Abstract
From January 1991 through December 2001, 600 patients underwent closure of a peri-membranous ventricular septal defect through a right atrial approach at our institution. In 122 of these patients, the operation included temporary detachment of a tricuspid valve septal leaflet from the annulus to allow complete visualization of a perimembranous ventricular septal defect. The mean age of the patients at surgery was 4.6 years in those who underwent leaflet detachment and 4.7 years in the 478 patients who did not (P > 0.05). Preoperatively, all patients were in sinus rhythm. Echocardiography showed trivial tricuspid regurgitation in 21 of the patients undergoing detachment and in 39 of the non-detachment patients. There was no difference in bypass time or aortic cross-clamp time between the 2 groups.
Postoperatively, 3 patients in the non-detachment group had heart block; all other patients were in sinus rhythm. Echocardiograms on the 7th postoperative day showed small residual ventricular septal defects in none of the patients who underwent valve detachment and in 10 of the non-detachment patients; mild tricuspid regurgitation was present in 12 non-detachment patients only; and trivial tricuspid regurgitation was present in 19 patients who underwent valve detachment and in 29 who did not. There was no hospital death in either group. Long-term follow-up showed no progression of tricuspid regurgitation or tricuspid stenosis. All patients remained in sinus rhythm. This study suggests that tricuspid valve detachment is a safe, effective technique that improves exposure for ventricular septal defect repair and does not adversely affect valve competence. (Tex Heart Inst J 2003;30:38–41)
Key words: Cardiac surgical procedures/methods; heart septal defects, ventricular; surgery; suture techniques; tricuspid valve/surgery; tricuspid valve insufficiency/physiology
In nearly all cases, accurate repair of a perimembranous ventricular septal defect (VSD) can be achieved through a right atrial approach, across the tricuspid valve. This approach has been used almost exclusively in our hospital since 1991 for 2 reasons: the incidence of right bundle branch block is lower than that seen with the transventricular approach, and a right ventricular scar is avoided with this technique. However, in some patients, the VSD is hidden under the septal leaflet of the tricuspid valve, making visualization of the defect and placement of sutures difficult or even impossible. Temporary detachment of the septal leaflet of the tricuspid valve from the annulus (TVD) is the best method to improve exposure of the VSD and to facilitate the placement of sutures. Nevertheless, there has been concern about the safety of this technique, and few long-term results are available. 1–7 Herein, we report our experience in closing perimembranous VSDs with and without the use of TVD.
Patients and Methods
We prospectively studied all cases of isolated VSD at our hospital from 1 January 1991 through 1 December 2001. Six hundred patients with perimembranous VSD who required transatrial closure of a VSD were identified as eligible for inclusion in the study. We used TVD only when one of the following criteria was met (Fig. 1): 1) the valve was attached to almost the entire rim of the VSD in such a way that it formed an aneurysm, which obscured not just the posteroinferior margin but the whole VSD margin; or 2) abnormal chordal attachments to the septum caused the superior and posteroinferior margin to be hidden beneath the septal leaflet of the tricuspid valve. Patients with other types of VSDs that required repair via the pulmonary artery or by right ventriculotomy were excluded.
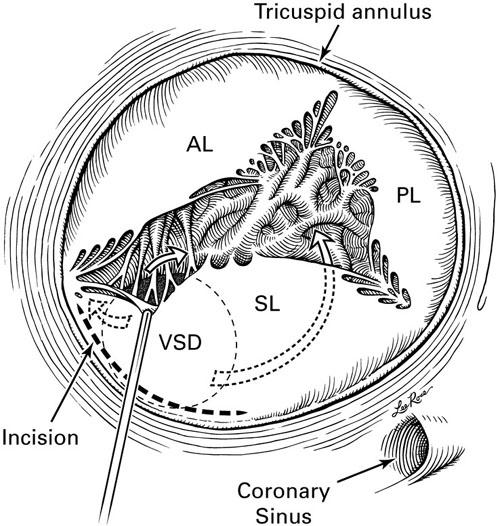
Fig. 1 The 2 criteria for temporary detachment of the septal leaflet of the tricuspid valve from the annulus are combined in this figure. Abnormal chordal attachments to the septum impair visibility of the superior and posteroinferior margins of the ventricular septal defect (VSD); and the valve is attached to the rim of the VSD, forming an aneurysm and impairing visibility of nearly the entire VSD margin. The 3 arrows indicate a left-to-right ventricular shunt through multiple openings at the mouth of the aneurysm (beneath the septal leaflet). (Illustration by Lee Rose)
AL = anterior leaflet; PL = posterior leaflet; SL = septal leaflet
Surgical Technique
Aortic and bicaval cardiopulmonary bypass were established with crystalloid cryocardioplegic solution. An oblique right atrial incision was made parallel to the atrioventricular groove. A left atrial vent was inserted through the interatrial septum. The VSD was examined by retracting the septal leaflet toward the right atrium (Fig. 1). When tricuspid valve detachment was deemed necessary to improve the visibility of the VSD, a circumferential incision was made in the septal leaflet at a distance of 1 mm from the annulus (Figs. 1 and 2), with the potential for extension of the incision onto the anterior leaflet for better exposure of the superior margin of the defect. The VSD was patched with use of a continuous suture that was started at the mid-point of the anterior margin. When the suture lines approached the 2 ends of the tricuspid valve detachment incision, they were continued onto the valve annulus and were used to sandwich the patch between the annulus and the leaflet (Fig. 3).
