Abstract
Objective
Very preterm birth (< 30 weeks' gestation) is a stressful event for parents, and few support interventions for these parents have been evaluated. In this study, we evaluated the effectiveness of parent-to-parent peer support for mothers of very preterm infants in a neonatal intensive care unit (NICU).
Methods
In this cohort study, 32 mothers were recruited for the intervention group from the Mount Sinai Hospital and 28 mothers were recruited for the control group from the Sunnybrook and Women's College Health Sciences Centre, both located in Toronto. The NICUs of these hospitals serve the same region and accept referrals on alternate days. Mothers in the intervention group were paired with trained mothers who had previously had a very preterm infant in the NICU and who provided principally telephone support. Participants in both groups received standard medical and social work services. Primary outcome data consisted of self-reported, standardized measures of parental stress, state anxiety and depression. Secondary measures included self-reported, standardized measures of perceived social support and trait anxiety.
Results
At 4 weeks after enrolment in the study, mothers in the intervention group reported less stress than those in the control group (mean score 1.54 v. 2.93, p < 0.001). At 16 weeks after enrolment, the intervention group reported less state anxiety (mean score 31.4 v. 38.6, p < 0.05), less depression (mean score 2.20 v. 4.88, p < 0.01) and greater perceived social support (mean score 6.49 v. 5.48, p < 0.01) than the control group. There was no difference between the groups in terms of trait anxiety. Of the 24 mothers who evaluated the program, 21 (87.5%) indicated that it was very helpful or helpful.
Interpretation
Support from individual, trained peers was found to be effective in helping mothers deal with the stress of very preterm birth.
From 1992 to 1994, 1.8% of all live births in Canada occurred at or before 33 weeks' gestation.1 Very preterm births (< 30 weeks' gestation) remain a major concern because they are associated with high mortality,2 negative biopsychosocial factors3,4,5,6,7 and poor infant outcomes, such as neurocognitive, ophthalmologic, respiratory and behavioural and emotional disorders.8,9,10,11 Thus, mothers of very preterm infants may be experiencing many challenges, and they may have medically fragile infants who are at risk of adverse developmental outcomes.
Although the focus in the neonatal intensive care unit (NICU) is on infant health, parents experience preterm birth as highly stressful.12,13,14,15,16 Interventions are being developed to help parents deal with the experience of preterm birth and improve parent–infant interaction17,18,19,20 and, ultimately, to enhance infant development.21,22,23
Two previous studies evaluated a professional-led, peer support group19 and individual peer support20 for parents while their preterm infants were in the NICU. Although both studies reported positive results, methodological weaknesses included reliance on clinical observations, lack of reporting on differences in the reliability of the raters, insufficient reporting of recruitment strategy and attrition, and uncontrolled baseline differences.
The purpose of the present study was to evaluate the effectiveness of a parent “buddy” program — a hospital-based intervention for parents of very preterm neonates — in alleviating stress, anxiety and depression and providing social support. Because of the confines of the NICU and the potential for contamination, a randomized controlled trial was not considered feasible; thus, a cohort study design was used with a control group for comparison. The Mount Sinai Hospital and the Sunnybrook and Women's College Health Sciences Centre were chosen as the study sites because they have tertiary care NICUs that service the same region of Ontario. Also, their NICUs accept referrals on alternate days, and their capacities, services and maternal and infant outcomes are similar. The intervention has been in existence consistently since 1996 at the Mount Sinai Hospital, but did not exist at the Sunnybrook and Women's College Health Sciences Centre at the time of our study. Ethics approval was obtained from research ethics boards at both hospitals.
Methods
At both sites, mothers were recruited by perinatal social workers from June 2000 to September 2001. At the Mount Sinai Hospital, potential subjects were asked if they would participate in the parent buddy program and, if so, would they participate in the study. At the Sunnybrook and Women's College Health Sciences Centre, potential subjects were asked if they would participate in a parent buddy program if the hospital had one and, if so, would they participate in the study. At both hospitals, women were eligible if they had a singleton or twin preterm birth before 30 weeks' gestation or the infant had a birth weight of less than 1500 g; the infant was less than 10 days old and did not have complications that would seriously compromise his or her chance of survival at 72 hours; and the mother was the primary caregiver, intended to keep the infant, had at least some ability to communicate in English and had no serious medical or psychiatric condition.
