Abstract
Objective
To assess the long term effectiveness of the “green prescription” programme, a clinician based initiative in general practice that provides counselling on physical activity.
Design
Cluster randomised controlled trial. Practices were randomised before systematic screening and recruitment of patients.
Setting
42 rural and urban general practices in one region of New Zealand.
Subjects
All sedentary 40-79 year old patients visiting their general practitioner during the study's recruitment period.
Intervention
General practitioners were prompted by the patient to give oral and written advice on physical activity during usual consultations. Exercise specialists continued support by telephone and post. Control patients received usual care.
Main outcome measures
Change in physical activity, quality of life (as measured by the “short form 36” (SF-36) questionnaire), cardiovascular risk (Framingham and D'Agostino equations), and blood pressure over a 12 month period.
Results
74% (117/159) of general practitioners and 66% (878/1322) of screened eligible patients participated in the study. The follow up rate was 85% (750/878). Mean total energy expenditure increased by 9.4 kcal/kg/week (P=0.001) and leisure exercise by 2.7 kcal/kg/week (P=0.02) or 34 minutes/week more in the intervention group than in the control group (P=0.04). The proportion of the intervention group undertaking 2.5 hours/week of leisure exercise increased by 9.72% (P=0.003) more than in the control group (number needed to treat=10.3). SF-36 measures of self rated “general health,” “role physical,” “vitality,” and “bodily pain” improved significantly more in the intervention group (P<0.05). A trend towards decreasing blood pressure became apparent but no significant difference in four year risk of coronary heart disease.
Conclusion
Counselling patients in general practice on exercise is effective in increasing physical activity and improving quality of life over 12 months.
What is already known on this topic
Counselling patients in general practice on exercise has resulted in gains in physical fitness and activity, but no health benefits have been found
What this study adds
Counselling patients in general practice on exercise is effective in increasing physical activity and improving quality of life over 12 months without evidence of adverse effects
The intervention may reduce blood pressure by an average of 1-2 mm Hg over 12 months
No changes in the risk of coronary heart disease were observed
The intervention is sustainable in usual general practice
Prompting practice staff to deliver the intervention may have increased its effectiveness
Introduction
Physical inactivity is an independent risk factor for cardiovascular and other diseases.1 Interventions using physical activity can help to reduce cardiovascular risk factors, diabetes, obesity, osteoporosis, and symptoms of depression.1 Such interventions can also improve quality of life, which is an important predictor of physical functioning among older age groups.2
General practice in New Zealand and the United Kingdom is an ideal setting to identify sedentary adults and deliver brief interventions advising on physical activity as more than 80% of adults visit at least once a year.3 Although gains in physical fitness and activity have been reported after such interventions in general practice,4–6 health benefits have not. Findings from previous studies have had limited generalisability because patients were drawn from only one or two practices,5,6 or were mostly volunteers from high socioeconomic groups.4 This study assessed the effectiveness of a sustainable, clinician based initiative providing advice on physical activity, the “green prescription” (see box), by using a screening process for physical inactivity and delivery of the intervention during typical consultations in general practice among a diverse population.
The “green prescription” intervention
Primary care clinicians are offered four hours of training in how to use motivational interviewing techniques to give advice on physical activity and the green prescription
Patients who have been identified as “less active” through screening at the reception desk and who agree to participate receive a prompt card, stating their stage of change, from the researcher, to give to the general practitioner during consultation
In the consultation, the primary care professional discusses increasing physical activity and decides on appropriate goals with the patient. These goals, usually home based physical activity or walking, are written on a standard green prescription and given to the patient
A copy of the green prescription is faxed to the local sports foundation with the patient's consent. Relevant details such as age, weight, and particular health conditions are often included
Exercise specialists from the sports foundation make at least three telephone calls (lasting 10-20 minutes) to the patients over the next three months to encourage and support them. Motivational interviewing techniques are used. Specific advice about exercise or community groups is provided if appropriate
Quarterly newsletters from the sports foundations about physical activity initiatives in the community and motivational material are sent to participants. Other mailed materials, such as specific exercise programmes, are sent to interested participants
The staff of the general practice is encouraged to provide feedback to the participant on subsequent visits to the practice
Methods
Design
We used a cluster randomised controlled trial design. We stratified participating general practices by size and computer randomised them at a distant site before recruiting patients. Rolling recruitment of patients from each practice was spread evenly from April 2000 to April 2001. Researchers spent one week at each practice enrolling patients and completing baseline assessments.
