Varicose veins are tortuous, widened veins in the subcutaneous tissues of the legs and are often easily visible. Their valves are usually incompetent so that reflux of blood occurs, and the resulting venous hypertension can cause symptoms. Varicose veins are widely seen as medically unimportant and deserving low priority for treatment. They are common, affecting nearly a third of adults in Western societies, and few people with varicose veins are ever harmed by them. However, they cause concern and distress on a large scale, most of which can be dealt with by good explanation and reassurance, or by a variety of treatments which are evolving rapidly at present. Patients can now be referred for more precise assessment and a greater range of therapeutic options than ever before.
Who gets varicose veins?
A large UK population study has shown age adjusted prevalences of 40% in men and 32% in women, although women more often present for treatment.1 The age of onset varies; some people develop varicose veins in their teens, but prevalence rises with age. Varicose veins often appear first in pregnancy, and further pregnancies can make them worse. A family history is common,1 but people should be reassured that having close relatives with severe symptoms from varicose veins or ulcers does not confer any great likelihood that they will have similar problems.
Data sources and selection criteria
This review is based on three main sources:
A personal archive of publications accumulated over 20 years of special interest, studies, and writing on varicose veins
Conversations with specialist vascular colleagues—particularly about the potential advantages and disadvantages of the newer treatments, indications for their use, and their place in the management of varicose veins
A Medline search for important recent publications.
Summary points
Most people with varicose veins are never harmed by them—good explanation and reassurance are fundamental
Ultrasound techniques (hand held Doppler and duplex) have replaced traditional tourniquet tests for assessing varicose veins before treatment
Conventional varicose vein surgery is a clinically and cost effective treatment
Laser and radiofrequency treatment simply replace one part of the traditional operation for varicose veins (“stripping”), and most varicosities still need to be treated by removal (phlebectomies) or by sclerotherapy
Traditional sclerotherapy works well for smaller veins below the knee: foam sclerotherapy can be used to treat larger and extensive varicose veins and is becoming increasingly popular
The place of newer treatments is not yet clear, and more information is needed
What problems can varicose veins cause?
Cosmetic concern
For the great majority of people varicose veins cause no symptoms and never cause harm. Dislike of their appearance is a common complaint, particularly for women. Cosmetic concern may increase the emphasis that patients place on other symptoms.
Fears about future harm
A questionnaire study found that many people are worried about the possible harm their varicose veins might cause, but these fears are usually inappropriate—particularly in relation to bleeding, ulcers, and deep vein thrombosis.2
Discomfort
Varicose veins can cause a variety of symptoms of discomfort in the legs, but it is important to try to differentiate these from the many other reasons for leg pains. The Edinburgh vein study found that the symptoms significantly associated with varicose vein were itching, heaviness, and aching, but the relation of these with varicose veins was inconsistent, particularly in men.3 Traditional pointers to symptoms being caused by varicose veins include worsening of symptoms after prolonged standing or walking and towards the end of the day, relieving symptoms by elevating the legs or wearing support hosiery, and tenderness over the veins.
Leg swelling
This is an uncommon symptom of varicose veins—other causes are much commoner. Unilateral swelling of a leg with big varicose veins is the most typical presentation.
Thrombophlebitis
Superficial thrombophlebitis (“phlebitis”) can complicate varicose veins. The risk of deep vein thrombosis is remote, but in a case series it occurred very occasionally if phlebitis extended above the knee.4 Veins may sometimes remain permanently occluded. Treatment of the varicose veins may be appropriate if phlebitis is recurrent or severe, or if the veins also cause other symptoms. Note that thrombophlebitis is not caused by infection, and treatment with antibiotics is unnecessary: drug treatment should be limited to anti-inflammatory analgesics.
Bleeding, skin changes, and ulcers
These are the complications of varicose veins that mandate consideration of treatment. They are all associated with high venous pressure in the upright position, as a result of incompetent venous valves. Bleeding is uncommon and usually occurs from a prominent vein on the leg or foot with thin, dark, unhealthy skin overlying it. “Skin changes” range from eczema, through brown discoloration, to florid lipodermatosclerosis with induration of the subcutaneous tissues (fig 1). Sometimes this can become painfully inflamed—“inflammatory liposclerosis”—which is often misdiagnosed as phlebitis or infection. If neglected, lipodermatosclerosis can lead to ulceration, which can be chronic and troublesome: treatment of ulcers will not be considered in this review.
