Abstract
The latex of the plant Calotropis procera has been reported to exhibit potent antiinflammatory activity against carrageenin and formalin that are known to release various mediators. In the present study, we have evaluated the efficacy of extracts prepared from the latex of C procera against inflammation induced by histamine, serotonin, compound 48/80, bradykinin (BK), and prostaglandin E2(PGE2) in the rat paw oedema model. The paw oedema was induced by the subplantar injection of various inflammagens and oedema volume was recorded using a plethysmometer. The aqueous and methanol extracts of the dried latex (DL) and standard antiinflammatory drugs were administered orally 1 hour before inducing inflammation. The inhibitory effect of the extracts was also evaluated against cellular influx induced by carrageenin. The antiinflammatory effect of aqueous and methanolic extracts of DL was more pronounced than phenylbutazone (PBZ) against carrageenin while it was comparable to chlorpheniramine and PBZ against histamine and PGE2, respectively. Both extracts produced about 80%, 40%, and 30% inhibition of inflammation induced by BK, compound 48/80, and serotonin. The histological analysis revealed that the extracts were more potent than PBZ in inhibiting cellular infiltration and subcutaneous oedema induced by carrageenin. The extracts of DL exert their antiinflammatory effects mainly by inhibiting histamine and BK and partly by inhibiting PGE2.
INTRODUCTION
The latex of Calotropis procera (Ait) R Br is well known for its toxic as well as medicinal properties. It has been reported to produce congestion of eyes, iridocyclitis, and dermatitis following accidental exposure [1, 2, 3]. Local administration of the latex has been reported to elicit an inflammatory response that is mediated through histamine and prostaglandins [4, 5, 6, 7]. However, in Indian traditional medicine it has been used for the treatment of skin diseases, rheumatism, and aches [8]. It has been reported to exhibit potent antiinflammatory, analgesic, and weak antipyretic activities when administered orally [9, 10, 11, 12]. The latex is as potent as standard antiinflammatory drug phenylbutazone (PBZ) in inhibiting inflammatory response induced by various inflammagens in acute and chronic models of inflammation [10]. However, the efficacy of latex of C procera against various inflammatory mediators has not been evaluated.
A number of mediators are involved in the inflammatory response elicited by various inflammagens. The early phase of acute inflammation involves cellular influx associated with the release of mediators like histamine and serotonin that is followed by the production of bradykinin (BK) and prostaglandins (PGEs) [13]. All these mediators produce inflammation when injected subcutaneously in the rat paw [14]. The present study was carried out to evaluate the antiinflammatory activity of the latex of C procera and its methanolic extract against various inflammatory mediators as well as on leucocyte influx induced by carrageenin in rat paw oedema model.
MATERIAL AND METHODS
Plant material and drugs
The C procera plant was identified by the Raw Materials, Herbarium and Museum Division, National Institute of Science Communication, CSIR, New Delhi, where a voucher specimen is preserved (voucher no PID 1739). The latex was collected from the aerial parts of the plant growing in the wild. It was dried under shade at ambient temperature, ground to small granules (DL), and sequentially soxhlated with petroleum ether and methanol to get the methanolic extract of DL (MeDL) with a yield of 25%. The crude DL and MeDL were triturated with gum acacia (1:1) in normal saline (NS), filtered, and administered orally to rats at doses ranging from 50 to 1000 mg/kg (DL-50, DL-500, DL-1000, MeDL-50, MeDL-500, and MeDL-1000). The drugs used in the study were obtained from Sigma-Aldrich Corporation (Bangalore, India) (histamine, serotonin, and compound 48/80), AstraZeneca (Bangalore, India) (PGE2), Spectrochem (Mumbai, India) (carrageenin), Merind India Ltd (Baroda, India) (cyproheptadine), SG Pharmaceuticals (Baroda, India) (phenylbutazone), Novartis (London, UK) (bradyzide), Bachem (Bubendorf, Switzerland) (bradykinin).
Animals
Male Wistar rats weighing 120–150 g were used for this study. The animals had free access to food and water. The experiments were performed as per the guidelines of the Institutional Animal Ethics Committee.
