SYNOPSIS
Objectives
Experiences of abuse increase the risk of psychiatric morbidity in women. This study assesses the prevalence of intimate partner violence and minor psychiatric morbidity and analyzes their association among aboriginal women in Taiwan.
Methods
Using system random sampling, 840 aboriginal women between the ages of 18 and 50 years old were recruited from four townships with aboriginal communities in southern Taiwan. Trained primary care nurses interviewed the participants at home by structured questionnaire.
Results
One hundred twenty-six of 840 (15%) of the aboriginal women had experienced physical abuse perpetrated by an intimate partner (her husband or cohabitant) during their lifetime; 10.1% had experienced it during the past 12 months; 4.0% had experienced sexual abuse by the partner; and 6.3% had experienced physical abuse during childhood at the hands of one or both parents. Multiple logistic regression revealed that after adjusting for women’s age, alcohol and drug use, religious activity and husband’s employment status, the experience of abuse (including partner physical abuse, partner sexual abuse, and childhood physical abuse) was significantly associated with suicidal ideation and depression.
Conclusions
Health care professionals need to provide adequate support and health education, develop interventions, and use referrals in primary care in the community in order to reduce and prevent domestic violence against aboriginal women in Taiwan.
Intimate partner violence (IPV) is a major, worldwide public health and human rights issue.1 Population-based studies conducted in 48 countries have revealed that 10% to 69% of women report having been physically assaulted by an intimate partner during their lifetimes.2 Although the results of family conflict studies or crime studies showed equal rates of assault by men and women,3,4 the injury rate for assaults by men is about seven times the injury rate for assaults by women.5
Moreover, aboriginal women have a significantly higher prevalence of violence by their partners compared to non-aboriginal women.6 The community survey of adult American Indian women found that the lifetime prevalence of physical violence against them was from 41.9% to 91%.7,8 The 1999 General Social Survey showed that 25% of aboriginal women and 8% of non-aboriginal women in Canada were assaulted by a current or former spouse.9
In Taiwan, there are ten aboriginal tribes which contain about 450,000 aboriginal people, constituting nearly 1.9% of the entire population.10 These aboriginal tribes can be distinguished from one another by their languages and their traditional societal systems. The aborigines’ health status is worse than that of the rest of the Taiwanese population.11 In a recent survey of aboriginal women who had just given birth in a hospital, 15.3% of them had ever been physical abused by their partner, and 6.9% had this experience during their recent pregnancy.12 In general, 8.3% of the married women in Taiwan had ever been physical assaulted by their spouse within the previous 12 months.13 The survey revealed that intimate partner violence is a health problem for aboriginal women in Taiwan.
In numerous studies, battered women have been found to be at increased risk for major depression, suicide, and alcohol or drug use.14–19 Partner violence has been associated with lifetime, 12-month, and current major depression in female Chinese Americans, and it has a dose-response relationship with the severity of major depression episodes.20 Although significant psychiatric morbidity has been associated with abused women,14 abused women’s depression or chronic stress in adverse living conditions may present to health care providers in the form of vague physical symptoms such as headache, fatigue, insomnia, choking sensations, gastrointestinal complaints, pelvic pain, and backache.17,21 Substance abuse, suicide, unemployment, and family violence were identified by Canadian aboriginal people as social problems in their community.22 Taiwanese aborigines similarly tend to experience such health-related problems, and their health status is worse than that of the rest of the Taiwanese population.11
No prior study has been done to determine the prevalence of IPV and the possible associations between IPV and psychiatric morbidity in the case of aboriginal women in Taiwan. Meanwhile, the association between intimate partner violence and mental health status is of great concern within the domain of public health policy decisions.
The purpose of the present study was to: (1) estimate the prevalence of intimate partner violence among Taiwanese aboriginal women, and (2) detect the associations between IPV experiences and the mental health status of aboriginal women. This study is intended for use in the development of IPV prevention programs in aboriginal communities in Taiwan, and in other countries where indigenous communities face similar problems.
