann SP. Socioeconomic status and health: how education, income, and occupation contribute to risk factors for cardiovascular disease. Am J Public Health. 1992;82:816–20. doi: 10.2105/ajph.82.6.816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Adler NE, Newman K. Socioeconomic disparities in health: pathways and policies. Health Aff (Millwood) 2002;21:60–76. doi: 10.1377/hlthaff.21.2.60. [DOI] [PubMed] [Google Scholar]
- 5.Marmot M. The influence of income on health: views of an epidemiologist. Health Aff (Millwood) 2002;21:31–46. doi: 10.1377/hlthaff.21.2.31. [DOI] [PubMed] [Google Scholar]
- 6.Huisman M, Kunst AE, Bopp M, Borgan JK, Borrell C, Costa G, et al. Educational inequalities in cause-specific mortality in middle-aged and older men and women in eight western European populations. Lancet. 2005;365:493–500. doi: 10.1016/S0140-6736(05)17867-2. [DOI] [PubMed] [Google Scholar]
- 7.Ross CE, Wu CL. The links between education and health. American Sociological Review. 1996;60:719–45. [Google Scholar]
- 8.Lantz PM, House JS, Lepkowski JM, Williams DR, Mero RP, Chen J. Socioeconomic factors, health behaviors, and mortality: results from a nationally representative prospective study of U.S. adults. JAMA. 1998;279:1703–8. doi: 10.1001/jama.279.21.1703. [DOI] [PubMed] [Google Scholar]
- 9.Committee on Health Literacy; Nielson-Bohlman L, Panzer AM, Kindig DA, editors. Health literacy: a prescription to end confusion. Washington: Institute of Medicine, Board of Neuroscience and Behavioral Health. National Academies Press; 2004. Apr 8, [PubMed] [Google Scholar]
- 10.Parker R. Health literacy: a challenge for American patients and their health care providers. Health Promot Int. 2000;15:277–83. [Google Scholar]
- 11.Beach MC, Cooper LA, Robinson KA, Price EG, Gary TL, Jenckes MW, et al. Johns Hopkins University Evidence-Based Practice Center. Evidence Report/Technology Assessment Number 90. Rockville (MD): Department of Health and Human Services, Agency for Healthcare Research and Quality; 2004. Strategies for improving minority healthcare quality. AHQR Pub. No. 04-E008-02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kirsch IS, Jungeblut A, Jenkins L, Kolstad A. Adult literacy in America: a first look at the results of the National Adult Literacy Survey. Washington: Department of Education (US), Office of Educational Research and Improvement, National Center for Education Statistics; 1993. [cited 2006 Jan 10]. Also available from: URL: http://nces.ed.gov/pubs93/93275.pdf. [Google Scholar]
- 13.Sum A, Kirsch I, Taggart R. Policy Information Report. Princeton (NJ): Educational Testing Service; 2002. The twin challenges of mediocrity and inequality: literacy in the U.S. from an international perspective. [Google Scholar]
- 14.Angell M. Privilege and health—what is the connection? N Engl J Med. 1993;329(2):126–7. doi: 10.1056/NEJM199307083290210. [DOI] [PubMed] [Google Scholar]
- 15.Weiss BD, Hart G, McGee DL, D’Estelle S. Health status of illiterate adults: relation between literacy and health status among persons with low literacy skills. J Am Board Fam Pract. 1992;5:257–64. [PubMed] [Google Scholar]
- 16.Baker DW. Reading between the lines: deciphering the connections between literacy and health. J Gen Intern Med. 1999;14:315–7. doi: 10.1046/j.1525-1497.1999.00342.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Department of Health and Human Services (US) Understanding and improving health. 2nd ed. Washington: Government Printing Office (US); 2000. [cited 2006 Jan 10]. Healthy People 2010. Also available from: URL: http://www.healthypeople.gov/publications/ [Google Scholar]