Participants
All urban and rural general practitioners in the central and eastern Waikato region of New Zealand were invited to participate. This region spans 10 000 km2 and has a population of 200 000, including one metropolitan city and 10 small rural and semirural towns.
All patients aged 40-79 years who attended the participating practices during a five day period received a screening form, based on currently recommended levels of physical activity,1 to establish eligibility. One question on the form was: “As a rule, do you do at least half an hour of moderate or vigorous exercise (such as walking or a sport) on five or more days of the week?” Patients who answered in the negative were invited to participate in a clinical trial that entailed a lifestyle intervention delivered by their general practitioner.
Patients were excluded if practice personnel considered them to be too unwell to participate, if they had a debilitating medical condition or a known unstable cardiac condition, if they did not understand English, or if they were expecting to leave the region. Patients remained blind to whether they had been allocated to the intervention during screening for activity and enrolment. No patients were excluded after enrolment.
Measures
Primary outcome measures, evaluated at baseline and at 12 month follow up, included change in total expenditure of energy and leisure time expenditure of energy, cardiovascular risk (as assessed by systolic and diastolic blood pressure and coronary heart disease risk), and quality of life. Measures of potential harm included change in injuries and falls in the previous month and admission to hospital in the previous year. We used a self administered questionnaire from the Auckland heart study, which prompts for recall of physical activity over three months, to estimate total and leisure time expenditure of energy. This questionnaire had been validated among 113 randomly selected adults,7 and was revalidated by our team with a seven day activity diary and pedometer among 34 less active adults in a primary care population before the main study (unpublished data). We measured pulse and blood pressure with a Speidal and Keller OSZ 5 electronic sphygmomanometer after participants had been sitting quietly for at least five minutes. We took three recordings and used the average of the second and third readings. We obtained weight from electronic scales and height from a standard tape measure. In addition to measuring variables electronically we used signed witness statements of verification to minimise assessor bias. We obtained random serum lipid values from a venous sample taken by a researcher and analysed all samples on the day of collection at an ISO 9002 accredited laboratory. We also recorded current prescribed medications. We used the self administered “short form 36” (SF-36) questionnaire to assess quality of life outcomes.8
Delivery of intervention
After we had enrolled patients and ascertained their physical activity status, patients receiving the intervention used a form given by the researcher to prompt their general practitioner or practice nurse during the consultation to deliver the green prescription programme. General practitioners in the control group delivered usual care to participants in the study. Control patients were offered the intervention at the end of the study.
Sample size calculation
A sample size of 800 patients from 40 practices (α=0.05, power=90%) was required to detect differences in change between the intervention and control groups of one hour of moderate physical activity per week, 4.5 mm Hg systolic blood pressure, 10% relative risk of cardiovascular events, and six points of SF-36 “vitality.” We assumed an attrition rate of 25%. To account for the effect of clustering, we adjusted the sample size calculations by using intraclass correlation coefficients of 0.05, 0.016, 0.0036, and 0.05 for physical activity, blood pressure, cardiovascular risk, and “vitality,” respectively, based on estimates from previous studies.9–11
Analysis
We used a self report questionnaire from the Auckland heart study to record duration, frequency, and intensity of physical activities and rest during leisure time, occupation, at home, and during transport. We used an empirically based compendium to calculate expenditure of energy during leisure time and in total (kcal/kg/week).12 We calculated four year risk of coronary heart disease for participants under 75 years of age, using the Framingham equation for participants without previous cardiovascular disease and the D'Agostino equation for participants with previous cardiovascular disease.13,14
We carried out the coding and double data entry using Microsoft Access (1997). We analysed differences between intervention and control groups in change of outcome variables by using random effects models in Stata 7.0 (generalised least squares) and SAS 8.2 (mixed model), to allow for clustering by practice. All outcome analyses were by intention to treat, according to random allocation. We adopted a conservative method whereby baseline observations were carried forward for missing data of all outcome variables except four year risk of coronary heart disease. For this variable, mean increase in risk in the control population was used for participants who failed to attend follow up. We adjusted analysis of blood pressure for changes in medication.