Methods
Study population and sampling
Bunun and Paiwan tribes are the main aborigines in southern Taiwan. From May to December 2002, two townships of each tribe, a total 5,170 households, were randomly selected. Thereafter, 20% of the eligible households with a woman aged 18 to 50 years and ever having had any intimate partner were recruited by systemic random sampling from the household records of the Household Registry Center in each township. In each household, one eligible woman was selected randomly to be interviewed. A total of 1,034 households were selected; among them, 876 agreed to participate in this study. The response rate was 84.7%. Unfortunately, 36 of them were not able to complete the interview. Thus, only 840 questionnaires were valid for further analysis. The participants were told that participation was voluntary and that all information disclosed would be confidential; verbal informed consent was obtained from the women beforehand. This study received ethical approval from the Human Research Ethics Committee of Kaohsiung Medical University.
Data collection
A questionnaire incorporating several instruments was developed and evaluated by the authors. Seven experts were asked to oversee the content coverage and adequacy of this questionnaire and instruments. The regional public health nurses (the majority were aborigines) in the community health station were trained to be the interviewers and data were collected by household interview; a telephone call was made beforehand to confirm the appointment. The public health nurses were already very familiar with those interviewees, which was helpful in facilitating the interviewing process. Both the interviewers and study participants could communicate fluently by Chinese Mandarin or by dialect.
The physical abuse screen contained three questions with yes/no answers that were derived from the Abuse Assessment Screen (AAS);23 these were used to rate the presence of experiences of abuse. The modified AAS has been validated by bilingual translation and back-translation and used in a similar aboriginal study in Taiwan.12 The test and test reliability of the physical abuse questions was 0.87 in that study. If a woman reported that she had ever been hit, slapped, kicked, or otherwise physically hurt by her intimate partner (defined as a current or former spouse, or cohabitant) in the past or during the preceding year, she was classified as “physically abused.” If a participant answered that she had been forced by her partner to have sex with him, she was classified as have been “sexually abused.”
The Suicidal Ideation Screening Questionnaire (SIS-Q), consisting of four items with yes/no answers, was used to predict the participants with suicidal ideation.24 After the procedure of bilingual translation and back-translation, it was used in a female aboriginal study in Taiwan; the reliability of this scale was 0.78.25 The SIS-Q included (1) sleep disturbance, (2) mood disturbance, (3) guilt, and (4) hopelessness. The SIS-Q is designed so that primary care professionals, using a combination of questions about sleep disturbance and mood disturbance, can set the tone for an interview in such a way that a client with suicidal thoughts will feel comfortable enough to disclose her feelings. One or more positive answers by a participant in response to these questions by the interviewer suggests suicidal ideation.24 In this study, suicidal ideation was not explored directly by SIS-Q; instead, symptoms from the Diagnostic Interview Schedule (DIS)26 were chosen for its strongly association with the occurrence of suicidal ideation. (The DIS is a structured interview designed for use by lay interviewers in epidemiologic studies, was used to assign psychiatric diagnoses according to criteria from the Diagnostic and Statistical Manual of Mental Disorders, Third Edition [DSM-III].) In addition, the two-question case finding instrument27 was applied to identify possible major depression. The questionnaire included two questions with yes/no answers: (1) “During the past month, have you often been bothered by feeling down, depressed mood, or hopeless?“ (2) “During the past month, have you often been bothered by little interest or pleasure in doing things?” One or more positive answers suggested major depression. The two-question case finding instrument had a sensitivity of 96% and a specificity of 57% in identifying subjects with the diagnosis of major depression.27 It is a useful measure for detecting depression in primary care. It has test characteristics similar to other case-finding instruments and is less time-consuming.27 The participants were also asked questions about their use of alcohol, cigarettes, and illicit (street) drugs.
