Abstract
The purpose of this paper is to look at what has happened in Russia during the last ten years in the health care sector from the point of view of integrated care. This country, when it still was the leading subject of the Soviet Union, hosted in 1978 the Alma Ata Conference on Primary Health Care, which in many countries gave a strong boost on the development of multidisciplinary, community based care in a gate-keeper position. In Soviet Russia, PHC became marginalised and identical to poor level of care in remote areas of the country where people had very little choice and did not want to use it. Has the situation changed, and is Russia in practice addressing the problems created by the lack of integration, vertical treatment structures and over specialisation?
In addition to the data sources that are referred to in the text, this paper is based on “gray literature” available in project reports and governmental documents, and on the personal experiences of the authors, who have worked for long periods of time in the Russian Federation as international experts dealing with health sector reforms and health policy formulation.
Introduction
About 146 million Russians live in a federation of 89 states. The federal legal assembly (Duma) is elected by direct vote, as well as the 89 regional assemblies. The federal and the regional assemblies have both legislative and taxation powers.
Russian health care has existed for decades in a society with a federal administration of 89 “Federal Subjects”, i.e. republics and regions (“oblasts”). Their average size is about 2 million inhabitants, which is more than in many European states. Their geographical size can be bigger than the whole of Western Europe (e.g. Krasnoyarsk and Yakutia).
The Soviet era saw the transformation of a rudimentary health care system of Tsarist times and created a substantial inheritance for the present Russian Federation. The advantages of this development were:
Free access to health care;
Extensive prevention of infectious diseases;
Developed curative service infrastructure;
Abundance of trained health personnel;
Primary health care via rural and urban health posts or city policlinics;
Public health services network through Sanitary Epidemiological system;
Occupational health services;
Health administration—experienced and authoritative;
Many statistical information sources and;
Scientific institutions for medical and health systems research.
Despite the real strengths and opportunities evident above, there are also enormous burdens on the health care system, some of which are directly associated with those features listed as positive. The belief that health care is free at the point of use is shared by the whole nation but is linked to excessive expectations and to unrealistic demands. People feel entitled to unlimited access to health services, and do not understand or respect the gatekeeper function. Recently performed household surveys indicate that approximately 30–50% of the total health care expenditure today comes directly from the patients' pockets. A substantial proportion of this is due to purchasing of pharmaceuticals by the patients.
The health infrastructure has expanded beyond any justified boundaries. There is a large amount of over capacity in terms of polyclinics, hospitals, beds and personnel. The continued existence of parallel health systems sponsored by public and private enterprises and by other ministries (e.g. Defence, Interior, Railways, etc.) exacerbates this issue. The question about over-capacity is a political taboo at all levels. The density of physicians is still rising, although the intake of medical students whose education is paid for by the state has decreased. Medical faculties are now allowed to train also students who pay fully their training expenses. Furthermore, most doctors continue to work way beyond the official retirement age. Quitting of work seems to be mainly dependent on the decision of the individual physician.
The primary health care system, although it exists as a collection of physical settings and staff, is poorly thought through and under utilised. Patients express little confidence in the feldshers and district doctors who are nominally the first point of contact. The concept of community outreach does not exist and disease prevention is seen as screening and periodic health check-ups. Health promotion is perceived as traditional health education (brochures and posters), not as a need for broader policy measures. There has not been a tradition of evidence based practice. Old practices and individual improvisation are encouraged. Although not just typical of Russia, non-evidence-based practices have proven very resilient to change both from professionals' and the patients' side.
After the demise of the Soviet Union, the economy of the Russian Federation collapsed in many areas of society and the country experienced hyperinflation. This resulted in the drastic devaluing of health sector expenditure and a financial crisis within the health system (see Table 1). The failure to pay health care institutions, or indeed staff, led to an ever greater reliance on unofficial out-of-pocket payments for pharmaceuticals and supplies and on under-the-table payments for the most basic of services [1].
Table 1.
Government expenditures on health (1991=100%)
| Health care, including | 1991 | 1992 | 1993 | 1994 | 1995 | 1996 | 1997 | 1998 |
|---|---|---|---|---|---|---|---|---|
| 100 | 80 | 108 | 98 | 72 | 71 | 81 | 67 | |
| State budget | 100 | 80 | 91 | 81 | 59 | 57 | 65 | 51 |
| Obligatory insurance | – | – | 17 | 17 | 13 | 14 | 16 | 16 |
| contributions of legal persons |
Source [2]: Calculated from the CSO (State Statistical committee) data using GDP deflator indices.