Mothers and infants in both groups received medical treatment and social work services as usual. Mothers in the intervention group participated in a support program; those in the control group did not receive any peer support intervention. The support program primarily consisted of educational parental support-group meetings and the parent buddy program. The parent buddy program consisted of individual parent-to-parent support, primarily telephone support given by a parent experienced with the NICU (a “buddy”) to a parent of a very preterm infant in the NICU. Buddies were parents who appeared to have adjusted to their previous experience of very preterm birth (as determined through a social work clinical assessment, which included a discussion with the buddy and an assessment to rule out signs of maladjustment [e.g., depression, anger, sadness, anxiety]) and were willing to give support. On a volunteer basis, they attended 5 hours of training to enhance their communication skills and self-awareness and to learn to recognize their boundaries of offering support.
Within a week after birth, all parents with a very preterm infant were asked if they would like to be connected with a buddy, unless there were concerns about child protection, domestic violence or psychiatric illness. Parents were matched with a buddy based on similarities in their infants' medical conditions, language and ethnic background and, if possible, geographic proximity.
The primary outcome variables were parental stress, anxiety and depression. To measure levels of stress, we used the Parental Stressor Scale: Neonatal Intensive Care Unit, which includes 4 subscales specific to the NICU: infant appearance, parental role alteration (e.g., not able to hold or feed infant), sights and sounds, and staff relations. This scale has displayed excellent internal consistency.15 Scores range from 1 (no stress) to 5 (high level of stress). Mothers were asked to complete the scale at baseline and 4 weeks after enrolment, a time when their infants would still likely be in hospital.
The State Anxiety Inventory (SAI) was used to measure state (at the moment) anxiety. This scale has demonstrated internal consistency (Cronbach's α = 0.93) and has high reliability and validity24,25 Scores range from 20 (not anxious) to 80 (extremely anxious); the norm for working female adults is 35.20 (standard deviation [SD] 10.6).24
The short form of the Beck Depression Inventory (BDI),26 adapted from the standard scale,27 was used to measure symptoms and attitudes of depression. The BDI has shown internal consistency (Cronbach's α = 0.83),28 reliability between different raters (kappa value = 0.62) and correlation with ratings by a panel of psychiatrists (kappa value = 0.77).29 Scores of 0–4 signify no depression; 5–8, mild depression; 9–15, moderate depression; and 16 or more, severe depression.
Mothers were asked to complete the SAI and BDI at baseline and at 16 weeks after enrolment, a time when they and their infants would probably have adjusted to the transition to home.
The secondary outcome variables were the level of perceived social support and proneness to anxiety in response to stressful events (trait anxiety). The Multidimensional Scale of Perceived Social Support measures perception of support rather than actual support; it has shown excellent internal consistency (Cronbach's α = 0.90 to 0.95) and validity.30 This scale ranges from 1 (very strongly disagree with statements regarding support) to 7 (very strongly agree with statements); the norm is reported as 5.58.30 This scale was used for both the intervention and control groups because it could be applied to the support that parents thought they received from their buddies as well as from friends. At baseline, this measure helped to reveal the similarity between the 2 groups in their perceptions of support, which has been described as a component of personality.31 At 16 weeks after enrolment, this measure was used to check whether mothers in the intervention group actually experienced support from their buddy.
The Trait Anxiety Inventory24,25 was used to assess the similarity between the 2 groups in terms of how prone they were to respond to stressful events with anxious reactions. To minimize subject burden, this variable was measured only at 16 weeks after enrolment. The scores can range from 20 (not prone to anxiety in response to stressful event) to 80 (extremely prone); the norm for working women is 34.79 (SD 9.22).24
In calculating the required sample size,32,33 the delta value was estimated as the change score deemed clinically significant in previous studies.34,35 Sample sizes were calculated for each of the 4 outcome measures used in this study, and the greatest value was used. To detect a clinically significant difference with 80% power, 25 subjects were required in each group.