Results
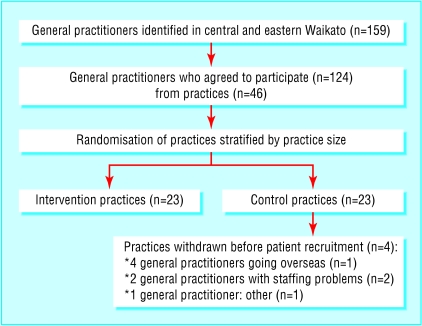
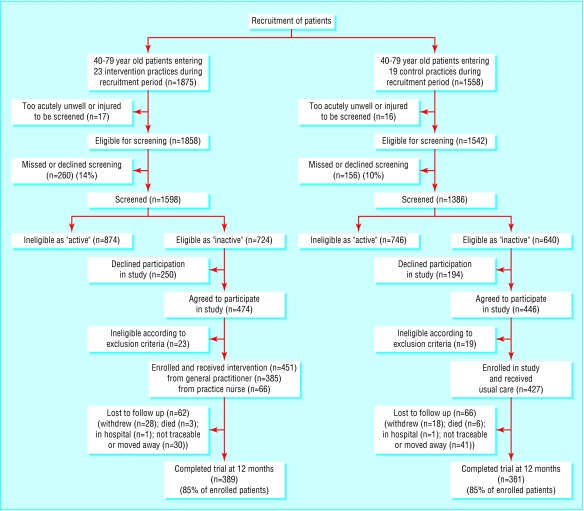
Figure 1 shows the practice recruitment rate (74%). Figure 2 shows screening of patients, recruitment, and follow up. Sixty six per cent of screened eligible patients (878/1322) were enrolled in the study. Follow up at 12 months was completed in 85% (750/878) of participants.
Figure 1.
Process of recruitment of general practitioners and randomisation of practices
Figure 2.
Progress of screening and recruiting patients and follow up stages of the trial after prior randomisation of practices
Of the 451 intervention patients, 385 received the intervention from a general practitioner and 66 from a practice nurse. Of the patients who attended follow up, 10/361 (2.8%) control and 370/389 (95%) intervention patients recalled receiving a green prescription during the previous year. Subsamples of 31 general practitioners and 19 nurses estimated spending an average of 7 minutes and 13 minutes per patient, respectively, delivering the green prescription intervention.
Table 1 shows close matching on baseline characteristics of intervention and control groups. Most primary outcome measures improved in both groups over 12 months. However, physical activity during leisure time and total expenditure of energy increased more in the intervention group than in the control group, as did the “general health,” “role physical,” “vitality,” and “bodily pain” scores on the SF-36 (table 2). Table 2 shows that systolic and diastolic blood pressure improved significantly from baseline in the intervention group, but the change did not differ significantly from that achieved in the control group. The difference in the change of risk of coronary heart disease between the two groups did not reach significance. The odds ratios of having a fall or injury in the previous month, or being admitted to hospital over the previous year at follow up compared with baseline were not significantly different between intervention and control groups. The odds ratios for intervention patients were 1.19 (95 confidence interval 0.82 to 1.72) for falls, 0.63 (0.44 to 0.896) for injuries, and 0.77 (0.60 to 0.996) for admissions to hospital. The odds ratios for control patients were 1.22 (0.85 to 1.75) for falls, 0.7 (0.48 to 1.02) for injuries, and 1.02 (0.796 to 1.33) for admissions to hospital.