Fig 1.
Skin changes (lipodermatosclerosis) caused by venous hypertension. Recognition of skin damage is fundamental in examination of varicose veins
What other conditions can varicose veins be confused with?
Many people have telangiectases on their legs—often called thread, spider, or broken veins. Small dark blue reticular veins are also common. All of these are of cosmetic importance only. They are not the same as varicose veins, though they often occur in association with them.
Many people with varicose veins worry about deep vein thrombosis, but the superficial veins of the legs that become varicose are separate and distinct from the deep veins where deep vein thrombosis occurs. Varicose veins pose no proved risk of deep vein thrombosis during people's normal daily lives. Varicose veins occurring as a result of a deep vein thrombosis are uncommon. However, varicose veins may coexist with deep vein incompetence, particularly in people with complications such as lipodermatosclerosis or ulcers, which makes treatment more difficult.
How should varicose veins be assessed?
Examination should be done with the patient standing in good light, when the extent and size of varicose veins and the presence of other venous blemishes (such as telangiectases) will be clear. The distribution of varicose veins may well suggest that they are related to the long or short saphenous system. Sometimes a large varix with a palpable defect in the fascia beneath provides clinical evidence of an incompetent perforating vein. The most important medical issue is the presence or absence of skin damage resulting from venous hypertension.
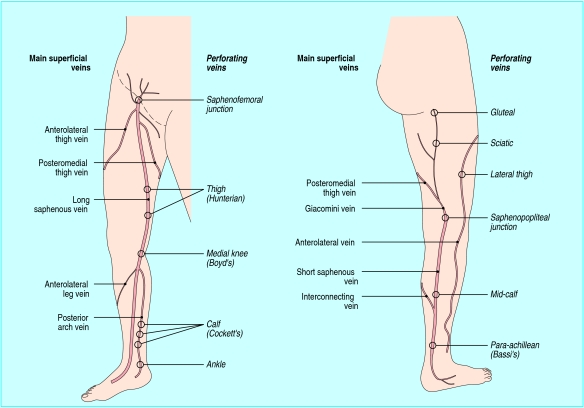
Tourniquet tests (such as the Trendelenberg test) have been abandoned by vascular specialists: they are inaccurate and have been superseded by the use of ultrasonography. Knowledge of the principle of tourniquet tests seems to persist in professional examinations as a test of the understanding of venous incompetence and the usual sites where it occurs. Incompetence at the saphenofemoral junction in the groin is by far the commonest: less common sites are the saphenopopliteal junction behind the knee, various perforating veins, and the deep veins (fig 2).
Fig 2.
Main superficial veins of the legs commonly affected by varicose veins. Incompetence at the saphenofemoral junction in the groin is the commonest cause of reflux from the deep to superficial systems, but there are many other potential sites. Incompetence of calf perforators is not (as was once believed) a common and important problem, and when present it is often corrected by long saphenous vein surgery. (The long and short saphenous veins are also called the great and small saphenous veins5)
Sites of venous incompetence are best diagnosed by duplex ultrasound scanning,6 which is being done increasingly during initial specialist assessment.7 Duplex scanning shows both venous anatomy and blood flow and is essential for assessing more complex cases (fig 3). Use of a hand held Doppler machine provides a quick screening test for selecting those who need duplex scanning.8 The main indications for a duplex scan are
Fig 3.
