Abstract
Dysregulated psychophysiological responses have been observed in patients with fibromyalgia syndrome (FMS), although the results are inconsistent. Surface electromyographic (EMG), systolic and diastolic blood pressure, heart rate (HR), and skin conductance levels (SCLs) were continuously recorded at baseline, and during a series of stress and relaxation tasks in 90 FMS patients and 30 age and sex matched healthy controls (HCs). The patient sample demonstrated lower baseline EMG levels compared to the HCs on all tasks. In contrast, the patients displayed elevated HR and SCL (sympathetic vasomotor and sudomotor indices, respectively) during both stress tasks. A cluster analysis identified four psychophysiological response patterns: 63.3% of HCs showed increased muscle tension and stable cardiovascular responses; 34.8% of FMS patients showed a pattern of increased sympathetic vasomotor reactivity with stable sudomotor and reduced muscular response; 12.2% of FMS patients showed a pattern of increased sympathetic sudomotor reactivity connected with increased sympathetic vasomotor response and reduced muscular response; and, in contrast, 46.7% of FMS patients showed a pattern of parasympathetic vasomotor reactivity and reduced sudomotor as well as muscular response. The identification of low baseline muscle tension in FMS is discrepant with other chronic pain syndromes and suggests that unique psychophysiological features may be associated with FMS. The different psychophysiological response patterns within the patient sample support the heterogeneity of FMS.
Introduction
Fibromyalgia syndrome (FMS) is defined as widespread pain combined with tenderness at 11 or more of 18 specific 'tender points' [1]. There is no consensus regarding the mechanisms underlying the set of symptoms reported by FMS sufferers. Additionally, several studies suggest heterogeneity in the diagnosis of FMS. For example, subgroup differences in biological variables such as positive antinuclear antibodies connected with features of connective tissue disease, interleukin 1β, interleukin-6, and tumor necrosis factor-alpha in skin (for example, see [2-4]), depression and cytokine abnormalities (for example, see [5,6]), and responses to pharmacological interventions (for example, see [7,8]) have been reported. Subgroups based on psychosocial responses have also been demonstrated [9]. Although abnormal responses to stress have been suggested to occur through a pathophysiological mechanism [10], research examining the influence of stress in FMS has yielded inconsistent results.
The majority of published studies evaluated the responses of the autonomic nervous system to physical stressful situations. This approach was used to test stress-reactivity as a potential cause of the maintenance of FMS symptoms. Several studies reported increased skin conductance levels (SCLs) [11], decreased heart rate (HR) variability [12], blood pressure (BP), and skin temperature [11] in response to physical stressors. These studies suggest an association between FMS and neurally mediated hypotension [13].
Although several studies that investigated surface electromyographic (EMG) activity failed to find differences between FMS patients and healthy controls (HCs) [14,15], others reported lower than average muscle tension levels in FMS patients in contrast to HCs during isometric exercises (for example, see [16,17]), following injection of hypertonic saline, or in antagonistic muscles [18,19]. Our own study used psychological stressors (for example, mental and social stress), and measured a complex physiological pattern consisting of EMG levels, BP, HR and SCLs. FMS patients displayed reduced muscle tension and increased heart rate. In contrast, HCs showed a modest HR response to stress. Furthermore, as a group the FMS patients demonstrated significant variability in stress reactivity and thus do not appear to be a homogeneous group when it comes to stress reactivity [20,21].
These results support the suggestion of autonomic response specificity [22,23] as an explanation for the different response patterns observed in FMS. Furthermore, the results suggest that patients who have the same diagnosis may have different psychophysiological response patterns.
The primary aim of the present study was to identify psychophysiological characteristics of FMS patients by examining BP, HR, SCLs, and surface EMG levels during baseline (BL) and stress conditions [23]. Based on the assumption of heterogeneity (for example, see [3,5,8,9]) and the studies by Qiao and colleagues. [11], Graven-Nielson and colleagues. [18], Sorensen and colleagues. [19], and Sprott and colleagues. [24], and our own study [20], we predicted enhanced autonomic system (for example, SCL, HR, and BP) responses, and lowered muscle tension (for example, EMG levels) and different psychophysiological response patterns within the FMS sample.
Materials and methods
Participants
Ninety female FMS patients recruited from a pain clinic, rheumatology outpatient departments and a hospital and thirty age and sex-matched HCs recruited from acquaintances of the investigated patients participated in the study. All patients met the American College of Rheumatology FMS criteria [1]. The exclusion criteria consisted of: inflammatory cause of the pain; neurological complications; pregnancy; concomitant severe disease; intake of muscle relaxants and opioids; major psychiatric disorder; and lack of language fluency. An institutional review board approved the study, which adhered to the Declaration of Helsinki and informed consent was obtained from all study participants.
Table 1 contains demographic and diagnostic information about the FMS patients and HCs. The sex-matched female HCs and FMS patients were comparable with respect to age and occupational status despite the fact that 25% of the FMS patients were receiving workers' compensation (chi(4) = 8.52, p = 0.074).
Table 1.
Demographic and clinical variables of the fibromyalgia syndrome patients and healthy controls
| FMS (n = 90) (mean ± SD (range)) | HC (n = 30) (mean ± SD (range)) | |
| Age (years) | 48.17 ± 10.32 (21–68) | 48.22 ± 9.02 (22–65) |
| Duration of pain (years) | 9.28 ± 9.23 (0.5–45) | |
| Painful regions | 6.80 ± 2.05 (3–12) | |
| Number of tender points | 16.09 ± 3.33 (14–18) | 2 ± 0.33 (0–4) |
| Mean tender points pain severitya | 5.89 ± 2.27 (2–10) | 3.13 ± 1.06 (0–3) |
| Use of antidepressive medications (number) | 0.36 ± 0.52 (0–3) | 0.21 ± 0.03 (0–2) |
| Occupational status | N (%) | N (%) |
| Working | 39 (43.3) | 17 (56.8) |
| Unemployed | 20 (22.2) | 9 (30.0) |
| Workers' compensation | 24 (26.7) | 0 (0.0) |
| Retired | 6 (6.7) | 2 (6.6) |
| Student | 1 (1.1) | 2 (6.6) |
aVisual analogue scale ranges from 0 = no pain to 10 = most intense pain. FMS, fibromyalgia syndrome; HC, healthy control; SD, standard deviation.