Table 1.
Baseline characteristics of sedentary 40-79 year old patients in general practice, by intervention (n=451) and control group (n=427). Values are means (SD) unless otherwise indicated
| Variable
|
Intervention group
|
Control group
|
|---|---|---|
| Age (years) | 57.2 (10.8) | 58.6 (11.5) |
| Systolic blood pressure (mm Hg) | 135.1 (19.6) | 135.4 (17.9) |
| Diastolic blood pressure (mmHg) | 82.4 (12.2) | 81.8 (12.1) |
| Body mass index (kg/m2) | 30.0 (6.7) | 29.9 (6.4) |
| Cholesterol concentration* (mmol/l) | 5.78 (1.0) | 5.64 (1.0) |
| High density lipoprotein concentration* (mmol/l) | 1.33 (0.4) | 1.34 (0.4) |
| Four year risk of coronary heart disease* (%) | 5.7 (6.2) | 5.5 (5.8) |
| Total energy expenditure (kcal/kg/week) | 237.5 (42.2) | 235.7 (45.3) |
| Leisure physical activity† (kcal/kg1/week) | 6.0 (12.2) | 6.5 (11.1) |
| Leisure exercise‡ (minutes/day) | 11.3 (21.7) | 12.0 (20.5) |
| No of medical drugs taken | 2.6 (2.5) | 2.4 (2.4) |
| No (%) of participants: | ||
| Female | 301 (67) | 281 (66) |
| Lower economic status§ | 205 (45) | 211 (49) |
| With post-high school qualification | 106 (24) | 121 (28) |
| European origin | 354 (78) | 324 (76) |
| Smokers | 78 (17) | 76 (18) |
| Diabetic | 46 (10) | 46 (11) |
| Hypertensive¶ | 240 (53) | 220 (52) |
| Previous cardiovascular disease | 93 (21) | 74 (17) |
| Obese (BMI>30) | 198 (44) | 176 (41) |
| Taking leisure exercise ⩾2.5 hours/week | 80 (18) | 91 (21) |
| SF-36 quality of life scores (out of 100): | ||
| Physical functioning | 71.3 (23.9) | 70.9 (24.6) |
| Role physical | 57.9 (41.7) | 60.4 (41.4) |
| Bodily pain | 61.1 (25.7) | 63.9 (26.9) |
| General health | 62.7 (20.7) | 66.1 (20.6) |
| Vitality | 53.8 (20.6) | 56.0 (21.2) |
| Social functioning | 77.9 (24.6) | 77.6 (25.2) |
| Role emotional | 69.6 (41.3) | 68.7 (40.6) |
| Mental health | 74.5 (17.3) | 74.0 (18.2) |
| No (%) of general practices and doctors: | ||
| Rural or semirural practices | 12 (52) | 9 (47) |
| Female general practitioners | 17 (28) | 18 (31) |
Cholesterol testing and 4 year risk assessment of coronary heart disease13 14 were carried out on a randomly selected subsample to contain costs (n=787). A further 51 participants declined to have cholesterol testing done.
Leisure physical activity refers to the energy expenditure of all leisure time physical activity considered moderate or vigorous by the respondent.
Leisure exercise refers to minutes spent per week in leisure time activities of moderate or vigorous intensity that required at least three times the metabolic energy expenditure of sitting quietly (3 METs) when classified according to a standard physical activity compendium.12 15
Economic status was measured at baseline by qualification for a low income health subsidy card. 43% of adults over 45 years of age in New Zealand qualify for this card.
Hypertensive refers to a previous diagnosis of hypertension and taking antihypertensive medication or a mean blood pressure of greater than 150 mm Hg systolic or 90 mm Hg diastolic.