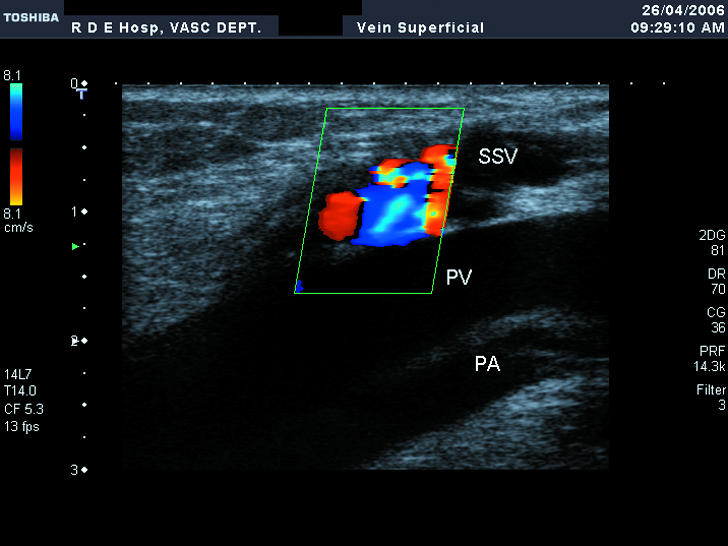
Duplex ultrasound scan of varicose veins showing the short saphenous vein (SSV) joining the popliteal vein (PV) with the popliteal artery (PA) adjacent. The patient is standing, and the calf has just been squeezed and released: the colour indicates reflux down the short saphenous vein as a result of an incompetent valve at the saphenopopliteal junction
Reflux in the popliteal fossa
Recurrent varicose veins
Complex or unusual varicose veins
History of deep vein thrombosis.
The accuracy of all Doppler tests is operator dependant, and venous Doppler examination is not a skill most doctors should expect to practise (unlike hand held Doppler assessment of arterial pressures for limb ischaemia).
What should people with varicose veins be told?
Good explanation is fundamental. Most patients need reassurance that their varicose veins are unlikely ever to cause them harm and that treatment is not essential. For those who need or want treatment, a variety of options is now available. In discussing these, it is important to specify the potential complications, especially for patients who want treatment for cosmetic reasons or minor symptoms. Medicolegal action against specialists for varicose vein treatments is relatively common.9 Patients should be told that varicose veins may recur—but this is less common after carefully planned treatment.
Patients for whom discomfort is the main problem should be advised that wearing support hosiery can provide good relief.10 Elevation of the legs may relieve symptoms. Advice about regular exercise sounds sensible but is not supported by any evidence. For people who are obese, weight loss may reduce symptoms and would make any intervention easier and safer (but losing a lot of weight may make varicose veins more visible).
Referral guidance for varicose veins from the National Institute for Health and Clinical Excellence (NICE)11
Emergency—Bleeding from a varicosity that has eroded the skin
Urgent—Varicosity that has bled and is at risk of bleeding again
Soon—Ulcer that is progressive or painful despite treatment
Routine—
Active or healed ulcer or progressive skin changes that may benefit from surgery
Recurrent superficial thrombophlebitis
Troublesome symptoms attributable to varicose veins, or patient and doctor feel that the extent, site, and size of varicosities are having a severe impact on quality of life
Referral for specialist advice
Guidelines from the National Institute for Health and Clinical Excellence (NICE) provide a good summary of the usual indications for referral, including the degrees of urgency for those with complications such as bleeding (see box).11
Operations for varicose veins
For patients with symptomatic veins and substantial venous incompetence, surgery has been the optimal treatment for many years. Inadequate assessment and operations done to mediocre standards gave varicose vein surgery a suspect reputation, but in recent years thorough treatment by interested specialists has become more widespread. Evidence from a recent UK based randomised controlled trial has shown that varicose vein surgery is both clinically and cost effective (within the normal parameters of the National Health Service).12,13 Nevertheless, varicose veins may gradually recur by a process of neovascularisation (regrowth and enlargement of veins) even after thorough surgery, or they may develop elsewhere in the legs.14
Conventional surgery
This usually means saphenofemoral ligation (not just a “high tie” but ligation of the long saphenous vein flush with the femoral vein) with stripping of the long saphenous vein and phlebectomies (stripping is supported by evidence from randomised controlled trials).14 Precise technique varies, mostly with the aim of reducing postoperative bruising. Patients with obese legs or big varicose veins may have considerable post-operative bruising, but many patients have little discomfort and recover quickly, requiring no further intervention and being completely rid of all their varicose veins.