Procedure
Clinical assessment
A physician performed an examination that included laboratory measures (for example, rheumatoid factor, antinuclear antibodies, erythrocyte sedimentation rate), and the evaluation of tender points (manual tender point survey [25]) on all FMS patients. The manual tender point survey was also performed on the HCs.
Psychophysiological assessment
Patients and HCs were instructed not to consume any analgesic or antidepressant medication for one day prior to their scheduled psychophysiological assessment. A 90 minute psychophysiological protocol was conducted subsequent to the medical and psychological assessments. The protocol consisted of 7 phases (Figure 1):
Figure 1.
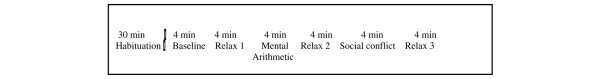
The design of the study.
1. Adaptation (30 minutes): sitting quietly in a chair with eyes open.
2. Resting BL (4 minutes): sitting quietly with eyes open and to move as little as possible.
3. Relaxation (REL1, 4 minutes): pleasant music played through headphones with eyes closed.
4. Mental arithmetic (MA, 4 minutes): add 10 one-figure numbers in the presence of white noise (60 db). On 30% of the answers the participants were informed that their answer was 'incorrect' independent of their response. An additional white noise (60 db) stressor was delivered to the participants through headphones.
5. REL2: as described in 3.
6. Social conflict (SC, 4 minutes): discuss a SC from the list of unsolvable problems identified during the initial assessment [26].
7. REL3: as described in 3.
The stressor conditions were presented in a counter-balanced order to reduce any order effects.
Immediately following each phase, participants were asked to rate the intensity of their pain and perceived stress on an 11 point scale with the endpoints 'no pain' to 'very intense pain', and 'not at all stressful' to 'very stressful'.
Psychophysiological recordings
Participants were seated and positioned in a straight back chair and were instructed to move as little as possible. A video camera located in the experimental room was activated throughout the psychophysiology protocol. All instructions were presented on a video screen.
EMG activity was recorded from the left and right m. trapezius according to the positioning recommended by Fridlund and Cacioppo [27]. BP was continuously monitored using an Ohmeda Finapres BP monitor (Datex-Ohmeda, Louisville, CO, USA). A MEDAT 6020 B Amplifier (Insight Instruments, Vienna, Austria) was used to record EMG, SCL, and HR. The presentation of the instructions, data acquisition, and data storage were computer-controlled. The sampling frequency of EMG signals was 3,000 Hz. The raw EMG was amplified by a factor of 100,000, passed through a bandpass filter (25 to 1,000 Hz), and integrated using contour-following integrators with a time constant of 70 ms.
BP was measured with a photoplethysmographic device on the fourth digit of the left hand (the accuracy of this procedure is ± 2 mmHg ± 0.25 kPa). A computer program that summed the digitized beat-by-beat waveforms averaged the sample time synchronized to the R-wave of the electrocardiogram, and divided them by the number of cardiac cycles. HR was determined with a multi-miniature transmitter using photoplethysmography of HR waveforms positioned on the tip of the fourth digit of the right hand. HR in beats per minutes was determined from this calculation [28]. SCL was measured through two electrodes in a multi-miniature sensor with a surface of 50.3 mm2 on the second digit of the right hand about a constant current procedure of 4 μA [29,30]. All physiological measurements were continuously recorded like a 24 h BP monitoring.
Data analysis
Data analyses were performed in several sequential steps. The first analyses assessed BL differences between the FMS and HC groups for the self-report and the psychophysiological variables. The second step examined differences in psychophysiological responses by the FMS and HC groups, using repeated measures analyses of variance (ANOVAs or ANCOVAs) depending on baseline differences with all six phases as within and the two groups as between factors. Significant ANOVA and ANCOVA effects were followed up by post hoc t tests in a third step. These post hoc analyses were used to calculate: (1) group differences over all six phases; (2) differences between the phases across both groups in order to test the stress induction; and (3) between group differences in stress reactivity. The stress and the relaxation phases were compared with the baseline for each group in the case of comparable baseline values. When there were baseline differences between the groups, ANCOVAs were performed. Significant effects were followed up by post hoc t tests to compare relaxation with stress phases. Bonferroni corrections were used to control for the large number of analyses (p < 0.005).
To identify psychophysiological response patterns we performed a z-transformation of all psychophysiological variables to create a common metric and thereby permit integration of the data as a fourth step. The z-transformations were performed for the overall sample to permit comparison of FMS patients and HCs. Finally, in order to examine the heterogeneity in physiological responding between and within the FMS and HC group, we performed a k-means cluster analysis [31]. The cluster analyses with z-transformed physiological variables permits identification of groups within the sample, the so-called 'psychophysiological patterns', and allows determination of the most stress-reactive physiological variable for each psychophysiological pattern. The cluster analysis used the means of all z-transformed physiological data collected during the BL, stress, and relaxation phases. The cluster analysis reveals an order of different psychophysiological variables with comparable z-scores. The variable with the highest z-score in each cluster characterizes the most reactive physiological system. The algebraic sign shows the direction of the stress response [32].