Data analysis
Statistical analysis
Chi-squared analysis and two-tailed significance tests were used for data analysis. Odds ratios (ORs) and 95% confidence intervals (CIs) were calculated for the associations of suicidal ideation, depression, and sociodemographic variables of the participants’ responses and to detect the association between intimate partner violence experiences and suicidal ideation and depression. Finally, multiple logistic regressions were used to assess the significant variables in relation to suicidal ideation and depression, while controlling for the effects of the other significant variables. Data analysis was performed using SAS statistical software, version 8.2.28 A p-value of less than 0.05 was considered statistically significant.
Results
Study population characteristics
The eligible participants were 18 to 50 years of age who had ever had any intimate partner. The participants’ mean age was 36.9 years (standard deviation [SD]58.1 years), the majority (58.3%) of the women had nine or fewer years of education, and 43.3% of the participants were employed.
Prevalence of abusive experience
A total of 126 (15.0%; 95% CI 12.6, 17.4) women reported ever experiencing physical abuse by their intimate partners and 85(10.1%; 95% CI 8.1, 12.1) had experienced physical abuse during the preceding year. Thirty-four (4.0%; 95% CI 2.7, 5.3) had experienced sexual abuse by the partner; 53 (6.3%; 95% CI 4.7, 7.9) had experienced severe beating by a parent when a child. Among the study participants, the childhood experiences of physical abuse were significantly related to physical abuse (OR54.59; 95% CI 2.54, 8.29) and sexual abuse by the partner (OR53.61; 95% CI 1.42, 9.18).
Prevalence of minor psychiatric morbidity
Among the responders, 318 (37.8%; 95% CI 34.5, 41.1) women reported to have depressive symptoms in the past month, as determined by the two-question case finding instrument. Based on the SIS-Q assessment, a total of 326 (38.7%; 95% CI 35.4, 42.0) women reported having suicidal ideation during the preceding year. In addition, we investigated the frequency of alcohol use (defined as having a drink of any sort of alcohol at least twice per week) during the preceding year. Among the study participants, 524 (62.4%; 95% CI 59.1, 65.7) reported that they drank alcohol, while 112 (14.2%; 95% CI 11.8, 16.6) reported that they ever used non-prescription drugs (sedatives or analgesics) during the preceding year.
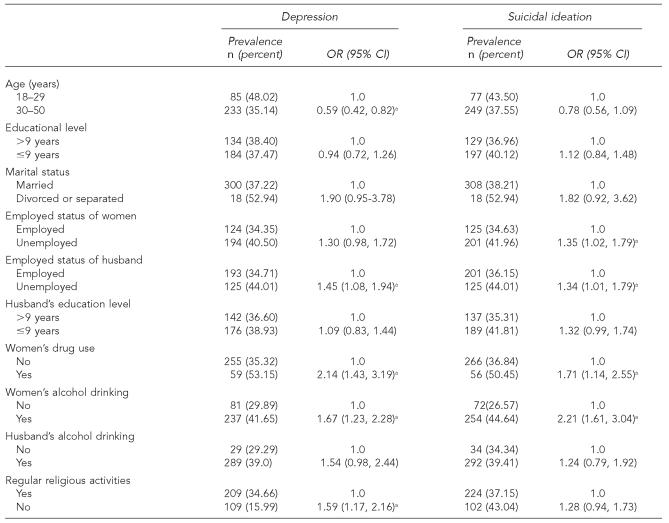
Table 1 illustrates the associations between the demographic characteristics of the women in this survey and their mental health status. The results indicated that the women who were younger than 30 years old, who were alcohol users or non-prescription drug users, whose husbands were unemployed, and who did not regularly engage in religious activities were more likely to report depressive symptoms. We also found that women who were unemployed or whose husbands were unemployed, and women who used alcohol or drugs, were more likely to report suicidal ideation.
Table 1.