Radiofrequency and laser ablation
These are alternatives to stripping of the long saphenous vein. If done without any other kind of treatment they may cause some varicose veins to disappear, but usually varicose veins need to be dealt with by phlebectomies or sclerotherapy. Radiofrequency and laser ablation each involve passing a probe up the long saphenous vein from knee level to the groin under ultrasound guidance and then ablating the vein in sections. This avoids a groin incision and may lead to less bruising and quicker recovery. These benefits have been documented in small randomised studies for radiofrequency ablation15,16 and by large case series for both methods,17-20 but the scale of the advantages remains uncertain. Some surgeons use these techniques under local anaesthetic infiltration rather than general anaesthesia.
Research
Most major studies of varicose veins are concerned with treatments for venous ulcers
Randomised studies on the clinical and cost effectiveness of foam sclerotherapy, and of radiofrequency and laser ablation compared with conventional surgery, are needed to establish the proper place of these treatments in the management of varicose veins
Data on long term outcomes (at least five years and preferably 10 years after treatment) are important because varicose veins may return gradually in the years after treatment
Information about large numbers of patients having foam sclerotherapy would be useful, with comprehensive data on adverse events to address concerns about the possible risk of stroke
The precise place of laser and radiofrequency ablation remains uncertain. They require dedicated equipment and use of intraoperative duplex ultrasonography, and they take longer to do than conventional surgery in experienced hands. The amount of benefit for patients is variable: obvious varicose veins still need to be treated, and phlebectomies of large veins are often the main cause of bruising and discomfort after the operation—not the groin incision. Varying longer term results (two to three years) have been reported, but in general outcomes seem similar to those of surgery.15 It has been suggested that endovenous ablation techniques may lead to less neovascularisation in the groin than surgical dissection, so reducing this cause of recurrence of varicose veins.
Sclerotherapy
Conventional sclerotherapy
This involves injection of a sclerosant—commonly sodium tetradecyl (STD) or polidocanol—into varicosities, followed by a period of compression bandaging and/or compression hosiery. There is little good evidence on how long compression needs to be worn and advice varies from a few days to three or four weeks. The main risk of sclerotherapy is injection outside the vein, which can result in local tissue necrosis and scarring.
Further reading
Medline Plus. Varicose veins. www.nlm.nih.gov/medlineplus/varicoseveins.html
Clinical Evidence. Varicose veins. www.clinicalevidence.com/ceweb/conditions/cvd/0212/0212.jsp
Michaels JA, Campbell WB, Brazier JE, MacIntyre JB, Palfreyman SJ, Ratcliffe J, et al. Randomized clinical trial, observational study and assessment of cost-effectiveness of the treatment of varicose veins (REACTIV trial). Health Technol Assess 2006;10(13). (www.hta.ac.uk/fullmono/mon1013.pdf)—This Health Technology Assessment monograph includes reviews of the epidemiology, assessment, and treatment of varicose veins, as well as a study on clinical and cost effectiveness of surgery and sclerotherapy
Information resources for patients
There are a lot of websites set up by clinicians and clinics treating varicose veins, which provide variable information. Some are objective and informative but many are quite brief and others are biased towards the particular treatments they are offering. Most give a reasonable basic description of varicose veins and the problems they can cause.