Results
Pain and stress response
Subjective pain ratings
As the BL pain ratings varied between the groups, an ANCOVA was performed. The results of this analyses revealed a significant main effect for groups (F(1,118) = 26.14, p < 0.001), indicating significantly higher pain ratings in the patient group than the HCs. A significant phase effect (F(5,114) = 7.79, p < 0.001) revealed that the pain ratings were higher in the stress than the REL phases (all ps < 0.01). The significant group × phase interaction (F(5,114) = 6.69, p < 0.001) indicated significant differences in pain ratings across phases for all FMS patients and the HCs controlled by covariate BL pain ratings.
Subjective stress ratings
As the BL values were different between groups (FMS and HC), an ANCOVA was performed with the BL scores as the covariate. The results of this analyses revealed that the group (F(1,118) = 52.27, p < 0.001), phase (F(5,114) = 32.43, p < 0.001), and a group × phase interaction (F(5,114) = 7.56, p < 0.001) were all statistically significant. FMS patients displayed significantly higher stress ratings than the HCs (all ps < 0.001; Table 2). The stress ratings were significantly higher in the stress compared to the REL phases (all ps < 0.001) controlled by covariate BL stress ratings.
Table 2.
Comparison of self-reported pain and stress between fibromyalgia syndrome patients and healthy controls
| Phase | FMS (N = 90) | HC (N = 30) | p value | ||
| Mean | SD | Mean | SD | ||
| Pain | |||||
| Baseline | 4.70 | (2.30) | 0.00 | (0.00) | <0.001 |
| Relax 1 | 4.75 | (2.14) | 0.00 | (0.00) | <0.001 |
| Arithmetic | 5.60 | (2.19) | 0.07 | (0.25) | <0.001 |
| Relax 2 | 5.33 | (1.70) | 0.00 | (0.00) | <0.001 |
| Conflict | 5.63 | (2.03) | 0.34 | (0.71) | <0.001 |
| Relax 3 | 5.40 | (1.79) | 0.23 | (0.50) | <0.001 |
| Stress | |||||
| Baseline | 2.65 | (0.92) | 1.17 | (0.79) | <0.001 |
| Relax 1 | 2.22 | (0.85) | 0.17 | (0.38) | <0.001 |
| Arithmetic | 4.70 | (2.01) | 2.37 | (0.72) | <0.001 |
| Relax 2 | 3.10 | (1.10) | 0.10 | (0.31) | <0.001 |
| Conflict | 5.60 | (1.88) | 3.33 | (1.03) | <0.001 |
| Relax 3 | 3.04 | (0.98) | 0.57 | (0.68) | <0.001 |
FMS, fibromyalgia syndrome; HC, healthy controls; SD, standard deviation.
Psychophysiological data
Electromyographic changes
There were no significant differences between the left and right trapezius across any of the phases, thus combined means are reported. As the between group BL values were significantly different, an ANCOVA was performed. The group main effect (F(1,118) = 10.29, p < 0.005) was significant. FMS patients displayed significantly lower trapezius EMG activity than the HCs (p < 0.001). There were no statistically significant differences in EMG between BL, stress, and REL phases for either group when BL EMG was used as a covariate (Table 3).
Table 3.
Differences in physiological variables between fibromyalgia syndrome patients and healthy controls
| Phase | FMS (N = 90) | HC (N = 30) | p value | ||
| Mean | SD | Mean | SD | ||
| EMG | |||||
| Baseline | 8.97 | (4.75) | 14.52 | (5.12) | <0.001 |
| Relax 1 | 8.77 | (4.83) | 15.83 | (5.23) | <0.001 |
| Mental arithmetic | 10.44 | (5.89) | 17.10 | (9.07) | <0.001 |
| Relax 2 | 8.91 | (4.91) | 17.60 | (9.44) | <0.001 |
| Social conflict | 9.59 | (5.59) | 17.04 | (8.92) | <0.001 |
| Relax 3 | 9.63 | (6.33) | 18.50 | (10.51) | <0.001 |
| SCL | |||||
| Baseline | 1.81 | (1.70) | 1.65 | (0.64) | ns |
| Relax 1 | 1.89 | (1.78) | 1.59 | (0.62) | ns |
| Mental arithmetic | 2.81 | (2.65) | 1.92 | (0.74) | <0.005 |
| Relax 2 | 2.31 | (2.01) | 1.76 | (0.69) | ns |
| Social conflict | 2.76 | (2.11) | 1.79 | (0.72) | <0.005 |
| Relax 3 | 2.41 | (2.15) | 1.69 | (0.71) | ns |
| HR | |||||
| Baseline | 77.07 | (11.22) | 68.56 | (22.49) | ns |
| Relax 1 | 75.45 | (10.54) | 65.68 | (21.11) | <0.005 |
| Mental arithmetic | 78.32 | (13.64) | 75.85 | (24.72) | ns |
| Relax 2 | 73.36 | (10.86) | 66.47 | (19.55) | ns |
| Social conflict | 77.88 | (10.64) | 66.85 | (20.88) | ns |
| Relax 3 | 73.96 | (9.59) | 62.79 | (18.11) | <0.005 |
| SBP | |||||
| Baseline | 133.5 | (19.03) | 132.9 | (13.40) | ns |
| Relax 1 | 131.4 | (16.65) | 130.4 | (11.58) | ns |
| Mental arithmetic | 141.7 | (19.52) | 140.8 | (14.35) | ns |
| Relax 2 | 128.1 | (13.20) | 124.9 | (21.00) | ns |
| Social conflict | 146.5 | (15.09) | 139.7 | (18.29) | ns |
| Relax 3 | 135.6 | (14.31) | 131.9 | (23.38) | ns |
| DBP | |||||
| Baseline | 78.43 | (13.89) | 77.10 | (8.83) | ns |
| Relax 1 | 76.23 | (8.27) | 76.24 | (7.79) | ns |
| Mental arithmetic | 81.11 | (10.80) | 82.51 | (10.83) | ns |
| Relax 2 | 76.82 | (14.54) | 73.37 | (7.61) | ns |
| Social conflict | 85.81 | (9.33) | 83.74 | (10.29) | ns |
| Relax 3 | 77.57 | (7.75) | 78.04 | (9.60) | ns |
DBP, diastolic blood pressure; EMG, electromyographic activity; FMS, fibromyalgia syndrome; HC, healthy controls; HR, heart rate; ns, not significant; SBP, systolic blood pressure; SCL, skin conductance level.