- 18.American Medical Association; Ad Hoc Committee on Health Literacy for the Council on Scientific Affairs. Health literacy: report of the Council on Scientific Affairs. JAMA. 1999;281:552–7. [PubMed] [Google Scholar]
- 19.Ratzan SC, Parker RM. Introduction. In: Selden CR, Zorn M, Ratzan SC, Parker RM, editors. Current bibliographies in medicine: health literacy. Bethesda (MD): Department of Health and Human Services (US), Public Health Service, National Institutes of Health, National Library of Medicine; 2000. [Google Scholar]
- 20.Parker RM, Baker DW, Williams MV, Nurss JR. The test of functional health literacy in adults: a new instrument for measuring patients’ literacy skills. J Gen Intern Med. 1995;10:537–41. doi: 10.1007/BF02640361. [DOI] [PubMed] [Google Scholar]
- 21.Davis TC, Long SW, Jackson RH, Mayeaux EJ, George RB, Murphy PW, et al. Rapid estimate of adult literacy in medicine: a shortened screening instrument. Fam Med. 1993;25:391–5. [PubMed] [Google Scholar]
- 22.DeWalt DA, Pignone MP. Reading is fundamental: the relationship between literacy and health. Arch Intern Med. 2005;165:1943–4. doi: 10.1001/archinte.165.17.1943. [DOI] [PubMed] [Google Scholar]
- 23.Sum A, Kirsch I, Yamamoto K. Policy Information Report. Princeton (NJ): Policy Information Center, Educational Testing Service; 2004. A human capital concern: the literacy proficiency of U.S. immigrants. [Google Scholar]
- 24.Grosse RN, Auffrey C. Literacy and health status in developing countries. Annu Rev Public Health. 1989;10:281–97. doi: 10.1146/annurev.pu.10.050189.001433. [DOI] [PubMed] [Google Scholar]
- 25.Baker DW, Parker RM, Williams MV, Clark WS, Nurss J. The relationship of patient reading ability to self-reported health and use of health services. Am J Public Health. 1997;87:1027–30. doi: 10.2105/ajph.87.6.1027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wolf MS, Gazmararian JA, Baker DW. Health literacy and functional health status among older adults. Arch Intern Med. 2005;165:1946–52. doi: 10.1001/archinte.165.17.1946. [DOI] [PubMed] [Google Scholar]
- 27.Baker DW, Gazmararian JA, Williams MV, Scott T, Parker RM, Green D, et al. Functional health literacy and the risk of hospital admission among Medicare managed care enrollees. Am J Public Health. 2002;92:1278–83. doi: 10.2105/ajph.92.8.1278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Williams MV, Baker DW, Honig EG, Lee TM, Nowlan A. Inadequate literacy is a barrier to asthma knowledge and self-care. Chest. 1998;114:1008–15. doi: 10.1378/chest.114.4.1008. [DOI] [PubMed] [Google Scholar]
- 29.Williams MV, Baker DW, Parker RM, Nurss JR. Relationship of functional health literacy to patients’ knowledge of their chronic disease: a study of patients with hypertension and diabetes. Arch Intern Med. 1998;158:166–72. doi: 10.1001/archinte.158.2.166. [DOI] [PubMed] [Google Scholar]
- 30.Schillinger D, Grumbach K, Piette J, Wang F, Osmond D, Daher C, et al. Association of health literacy with diabetes outcomes. JAMA. 2002;288:475–82. doi: 10.1001/jama.288.4.475. [DOI] [PubMed] [Google Scholar]
- 31.Piette JD, Wagner TH, Potter MB, Schillinger D. Health insurance status, cost-related medication underuse, and outcomes among diabetes patients in three systems of care. Med Care. 2004;42:102–9. doi: 10.1097/01.mlr.0000108742.26446.17. [DOI] [PubMed] [Google Scholar]
- 32.UK Prospective Diabetes Study (UKPDS) Group. Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33) Lancet. 1998;352:837–53. [PubMed] [Google Scholar]
- 33.Schillinger D. Health literacy: a prescription to end confusion. Washington: Institute of Medicine; National Academies Press; 2004. Improving chronic disease care for populations with limited health literacy. [Google Scholar]