Rat paw oedema test
Pedal oedema was induced by injecting carrageenin (0.1 mL of 1% suspension in NS), histamine (0.1 mL of 0.1% solution in NS), serotonin (0.1 mL of 0.02% solution in NS), compound 48/80 (0.1 mL of 0.01% solution in NS), PGE2 (0.1 mL of 0.0002% solution in NS), and BK (0.1 mL of 0.001% solution in NS) into the subplantar surface of the rat paw. In case of BK-induced inflammation, all animals were pretreated with captopril (5 mg/kg, subcutaneous) 1 hour earlier, to prevent BK degradation [15]. The paw volume was measured up to the lateral malleolus by the mercury displacement method just before and at hourly intervals after injection of inflammagen, and the time of peak inflammatory response was recorded [16]. Oedema volume at each interval was calculated. DL and MeDL (50–1000 mg/kg) were administered orally one hour before injecting inflammagen and the paw volume was measured at the time of peak inflammation, that is, 30 minutes for histamine-, serotonin-, and BK-induced inflammation, 1 hour in case of compound 48/80, 2 hours for PGE2-induced inflammation, and 3 hours in case of carrageenin-induced inflammation. The antiinflammatory activity was expressed as percent inhibition against the respective control. The antiinflammatory effect of DL and MeDL was compared with that of standard antiinflammatory drug phenylbutazone (PBZ, 100 mg/kg), antihistaminic drug chlorpheniramine (CPM, 3 mg/kg), antiserotonergic drug cyproheptadine (CPH, 3 mg/kg), and bradykinin-antagonist bradyzide (BZ 0.5 and 1.0 μmol/kg) administered orally.
Histological changes associated with carrageenin-induced rat paw oedema
Pedal oedema was induced by injecting 0.1 mL of 1% carrageenin suspension in NS into the subplantar surface of the rat hind paw. Rats were sacrificed at different time intervals using overdose of anaesthetic ether and the inflammed paw was cut at lateral malleolus and fixed in formalin solution. Paw sections of 10 μm were cut and stained with haematoxylin and eosin to observe the histological changes. The effect of crude DL (500 mg/kg), MeDL (500 mg/kg), and PBZ (100 mg/kg) were studied at 3 hours.
Statistical analysis
Values are expressed as mean ± SEM of six observations. Data was analysed by Student t test using computerised software SPSS (version 10). P ≤ .05 (a) and P ≤ .001 (b) were considered to be statistically significant.
RESULTS
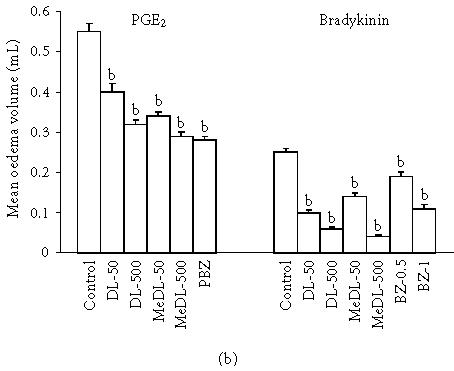
Temporal changes in paw volume produced by various inflammagens
Injection of various inflammagens into the subplantar surface of rat hind paw produced a marked increase in paw volume as compared to the saline control. While histamine, serotonin, and BK produced peak inflammation 30 minutes, the peak effect with compound 48/80, PGE2, and carrageenin was obtained at 1, 2, and 3 hours respectively (Figures 1a and 1b).
Figure 1.

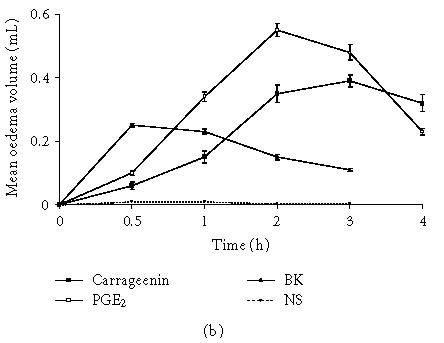
(a) Time course of inflammation induced by carrageenin, biogenic amines, compound 48/80, and NS in rat paw. Values given are mean ± SEM (n = 6). (b) Time course of inflammation induced by carrageenin, PGE2, BK, and NS in rat paw. Values given are mean ± SEM (n = 6).
Effect of DL, MeDL, and other antiinflammatory drugs on paw oedema
The inhibitory effect of DL, MeDL, and other antiinflammatory drugs on paw oedema formation was evaluated at the time of peak inflammation. Both DL and MeDL were more effective against carrageenin-induced oedema as compared to standard antiinflammatory drug PBZ. The oedema volumes in DL-50 and DL-500 groups were 0.13 ± 0.03 and 0.03 ± 0.01 mL against 0.39 ± 0.02 mL in the control group (67 and 92% inhibition). MeDL was less effective than crude DL and produced 46% and 62% inhibition of carrageenin-induced oedema. On the other hand antihistaminic drug, CPM, and antiserotonergic drug, CPH, produced marginal inhibitory effect (33% and 18% inhibition) against carrageenin-induced paw oedema (Figure 2a).