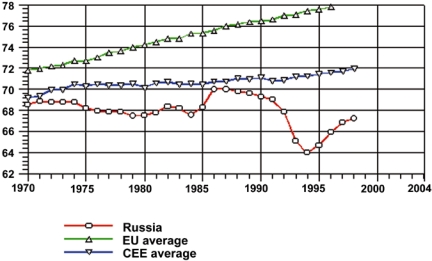
Although the collapse of the Soviet Union has been an unmitigated disaster for the population in terms of health, the causes of this were to be found behind the retrospective latency time. Similar examples from some decades before can be found from the earlier experiences e.g. in China, Scotland and Finland. The decline in Russian health status has been profound with life expectancy plummeting and almost all other health indicators nose-diving (see Figure 1). Some of this trend may be attributable to an ongoing neglect of non-communicable diseases that predated the establishment of the Russian Federation. Some may be due to shifts in data collection and reporting methods. However, it is evident that there has been a real and appreciable worsening of the population's health [3]. Middle-aged men in particular seem to lack the coping mechanisms to deal with such upheaval. They have developed damaging survival strategies, including inappropriate risk taking (dangerous driving, violence) and worsening health behaviours (smoking, drinking, substance misuse) which have all contributed to escalating mortality rates. There is growing evidence also about the increasing incidence of other non-infectious diseases e.g. the incidence of breast cancer among Russian women.
Figure 1.
Years of life expectancy at birth in European Union (EU), Countries of Central and Eastern Europe and the Russian Federation 1970–1998. Source: WHO Regional Office for Europe, HFA database 2000.
The realisation that in the first four years of the existence of the Russian Federation there were a million extra deaths, which would not have occurred had the age and sex specific death rates for 1991 been maintained, was a salutary reminder to planners and politicians that reform was needed.
Legislative and financial changes in Russian health care sector
The reform of the health sector was prompted by numerous collapses in the economy and the pressing need to build cost containment and efficiency into the system, combined with fears about health status and a long overdue recognition of the political aspirations of the regions for more autonomy. The previously highly vertical administrative structure (from federal level to individuals) was to be replaced by horizontal regional and local structures. However, the reform process has not simply been a response to irresistible pressures. Health sector reform was also seen as a real opportunity to address the concerns of planners, providers and population about
the system's ability to respond to local concerns and to non-infectious diseases;
the balance between primary and secondary, general and specialist, inpatient and outpatient;
equity between individuals and between regions;
the implications of under-the-table payments for equity, quality, and humanity of care.
Presently there are at least 25 laws in the field of health and health care, starting from Article 41 of the Constitution of the Russian Federation. Additionally, there are 16 Decrees and Edicts, 8 “Concepts” (“white papers”) and 8 other administrative documents. However, many of these are not yet co-ordinated and fully compatible with each other. Due to the changing administrative structure, the federal, regional and local policies have not been fitted together and the horizontal integration of health care with the intersectoral activities at various levels of governance is missing. National health policy, as WHO understands it, does not yet exist. However, some of the “Concepts” come relatively close to what can be understood as “health care policy”, although the goals have been set very broadly without clear numerical targets such as numbers of hospital beds per population, training of doctors and nurses, future of parallel health services, out-of-pocket payments, etc. However, some regional (state specific) health policy documents have already been developed e.g. in Chelyabinsk and Vologda regions.
New health insurance legislation became effective from the beginning of 1993. The aim was to supplement health care allocation at all levels (federal, regional and local) by traditional funds provided by the compulsory Mandatory Health Insurance. In theory, all citizens are guaranteed basic medical care. In practice it does not work. The premiums, 3.6% of salaries, are collected from employers, while the local government should cover the cost of care for the non-employed (e.g. the children, pensioners and the disabled) by making contributions to the medical insurance fund. In reality more than half of municipalities do not give their contribution stipulated by law to health insurance but instead prefer to give their subsidies directly to health care institutions. In some of the 89 regions, the regional taxes are also used to finance health care. The Russian health insurance system continues to confront major problems of implementation. The low pay of physicians (average official salaries in the range of $40–50 per month) provides a poor base on which to build a structure of incentives, and the country still lacks the service-infrastructure, which could facilitate change.
Many figures for health care expenditure in the Russian Federation are problematic due to issues in the reporting of finances. The indicators widely used in OECD-countries are absent and make international comparisons complex. Core areas of concern are the budget provided by the parallel health system, which go unrecorded.