- 34.Goldman DP, Smith JP. Can patient self-management help explain the SES health gradient? Proc Natl Acad Sci USA. 2002;99:10929–34. doi: 10.1073/pnas.162086599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Karter AJ, Ackerson LM, Darbinian JA, D’Agostino RB, Jr, Ferrara A, Liu J, et al. Self-monitoring of blood glucose levels and glycemic control: the Northern California Kaiser Permanente Diabetes registry. Am J Med. 2001;111:1–9. doi: 10.1016/s0002-9343(01)00742-2. [DOI] [PubMed] [Google Scholar]
- 36.Chaturvedi N, Stephenson JM, Fuller JH. The relationship between socioeconomic status and diabetes control and complications in the EURODIAB IDDM Complications Study. Diabetes Care. 1996;19:423–30. doi: 10.2337/diacare.19.5.423. [DOI] [PubMed] [Google Scholar]
- 37.van der Meer JB, Mackenbach JP. The care and course of diabetes: differences according to level of education. Health Policy. 1999;46:127–41. doi: 10.1016/s0168-8510(98)00058-x. [DOI] [PubMed] [Google Scholar]
- 38.Wilder RP. Education and mortality in type 2 diabetes. Diabetes Care. 2003;26(5):1650. doi: 10.2337/diacare.26.5.1650. [DOI] [PubMed] [Google Scholar]
- 39.Steenland K, Henley J, Thun M. All-cause and cause-specific death rates by educational status for two million people in two American Cancer Society cohorts, 1959–1996. Am J Epidemiol. 2002;156:11–21. doi: 10.1093/aje/kwf001. [DOI] [PubMed] [Google Scholar]
- 40.Cowie CC, Eberhardt MS. Sociodemographic characteristics of persons with diabetes. In: Harris MI, Cowie CC, Reiber G, Boyko E, Stern M, Bennett P, editors. Diabetes in America. 2nd ed. Washington: Government Printing Office (US); 1995. pp. 85–116. [Google Scholar]
- 41.Cooper R, Cutler J, Desvigne-Nickens P, Fortmann SP, Friedman L, Havlik R, et al. Trends and disparities in coronary heart disease, stroke, and other cardiovascular diseases in the United States: findings of the National Conference on Cardiovascular Disease Prevention. Circulation. 2000;102:3137–47. doi: 10.1161/01.cir.102.25.3137. [DOI] [PubMed] [Google Scholar]
- 42.Schillinger D, Bindman A, Stewart A, Wang F, Piette J. Functional health literacy and the quality of physician-patient communication among diabetes patients. Patient Educ Couns. 2004;52:315–23. doi: 10.1016/S0738-3991(03)00107-1. [DOI] [PubMed] [Google Scholar]
- 43.Hart AC, Hopkins CA, editors. International Classification of Diseases, 9th rev., clinical modification. Salt Lake City: Ingenix; 2003. ICD-9-CM expert for physicians, volumes 1 and 2. [Google Scholar]
- 44.Marin G, Sabogal F, Marin BV, Otero-Sabogal R, Perez-Stable EJ. Development of a short acculturation scale for Hispanics. Hisp J Behav Sci. 1987;9:183–205. [Google Scholar]
- 45.Fitzgerald JT, Davis WK, Connell CM, Hess GE, Funnell MM, Hiss RG. Development and validation of the Diabetes Care Profile. Eval Health Prof. 1996;19:208–30. doi: 10.1177/016327879601900205. [DOI] [PubMed] [Google Scholar]
- 46.Baker DW, Williams MV, Parker RM, Gazmararian JA, Nurss J. Development of a brief test to measure functional health literacy. Patient Educ Couns. 1999;38:33–42. doi: 10.1016/s0738-3991(98)00116-5. [DOI] [PubMed] [Google Scholar]
- 47.Taylor WL. “Cloze procedure”: a new tool for measuring readability. Journalism Quarterly. 1953;30:415–33. [Google Scholar]
- 48.Powers RD, Sumner WA, Kearl BE. A recalculation of four adult readability formulas. J Educ Psych. 1958;49:99–105. [Google Scholar]
- 49.Williams MV, Parker RM, Baker DW, Parikh NS, Pitkin K, Coates WC, et al. Inadequate functional health literacy among patients at two public hospitals. JAMA. 1995;274:1677–82. [PubMed] [Google Scholar]