-
For greater detail, with supporting evidence, the following may be helpful:
The Medline Plus and Clinical Evidence web pages cited above
Best Treatments. Varicose veins. www.besttreatments.co.uk/btuk/conditions/15366.html
MayoClinic.com. Varicose veins overview. www.mayoclinic.com/health/varicose-veins/DS00256
Campbell B. Understanding varicose veins. Poole: Family Doctor Publications, 2006
Tips for GPs
People with varicose veins often present because of fears about possible future harm: these fears are usually inappropriate and can be allayed by explanation and reassurance
Many patients with varicose veins have leg symptoms for other reasons: a few questions will often identify a different problem
The most important medical reason to refer is recognition of complications such as bleeding or skin damage due to venous hypertension
Referral for symptoms of discomfort or for cosmetic reasons is often influenced by local guidelines, but clear criteria are elusive and decisions can be difficult
There is no need to assess the precise sites of venous incompetence: clinical tests are inaccurate, and Doppler ultrasound assessment can be done after referral. Simple observation of the size and distribution of the varicose veins and recognising skin damage from venous hypertension are the important issues
Superficial thrombophlebitis is not an infective condition and does not require antibiotic treatment. A hard, red, tender area just above the ankle is often inflammatory liposclerosis and not thrombophlebitis
Conventional sclerotherapy is a clinically and cost effective treatment for smaller varicose veins, particularly those that are not subject to upstream incompetence and those below the knee.12,13 However, its results are not long lasting in the presence of saphenofemoral reflux (the most usual situation for varicose veins with troublesome symptoms): a randomised controlled trial found that most varicose veins recur within five years.21 Sclerotherapy became popular in the 1970s, but its use then declined because so many varicose veins recurred.
Foam sclerotherapy
This involves mixing sclerosant with a small quantity of air (or other gas) to produce a foam that spreads rapidly and widely through the veins, pushing the blood aside and causing the veins to go into spasm. This is believed to increase the effectiveness of sclerosant in obliterating long segments of superficial veins. Duplex ultrasonography is used to guide placement of the injecting cannula in the chosen vein and to monitor spread of sclerosant through the veins (fig 4). The treated leg is bandaged, and compression hosiery is advised for up to a month after treatment. After treatment, larger varicose veins are commonly hard and prominent for many weeks before they gradually shrivel. Further sessions of foam treatment may be required for extensive or bilateral varicose veins.
Fig 4.
Foam sclerotherapy: the short saphenous vein is being cannulated under duplex ultrasound guidance before injection of foam
A recent randomised controlled trial found that foam treatment (combined with saphenofemoral ligation) had short term advantages compared with conventional surgery.22 Evidence for the longer term effectiveness of foam sclerotherapy is mostly from large case series, which show obliteration of varicose veins for up to three years.23
There has been concern about the possibility of foam entering the deep veins and causing venous thromboembolism, but this seems rare. Visual disturbances have been reported, particularly in individuals prone to migraine, and these may be due to vasospasm. Of greater concern is the possibility of foam passing through a patent foramen ovale (present in many people) to enter small arteries in the eye or brain. A recent report of a stroke attributed to foam treatment, albeit after injection of an unusually large volume of foam, must sound a note of caution.24 Nevertheless, the popularity of foam sclerotherapy continues to increase among both patients and specialists, and it looks set to become an important treatment for varicose veins.
Which treatment should patients choose for their varicose veins?
It is not yet clear just how the various treatments will fit into the management of varicose veins. It may well be that some are more suitable for certain kinds of patients (for example, those with large varicosities or obese legs), and patients may have personal preferences. It is unlikely that most specialists will offer all the possible treatment modalities, but they ought to be able to give good advice about treatment choices and to provide a range of options. The table shows some of the considerations that may guide the choice of treatment.
Table 1.
Features of the various treatments now available for varicose veins*
| Conventional surgery | Radiofrequency and laser ablation | Foam sclerotherapy | |
|---|---|---|---|
| Anaesthesia required |
General |
General or extensive infiltration of local |
Local or none |
| Postoperative pain and discomfort |
Variable—many patients have minimal discomfort, but others are very bruised |
Avoids a groin incision and causes less thigh bruising in many patients |
No incisions or bruising, but veins may be lumpy and tender for weeks |
| Need for compression (bandaging or stocking) |
Usually advised for up to 10 days but not essential |
Usually advised for several days (like surgery), sometimes longer |
Usually advised for about two weeks, but up to four weeks |
| Can both legs be treated at a single procedure? |
Yes |
Yes under general anaesthesia |
No, usually not |
| Further procedures required for clearance of varicose veins? |
No |
Frequently, unless done under general anaesthesia with conventional phlebectomies (or sclerotherapy) |
Yes, frequently |
| Long term freedom from varicose veins | A few varicose veins reappear in many patients: about a third have troublesomerecurrence at 10 years25 | Similar to surgery up to three years. Longer term results not known | Probably similar to surgery up to three years, but may need further treatments. Longer term results not known |
Many variations exist: for example, radiofrequency or laser treatment may be done alone or in combination with phlebectomies or sclerotherapy (conventional or foam) in a single procedure or in separate procedures. What is possible in a single session depends on the type of anaesthesia used (general, regional, or local): although varicose vein surgery is usually done under general anaesthesia, spinal or extensive local infiltration can be used.