The demographic variables associated with the mental health outcomes of aboriginal women in southern Taiwan
p<0.05
Association between abusive experiences and mental health outcomes
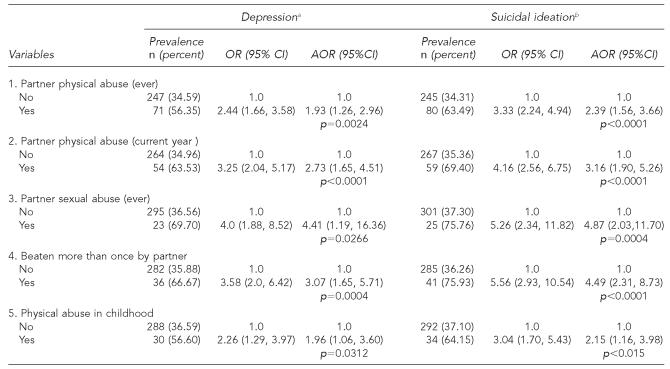
Multiple logistic regression was performed to examine the independent associations between experiences of abuse (physical abuse by intimate partner, sexual abuse by partner, physical abuse in childhood) and mental health outcomes. Table 2 shows that after adjusting for significant demographic characteristics (women’s age, women’s alcohol and drug use, husband’s employment status, religious activity) and physical abuse during childhood, the victims of partner physical abuse were more likely than non-victims to report depressive symptoms (56.4% vs. 34.6%; OR51.93; 95% CI 1.26, 2.96) and to report suicidal ideation (63.5% vs. 34.3%; OR52.39; 95% CI 1.56, 3.66). We also found that women who experienced partner sexual abuse or physical abuse in childhood were more likely to have poor mental health outcomes after adjusting the demographic variables and partner physical abuse. The adjusted odds ratio demonstrated a stronger association of physical abuse with reporting depressive symptoms or reporting suicidal ideation during the past 12 months compared to any period prior to that.
Table 2.
Association between the experiences of various abuse patterns and mental health outcomes among the aboriginal women in southern Taiwan
Depression: AOR: odds ratio was adjusted for women’s age, women’s alcohol and drug use, husband’s employment status, religious activity and physical abuse during childhood in variable 1, 2, 3, 4. Ever physical abuse by partner was added in addition to the demographic variables in the analysis of variable 5.
Suicidal ideation: AOR: odds ratio was adjusted for women’s and husbands’ employment status, women’s alcohol and drug use and physical abuse during childhood in variable 1, 2, 3, 4. Physical abuse ever by partner was added in addition to the demographic variables in the analysis of variable 5.
OR = odds ratio
AOR = adjusted odds ratio
Women who had experienced physical abuse by a partner were more likely to use non-prescription hypnotics (47.8% vs. 14.1%; OR55.57; 95% CI 2.40, 12.93) and analgesics (24.4% vs.13.2%; OR52.12; 95% CI 1.35, 3.32) compared with those who did not have such experiences. The results of the multiple logistic regression show that women’s drug misuse was independently associated with reporting depressive symptom and with reporting suicidal ideation (Table 2).
Discussion
We measured a broad range of physical abuse experiences and mental health outcomes from a random sample of the aboriginal communities. We found that those aboriginal women who had ever experienced IPV were 1.9 times more likely to report having depressive symptoms, 2.4 times more likely to report having suicidal ideation during the past year, and were 5.6 times more likely to report using non-prescription hypnotics than those who were not victims of IPV. We found the lifetime prevalence of physical abuse by intimate partners was 15%, which accords with the finding of the IPV lifetime prevalence (ranging from 10% to 69% in population-based studies conducted in 48 countries).2 But this prevalence is lower than that of adult American Indian women, which studies have shown to range from 41.9% to 91%.7,8 The discrepancy would be attributable to differences in sampling, and possible reporting bias or cultural stigma.
Experience of abuse is highly stressful for women. Battered women used psychoactive substances to self-medicate for stress29 and women with a history of childhood abuse were more likely to be abusing drugs.30 Similar results were found in our study; among the women who had experienced IPV or partner sexual abuse, we found a significantly higher rate of non-prescription hypnotics use and analgesic use.