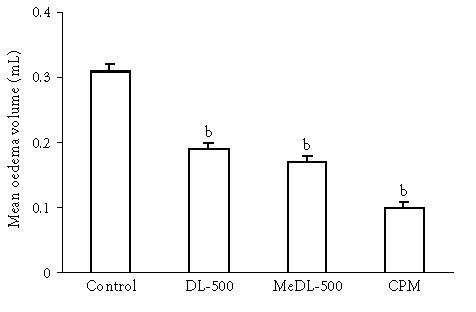
Figure 2.
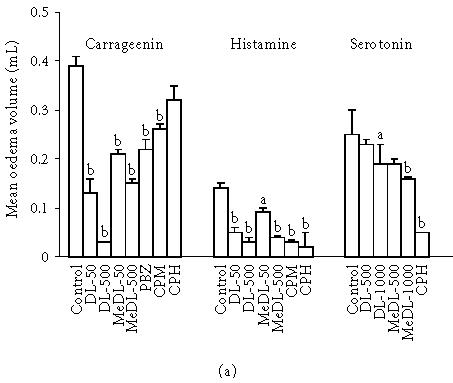
Antiinflammatory effect of DL and MeDL against inflammation induced by (a) carrageenin, histamine, and serotonin; (b) PGE2 and BK. Values given are mean ± SEM (n = 6). a denotes P ≤ .05; b denotes P ≤ .001.
We further tested the antiinflammatory effect of DL and MeDL against inflammation induced by biogenic amines. Both DL and MeDL produced a significant decrease in paw oedema induced by histamine (P < .001). The oedema volume in DL-50 and DL-500 was 0.05 ± 0.01 and 0.03 ± 0.01 mL against 0.14 ± 0.02 mL in the control group (64% and 79% inhibition). Similarly MeDL also produced 36% and 71% inhibition at 50 and 500 mg/kg doses. The inhibitory effect of DL and MeDL was comparable to that of CPM (79% inhibition). CPH, however, was more effective in this regard and produced 86% inhibition of histamine-induced paw oedema (Figure 2a). DL and MeDL produced marginal inhibition of oedema induced by serotonin (25%–35% inhibition) as against CPH that produced 80% inhibition (Figure 2a).
DL and MeDL were not so effective against PGE2-induced inflammation and the inhibitory effect of DL-500 and MeDL-500 was comparable to PBZ (42% and 47% versus 49% inhibition) (Figure 2b). Further, the inhibitory effect of DL and MeDL was more pronounced against BK-induced paw oedema as compared to BZ that produced 24% and 56% inhibition at 0.5 and 1.0 μmol/kg doses. DL-50 and DL-500 produced 60% and 76% inhibition while MeDL-50 and MeDL-500 produced 44% and 84% inhibition of BK-induced paw oedema (Figure 2b). The antiinflammatory effect of DL and MeDL was also tested against compound 48/80-induced inflammation. Both DL and MeDL significantly inhibited the compound 48/80-induced oedema formation (40%–45% inhibition) while CPM produced 68% inhibition (Figure 3).
Figure 3.
Antiinflammatory effect of DL and MeDL against inflammation induced by compound 48/80. Values given are mean ± SEM (n = 6); b denotes P ≤ .001.
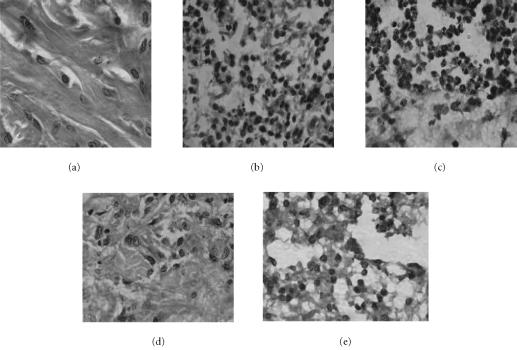
Effect of DL and MeDL on histological changes associated with carrageenin-induced rat paw oedema
Figure 4 shows the histological changes in the paw tissues following the subplantar injection of carrageenin and the antiinflammatory effect of DL and MeDL. The peak inflammatory response induced by carrageenin at 3 hours was found to be associated with subcutaneous oedema along with heavy infiltration of the inflammatory cells, particularly neutrophils, at the site of injection as compared to the control. Both DL and MeDL produced a significant decrease in the number of cellular infiltrates and their effect was comparable. However, DL was more potent in inhibiting the oedema formation as compared to MeDL. PBZ, a standard antiinflammatory drug, partially reduced the oedematogenic effects of carrageenin but did not affect the presence of the inflammatory cells.