- 50.Wagner EH, Sandhu N, Newton KM, McCulloch DK, Ramsey SD, Grothaus LC. Effect of improved glycemic control on health care costs and utilization. JAMA. 2001;285:182–9. doi: 10.1001/jama.285.2.182. [DOI] [PubMed] [Google Scholar]
- 51.The Diabetes Control and Complications Trial Research Group. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med. 1993;329:977–86. doi: 10.1056/NEJM199309303291401. [DOI] [PubMed] [Google Scholar]
- 52.Bio-Rad Laboratories. DiaSTAT Hemoglobin A1c Analyzer. Hercules (CA): Bio-Rad Laboratories; [cited 2005 Oct 21]. Available from: URL: http://www.bio-rad.com. [Google Scholar]
- 53.Hoyle RH, Smith GT. Formulating clinical research hypotheses as structural equation models: a conceptual overview. J Consult Clin Psych. 1994;62:429–40. doi: 10.1037//0022-006x.62.3.429. [DOI] [PubMed] [Google Scholar]
- 54.LISREL 8: user’s reference guide. Lincolnwood (IL): Scientific Software International Inc; 1996. Scientific Software International. [Google Scholar]
- 55.Piette JD, Wagner TH, Potter MB, Schillinger D. Health insurance status, cost-related medication underuse, and outcomes among diabetes patients in three systems of care. Med Care. 2004;42:102–9. doi: 10.1097/01.mlr.0000108742.26446.17. [DOI] [PubMed] [Google Scholar]
- 56.Brown AF, Ettner SL, Piette J, Weinberger M, Gregg E, Shapiro MF, et al. Socioeconomic position and health among persons with diabetes mellitus: a conceptual framework and review of the literature. Epidemiol Rev. 2004;26:63–77. doi: 10.1093/epirev/mxh002. [DOI] [PubMed] [Google Scholar]
- 57.Steiger JH. Structural model evaluation and modification: an interval estimation approach. Multivariate Behavioral Research. 1990;25:173–80. doi: 10.1207/s15327906mbr2502_4. [DOI] [PubMed] [Google Scholar]
- 58.Brown M, Cudeck R. Alternative ways of assessing model fit. In: Bollen K, Long J, editors. Testing structural equation models. London: Sage; 1993. [Google Scholar]
- 59.Williams MV, Davis T, Parker RM, Weiss BD. The role of health lit-eracy in patient-physician communication. Fam Med. 2002;34:383–9. [PubMed] [Google Scholar]
- 60.Schillinger D, Machtinger E, Wang F, Rodriguez M, Bindman AB. Preventing medication errors in ambulatory care: the importance of establishing regimen concordance. In: Henriksen K, Battles J, Lewin DI, Marks E, editors. Advances in patient safety: from research to implementation Vol. 1, Research findings. Rockville (MD): Agency for Healthcare Research and Quality; 2005. pp. 199–210. [PubMed] [Google Scholar]
- 61.Roter DL, Stashefsky-Margalit R, Rudd R. Current perspectives on patient education in the US. Patient Educ Couns. 2001;44:79–86. doi: 10.1016/s0738-3991(01)00108-2. [DOI] [PubMed] [Google Scholar]
- 62.Castro C, Wilson C, Wang F, Schillinger D. Babel babble: physicians’. use of jargon with diabetes patients; Proceedings of the 27th Annual Society of General Internal Medicine Annual Meeting; Chicago: IL; 2004. May 12–15, [Google Scholar]
- 63.Schillinger D, Piette J, Grumbach K, Wang F, Wilson C, Daher C, et al. Closing the loop: physician communication with diabetic patients who have low health literacy. Arch Intern Med. 2003;163:83–90. doi: 10.1001/archinte.163.1.83. [DOI] [PubMed] [Google Scholar]
- 64.Heisler M, Bouknight RR, Hayward RA, Smith DM, Kerr EA. The relative importance of physician communication, participatory decision making, and patient understanding in diabetes self-management. J Gen Intern Med. 2002;17:243–52. doi: 10.1046/j.1525-1497.2002.10905.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Piette JD, Schillinger D, Potter MB, Heisler M. Dimensions of patient-provider communication and diabetes self-care in an ethnically diverse population. J Gen Intern Med. 2003;18:624–33. doi: 10.1046/j.1525-1497.2003.31968.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Grant RW, Pirraglia PA, Meigs JB, Singer DE. Trends in complexity of diabetes care in the United States from 1991 to 2000. Arch Intern Med. 2004;164:1134–9. doi: 10.1001/archinte.164.10.1134. [DOI] [PubMed] [Google Scholar]