Skin conductance level
A statistically significant phase effect (F(5,114) = 7.49, p < 0.001) indicated higher SCLs in the stress than the REL phases (all ps < 0.001). The significant group × phase interaction (F(5,114) = 3.84, p < 0.005) indicated that the FMS patients showed a significant increase from BL to REL1, and a significant increase from BL to MA and SC phases, in contrast to HC with no significant changes (Table 3).
Heart rate
HR showed a statistically significant group main effect (F(3,116) = 14.94, p < 0.001), indicating higher HR in FMS patients compared to the HCs (p < 0.001). The significant phase effect (F(5,114) = 15.08, p < 0.001) showed that HR increased in stress and decreased in REL phases across all FMS subgroups and the HCs (p < 0.001) (Table 3).
Blood pressure
A statistically significant phase effect (systolic blood pressure (SBP), F(5,114) = 30.92, p < 0.001; diastolic blood pressure (DBP), F(5,114) = 41.95, p < 0.001) indicated that SBP and DBP increased in stress and decreased in REL phases across the groups (p < 0.001). In contrast to SBP, DBP showed a statistically significant group × phase interaction (F(5,115) = 4.16, p < 0.005). The level of DBP in FMS patients decreased from BL to REL1 (p < 0.001), and increased from BL to MA and SC (all, ps < 0.001). The level of DBP increased in HCs from BL to MA and SC (all, ps < 0.005) (Table 3).
Psychophysiological patterns
Characteristics of psychophysiological response patterns
The k-means cluster analysis (Table 4) yielded four clusters. The means of SBP (p < 0.001), DBP (p < 0.001), HR (p < 0.01), SCL (p < 0.001), and EMG (p < 0.001) were significantly different between the psychophysiological patterns (Table 4). The largest psychophysiological subgroup (n = 48) was characterized by a low autonomic and muscular response pattern with reduced SBP, DBP and HR and by very low SCLs and EMG levels. The low BP was the most reactive physiological system of the largest psychophysiological response pattern (for example, hypotensive reactivity). The second subgroup (n = 39) showed a high cardiovascular response pattern with elevated DBP, SBP, and HR, a moderate SCL response, and reduced EMG levels. The high BP was the most reactive physiological system. Elevated EMG levels and average responses in all other physiological data characterized the third subgroup (n = 22) with an enhanced muscular reactivity. The fourth pattern (n = 11) was characterized by a high autonomic and low muscular response pattern with high SCLs, increased cardiovascular variables and reduced EMG levels. The smallest pattern was characterized by SCL reactivity. The low autonomic and muscular stress response pattern with hypotensive BP reactivity was shown by 46.7% of FMS patients. The high cardiovascular response pattern with enhanced BP reactivity was shown by 37.8%, and the high SCL pattern with SCL reactivity by 12.2% of FMS patients. The high muscular response pattern with enhanced muscle reactivity was shown by 63.3% of HCs in contrast to only 3.3% of FMS patients (Table 5).
Table 4.
Z-scores of the four psychophysiological response patterns
| Variable | Physiological response pattern | F | p value | |||
| 1 | 2 | 3 | 4 | |||
| Z-DBP-M | -0.69 | 0.70 | 0.18 | 0.48 | 31.044 | <0.001 |
| Z-SBP-M | -0.71 | 0.65 | 0.14 | 0.57 | 38.079 | <0.001 |
| Z-HR-M | -0.02 | 0.45 | -0.04 | 0.21 | 4.612 | 0.005 |
| Z-SCL-M | -0.43 | -0.10 | -0.18 | 2.71 | 131.298 | <0.001 |
| Z-EMG-M | -0.22 | -0.35 | 1.34 | -0.40 | 43.799 | <0.001 |
Bold text indicates the highest values of each group. DBP, diastolic blood pressure; EMG, electromyographic activity; HR, heart rate; SBP, systolic blood pressure; SCL, skin conductance level.
Table 5.
Psychophysiological response patterns in fibromyalgia syndrome patients and healthy controls
| Group | PRP1 | HC (N = 30) | FMS (N = 90) | Total | |||
| N | % | N | % | N | % | ||
| 1 | Low BP | 6 | 20.0 | 42 | 46.7 | 48 | 40.0 |
| 2 | High BP | 5 | 16.7 | 34 | 37.8 | 39 | 32.5 |
| 3 | High EMG | 19 | 63.3 | 3 | 3.3 | 22 | 18.3 |
| 4 | High SCL | 0 | 0.0 | 11 | 12.2 | 11 | 9.2 |
| Total | 30 | 100.0 | 90 | 100.0 | 120 | 100.0 | |
Bold text indicates the highest values of each group. 1Psychophysiological response patterns: Low BP: low systolic blood pressure (SBP), diastolic blood pressure (DBP), heart rate (HR), skin conductance level (SCL) and electromyographic activity (EMG); High BP: enhanced SBP, DBP, HR as well as moderate SCL and low EMG; High EMG: enhanced EMG as well as stable physiological response; High SCL: enhanced SCL as well as enhanced BP, moderate HR and reduced EMG. HC, healthy control; FMS, fibromyalgia syndrome.
Associations between psychophysiological response and self-reported measures
An ANOVA showed significant differences between the psychophysiological response patterns in pain (all F(3,117) = 7.46–12.31, p < 0.001) and stress ratings (F(3,117) = 4.06–13.25, p < 0.01) for all phases, as well as in the duration of pain (F(3,117) = 3.38, p < 0.05), although the latter two did not reach the Bonferroni-adjusted levels of statistical significance.