Depression is one of the most prevalent negative health consequences of domestic violence.2 Previous studies found that battered women were more likely to be at increased risk for major depression, suicide, and alcohol or drug use.14–19 Partner violence has been associated with lifetime, 12-month, and current major depression in female Chinese Americans, and it has a dose-response relationship with the severity of major depression episodes.20 In this study, we used a two-question case finding instrument to identify probable cases of major depression and used SIS-Q to identify possible cases of suicidal ideation.24,27 After controlling for the demographic risk factors, we found an association of experiences of abuse (included partner physical abuse, partner sexual abuse, and physical abuse in childhood) with depressive symptoms and suicidal ideation. Even when it is not an actually diagnosed depression, those with depressive symptoms and suicidal ideation identified in this study were more likely to have a higher prevalence of IPV. These findings are supported by the same consistent pattern of findings as in other international studies.14–20,31
In this study, we found that women who were physically abused in childhood were more likely to report depressive symptoms and to report suicidal ideation, and were more likely to have been physically or sexually abused by intimate partners. This finding is consistent with previous reports linking exposure to childhood maltreatment to more frequent adverse mental health outcomes.32–34 Due to the cross-sectional nature of this study, it cannot provide information about cause and effect relationships. As other authors have suggested, a history of childhood abuse may not lead to greater vulnerability for psychiatric morbidity, but rather confounding social and familial factors (such as poverty and dysfunctional family environment) are associated with both the experience of child abuse and greater risk of poor mental health outcomes.35 In addition, a study of the intergenerational transmission of violence found that all forms of family-of-origin violence (father to mother, mother to father, parent to child) were predictive of physical abuse in intimate relationships.36
In America, indigenous women have been proven to have a higher death rate from alcohol abuse and suicide.37 One study of indigenous women in Pakistan that explored the pattern of suicide there showed that the majority of the subjects were under 30 years of age and domestic problems were the most common reason stated for attempting suicide.38 Our study results suggest that IPV against women was a dominant factor in substance misuse and reporting suicidal ideation and depressive symptoms among women in aboriginal communities. The consistent pattern of this association and its commonality across different populations suggests a possible causal role for partner violence, which needs further investigation of major depression in women.20
In conclusion, after controlling for demographic risk factors, women with experiences of IPV were more likely to report depressive symptoms, suicidal ideation, and substance use. Strategies of prevention and intervention of partner physical abuse among Taiwanese aboriginal women should include: (1) greater support and professional assessment for depression, suicidality, and substance abuse among Taiwanese aboriginal women; and (2) increased awareness among primary care professionals of the necessity to assess potential victims of abuse among aboriginal women, especially during primary care.
Acknowledgments
The authors wish to thank all the participants in the study and the nursing staff of the health stations involved in the study for their help in collecting data.
Footnotes
This work was supported by grants from the National Science Council (NSC 91-2314-B-037-242) and (in part) from Department of Health, Executive Yuan, R.O.C.
REFERENCES
- 1.Ferris LE. Intimate partner violence. BMJ. 2004;328:595–6. doi: 10.1136/bmj.328.7440.595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Heise L, Garcia-Moreno C. Violence by intimate partners. In: Krug E, Dahlberg LL, Mercy JA, Zwi AB, Lozano R, editors. World Report on Violence and Health. Geneva, Switzerland: World Health Organization; 2002. pp. 87–121. [Google Scholar]
- 3.Straus MA. The controversy over domestic violence by women: a methodological, theoretical, and sociology of science analysis. 1999. [cited 2005 Nov 25]. Available from: URL: http://www.batteredmen.com/straus99.htm.