- 67.Schillinger D, Chen AH. Literacy and language. Disentangling measures of access, utilization, and quality. J General Intern Med. 2004;19:288–90. doi: 10.1111/j.1525-1497.2004.40102.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Yen IH, Moss N. Unbundling education: a critical discussion of what education confers and how it lowers risk for disease and death. Ann N Y Acad Sci. 1999;896:350–1. doi: 10.1111/j.1749-6632.1999.tb08138.x. [DOI] [PubMed] [Google Scholar]
- 69.Singh-Manoux A, Ferrie JE, Chandola T, Marmot M. Socioeconomic trajectories across the life course and health outcomes in midlife: evidence for the accumulation hypothesis? Int J Epidemiol. 2004;33:1072–9. doi: 10.1093/ije/dyh224. [DOI] [PubMed] [Google Scholar]
- 70.Wallerstein N. Powerlessness, empowerment, and health: implications for health promotion programs. Am J Health Promot. 1992;6:197–205. doi: 10.4278/0890-1171-6.3.197. [DOI] [PubMed] [Google Scholar]
- 71.Baker DW, Gazmararian JA, Sudano J, Patterson M, Parker RM, Williams MV. Health literacy and performance on the Mini-Mental State Examination. Aging Ment Health. 2002;6:22–9. doi: 10.1080/13607860120101121. [DOI] [PubMed] [Google Scholar]
- 72.Kanaya AM, Barrett-Connor E, Gildengorin G, Yaffe K. Change in cognitive function by glucose tolerance status in older adults: a 4-year prospective study of the Rancho Bernardo study cohort. Arch Intern Med. 2004;164:1327–33. doi: 10.1001/archinte.164.12.1327. [DOI] [PubMed] [Google Scholar]
- 73.Yaffe K, Kanaya A, Lindquist K, Simonsick EM, Harris T, Shorr RI, et al. The metabolic syndrome, inflammation, and risk of cognitive decline. JAMA. 2004;292:2237–42. doi: 10.1001/jama.292.18.2237. [DOI] [PubMed] [Google Scholar]
- 74.Piette JD, Weinberger M, McPhee SJ. The effect of automated calls with telephone nurse follow-up on patient-centered outcomes of diabetes care: a randomized, controlled trial. Med Care. 2000;38:218–30. doi: 10.1097/00005650-200002000-00011. [DOI] [PubMed] [Google Scholar]
- 75.Lynch J, Kaplan G. Socioeconomic position. In: Berkman LF, Kawachi I, editors. Social epidemiology. New York: Oxford University Press; 2000. pp. xxii–39. [Google Scholar]
- 76.Bindman AB, Grumbach K, Osmond D, Komaromy M, Vranizan K, Lurie N, et al. Preventable hospitalizations and access to health care. JAMA. 1995;274:305–11. [PubMed] [Google Scholar]
- 77.St Leger L. Schools, health literacy and public health: possibilities and challenges. Health Promot Int. 2001;16:197–205. doi: 10.1093/heapro/16.2.197. [DOI] [PubMed] [Google Scholar]
- 78.Rothman RL, DeWalt DA, Malone R, Bryant B, Shintani A, Crigler B, et al. Influence of patient literacy on the effectiveness of a primary care-based diabetes disease management program. JAMA. 2004;292:1711–6. doi: 10.1001/jama.292.14.1711. [DOI] [PubMed] [Google Scholar]
- 79.DeWalt DA, Pignone M, Malone RM, Bryant B, Felix K, Corr K, et al. Randomized controlled trial of a primary care-based heart failure disease management program for patients with low literacy. J Gen Intern Med. 2004;19(s1):203. [Google Scholar]
- 80.Parker RM, Ratzan SC, Lurie N. Health literacy: a policy challenge for advancing high-quality health care. Health Aff (Millwood) 2003;22:147–53. doi: 10.1377/hlthaff.22.4.147. [DOI] [PubMed] [Google Scholar]