The high muscle response pattern showed significantly lower pain (p < 0.001), and the shortest duration of pain (p < 0.005) in contrast to the other psychophysiological response patterns (Table 6). There were no significant differences in pain and stress ratings between the other psychophysiological response patterns.
Table 6.
Self-reported pain and stress during the experiment and significant differences between psychophysiological response patterns
| Phase | Low BP (N = 48) | High BP (N = 39) | High EMG (N = 22) | High SCL (N = 11) | Significant difference | |||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | F | p | |
| Pain | ||||||||||
| Baseline | 3.36 | (2.46) | 3.73 | (2.53) | 1.00 | (2.05) | 5.17 | (3.19) | 7.46 | <0.001 |
| Relax 1 | 3.18 | (2.45) | 3.39 | (2.32) | 0.92 | (1.90) | 5.06 | (3.06) | 7.52 | <0.001 |
| Arithmetic | 4.02 | (2.86) | 4.61 | (2.56) | 0.95 | (1.93) | 6.11 | (3.06) | 11.02 | <0.001 |
| Relax 2 | 3.64 | (2.50) | 4.26 | (2.48) | 0.95 | (2.04) | 5.50 | (2.84) | 10.12 | <0.001 |
| Conflict | 3.88 | (2.51) | 4.69 | (2.67) | 0.92 | (2.02) | 6.06 | (3.00) | 12.12 | <0.001 |
| Relax 3 | 4.15 | (2.56) | 4.43 | (2.31) | 1.00 | (2.00) | 6.17 | (3.10) | 12.30 | <0.001 |
| Stress | ||||||||||
| Baseline | 2.40 | (1.18) | 2.31 | (0.95) | 1.58 | (0.96) | 3.11 | (1.96) | 4.06 | 0.009 |
| Relax 1 | 1.79 | (0.99) | 2.00 | (1.13) | 0.47 | (0.84) | 3.11 | (1.96) | 13.25 | <0.001 |
| Arithmetic | 4.40 | (2.32) | 4.84 | (1.84) | 3.00 | (1.20) | 5.94 | (2.21) | 5.52 | 0.001 |
| Relax 2 | 2.57 | (1.55) | 2.69 | (1.37) | 0.53 | (1.07) | 3.44 | (1.88) | 12.81 | <0.001 |
| Conflict | 5.25 | (1.94) | 6.08 | (2.09) | 3.84 | (1.77) | 6.56 | (2.24) | 6.41 | 0.001 |
| Relax 3 | 2.83 | (1.53) | 2.62 | (1.23) | 1.00 | (1.11) | 3.33 | (2.23) | 8.75 | <0.001 |
| Duration of pain | 8.35 | (10.61) | 7.16 | (6.80) | 1.33 | (3.24) | 5.33 | (2.54) | 3.38 | 0.022 |
BP, blood pressure; EMG, electromyographic activity FMS, fibromyalgia syndrome; HC, healthy controls; SCL, skin conductance level; SD, standard deviation.
Discussion
The results of this study demonstrate different physiological stress responses within FMS patients and between FMS patients and HC. The significant increase of BP, HR, and SCLs in the stress compared to the BL phase and the reduction in the REL phases indicates that stress and relaxation were induced, confirming the ecological validity of the stressors (compare to [33]).
Consistent with other studies [18,34], in the FMS patients, muscle tension at the BL and the experimental phases were significantly lower compared to the HCs. Moreover, although the FMS patients rated the SC and MA tasks as stressful, their muscle tension levels did not display elevations comparable to the HCs. It appears that neither mental stress nor pain intensity influence muscle tension in FMS patients.
Studies with P magnetic resonance imaging have reliably identified several abnormalities in the muscles of patients with FMS, including low levels of phosphocreatine and ATP at rest, low phosphorylation potential and total oxidative capacity, and a reduced number and size of mitochondria [23,35]. Additionally, the slower degradation of acetylcholine [36], which is involved in the production of corticosteroids and growth hormones [10,36], is an important regulator of muscle remodeling and performance [37]. Taken together, the results of the present study and other physiological studies [16-19,32] suggest that FMS is characterized by decreased muscle activity connected with an inability to respond adaptively to stress and relaxation. The reason for the decreased muscle activity in FMS does not appear to be only the result of physical deconditioning; ultrastructural changes in the muscle also appear to be involved [23,31]. Further investigations are needed to examine the interactions between muscle and the endocrine [37] and central nervous systems [38].
The four psychophysiological stress response patterns identified differentiated among the FMS sample and the HCs. The HCs were included to examine the diagnosis specificity of each of the FMS patterns. If the HCs had not been included in the analyses, it would not have been possible to interpret the three psychophysiological FMS patterns as we would not have known whether any of these three clusters reflected a normal stress reaction. The inclusion of the HCs permitted us to demonstrate that the FMS patterns were all completely different when compared to the response pattern showed by the HCs.
These differences are important because autonomic variables may be involved in the development and maintenance of chronic disease [21,22]. Flor and colleagues [39] found increased muscle reactivity in back pain patients following a psychological stress induction. Johannes and colleagues [32] found greater BP reactivity in patients with hypertension compared to HCs. The largest percentage of the FMS sample (46.7%) in the present study showed hypotensive reactivity within a stress response pattern that is characterized by decreased cardiovascular, SCL, and EMG values. The significantly lower BP suggests that the influence of parasympathetic reactivity may be extended during stress situations. Based on the the endocrine influence on the autonomic nervous system [40-42] and the central sensitization of FMS [43], a parasympathetic response pattern seems to be connected with the enhanced adrenocorticotrophic hormone production described in FMS (for example, see [10,36]).