Uncertainties and the need for further research
The most important studies required are randomised comparisons of the different treatments with good long term follow up—in particular, comparison of foam sclerotherapy with conventional surgery. It will be several years before long term (≥ 10 years) data are known for the newer treatments. Studies need to include economic modelling which will help to guide the way services are delivered: for example, are repeated outpatient treatments with foam sclerotherapy more cost effective than a single operation under general anaesthesia for bilateral varicose veins? Meanwhile, specialists will need to advise patients as objectively as they are able about choices of treatment and to audit their own results as thoroughly as they can.
I thank Georgios Lyratzopoulos, consultant in public health medicine, David Kernick, general practitioner, and Andrew Cowan, consultant vascular surgeon, for their critical and helpful advice during the preparation of this review. I also thank the Medical Photography Department of the Royal Devon and Exeter Hospital and the Clinical Measurements Department for preparing the figures.
Funding. None
Competing interests. None declared.
References
- 1.Lee AJ, Evans CJ, Allan PL, Ruckley CV, Fowkes GFR. Lifestyle factors and the risk of varicose veins. J Clin Epidemiol 2003;56: 171-9. [DOI] [PubMed] [Google Scholar]
- 2.Campbell WB, Decaluwe H, MacIntyre J, Thompson JF, Cowan AR. Most patents with varicose veins have fears or concerns about the future, in addition to their presenting symptoms. Eur J Vasc Endovasc Surg 2006;31: 332-4. [DOI] [PubMed] [Google Scholar]
- 3.Bradbury A, Evans C, Allan P, Lee A, Ruckley CV, Fowkes FG. What are the symptoms of varicose veins? Edinburgh vein study cross sectional population survey. BMJ 1999;318: 353-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chengelis DL, Bendick PJ, Glover JL, Brown OW, Ranval TJ. Progression of superficial venous thrombosis to deep vein thrombosis. J Vasc Surg 1996;24: 745-9. [DOI] [PubMed] [Google Scholar]
- 5.Caggiati A, Bergan JJ, Gloviczki P, Jantet G, Wendell-Smith CP, Parssch H. Nomenclature of the veins of the lower limbs: an international interdisciplinary consensus statement. J Vasc Surg 2002;36: 416-22. [DOI] [PubMed] [Google Scholar]
- 6.Darke SG, Vetrivel S, Foy DMA, Smith S, Baker S. A comparison of duplex scanning and continuous wave Doppler in the assessment of primary and uncomplicated varicose veins. Eur J Vasc Endovasc Surg 1997;14: 457-61. [DOI] [PubMed] [Google Scholar]
- 7.Mercer KG, Scott DJA, Berridge DC. Preoperative duplex imaging is required before all operations on primary varicose veins. Br J Surg 1998;85: 1495-7. [DOI] [PubMed] [Google Scholar]
- 8.Campbell WB, Niblett PG, Peters AS, MacIntyre JB, Sherriff S, Palfreyman S, et al. The clinical effectiveness of hand held Doppler examination for diagnosis of reflux in patients with varicose veins. Eur J Vasc Endovasc Surg 2005;30: 664-9. [DOI] [PubMed] [Google Scholar]
- 9.Goodwin H. Litigation and surgical practice in the UK. Br J Surg 2000;87: 977-9. [DOI] [PubMed] [Google Scholar]
- 10.Chant ADB, Magnussen P, Kershaw C. Support hose and varicose veins. BMJ 1985;290: 204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.National Institute for Clinical Excellence. Referral advice for varicose veins. London: NICE, 2001.