- 4.Home Office. British crime survey. London: HMSO; 1998. [Google Scholar]
- 5.Stets JE, Straus MA. Gender differences in reporting of marital violence and its medical and psychological consequences. In: Straus MA, Gelles RJ, editors. Physical violence in American families: risk factors and adaptations to violence in 8,145 families. New Brunswick (NJ): Transaction; 1990. pp. 151–65. [Google Scholar]
- 6.Brownridge DA. Male partner violence against aboriginal women in Canada: an empirical analysis. J Interpers Violence. 2003;18:65–83. [Google Scholar]
- 7.Fairchild DG, Fairchild MW, Stoner S. Prevalence of adult domestic violence among women seeking routine care in a Native American health care facility. Am J Public Health. 1998;88:1515–7. doi: 10.2105/ajph.88.10.1515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Robin RW, Chester B, Rasmussen JK. Intimate violence in a southwestern American Indian tribal community. Cult Divers Ment Health. 1998;4:335–44. [PubMed] [Google Scholar]
- 9.Trainor C, Mihorean K, editors. Family violence in Canada: a statistical profile 2001. Ottawa: Minister of Industry, Statistics Canada: Canadian Centre for Justice Statistics; 2001. Jun, Catalogue no.: 85-224-XIE. [Google Scholar]
- 10.Council of Indigenous People, Executive Yuan (Taiwan) Statistics of indigenous population in Taiwan and Fukien areas for townships, cities and districts; 2005 Jan 31. [cited 2005 Mar 26]. Available from: URL: http://others.apc.gov.tw/popu/9401/aprp5123.htm.
- 11.Ko YC, Liu BH, Hsieh SF. Issues on aboriginal health in Taiwan. Kaohsiung J Med Sci. 1994;10:337–51. [PubMed] [Google Scholar]
- 12.Yang MS, Yang MJ, Chou FH, Yang HM, Wei SL, Lin JR. Physical abuse against pregnant aborigines in Taiwan: prevalence and risk factors. Int J Nurs Stud. 2005;43:21–7. doi: 10.1016/j.ijnurstu.2004.12.005. [DOI] [PubMed] [Google Scholar]
- 13.Yang WS. 2002 Conference on Social Problems: the Analyses of Taiwan Social Change Survey; 2002. Taiwan: Taipei: Institute of Sociology Academia Sinica; 2002. Sep 27–28, Estimates of the intimate partner violence among married couples in Taiwan. [Google Scholar]
- 14.Crowell NA, Burgess AW, editors. Understanding violence against women. Washington: National Academy Press; 1996. [Google Scholar]
- 15.Campbell J, Kub JE, Rose L. Depression in battered women. J Am Med Womens Assoc. 1996;51:106–10. [PubMed] [Google Scholar]
- 16.Coid J, Petruckevitch A, Feder G, Chung W, Richardson J, Moorey S. Relation between childhood sexual and physical abuse and risk of revictimisation in women: a cross-sectional survey. Lancet. 2001;358:450–4. doi: 10.1016/s0140-6736(01)05622-7. [DOI] [PubMed] [Google Scholar]
- 17.Diaz-Olavarrieta C, Ellertson C, Paz F, de Leon SP, Alarcon-Segovia D. Prevalence of battering among 1780 outpatients at an internal medicine institution in Mexico. Soc Sci Med. 2002;55:1589–602. doi: 10.1016/s0277-9536(01)00293-3. [DOI] [PubMed] [Google Scholar]
- 18.Nedd DM. Self-reported health status and depression of battered black women. ABNF J. 2001;12:32–5. [PubMed] [Google Scholar]
- 19.Weingourt R, Maruyama T, Sawada I, Yoshino J. Domestic violence and women’s mental health in Japan. Int Nurs Rev. 2001;48:102–8. doi: 10.1046/j.1466-7657.2001.00059.x. [DOI] [PubMed] [Google Scholar]
- 20.Hicks MH, Li Z. Partner violence and major depression in women: a community study of Chinese Americans. J Nerv Ment Dis. 2003;191:722–9. doi: 10.1097/01.nmd.0000095124.05023.e1. [DOI] [PubMed] [Google Scholar]