The second largest response pattern (37.8%) of FMS patients was exemplified by increased BP reactivity. Increased cardiovascular stress responses and decreased SCLs and EMG levels also characterized this response pattern. The increased cardiac response suggests a tendency for higher peripheral sympathetic tones under stress. This psychophysiological response pattern replicates the results reported by Martinez-Lavin [44], who discussed FMS as a sympathetically maintained pain syndrome. Increased DBP appears to be connected to pain intensity (r = 0.32, p < 0.05). It is comparable to the stress response observed in rheumatoid arthritis patients who also showed enhanced BP reactivity [32]. Additional studies are necessary to confirm these results and to determine the mechanisms underlying these patterns.
The third largest response pattern of FMS (12.2%) was characterized by elevated SCL reactivity as sympathetic sudomotor reactivity and increased cardiovascular response as sympathetic vasomotor response as well as the FMS specific reduction in muscle tension. Patients with acute musculoskeletal injury also showed elevated sympathetic vaso- and sudomotor responses [45]. These sympathetic response patterns suggest that there is an interaction between cutaneous and vasomotor sympathetic neurons in response to acute musculoskeletal injury or to chronic pain. This is reflected by increased afferent input from sensitized nociceptors and other sensory neurons, resulting in alterations in autonomic function [45].
Johannes and colleagues [32] also found sympathetic and parasympathetic response patterns in the comparison of patients with hypertension, rheumatoid arthritis, and systemic lupus erythematosus. As the sympathetic and parasympathetic response patterns are present in FMS as well, it may be that these response patterns are relatively independent of the specific disease entity.
Moreover, the patients were medication-free only one day before the study. It is known that antidepressant medication affects autonomic nervous system activity. However, a comparison of the physiological stress responses of the subgroups of patients with (n = 20) and without (n = 60) antidepressant medication did not yield significant effects (parasympathetic DBP, t(46) = 0.08, p = 0.94); sympathetic stress response t(37) = 1.15, p = 0.26). Antidepressant use was not associated with altered stress response. Further, the physiological response did not show significant differences between patients with and without antidepressant use.
Conclusion
The results of this study support the suggestion of heterogeneity of the mechanisms involved in FMS. They suggest further that differential treatment strategies matched to different patterns may be appropriate [46,47].
Although the overall sample size for the patient group appears reasonable, subdividing the total sample into four psychophysiological patterns produced relatively small groups. Thus, the interpretation of the results of the cluster analysis on the subgroups must be treated with caution. Research with larger samples is needed to replicate autonomic response specificity observed in the different psychosocial subgroups. Moreover, studies are needed to compare the psychophysiological reactivity in FMS with other chronic pain conditions to determine if the patterns observed are unique to FMS or are characteristic of chronic pain. Further, future research is needed to test endocrine predictors of stress reactivity in FMS to determine if the endocrine reaction is the cause or the consequence of FMS.
Abbreviations
BL = baseline phase; BP = blood pressure; DBP = diastolic blood pressure; EMG = electromyographic activity; FMS = fibromyalgia syndrome; HC = healthy control; HR = heart rate; MA = mental arithmetic phase; REL = relaxation phase phase; SBP = systolic blood pressure; SC = social conflict phase; SCL = skin conductance level.
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
KT: recruitment of the patients, organization and realization of the experimental design, statistical analyses, preparation of the manuscript. DCT: statistical analyses, preparation of the manuscript.
Acknowledgments
Acknowledgements
The author's work on psychophysiological response patterns in FMS has been supported by grants from the Deutsche Forschungsgemeinschaft to KT (Th 899-1/2 and 899-2/2), and grants from the National Institute of Arthritis and Musculoskeletal and Skin Diseases (AR44724 and AR 47298) to DCT.
Contributor Information
Kati Thieme, Email: thiemek@u.washington.edu.
Dennis C Turk, Email: turkdc@u.washington.edu.
References
- Wolfe F, Smythe HA, Yunus MB, Benett RM, Bombardier C, Goldenberg DL, Tugwell P, Campbell SM, Abeles M, Clark P, et al. The American College of Rheumatology 1990 Criteria for the classification of Fibromyalgia. Report of the Multicenter Criteria Committee. Arthritis Rheum. 1990;33:160–172. doi: 10.1002/art.1780330203. [DOI] [PubMed] [Google Scholar]
- Al-Allaf AW, Ottewell L, Pullar T. The prevalence and significance of positive antinuclear antibodies in patients with fibromyalgia syndrome: 2–4 years' follow-up. Clin Rheumatol. 2002;21:472–477. doi: 10.1007/s100670200118. [DOI] [PubMed] [Google Scholar]