Data collection occurred in hospital at baseline, by telephone at 4 weeks after enrolment and by mail at 16 weeks after enrolment. Baseline data were analyzed using t-tests and χ2 tests. Outcome data were analyzed on an intention-to-treat basis using analysis of covariance, with pretest scores entered as one covariate36 and one baseline difference (the number of days from birth to entry into the study) as a second covariate. The assumption of equality of variance was not met for the Parental Stress Scale, which was analyzed using the Mann–Whitney U-test.
Results
Of the 41 potential candidates who met the inclusion criteria and who were approached at the Mount Sinai Hospital, 32 (78%) participated in the study (Fig. 1). At 4 weeks after enrolment 31 mothers completed the measure of parental stress, and at 16 weeks 24 (75%) mothers completed the tests. At the Sunnybrook and Women's Health Sciences Centre, 28 mothers were enrolled in the study and completed the measure of parental stress at 4 weeks after enrolment; 25 (89%) completed all outcome measures. The difference in attrition between the 2 groups at 16 weeks after enrolment was not statistically significant. The mothers who did not complete the study (n = 11) did not differ statistically from the whole sample in terms of their demographic information, infant characteristics and outcome measures.
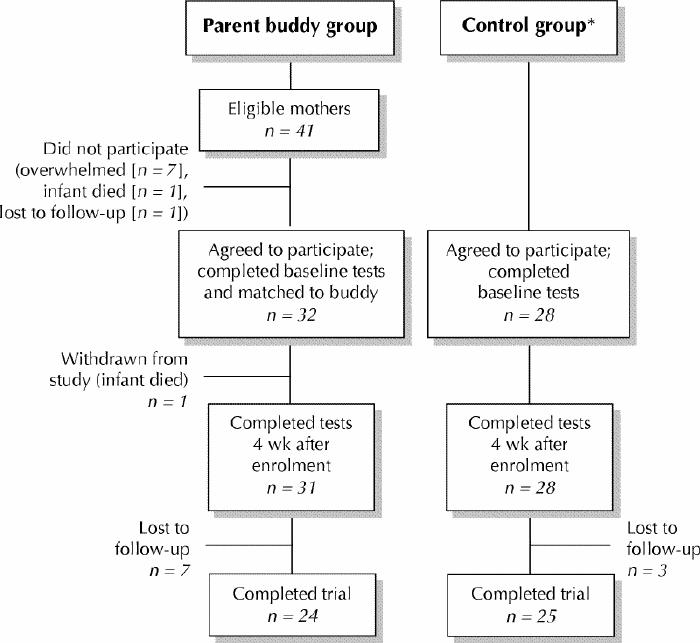
Fig. 1: Profile of study participants. *Number of eligible mothers not known.
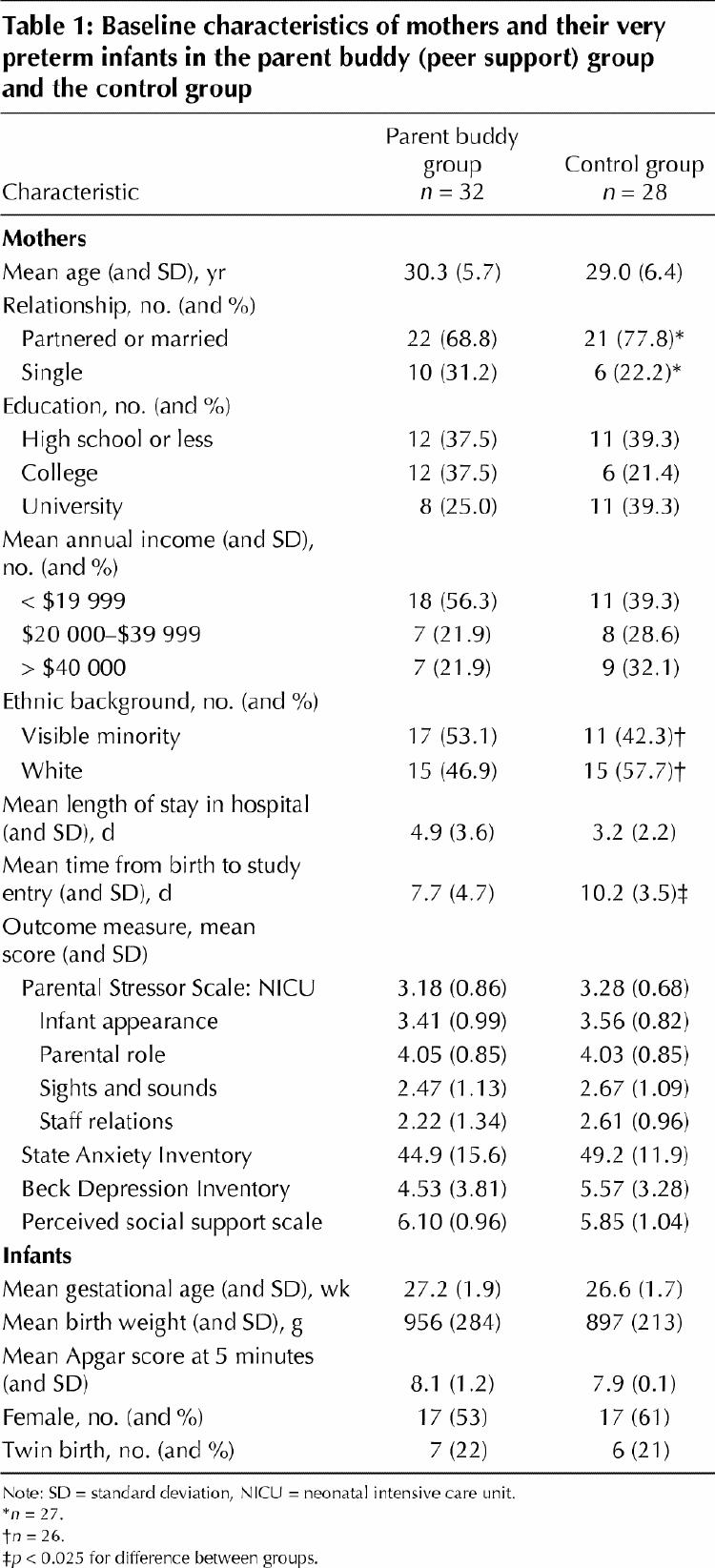
There were no statistical differences (p > 0.10) between the intervention and control groups in terms of demographic and infant characteristics or outcome measures taken at baseline (Table 1). Half of the mothers were employed in low-paying work, such as clerical jobs, factory work or hair styling; 23% did not work outside the home. These mothers represented diverse ethnic backgrounds. At baseline, the mothers reported considerable stress, some anxiety and depression, and a high level of social support. The only characteristic by which the groups differed significantly at baseline was the number of days between giving birth and entry into the study (mean 7.72 v. 10.25; t = 2.39, p = 0.025). The clinical significance of this difference is uncertain.
Table 1
There were statistically significant differences between the intervention and control groups on all primary outcome scores (Table 2). Because the Mann–Whitney U-test was used, the analysis of the stress scores did not include adjustment for covariates. However, at 4 weeks after enrolment, the mothers in the intervention group reported considerably less stress than those in the control group.
Table 2
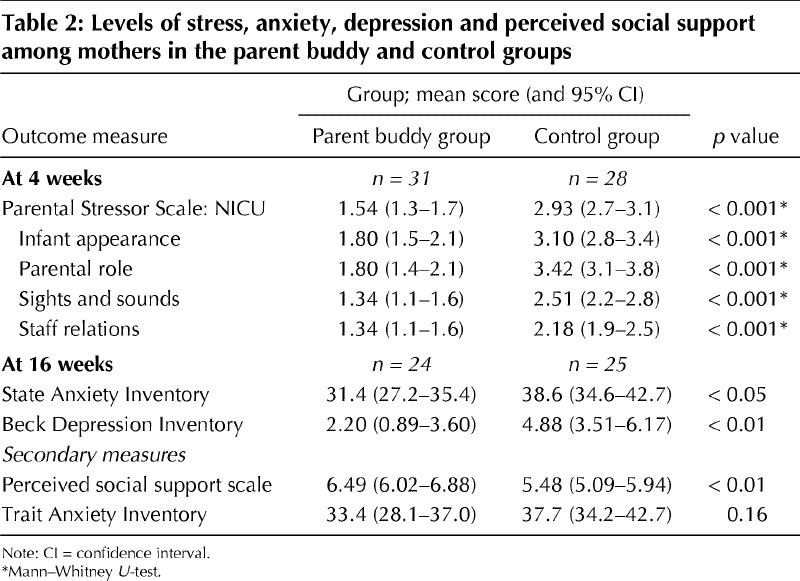
At 4 weeks after enrolment, 61% of the mothers in each group still had an infant in the NICU (19 intervention and 17 control). Mothers whose infants had been transferred to a level II nursery or community hospital were asked to rate their stress associated with this unit. No infants had been discharged from hospital to home.
At 16 weeks after enrolment, mothers in the intervention group reported less state anxiety and depression and greater perceived social support than those in the control group (Table 2). The mean SAI scores for both groups were close to the norm. The mean BDI score for the mothers in the intervention group indicated no clinical depression, whereas the mean for those in the control group indicated mild clinical depression. There was no statistical difference between the groups in terms of trait anxiety.
At 16 weeks after enrolment, there were no statistical differences between the intervention and control groups in terms of the infants' length of stay (mean 69 days, t = 0.14, p = 0.89), number of days home (mean 47 days, t = 0.51, p = 0.62) and number of medical appointments beyond their regular checkups (mean 1.5, t = 0.25, p = 0.80). These findings suggest that the health status of the infants in the 2 groups was similar and that the intervention appeared to have no effect on subsequent medical contacts.
Of the 24 mothers in the intervention group who completed an evaluation form, 21 (87.5%) indicated that their buddy was very helpful or helpful; 2 mothers indicated no difference and 1 mother disclosed that she found the buddy unhelpful. Mothers reported 9 contacts on average (range 1–50) with their buddies while their infants were in hospital, and 11 mothers indicated 3 contacts on average after their infants were discharged. The total length of all contacts ranged from 5 minutes to over 80 hours (mean 9 hours). Of the 23 mothers who indicated whether they attended group sessions, 8 (35%) did not attend any sessions, 7 (30%) attended 1–3 group sessions, 5 (22%) attended 4–6 sessions, and 3 (13%) attended 10–15 sessions. The group sizes were too small to test the effects of group participation, and thus group participation may be a confounder.
Interpretation
The mothers who participated in the parent buddy program reported less stress, state anxiety and depression than the mothers in the control group. The difference between the mean Parental Stressor Scale scores for the intervention and control groups was 1.39 at 4 weeks; the delta value used in the sample size calculation was 0.5. According to Chan and colleagues,37 in the absence of empirical research and expert panel consensus, this is the next best level of justification of clinical importance. However, the practical and clinical importance of the effects on anxiety and depression were not conclusively demonstrated in our study.
At baseline, there was no statistical difference between the intervention and control groups' reported social support scores. Their high scores suggest that both groups belonged to a social network38 that could help them during crises.39,40 At 16 weeks after enrolment, a statistically and clinically significant37 difference was evident. Previously, mothers have indicated that their interactions with their buddy helped to reduce their feelings of isolation, provided validation of their emotional experiences, provided understanding and helped to normalize the situation.41 Theoretically, this support may have provided a social reference42,43,44 in the time of crisis that permitted reappraisal, accommodation, a model or referent information for coping purposes. The therapeutic effect may be due to empathic understanding provided by the specialized peer support and at a time when mothers were experiencing considerable stress15 (i.e., while their infants were still in the NICU).
Most of the mothers relied on telephone support, which may reflect obstacles to meeting in person, such as lack of child care. It may also reflect the spontaneity that telephone contact permits. Because the health status of very preterm infants fluctuates, the timing of contact may be an important factor. Although it is suspected that parents who meet in person perceive greater benefit than those who do not, at least one previous study of peer support groups45 found no difference in outcome between support provided via the telephone and support provided in person.
Limitations of the study included reliance on a quasi-experimental design and the resulting potential threats to internal validity, namely differential maturation (e.g., differences in cognitive growth between groups); differential statistical regression; different settings (e.g., the existence of staffing shortages at one setting)36 and selection bias. Other limitations included the lack of long-term, objective measures of infant and maternal well-being and the lack of blinding of researchers.
Most of the mothers in our study considered their buddy helpful; however, the 1 mother who reported an adverse relationship suggests that more care should be taken when matching mothers to buddies and that the relationships should be monitored.
Individual peer support was found to be effective for mothers who reported a relatively low income and diverse ethnic background; however, it is not known whether these findings can be applied to other populations with different demographic characteristics. A multiple-site randomized controlled trial, a larger sample and economic evaluation are needed to establish the causal relation between intervention and outcomes and the long-term benefits of a parent buddy program for mothers of very preterm infants.
Acknowledgments
We gratefully acknowledge Dr. Arne Ohlsson, Mount Sinai Hospital, for his critical review of a draft of this manuscript; Professor Lynn McDonald, Michele Preyde's thesis supervisor, and committee members Professors Joseph Beyene, Marion Bogo and Kevin Gorey; social work and nursing staff at the Mount Sinai Hospital, particularly Diane Savage, Joanne Sulman, Heather Bartlett, Maureen McGillivray, Marianne Bracht, Annette Bot and Margareta Kata, and at the Sunnybrook and Women's College Health Sciences Centre, particularly Mary Joyall, Marisa Amorosa, Sharon Gibbons and Jennifer Stannard; and the mothers and buddies who participated in this study.
Footnotes
This article has been peer reviewed.
Contributors: Michele Preyde was the principal investigator; she designed and conducted this research as the basis of her PhD dissertation at the Faculty of Social Work, University of Toronto. She collected, analyzed and interpreted the data and wrote the manuscript. Frida Ardal developed the intervention, contributed to the conception of the design, collected data and critically revised the manuscript. Both authors gave final approval of the version to be published.
Competing interests: None declared.
Correspondence to: Michele Preyde, Department of Family Relations and Applied Nutrition, University of Guelph, Guelph ON N1G 2W1
References
- 1.Joseph KS, Kramer MS, Marcoux S, Ohlsson A, Wen SW, Allen A, et al. Determinants of preterm birth rates in Canada from 1981 through 1983 and from 1992 through 1994. N Engl J Med 1998;339:1434-9. [DOI] [PubMed]
- 2.Sankaran K, Chien LY, Walker R, Seshia M, Ohlsson A, Lee SK, and the Canadian Neonatal Network. Variations in mortality rates among Canadian neonatal intensive care units. CMAJ 2002;166(2):173-8. [PMC free article] [PubMed]
- 3.Ancel PY, Saurel-Cubizolles MJ, Di Renzo GC, Papiernik E, Breart G. Very and moderate preterm births: are the risk factors different? Br J Obstet Gynaecol 1999;106:1162-70. [DOI] [PubMed]
- 4.Kramer MS, Seguin L, Lydon J, Goulet L. Socio-economic disparities in pregnancy outcome: why do the poor fare so poorly? Paediatr Perinat Epidemiol 2000;14:194-210. [DOI] [PubMed]
- 5.Martius JA, Steck T, Oehler MK, Wulf KH. Risk factors associated with preterm (<37+0 weeks) and early preterm birth (<32+0 weeks): univariate and multivariate analysis of 106,345 singleton births from the 1994 statewide perinatal survey of Bavaria. Eur J Obstet Gynecol Reprod Biol 1998;80:183-9. [DOI] [PubMed]
- 6.Misra DP, O'Campo P, Strobino D. Testing a sociomedical model for preterm delivery. Paediatr Perinat Epidemiol 2001;15:110-22. [DOI] [PubMed]
- 7.Pritchard CW, Teo PY. Preterm birth, low birthweight and the stressfulness of the household role for pregnant women. Soc Sci Med 1994;38:89-96. [DOI] [PubMed]
- 8.McCormick MC, Workman-Daniels K, Brooks-Gunn J. The behavioral and emotional well-being of school-age children with different birth weights. Pediatrics 1996;97:18-25. [PubMed]
- 9.Peterson BS, Vohr B, Staib LH, Cannistraci CJ, Dolberg A, Schneider KC, et al. Regional brain volume abnormalities and long-term cognitive outcome in preterm infants. JAMA 2000;284:1939-47. [DOI] [PubMed]
- 10.Schothorst PF, van Engeland H. Long-term behavioral sequelae of prematurity. J Am Acad Child Adolesc Psychiatry 1996;35:175-83. [DOI] [PubMed]
- 11.Wood NS, Marlow N, Costeloe K, Gibson AT, Wilkinson AR. Neurologic and developmental disability after extremely preterm birth. N Engl J Med 2000; 343:378-84. [DOI] [PubMed]
- 12.Meyer EC, Garcia Coll CT, Seifer R, Ramos A, Kilis E, Oh W. Psychological distress in mothers of preterm infants. J Dev Behav Pediatr 1995;16:412-7. [PubMed]
- 13.Miles MS, Funk SG, Kasper MA. The neonatal intensive care unit environment: sources of stress for parents. AACN Clin Issues Crit Care Nurs 1991;2: 346-54. [DOI] [PubMed]
- 14.Young Siedeman R, Watson MA, Corff KE, Odle P, Haase J, Bowerman JL. Parent stress and coping in the NICU and PICU. J Pediatr Nurs 1997;12:169-77. [DOI] [PubMed]
- 15.Miles MS, Funk SG, Carlson J. Parental Stressor Scale: neonatal intensive care unit. Nurs Res 1993;42:148-52. [PubMed]
- 16.Shields-Poe PD, Pinelli J. Variables associated with parental stress in neonatal intensive care units. Neonatal Netw 1997;16:29-37. [PubMed]
- 17.Bracht M, Ardal F, Bot A, Cheng CM. Initiation and maintenance of a hospital-based parent group for parents of premature infants: key factors for success. Neonatal Netw 1998;17:33-7. [PubMed]
- 18.Meyer EC, Coll CT, Lester BM, Boukydis CF, McDonough SM, Oh W. Family-based intervention improves maternal psychological well-being and feeding interaction of preterm infants. Pediatrics 1994;93:241-6. [PubMed]
- 19.Minde K, Shosenberg N, Marton P, Thompson J, Ripley J, Burns S. Self-help groups in a premature nursery — a controlled evaluation. J Pediatr 1980; 96: 933-40. [DOI] [PubMed]
- 20.Roman LA, Lindsay JK, Boger RP, DeWys M, Beaumont EJ, Jones AS, et al. Parent-to-parent support initiated in the neonatal intensive care unit. Res Nurs Health 1995;18:385-94. [DOI] [PubMed]
- 21.Landry SH, Smith KE, Miller-Loncar CL, Swank PR. The relation of change in maternal interactive styles to the developing social competence of full-term and preterm children. Child Dev 1998;69:105-23. [PubMed]
- 22.Smith KE, Landry SH, Swank PR, Baldwin CD, Denson SE, Wildin S. The relation of medical risk and maternal stimulation with preterm infants' development of cognitive, language and daily living skills. J Child Psychol Psychiatry 1996;37:855-64. [DOI] [PubMed]
- 23.Wyly VM, Allen J, Wilson J. Premature infants and their families: developmental interventions. San Diego: Singular Publishing Group; 1995.
- 24.Spielberger CD, Gorsuch RL, Lushene R, Vagg PR, Jacobs GA. State-Trait Anxiety Inventory for adults. Palo Alto: Mind Garden; 1983.
- 25.Spielberger CD, Gorsuch RL, Lushene RE. Manual for the State-Trait Anxiety Inventory. Palo Alto: Consulting Psychologists Press; 1970.
- 26.Beck AT, Beck RW. Screening depressed patients in family practice: a rapid technic. Postgrad Med 1972;52:81-5. [DOI] [PubMed]
- 27.Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Arch Gen Psychiatry 1961;4:561-71. [DOI] [PubMed]
- 28.Reynolds WM, Gould JW. A psychometric investigation of the standard and short form Beck Depression Inventory. J Consult Clin Psychol 1981;49:306-7. [DOI] [PubMed]
- 29.Bumberry W, Oliver JM, McClure JN. Validation of the Beck Depression Inventory in a university population using psychiatric estimate as the criterion. J Consult Clin Psychol 1978;46:150-5.
- 30.Zimet GD, Dahlem NW, Zimet SG, Gordon KF. The Multidimensional Scale of Perceived Social Support. J Pers Assess 1988;52:30-41.
- 31.Pierce GR, Lakey B, Sarason IG, Sarason BR, Joseph HJ. Personality and social support processes: a conceptual overview. In: Pierce GR, Lakey B, Sarason IG, Sarason BR, editors. Sourcebook of social support and personality. New York: Plenum Press; 1997. p. 3-18.
- 32.Rosner B. Fundamentals of biostatistics. 4th ed. Belmont (CA): Duxbury Press; 1995.
- 33.Norman GR, Streiner DL. Biostatistics: the bare essentials. Hamilton (ON): BC Decker; 1998. p. 49-51.
- 34.Cohen J. Statistical power analysis for the behavioral sciences. Hillsdale (NJ): Lawrence Erlbaum; 1988.
- 35.Jacobson NS, Truax P. Clinical significance: a statistical approach to defining meaningful change in psychotherapy research. J Consult Clin Psychol 1991; 59:12-9. [DOI] [PubMed]
- 36.Cook TD, Campbell DT. Quasi-experimentation: design and analysis issues for field settings. Boston: Houghton Mifflin; 1979.
- 37.Chan KB, Man-Son-Hing M, Molnar FJ, Laupacis A. How well is the clinical importance of study results reported? An assessment of randomized controlled trials. CMAJ 2001;165(9):1197-202. [PMC free article] [PubMed]
- 38.Cobb S. Social support as a moderator of life stress. Psychosom Med 1976; 38: 300-14. [DOI] [PubMed]
- 39.Caplan G. The family as support system. In: Caplan G, Killilea M, Abrahams RB, editors. Support systems and mutual help: multidisciplinary explorations. New York: Grune and Stratton; 1976.
- 40.Cassel J. The contribution of the social environment to host resistance. Am J Epidemiol 1976;104:107-23. [DOI] [PubMed]
- 41.Preyde MR, Ardal A, Bracht M. Mothers' perceptions of the parent buddy program: a program for mothers of very preterm, hospitalised infants. Can Soc Work 2001;3(2):43-56.
- 42.Bem DJ. Self-perception theory. In: Berkowitz L, editor. Advances in experimental social psychology. Vol 6. New York: Academic Press; 1972. p. 2-62.
- 43.Bandura A. Social learning theory. Englewood Cliffs (NJ): Prentice-Hall; 1977.
- 44.Festinger L. A theory of social comparison process. Hum Relat 1954;7:117-40.
- 45.Brown R, Pain K, Berwald C, Hirschi P, Delehanty R, Miller H. Distance education and caregiver support groups: comparison of traditional and telephone groups. J Head Trauma Rehabil 1999;14:257-68. [DOI] [PubMed]