Figure 4.
Antiinflammatory effect of DL and MeDL against carrageenin-induced cellular infiltration and oedema as revealed by histological sections: (a) normal, (b) carrageenin, (c) carrageenin + PBZ, (d) carrageenin + DL, (e) carrageenin + MeDL.
DISCUSSION
The latex of C procera has been demonstrated to possess potent antiinflammatory activity in various acute and chronic models of inflammation when administered orally [10]. The present study was carried out to characterise the antiinflammatory activity of DL against various inflammatory mediators using pharmacological reagents. Both DL and MeDL significantly inhibited carrageenin-induced paw oedema while PBZ, CPM, and CPH were not so effective, suggesting thereby that peak inflammatory response induced by carrageenin at 3 hours involves mediators other than biogenic amines. It has been well established that biogenic amines, histamine and 5-HT, are early mediators in carrageenin-induced inflammation while PG and BK play an important inflammatory role at the later hours [13]. We further evaluated the antiinflammatory effect of DL against early and late mediators of inflammation and compared it with respective antagonists. When tested against biogenic amines, DL and MeDL were found to be more effective against histamine-induced inflammation as compared to serotonin where they produced a marginal inhibitory effect. The antiinflammatory activity of DL and MeDL was comparable to antihistaminic drug CPM. CPH on the other hand was more effective in this regard due to its ability to inhibit histamine, serotonin, and BK [17]. The inhibitory effect of both DL and MeDL against PGE2 was comparable to that produced by PBZ. Since PBZ is known to produce inhibition of cyclooxygenase pathway, inhibition of PGE2-induced inflammation could be either due to inhibition of endogenous PG synthesis or due to its effect on vascular permeability [5]. It is interesting to note that DL and MeDL were more effective against BK-induced inflammation as compared to BZ that inhibits the effect of BK on B2 receptors [18]. This is also substantiated by the inhibitory effect of DL against carrageenin where BK plays an important role in mediating the inflammatory response [13]. It has been demonstrated that BK mediates its inflammatory response by the production and release of PGE2, histamine, and serotonin [19, 20].
As our results indicate that DL was effective against inflammation induced by histamine, we further tested the ability of DL to inhibit the action of histamine released from the mast cells. This was studied by inducing inflammation with compound 48/80 that is known to release endogenous histamine and serotonin stored in the mast cells [21]. Both DL and MeDL produced inhibitory effect on compound 48/80-induced inflammation to a similar extent and CPM was more active in this regard. As DL and MeDL were found to be more effective against inflammation induced by histamine as compared to serotonin, it is quite possible that the partial inhibition of inflammatory effect of compound 48/80 was due to the inhibition of histamine and the effect of serotonin released from the mast cells was not completely blocked.
Paw oedema induced by carrageenin, a widely used inflammagen, was associated with marked oedema and neutrophil infiltration at 3 hours as revealed by histological sections. Though DL and MeDL were equieffective in inhibiting cellular infiltration, DL was more effective in inhibiting carrageenin-induced oedema. This is also corroborated by our findings on the inhibitory effect of DL and MeDL on the paw volume. The greater efficacy of DL could be attributed to constituents present in DL other than those present in MeDL. Both DL and MeDL were found to be more effective than standard antiinflammatory drug PBZ in inhibiting cellular infiltration. Thus, our study indicates that DL, by virtue of its ability to inhibit both oedema as well as cellular infiltration, could be used as a promising antiinflammatory agent.
ACKNOWLEDGMENT
Soneera Arya is a Senior Research Fellow of the Council of the Scientific and Industrial Research, New Delhi, India.