- Russell AS. Effect of gamma-hydroxybutyrate on pain, fatigue, and alpha sleep anomaly in patients with fibromyalgia. J Rheumatol. 1999;26:2712. [PubMed] [Google Scholar]
- Salemi S, Rethage J, Wollina U, Michel BA, Gay RE, Gay S, Sprott H. Detection of interleukin 1beta (IL-1beta), IL-6, and tumor necrosis factor-alpha in skin of patients with fibromyalgia. J Rheumatol. 2003;30:146–150. [PubMed] [Google Scholar]
- Gur A, Karakoc M, Nas K, Remzi FH, Cevik C, Denli A, Sarac J. Cytokines and depression in cases with fibromyalgia. J Rheumatol. 2002;29:358–361. [PubMed] [Google Scholar]
- Wallace DJ, Linker-Israeli M, Hallegua D, Silverman S, Silver D, Weisman MH. Cytokines play an aetiopathogenetic role in fibromyalgia: a hypothesis and pilot study. Rheumatology (Oxford) 2001;40:743–749. doi: 10.1093/rheumatology/40.7.743. [DOI] [PubMed] [Google Scholar]
- Rossy LA, Buckelew SP, Dorr N, Hagglund KJ, Thayer JF, McIntosh MJ, Hewett JE, Johnson JC. A meta-analysis of fibromyalgia treatment interventions. Ann Behav Med. 1999;21:180–191. doi: 10.1007/BF02908299. [DOI] [PubMed] [Google Scholar]
- Wolfe F, Zhao S, Lane N. Preference for nonsteroidal antiinflammatory drugs over acetaminophen by rheumatic disease patients: a survey of 1,799 patients with osteoarthritis, rheumatoid arthritis and fibromyalgia. Arthritis Rheum. 2000;43:378–385. doi: 10.1002/1529-0131(200002)43:2<378::AID-ANR18>3.0.CO;2-2. [DOI] [PubMed] [Google Scholar]
- Turk DC, Okifuji A, Sinclair JD, Starz TW. Pain, disability, and physical functioning of patients with fibromyalgia. J Rheumatol. 1996;23:1255–1262. [PubMed] [Google Scholar]
- Crofford LJ, Young EA, Engleberg NC, Korszun A, Brucksch CB, McClure LA, Brown MB, Demitrack MA. Basal circadian and pulsatile ACTH and cortisol secretion in patients with fibromyalgia and/or chronic fatigue syndrome. Brain Behav Immun. 2004;18:314–325. doi: 10.1016/j.bbi.2003.12.011. [DOI] [PubMed] [Google Scholar]
- Qiao ZG, Vaeroy H, Morkrid L. Electrodermal and microcirculatory activity in patients with fibromyalgia during baseline, acustic stimulation and cold pressor tests. J Rheumatol. 1991;18:1383–1389. [PubMed] [Google Scholar]
- Martinez-Lavin M, Hermosillo AG, Rosas M, Soto ME. Circadian studies of autonomic nervous balance in patients with fibromyalgia: a heart rate variability analysis. Arthritis Rheum. 1998;41:1966–1971. doi: 10.1002/1529-0131(199811)41:11<1966::AID-ART11>3.0.CO;2-O. [DOI] [PubMed] [Google Scholar]
- Bou-Holaigah I, Calkins H, Flynn JA, Tunin C, Chang HC, Kan JS, Rowe PC. Provocation of hypotension and pain during upright tilt table testing in adults with fibromyalgia. Clin Exp Rheumatol. 1997;15:239–246. [PubMed] [Google Scholar]
- Elert JE, Rantapaa-Dahlqvist SB, Henriksson-Larsen K, Lorentzon R, Gerdle BU. Muscle performance, electromyography and fibre type composition in fibromyalgia and work-related myalgia. Scand J Rheumatol. 1992;21:28–34. doi: 10.3109/03009749209095059. [DOI] [PubMed] [Google Scholar]
- Svebak S, Anjia R, Karstad SI. Task-induced electromyographic activation in fibromyalgia subjects and controls. Scand J Rheumatol. 1993;22:124–130. doi: 10.3109/03009749309099256. [DOI] [PubMed] [Google Scholar]
- Elam M, Johansson G, Wallin BG. Do patients with primary fibromyalgia have an altered muscle sympathetic nerve activity? Pain. 1992;48:371–375. doi: 10.1016/0304-3959(92)90086-Q. [DOI] [PubMed] [Google Scholar]
- Vestergaard-Poulsen P, Thomsen C, Norregaard J, Bulow P, Sinkjaer T, Henriksen O. 31P NMR spectroscopy and electromyography during exercise and recovery in patients with fibromyalgia. J Rheumatol. 1995;22:1544–1551. [PubMed] [Google Scholar]
- Graven-Nielsen T, Svensson P, Arendt-Nielsen L. Effects of experimental muscle pain on muscle activity and co-ordination during static and dynamic motor function. Electroencephalogr Clin Neurophysiol. 1997;105:156–164. doi: 10.1016/S0924-980X(96)96554-6. [DOI] [PubMed] [Google Scholar]
- Sorensen J, Graven-Nielson T, Henriksson KG, Bengtsson M, Arendt-Nielson L. Hyperexcitability in fibromyalgia. J Rheumatol. 1998;25:152–155. [PubMed] [Google Scholar]
- Thieme K, Rose U, Pinkpank T, Spies C, Flor H, Turk DC. Psychophysiological Responses in Patients with Fibromyalgia Syndrome. Psychother Psychosom. [DOI] [PubMed]
- Turk DC, Flor H. Primary fibromyalgia is greater than tender points: toward a multiaxial taxonomy. J Rheumatol Suppl. 1989;19:80–86. [PubMed] [Google Scholar]
- Wenger MA, Clemens TL, Coleman DR, Cullen TD, Engel BT. Autonomic response specificity. Psychosom Med. 1961;23:185–193. doi: 10.1097/00006842-196105000-00001. [DOI] [PubMed] [Google Scholar]
- Lacey JI. Individual differences in somatic response patterns. J Comp Physiol Psychol. 1950;43:338–350. doi: 10.1037/h0057436. [DOI] [PubMed] [Google Scholar]
- Sprott H, Salemi S, Gay RE, Bradley LA, Alarcon GS, Oh SJ, Michel BA, Gay S. Increased DNA fragmentation and ultrastructural changes in fibromyalgic muscle fibres. Ann Rheum Dis. 2004;63:245–251. doi: 10.1136/ard.2002.004762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Okifuji A, Turk DC, Sinclair JD, Starz TW, Marcus DA. A standardized manual tender point survey. I. Development and determination of a threshold point for the identification of positive tender points in fibromyalgia syndrome. J Rheumatol. 1997;24:377–383. [PubMed] [Google Scholar]