Table 2.
Mean changes (95% confidence intervals) in physical activity, cardiovascular, and quality of life outcomes in the control and intervention groups, at 12 months
| Measure
|
Intervention* (n=451)
|
Control*
|
Difference between groups† (n=878)
|
P value
|
|---|---|---|---|---|
| Primary outcomes: | ||||
| Total energy expenditure (kcal/kg/week) | 9.76 (5.85 to 13.68) | 0.37 (−3.39 to 4.14) | 9.38 (3.96 to 14.81) (975 kcal/week) |
0.001‡ |
| Leisure physical activity (kcal/kg/week) | 4.32 (3.26 to 5.38) | 1.29 (0.11 to 2.47) | 2.67 (0.48 to 4.86) (247 kcal/week) |
0.02§ |
| Leisure exercise (minutes/week) | 54.6 (41.4 to 68.4) | 16.8 (6.0 to 32.4) | 33.6 (2.4 to 64.2) | 0.04§ |
| Systolic blood pressure (mm Hg) | −2.58 (−4.02 to −1.13) | −1.21 (−2.57 to 0.15) | −1.31 (−3.51 to 0.89) | 0.2 |
| Diastolic blood pressure (mm Hg) | −2.62 (−3.62 to −1.61) | −0.81 (−1.77 to 0.16) | −1.40 (−3.35 to 0.56) | 0.2 |
| 4 year risk of coronary heart disease (%) | 0.42 (0.23 to 0.60) | 0.52 (0.32 to 0.72) | −0.10 (−0.43 to 0.23) | 0.6 |
| SF-36 quality of life scores: | ||||
| Physical functioning | 3.16 (1.61 to 4.71) | 1.63 (−0.04 to 3.31) | 1.23 (−1.35 to 3.81) | 0.3 |
| Role physical | 10.53 (6.8 to 14.3) | 4.16 (0.63 to 7.68) | 7.24 (0.16 to 14.31) | 0.045§ |
| Bodily pain | 6.51 (4.28 to 8.74) | 2.50 (0.15 to 4.86) | 4.01 (0.78 to 7.24) | 0.02§ |
| General health | 5.95 (4.43 to 7.47) | 1.60 (0.22 to 2.99) | 4.51 (2.07 to 6.95) | 0.000‡ |
| Vitality | 5.36 (3.76 to 6.96) | 3.06 (1.44 to 4.68) | 2.30 (0.03 to 4.57) | 0.047§ |
| Social functioning | 3.02 (0.68 to 5.36) | 2.85 (0.57 to 5.13) | 0.36 (−3.53 to 4.26) | 0.9 |
| Role emotional | 5.32 (1.43 to 9.21) | 5.70 (2.07 to 9.32) | −0.38 (−5.70 to 4.94) | 0.9 |
| Mental health | 2.61 (1.17 to 4.04) | 1.63 (0.28 to 2.98) | 0.98 (−0.99 to 2.95) | 0.3 |
| Other variables: | ||||
| Body mass index (kg/m2) | −0.11 (−0.25 to 0.02) | −0.05 (−0.18 to 0.07) | −0.06 (−0.24 to 0.12) | 0.5 |
| Cholesterol concentration (mmol/l) | −0.019 (−0.08 to 0.05) | 0.01 (−0.05 to 0.06) | −0.02 (−0.12 to 0.09) | 0.7 |
Unadjusted for clustering.
Adjusted for clustering by medical practice.
Significant at 0.01 level.
Significant at 0.05 level.
The proportion of participants in the intervention who achieved 2.5 hours of moderate or vigorous leisure physical activity per week increased by 66/451 (14.6%) compared with 21/427 (4.9%) in the control group (P=0.003), with a number needed to treat of 10.3. Increases in occupational activity contributed substantially to the additional increase in total energy expenditure (P<0.001), although domestic and transport activity did not. