A 26-year-old woman was admitted to hospital at 29 weeks' gestation because of low-back pain and the possibility of premature labour. Her antenatal course had been uncomplicated except for subcutaneous heparin abdominal injections she had received throughout her pregnancy for a known protein C deficiency.
On admission to hospital the woman received oral doses of indomethacin and 2 intramuscular injections of betamethasone in the right buttock 24 hours later to promote fetal lung maturation. Three days later she complained of fever and a tender area of erythema and swelling over her right buttock and flank. She had no abdominal pain. Her leukocyte count was elevated (13.4 х 109/L). Intravenous cefazolin therapy was started for presumed cellulitis originating at the site of her betamethasone injections.
The woman's condition improved clinically. However, after 72 hours the erythema and swelling increased, and purulent drainage was noted through several areas over her right greater trochanter. An MRI scan revealed a large (30 х 18 cm) abscess in the right gluteal area extending superiorly above the iliac crest and posteriorly to the quadratus lumborum muscles and piercing the posterolateral abdominal wall. Fig. 1 shows an MRI axial view of the fluid collection (arrow) involving the gluteal region and extending to the retroperitoneum.
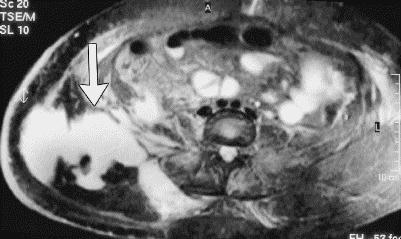
Figure 1. Photo: Images courtesy of Dr. Gordon Cuddington
Surgical treatment of the abscess was postponed because, within a few hours after the MRI, the fetal membranes ruptured and uterine contractions began. Fetal bradycardia necessitated a forceps delivery of a healthy baby.
The woman was taken to the operating room for extensive débridement of the right gluteal region (Fig. 2). Within the wound, a few plant seeds, a possible fecalith and a loose, small, white tubular structure (later confirmed histologically to be the woman's appendix) were found. These findings suggested that the abscess originated from an intraperitoneal gastrointestinal perforation, probably her appendix, which led to a retroperitoneal spread and eventual tracking through the muscle plains to her skin. The woman's wound was left open, and postoperatively a vacuum device was used to assist wound closure. She was given broad-spectrum antibiotics intravenously and made an unremarkable recovery over 3 weeks.

Figure 2. Photo: Images courtesy of Dr. Gordon Cuddington
Appendicitis is difficult to diagnose in pregnancy. The incidence of appendicitis in pregnancy (0.05%–0.07%)1 is similar to that in the general population, but pregnant patients are more likely to present with perforations (43% v. 4%–19% in the general population).2,3 Perforations in pregnancy often lead to serious complications, including intraperitoneal infections and fetal death. The risk of perforation appears to increase with gestational age,4 and perforation in the third trimester often results in the onset of preterm labour.4
Pregnancy is associated with anatomic and physiologic changes that may disguise and delay the diagnosis of acute appendicitis. These include the cephalad displacement of the appendix from the right lower quadrant by the enlarged uterus,5 the increased leukocyte count in pregnancy and the physiologic increase in maternal blood volume that diminishes the woman's ability to demonstrate tachycardia or hypotension. A review of 22 cases of pregnant patients with appendicitis4 revealed that, although such women typically have abdominal pain, the typical presentation of appendicitis (abdominal pain, nausea and vomiting, fever and an increased leukocyte count) are unreliable in the pregnant patient.
Although imperfect, history and physical examination continue to be the best way to diagnose appendicitis in pregnancy. For indeterminate cases, some authors argue that laparoscopy may be acceptable, given the risk of fetal loss (1.5% in uncomplicated appendicitis, 35% in ruptured appendicitis) with a delayed or missed diagnosis.6
Rizwan A.B. Somani Gordon Kaban Gordon Cuddington Department of Surgery Regina General Hospital Regina, Sask. Ross McArthur Department of Radiology University of Saskatchewan Saskatoon, Sask.
References
- 1.Greenfield LJ, Mulholland MW, Oldham KT, Zelenock GB, Lillemoe KD. Surgery: scientific principles and practice. 3rd ed. Philadelphia: Lippincott Williams & Wilkins; 2001. p. 2226-30.
- 2.Tamir IL. Acute appendicitis in the pregnant patient. Am J Surg 1990;160:571-6. [DOI] [PubMed]
- 3.Hale DA, Molloy M, Pearl RH, Schutt DC, Jaques DP. Appendectomy: a contemporary appraisal. Ann Surg 1997;225:252-61. [DOI] [PMC free article] [PubMed]
- 4.Tracy M, Fletcher S. Appendicitis in pregnancy. Am Surg 2000;66(6):555-9. [PubMed]
- 5.Baer JL, Reis RA, Arens RA. Appendicitis in pregnancy with changes in position and axis of normal appendix in pregnancy. JAMA 1932;98:1359.
- 6.Al-Fozan F, Tulandi T. Safety and risks of laparoscopy in pregnancy. Curr Opin Obstet Gynecol 2002;14(4):375-9. [DOI] [PubMed]