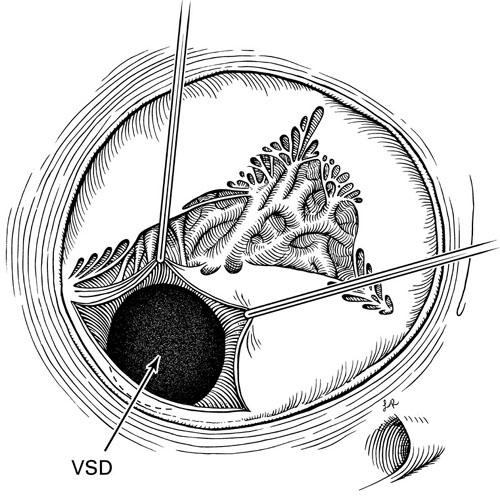
Fig. 2 The septal leaflet of the tricuspid valve has been partially detached from the annulus by an incision made at a distance of 1 to 2 mm from the annulus. Visibility of the ventricular septal defect is greatly improved. (Illustration by Lee Rose)
VSD = ventricular septal defect
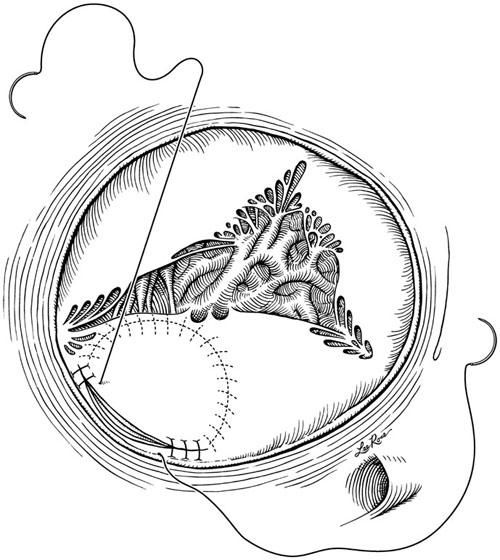
Fig. 3 The patch closure of the ventricular septal defect has been made through the leaflet incision with use of a continuous suture. When the suture lines approach the 2 ends of the valve incision, the patch is sandwiched between the annulus and the leaflet. (Illustration by Lee Rose)
Follow-Up. Electrocardiography and echocardiography were performed routinely on the 7th postoperative day, and annually thereafter at the outpatient department of our hospital.
Results
Temporary TVD was used in 122 of the 600 patients (20.3%). The VSD was closed with a patch in all TVD patients. The mean age at operation was 4.6 ± 1.5 (SD) years in the TVD group and 4.7 ± 1.6 years in the non-TVD group (P > 0.05). The mean pulmonary pressure was 40 ± 6 mmHg in the TVD group and 39 ± 5 mmHg in the non-TVD group (P > 0.05). The preoperative electrocardiograms indicated sinus rhythm in all patients. Preoperative echocardiography showed trivial tricuspid regurgitation (TR) in 39 patients in the non-TVD group and in 21 patients in the TVD group. No additional procedure was performed in any patient. There was no significant difference in bypass time or aortic cross-clamp time between the 2 groups (P > 0.05). Postoperatively, all patients in the TVD group were in sinus rhythm; 3 in the non-TVD group had heart block. Echocardiography performed on the 7th postoperative day showed small residual VSDs in none of the TVD patients and in 10 non-TVD patients; mild TR in 12 non-TVD patients only; and trivial TR in 19 TVD patients and in 29 non-TVD patients. There was no hospital death in either group. The median duration of postoperative hospitalization was 8 ± 2 days and was not significantly different between the 2 groups of patients (P > 0.05).
Follow-Up. The mean follow-up time was 62.5 months. Two patients in the non-TVD group required late reoperation for residual VSD: one had infective endocarditis, and the other had increasing pulmonary artery pressure. Spontaneous closure of the small residual VSD occurred in 5 patients in the non-TVD group. There was no progression of severity of TR in any patient on follow-up, as determined by comparison of the follow-up echocardiograms with the findings from the 7th postoperative day, and there was no tricuspid stenosis. All patients remained in sinus rhythm.