- 12.Michaels JA, Brazier JE, Campbell WB, MacIntyre JB, Palfreyman SJ, Ratcliffe J. Randomised controlled trial comparing surgery with conservative treatment for uncomplicated varicose veins. Br J Surg 2006;93: 175-81. [DOI] [PubMed] [Google Scholar]
- 13.Ratcliffe J, Brazier JE, Campbell WB, Palfreyman S, MacIntyre JB, Michaels JA. Cost effectiveness analysis of surgery versus conservative treatment for uncomplicated varicose veins in a randomised controlled trial. Br J Surg 2006;93: 182-6. [DOI] [PubMed] [Google Scholar]
- 14.Dwerryhouse S, Davies B, Harradine K, Earnshaw JJ. Stripping the long saphenous vein reduces the rate of reoperation for recurrent varicose veins: five year results of a randomized trial. J Vasc Surg 1999;29: 589-92. [DOI] [PubMed] [Google Scholar]
- 15.Lurie F, Creton D, Eklof B, Kabnick LS, Kistner RL, Pichot O, et al. Prospective randomized study of endovenous radiofrequency ablation (Closure procedure) versus ligation and vein stripping (EVOLVeS): two-year follow-up. Eur J Vasc Endovasc Surg 2005;29: 67-73. [DOI] [PubMed] [Google Scholar]
- 16.Rautio T, Ohinmaa A, Perala J, Ohtonen P, Heikkinen T, Wiik H, et al. Endovenous obliteration versus conventional stripping operation in the treatment of primary varicose veins: a randomised controlled trial with comparison of the costs. J Vasc Surg 2002;53: 958-65. [DOI] [PubMed] [Google Scholar]
- 17.Merchant RF, DePalma RG, Kabnick LS. Endovascular obliteration of saphenous reflux: a multicenter study. J Vasc Surg 2002;35: 1190-6. [DOI] [PubMed] [Google Scholar]
- 18.Nicolini PH and the Closure Group. Treatment of primary varicose veins by endovenous obliteration with the VNUS closure system: results of a multicentre study. Eur J Vasc Endovasc Surg 2005;29: 433-9. [DOI] [PubMed] [Google Scholar]
- 19.Min RJ, Khilnani N, Zimmet SE. Endovenous laser treatment of saphenous vein reflux: long term results. J Vasc Interv Radiol 2003;14: 991-6. [DOI] [PubMed] [Google Scholar]
- 20.Mundy L, Merlin TL, Fitridge RA, Hillier JE. Systematic review of endovenous laser treatment for varicose veins. Br J Surg 2005;92: 1189-94. [DOI] [PubMed] [Google Scholar]
- 21.Hobbs JT. Surgery and sclerotherapy in the treatment of varicose veins. Arch Surg 1974;109: 793-6. [DOI] [PubMed] [Google Scholar]
- 22.Bountouroglou DG, Azzam M, Kakkos SK, Pathmaraj M, Young P, Geroulakos G. Ultrasound-guided foam sclerotherapy combined with sapheno-femoral ligation compared to surgical treatment of varicose veins: early results of a randomised controlled clinical trial. Eur J Vasc Endovasc Surg 2006;31: 93-100. [DOI] [PubMed] [Google Scholar]
- 23.Cabrera J, Cabrera J Jr, Garcia-Olmedo MA. Treatment of varicose long saphenous veins with sclerosant in microfoam form: long-term outcomes. Phlebology 2000;15: 19-23. [Google Scholar]
- 24.Forlee MV, Grouden M, Moore DJ, Shanik G. Stroke after varicose vein foam injection sclerotherapy. J Vasc Surg 2006;43: 162-4. [DOI] [PubMed] [Google Scholar]
- 25.Campbell WB, Kumar AV, Collin TW, Allington KL, Michaels JA. The outcome of varicose vein surgery at 10 years: clinical findings, symptoms and patient satisfaction. Ann R Coll Surg Engl 2003;85: 52-7. [DOI] [PMC free article] [PubMed] [Google Scholar]