- 21.Swanson RW. Battered wife syndrome. CMAJ. 1984;130:709–12. [PMC free article] [PubMed] [Google Scholar]
- 22.MacMillan HL, MacMillan AB, Offord DR, Dingle JL. Aboriginal health. CMAJ. 1996;155:1569–78. [PMC free article] [PubMed] [Google Scholar]
- 23.McFarlane J, Parker B, Soeken K. Physical abuse, smoking, and substance use during pregnancy: prevalence, interrelationships, and effects on birth weight. J Obstet Gynecol Neonatal Nurs. 1996;25:313–20. doi: 10.1111/j.1552-6909.1996.tb02577.x. [DOI] [PubMed] [Google Scholar]
- 24.Cooper-Patrick L, Crum RM, Ford DE. Identifying suicidal ideation in general medical patients. JAMA. 1994;272:1757–62. [PubMed] [Google Scholar]
- 25.Yang MS, Yang MJ. Correlated risk factors for suicidal ideation in aboriginal Southern Taiwanese women of childbearing age. Public Health. 2000;114:291–4. doi: 10.1038/sj.ph.1900639. [DOI] [PubMed] [Google Scholar]
- 26.American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 3rd ed. Washington: American Psychiatric Association; 1980. [Google Scholar]
- 27.Whooley MA, Avins AL, Miranda J, Browner WS. Case-finding instruments for depression. Two questions are as good as many. J Gen Intern Med. 1997;12:439–45. doi: 10.1046/j.1525-1497.1997.00076.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. SAS Corporation. SAS version 8.2. Cary (NC); 2001.
- 29.Kearney MH. Truthful self-nurturing: a grounded formal theory of women’s addiction recovery. Qual Health Res. 1998;8:495–512. doi: 10.1177/104973239800800405. [DOI] [PubMed] [Google Scholar]
- 30.McCauley J, Kern DE, Kolodner K, Dill L, Schroeder AF, DeChant HK, et al. Clinical characteristics of women with a history of childhood abuse: unhealed wounds. JAMA. 1997;277:1362–8. [PubMed] [Google Scholar]
- 31.Kaslow NJ, Thompson MP, Okun A, Price A, Young S, Bender M, et al. Risk and protective factors for suicidal behavior in abused African American women. J Consult Clin Psychol. 2002;70:311–9. doi: 10.1037//0022-006x.70.2.311. [DOI] [PubMed] [Google Scholar]
- 32.MacMillan HL, Fleming JE, Streiner DL, Lin E, Boyle MH, Jamieson E, et al. Childhood abuse and lifetime psychopathology in a community sample. Am J Psychiatry. 2001;158:1878–83. doi: 10.1176/appi.ajp.158.11.1878. [DOI] [PubMed] [Google Scholar]
- 33.Mullen PE, Martin JL, Anderson JC, Romans SE, Herbison GP. Childhood sexual abuse and mental health in adult life. Br J Psychiatry. 1993;163:721–32. doi: 10.1192/bjp.163.6.721. [DOI] [PubMed] [Google Scholar]
- 34.Weiss EL, Longhurst JG, Mazure CM. Childhood sexual abuse as a risk factor for depression in women: psychosocial and neurobiological correlates. Am J Psychiatry. 1999;156:816–28. doi: 10.1176/ajp.156.6.816. [DOI] [PubMed] [Google Scholar]
- 35.Mullen PE, Martin JC, Romans SE, Herbison GP. The long-term impact of the physical, emotional, and sexual abuse of children: a community study. Child Abuse Negl. 1996;20:7–21. doi: 10.1016/0145-2134(95)00112-3. [DOI] [PubMed] [Google Scholar]
- 36.Kwong MJ, Bartholomew K, Henderson AJ, Trinke SJ. The intergenerational transmission of relationship violence. J Fam Psychol. 2003;17:288–301. doi: 10.1037/0893-3200.17.3.288. [DOI] [PubMed] [Google Scholar]
- 37.Department of Health and Human Services (US) Regional differences in Indian health, 1998-1999. Indian Health Service: Rockville (MD); 1999. [Google Scholar]
- 38.Khan MM, Reza H. The pattern of suicide in Pakistan. Crisis. 2000;21:31–5. doi: 10.1027//0227-5910.21.1.31. [DOI] [PubMed] [Google Scholar]