Discussion
Of all the operations performed for the correction of congenital heart defects, surgical repair of VSDs is the most common. Surgical techniques for the repair of VSDs have now been standardized. Several different approaches are used for the repair, via the right atrium, the pulmonary artery, the aorta, and the ventricle. The approach is chosen according to the exact location of the VSD. The most frequently used route is through the right atrium. Successful transatrial repair of a VSD requires adequate exposure of the margins of the defect in order to avoid residual shunt, injury of conduction tissue, and distortion of the septal leaflet of the tricuspid valve. In most cases, the right atrial route is adequate to achieve these goals. However, in some patients, exposure of the VSD is very difficult and requires temporary detachment of the septal leaflet of the tricuspid valve at its base. In our patients, about 20% of the VSDs required TVD as part of the repair; this requirement is similar to the percentages reported by others. 3,7
We shared the concerns of other surgeons—that TVD entailed the risk of postoperative tricuspid regurgitation. Therefore, we used TVD only when a valve was attached to the rim of the VSD and formed an aneurysm that obscured the whole VSD margin; or when abnormal chordal attachments to the septum caused the superior and posteroinferior margin to be hidden beneath the septal leaflet of the tricuspid valve. The technique that we used in this study is similar to that described by Gaynor and colleagues. 7 Circumferential detachment of the septal leaflet of the tricuspid valve can be used in any situation in which exposure of the VSD is extremely difficult. This technique is not so challenging as is tricuspid valve chordal detachment. 6 We used continuous suture with 4-0 Prolene, beginning at the mid-point of the anterior margin of the VSD. When the sutures reached the circumferential incision of septal leaflet, they were continued onto the tricuspid annulus and were used to sandwich the patch between the annulus and the leaflet. The enhanced visibility of the defect and the use of continuous suture generally limited the aortic cross-clamping time to about 20 to 25 minutes.
In our patients, the short- and long-term outcomes after transatrial closure of the VSD were excellent. The use of TVD reduced the incidence both of residual shunt and of surgically induced heart block, because TVD improved the visibility of the VSD margin, enabling more accurate suture placement. Early postoperative echocardiography revealed that TVD did not result in tricuspid regurgitation. This finding suggests that TVD exerts less distortion of the tricuspid valve apparatus than does chordal detachment. Moreover, long-term echocardiographic follow-up showed no progression in the severity of TR.
Tatebe and associates 4 recommended that repair of the incised septal leaflet not be performed with the use of running sutures alone. However, in the current study, we used only continuous suture, and no late TR or tricuspid stenosis was found on the echocardiograms. These results suggest that the use of continuous suture is appropriate for this procedure.
We conclude that tricuspid valve detachment is a safe, effective technique that improves exposure for ventricular septal defect repair and does not adversely affect valve competence.
Footnotes
Address for reprints: Jinping Zhao, MD, Department of Cardiothoracic Surgery, Tongji Hospital, 430030 Wuhan, P.R.C.
E-mail: zhao_jinping@hotmail.com
References
- 1.Frenckner BP, Olin CL, Bomfim V, Bjarke B, Wallgren CG, Bjork VO. Detachment of the septal tricuspid leaflet during transatrial closure of isolated ventricular septal defect. J Thorac Cardiovasc Surg 1981;82:773–8. [PubMed]
- 2.Pridjian AK, Pearce FB, Culpepper WS, Williams LC, Van Meter CH, Ochsner JL. Atrioventricular valve competence after takedown to improve exposure during ventricular septal defect repair. J Thorac Cardiovasc Surg 1993;106:1122–5. [PubMed]
- 3.Bol-Raap G, Bogers AJ, Boersma H, De Jong PL, Hess J, Bos E. Temporary tricuspid valve detachment in closure of congenital ventricular septal defect. Eur J Cardiothorac Surg 1994;8:145–8. [DOI] [PubMed]
- 4.Tatebe S, Miyamura H, Watanabe H, Sugawara M, Eguchi S. Closure of isolated ventricular septal defect with detachment of the tricuspid valve. J Card Surg 1995;10:564–8. [DOI] [PubMed]
- 5.Mullen JC, Lemermeyer G, Schipper SA, Bentley MJ. Perimembranous ventricular septal defect repair: keeping it simple. Can J Cardiol 1996;12:817–21. [PubMed]
- 6.Kapoor L, Gan MD, Bandyhopadhyay A, Das MB, Chatterjee S. Improved exposure of isolated perimembranous ventricular septal defects. Ann Thorac Surg 2000;69:291–2. [DOI] [PubMed]
- 7.Gaynor JW, O'Brien JE Jr, Rychik J, Sanchez GR, DeCampli WM, Spray TL. Outcome following tricuspid valve detachment for ventricular septal defects closure. Eur J Cardiothorac Surg 2001;19:279–82. [DOI] [PubMed]