The precise amount being spent in the various oblasts now exercising independent control and deviating from expected norms is not usually known. In addition, little is done to record the amounts of money raised by the sale of services within the hospital and polyclinic system and there is no way of recording the extent of under-the-table payments or the financial incentives provided by the pharmaceutical industry to the individual physicians. Further complexity is added to estimates by the experience of rapid inflation and changes in governmental approaches to recording.
Between 1990–1995 Russian Statistical Commissions estimated that only 3.2–4.5% of GDP was devoted to health sector. Other sources have described health spending at a higher percentage share of GDP. One of the latest of these is the World Health Report 2000 [4], which estimates as an internationally comparable figure for Russia (1997) the total expenditure for health as share of GDP 5.4%. Public expenditure of this is estimated as 76.9% and private (out-of-pocket) expenditure 23.1%. The Russian estimates for actual money spent per capita in 1990–1995 ranged from $245 to $23. However, to estimate this in purchasing power is difficult, as the value of rouble against dollar was changing constantly and rapidly. The World Health Report (2000) estimated that the total per capita expenditure in Russia was $251 (in “international dollars”) in 1997. To compare, in 1997 the same figure in Poland was 1.6 times higher, in the UK 4.6 times higher and in the Netherlands 7.6 times higher than in the Russian Federation. At a similar level with Russia were countries like Latvia, Malaysia, Peru and Turkey. This comparison is further complicated by the fact that many Russian health care expenditures are included e.g. in the industrial production costs.
The fact that health sector personnel are paid relatively low salaries goes some way to protecting the purchasing power of the health budget. However, the privatisation of pharmaceutical, energy and food supplies has created a rapid inflation in the cost of these inputs. Prices for particular goods are comparable with those in countries with far higher GDP per capita and this places further strains on health budgets.
There are clear trends that the proportion of money spent on capital investment has declined dramatically from a high point in the 1970s when building and expansion was taking place. Building programmes have ceased in many areas altogether and there has also been a marked decline in the money spent on equipment. Pharmaceuticals are taking up a greater share of the budget, largely as the result of rising costs and an opening up of the market to imports. However, the percentage spent on inpatient care is largely static, despite statements by planners and policy makers that they would encourage a shift to primary care and preventive measures. The cost-plus budgeting system does not allow for incentives to alter the structure of service supply.
Health care reform in Russia and the quest for integrated care
The Soviet system traditionally focused on inpatient, secondary and tertiary care at the expense of outpatient primary and preventive medicine. This is not very different from the history in the Western developed countries. Funding mechanisms, which linked hospital budgets to bed numbers thus creating perverse incentives for hospital doctors to keep open and fill unnecessary beds, then perpetuated the over-provision of beds. By 1991 the bias towards hospital-based care was deeply entrenched and hospitals were absorbing the excessive share of resources (Table 2).
Table 2.
Indicators of health care supply to the population in Russian Federation 1985–1998 (population in 146 million in 1998)
| 1985 | 1990 | 1992 | 1994 | 1996 | 1998 | |
|---|---|---|---|---|---|---|
| Number of hospitals (thousands) | 12.5 | 12.8 | 12.6 | 12.3 | 12.0 | 11.2 |
| Number of hospital beds (per 1000 inhabitants) | 13.5 | 13.8 | 13.1 | 12.7 | 12.4 | 11.9 |
| Number of out-patient clinics (thousands) | 19.4 | 21.5 | 20.7 | 21.6 | 22.0 | 22.0 |
| Number of physicians of all specialisations (thousands) | 620.7 | 667.3 | 637.2 | 636.8 | 669.2 | 682.0 |
| Physicians per 10,000 inhabitants | 43.2 | 45.0 | 43.0 | 43.3 | 45.7 | 46.9 |
| Number of middle level health personnel (thousands) | 1756.7 | 1844.0 | 1709.1 | 1613.2 | 1648.6 | 1615.0 |
| Nurses per 10,000 Inhabitants | 122.4 | 124.5 | 115.3 | 109.7 | 112.7 | 111.1 |
Source (Shishkin): CSO (State Statistical Committee) 1997 & 1999 and USAID, 1999.
The intention of the reform programme was originally very much to increase quality and patient choice but also to address the imbalance between hospital and primary medical services. Policy-makers assumed that the devolution of funds to insurance companies would create incentives to spend money as efficiently as possible. To the planners of the reforms this implied shifting resources into primary care and preventive medicine. However, insurance companies do not often have the skills or the tools to measure and implement the most cost-efficient approaches, nor do they tend to take the long-term view that would make investment in health promotion worthwhile. Instead, they have tended to fall back on traditional patterns of provision and to perpetuate the imbalance between the secondary and primary sectors. The shift to billing on a fee per case basis and the insurance company taking a percentage of the charges processed as a handling fee have only exacerbated this tendency. These patterns have allowed hospital expenses to continue unchecked. The fee per case approach counteracts other measures of disease prevention, both primary and secondary prevention.