- Hahlweg K. Fragebogen zur Partnerschaftsdiagnostik [Questionnaire for the assessment of spousal relationships] Göttingen: Hogrefe; 1996. [Google Scholar]
- Fridlund AJ, Cacioppo JT. Guidelines for human electromyographic research. Psychophysiology. 1986;23:567–589. doi: 10.1111/j.1469-8986.1986.tb00676.x. [DOI] [PubMed] [Google Scholar]
- Jennings JR, Berg WK, Hutcheson JS, Obrist P, Porges S, Turpin G. Committee report. Publication guidelines for heart rate studies in man. Psychophysiology. 1981;18:226–231. doi: 10.1111/j.1469-8986.1981.tb03023.x. [DOI] [PubMed] [Google Scholar]
- Boucsein W. Elektrodermale Aktivitaet [Electrodermal activity] Berlin, Heidelberg, New York: Springer; 1988. [Google Scholar]
- Fowles DC, Christie MJ, Edelberg R, Grings WW, Lykken DT, Venables PH. Committee report. Publication recommendations for electrodermal measurements. Psychophysiology. 1981;18:232–239. doi: 10.1111/j.1469-8986.1981.tb03024.x. [DOI] [PubMed] [Google Scholar]
- Everitt B. Cluster analysis is a generic term for a wide range of numerical methods for examining data. Stat Methods Med Res. 2004;13:343–345. doi: 10.1191/0962280204sm371ed. [DOI] [PubMed] [Google Scholar]
- Johannes B, Salnitski VP, Thieme K, Kirsch KA. Differences in the autonomic reactivity pattern to psychological load in patients with hypertension and rheumatic diseases. Aviakosm Ekolog Med. 2003;37:28–42. [PubMed] [Google Scholar]
- Flor H, Turk DC. Psychophysiology of chronic pain: do chronic pain patients exhibit symptom-specific psychophysiological responses? Psychol Bull. 1989;105:215–259. doi: 10.1037/0033-2909.105.2.215. [DOI] [PubMed] [Google Scholar]
- Bansevicius D, Westgaard RH, Stiles T. EMG activity and pain development in fibromyalgia patients exposed to mental stress of long duration. Scand J Rheumatol. 2001;30:92–98. doi: 10.1080/03009740151095367. [DOI] [PubMed] [Google Scholar]
- Jubrias SA, Bennett RM, Klug GA. Increased incidence of a resonance in the phosphodiester region of 31P nuclear magnetic resonance spectra in the skeletal muscle of fibromyalgia patients. Arthritis Rheum. 1994;37:801–807. doi: 10.1002/art.1780370604. [DOI] [PubMed] [Google Scholar]
- Neeck G. Neuroendocrine and hormonal perturbations and relations to the serotonergic system in fibromyalgia patients. Scand J Rheumatol Suppl. 2000;113:8–12. [PubMed] [Google Scholar]
- Sheffield-Moore M, Urban RJ. An overview of the endocrinology of skeletal muscle. Trends Endocrinol Metab. 2004;15:110–115. doi: 10.1016/j.tem.2004.02.009. [DOI] [PubMed] [Google Scholar]
- Zidar J, Backman E, Bengtsson A, Henriksson KG. Quantitative EMG and muscle tension in painful muscles in fibromyalgia. Pain. 1990;40:249–254. doi: 10.1016/0304-3959(90)91122-Y. [DOI] [PubMed] [Google Scholar]
- Flor H, Birbaumer N, Schugens MM, Lutzenberger W. Symptom-specific psychophysiological responses in chronic pain patients. Psychophysiology. 1992;29:452–460. doi: 10.1111/j.1469-8986.1992.tb01718.x. [DOI] [PubMed] [Google Scholar]
- Schommer NC, Hellhammer DH, Kirschbaum C. Dissociation between reactivity of the hypothalamus-pituitary-adrenal axis and the sympathetic-adrenal-medullary system to repeated psychosocial stress. Psychosom Med. 2003;65:450–460. doi: 10.1097/01.PSY.0000035721.12441.17. [DOI] [PubMed] [Google Scholar]
- Ayala AR, Pushkas J, Higley JD, Ronsaville D, Gold PW, Chrousos GP, Pacak K, Calis KA, Gerald M, Lindell S, et al. Behavioral, adrenal, and sympathetic responses to long-term administration of an oral corticotropin-releasing hormone receptor antagonist in a primate stress paradigm. J Clin Endocrinol Metab. 2004;89:5729–5737. doi: 10.1210/jc.2003-032170. [DOI] [PubMed] [Google Scholar]
- Andersson IJ, Barlind A, Nystrom HC, Olsson B, Skott O, Mobini R, Johansson M, Bergstrom G. Reduced sympathetic responsiveness as well as plasma and tissue noradrenaline concentration in growth hormone transgenic mice. Acta Physiol Scand. 2004;182:369–378. doi: 10.1111/j.1365-201X.2004.01368.x. [DOI] [PubMed] [Google Scholar]
- Staud R, Cannon RC, Mauderli AP, Robinson ME, Price DD, Vierck CJ., Jr Temporal summation of pain from mechanical stimulation of muscle tissue in normal controls and subjects with fibromyalgia syndrome. Pain. 2003;102:87–95. doi: 10.1016/s0304-3959(02)00344-5. [DOI] [PubMed] [Google Scholar]
- Martinez-Lavin M. Fibromyalgia as a sympathetically maintained pain syndrome. Curr Pain Headache Rep. 2004;8:385–389. doi: 10.1007/s11916-996-0012-4. [DOI] [PubMed] [Google Scholar]
- Grimm DR, Cunningham BM, Burke JR. Autonomic nervous system function among individuals with acute musculoskeletal injury. J Manipulative Physiol Ther. 2005;28:44–51. doi: 10.1016/j.jmpt.2004.12.006. [DOI] [PubMed] [Google Scholar]
- Thieme K, Gromnica-Ihle E, Flor H. Operant behavioral treatment of fibromyalgia: a controlled study. Arthritis Rheum. 2003;49:314–320. doi: 10.1002/art.11124. [DOI] [PubMed] [Google Scholar]
- Turk DC, Okifuji A, Sinclair JD, Starz TW. Differential responses by psychosocial subgroups of fibromyalgia syndrome patients to an interdisciplinary treatment. Arthritis Care Res. 1998;11:397–404. doi: 10.1002/art.1790110511. [DOI] [PubMed] [Google Scholar]