References
- 1.Tomar VP, Agarwal PK, Agarwal BL. Toxic iridocyclitis caused by Calotropis procera. J All India Ophthalmol Soc. 1970;18(1):15–16. [PubMed] [Google Scholar]
- 2.Handa F, Sadana JK, Sharma PK. Allergic contact dermatitis due to the plant Calotropis procera (Vern: AK). A case report. Indian J Dermatol. 1984;29(3):27–29. [PubMed] [Google Scholar]
- 3.Biedner B, Rothkoff L, Witzum A. Calotropis procera (Sodom apple) latex keratoconjunctivitis. Isr J Med Sci. 1977;13(9):914–916. [PubMed] [Google Scholar]
- 4.Singh H, Kumar S, Dewan S, Kumar VL. Inflammation induced by latex of Calotropis procera—a new model to evaluate anti-inflammatory drugs. J Pharmacol Toxicol Methods. 2000;43(3):219–224. doi: 10.1016/s1056-8719(00)00105-2. [DOI] [PubMed] [Google Scholar]
- 5.Shivkar YM, Kumar VL. Histamine mediates the pro-inflammatory effect of latex of Calotropis procera in rats. Mediators Inflamm. 2003;12(5):299–302. doi: 10.1080/096293503310001619708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Shivkar YM, Kumar VL. Effect of anti-inflammatory drugs on pleurisy induced by latex of Calotropis procera in rats. Pharmacol Res. 2004;50(3):335–340. doi: 10.1016/j.phrs.2004.01.011. [DOI] [PubMed] [Google Scholar]
- 7.Kumar VL, Shivkar YM. Involvement of prostaglandins in inflammation induced by latex of Calotropis procera. Mediators Inflamm. 2004;13(3):151–155. doi: 10.1080/09511920410001713583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.CSIR Publication and Information . Wealth of India: Raw materials III. New Delhi, India: CSIR Publication and Information Directorate; 1992. pp. 78–84. [Google Scholar]
- 9.Kumar VL, Basu N. Anti-inflammatory activity of the latex of Calotropis procera. J Ethnopharmacol. 1994;44(2):123–125. doi: 10.1016/0378-8741(94)90078-7. [DOI] [PubMed] [Google Scholar]
- 10.Sangraula H, Dewan S, Kumar VL. Evaluation of anti-inflammatory activity of latex of Calotropis procera in different models of inflammation. Inflammopharmacol. 2002;9(3):257–264. [Google Scholar]
- 11.Dewan S, Sangraula H, Kumar VL. Preliminary studies on the analgesic activity of latex of Calotropis procera. J Ethnopharmacol. 2000;73(1-2):307–311. doi: 10.1016/s0378-8741(00)00272-5. [DOI] [PubMed] [Google Scholar]
- 12.Dewan S, Kumar S, Kumar VL. Antipyretic effect of latex of Calotropis procera. Indian J Pharmacol. 2000;32:252. [Google Scholar]
- 13.Di Rosa M, Giroud JP, Willoughby DA. Studies on the mediators of the acute inflammatory response induced in rats in different sites by carrageenan and turpentine. J Pathol. 1971;104(1):15–29. doi: 10.1002/path.1711040103. [DOI] [PubMed] [Google Scholar]
- 14.Vogel GH, Vogel WH. Drug Discovery and Evaluation. Pharmacological Assays. New York, NY: Springer; 1997. Anti-inflammatory activity; pp. 406–409. [Google Scholar]
- 15.Campos MM, Calixto JB. Involvement of B1 and B2 receptors in bradykinin-induced rat paw oedema. Br J Pharmacol. 1995;114(5):1005–1013. doi: 10.1111/j.1476-5381.1995.tb13305.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Winter CA, Risley EA, Nuss GW. Carrageenin-induced edema in hind paws of the rat as an assay for anti-iflammatory drugs. Proc Soc Exp Biol Med. 1962;111:544–547. doi: 10.3181/00379727-111-27849. [DOI] [PubMed] [Google Scholar]
- 17.Reylon V, Siddiqui HH. Anti-spasmogenic effect of cyproheptadine on guinea-pig ileum. Indian J Physiol Pharmac. 1983;27(4):342–344. [PubMed] [Google Scholar]
- 18.Burgess GM, Perkins MN, Rang HP, et al. Bradyzide, a potent non-peptide B(2) bradykinin receptor antagonist with long-lasting oral activity in animal models of inflammatory hyperalgesia. Br J Pharmacol. 2000;129(1):77–86. doi: 10.1038/sj.bjp.0703012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hall JM. Bradykinin receptors pharmacological properties and biological roles. Pharmacol Ther. 1992;56(2):131–190. doi: 10.1016/0163-7258(92)90016-s. [DOI] [PubMed] [Google Scholar]
- 20.Burch RM, Kyle DJ, Stromenn TM. In: Molecular Biology and Pharmacology of Bradykinin Receptors. Burch RM, editor. Austin, Tex: RG Landes Co; 1993. [Google Scholar]
- 21.Irman-Florjanc T, Erjavec F. Compound 48/80 and substance P induced release of histamine and serotonin from rat peritoneal mast cells. Agents Actions. 1983;13(2-3):138–141. doi: 10.1007/BF01967317. [DOI] [PubMed] [Google Scholar]