Attempts to shift care to an outpatient mode have also suffered in the face of patient preferences. Traditionally, it was perceived that the least qualified and least able doctors went into primary care and prevention while those that became outpatient specialists in polyclinics were only a rank higher in the professional order. This was one of the drawbacks of the Kemorovo model in West-Siberia, which had polyclinic doctors acting as fundholders. Their lack of authority in the eyes of patients and of other doctors undermined their ability to be effective as budget holders. The best doctors were believed to go into hospital medicine and in consequence patients continue to push for referral to hospitals rather than accepting care in an ambulatory setting. Partly this belief was re-enforced by the insufficient training of general practitioners in most of the 47 medical schools.
The Soviet system also, inadvertently, encouraged patient preferences for hospital admission through its prescription costs policy. Inpatients received pharmaceuticals free of charge while outpatients were expected to pay for pharmaceuticals unless they were exempted due to several privileged categories (e.g. registered invalids, veterans of World War II, pensioners, etc.). This policy continues and it has more impact now when pharmaceuticals are supplied through private sector and are becoming increasingly expensive. Preliminary analysis has shown that e.g. hypertensive patients spend about the equivalent of the cost of a summerhouse on anti-hypertensive pharmaceuticals within their life span. Patients are more likely to benefit financially from hospital admission despite the extra strain this places on the finances of the system as a whole. Rising pharmaceutical cost is a feature of health care expenditure in its own right and it takes up an increasing proportion of total annual health care spending.
Cultural expectations of medical transactions appear to include the belief that each consultation should lead to the prescription of some drug or other. Certainly, consumption of pharmaceuticals before 1991 was relatively high in terms of prescriptions per consultation if not in terms of costs. As the private sector has become involved in the supply of pharmaceuticals and as foreign firms have begun to market directly to consumers, the pressures on doctors to prescribe have increased.
The Ministry of Health, in consultation with external counterparts has taken steps to improve the cost-effective consumption of pharmaceuticals. In July 1994, Ministerial Order number 157 adopted a list of essential drugs, which included 96 drugs in 31 different categories. Hospitals and polyclinics are encouraged to restrict themselves to the administration of drugs listed as essential but compliance is incomplete. There is not a negative list as such. Also, the Constitutional Article 41, which federally allows for a free medical care, does not include the supply of pharmaceuticals.
What has happened in reality, some practical examples?
Russia is a large country. Like a big boat, it changes direction slowly. As the Resolution of the Board meeting of the Ministry of Health of the Russian Federation dated 15 March 2000, in many areas of health care reform, the principle changes in direction have been positive, such as:
Establishment of health insurance in 1991 and mandatory health insurance in 1993;
Establishment of legal and methodological framework for general practice in 1998;
Setting up a system of basic benefits' package in 1998.
However, in spite of good intentions, the current underneath clearly points in another direction. There have been several development projects funded by TACIS of the European Union, the World Bank, and several bilateral agencies in places like St. Petersburg, Kemerovo, Samara, Chelyabinsk, etc. However, after external funding of these pilot projects has finished, the lessons learned have not been actively disseminated to other localities. The official number of GPs working in Russia was 1100 in March 2000. Just to reach a level of one GP per 2000 inhabitants would require about 73,000 practising GPs in Russia. At the present speed, the number of GPs needed will be reached in 100 years. One reason for this is that postgraduate training to a great extent is paid by the trainees themselves or their sponsors.
Polyclinic No 34 in St. Petersburg has 10 GPs who have been trained by Swedish funding in Russia and in Sweden. Strikingly, a reception room does not have any equipment for injections or any other procedures to which a western-trained GP would be used. The explanation is that according to the public health (“San-Epid”) rules of the Federal Ministry of Health, such manoeuvres are only allowed in specifically designed premises. Gynaecological examinations are not allowed either. They can only be performed by a gynaecologist. Children under 15 are not allowed to be treated by a Russian GP, as this is the domaine of a paediatrician.
The mere good intention does not turn a boat, whether big or small. Real action is needed also in the infrastructure. So far no one in Russian health policy has really wanted to challenge the establishment of specialist clinics, which are bound to experience a major decline in their clientele—and revenues—if the first contact level (general practice) really is allowed to function. The changes in the infrastructure are prerequisites which include at least the reorientation of educational and manpower policy, reimbursement policy, budgeting policy, and capital investment policy.
Conclusions
As was indicated earlier in the paper, the views presented in this article are partially based on the personal experience of the authors and on “gray literature”. Therefore, generalisations are difficult in Russia because of its vast geographical size and because all 89 “Federal Subjects” (regions, republics, autonomic areas, etc.) can be very different when it comes to health care implementation. The following conclusions and predictions of the future need to be made with great caution.
A major shift in the health of the Russian population has resulted in a rapid rise of non-infectious diseases e.g. cardiovascular diseases, cancer and accidents. In addition, some infectious diseases have increased due to a deterioration of some previously systematic approaches in public health practices and new social behavioural patterns e.g. the sexually transmitted diseases.
Areas of special concern include the continuing pressures on health status that arise from the chaotic socio-economic conditions and the emerging inequities. Much was expected from the shift to insurance and great reliance was placed on its quasi-market elements to create incentives for efficiency and equity of care.
The insurance system has never functioned as first envisaged. Public policies on business practices were simply not in place, not to mention the necessities of controlling the causes and consequences of market failures in health care. It is necessary to modify the structures as it has become increasingly clear that the private sector insurance companies were not emerging and where they did, they could not be entrusted with lump sum payments that represented the planned health care expenditure for whole populations. Their role in quality control could not come into being, as quality indicators are poorly developed and as most insurance companies could not understand what good quality in health care was about.
There are some positive signs that trained primary health care doctors (general practitioner/family doctor) in Russia as anywhere else can gain trust from their catchment population. However, as long as PHC remains the lowest level in the hierarchical health care system under the administrative and financial control of superseding specialist structures, it is unlikely that the situation would change. If more patients were treated at the first contact level, it would undermine the income of any professional group above them. Furthermore, denial of referral, albeit unnecessary, would undermine the income of the first contact doctor, who receives additional income for making an effective and quick referral. The appropriate economic incentives of PHC are not in place.
For the time being, it is unreasonable to assume a quick change towards integrated care in Russia. There are too many powerful groups who would feel that they would lose out and the medical training structure does not provide adequate professional support or infrastructure for a change. The general public does not perceive well-developed primary health care as a realistic option for them, either. The group of general practitioners is too small, and with the speed they are being trained (by 1999 approximately 5000, about 0.7% of all doctors), they will remain so for a long period.
On the other hand, if the political will would be in place—beyond well meaning concepts and resolutions—it might be possible to have relatively rapid progress, especially now as the Russian economy due to high oil prices is relatively strong. After all, in Russia the responsibility for planning, implementing and financing of medical education is one of the key roles of the Ministry of Health of the Russian Federation. As long as general practitioners and family nurses are rare, a team consisting of a first level internist, paediatrician and obstetrician could become a primary health care team with a fixed catchment population and capitation payment. However, they would need good supervision, to be liberated from the constrictive control of the second level specialists, and they need to be empowered to treat their patients at the first contact level.
For an integrated Russian health care, the resources and the means are there—but the appropriate incentives are not.
Contributor Information
Mikko A. Vienonen, WHO Special Representative of the Director General in Russia, WHO Office, 28 Ostozhenka St., 119034 Moscow, Russian Federation. Phone: +7-095-787 21 66 Fax: +7-095-787 21 19.
Ilkka J. Vohlonen, Center for Pharmaceutical Policy and Economics, University of Kuopio, P.O. Box 1627, FIN-70211 Kuopio, Finland. Phone: + 358 17 162 592 Fax: +358 17 162 515.
References
- 1.Ensor T. The unofficial business of health care in transitional Europe. Eurohealth. 2000 Spring;6(2 Special Issue):35–7. [Google Scholar]
- 2.Shishkin S. Issues of health care financing in Russia. SPIDER-PE: Stockholm St. Petersburg Institutional development in Education and Research Public Economics. Published by St. Petersburg State University, School of Management; 2000. (Working paper series no 16, 2000) [Google Scholar]
- 3.Leon D, Chenet L, Shkolnikov V, Zakharov S, Shapiro J, Rachmanova G, et al. Huge variations in Russian mortality rates 1984–94: artefact, alcohol or what? Lancet. 1997 Aug 9;350(9075):383–8. doi: 10.1016/S0140-6736(97)03360-6. [DOI] [PubMed] [Google Scholar]
- 4.The World Health. Report Health systems: improving performance. Geneva: WHO; 2000. [Google Scholar]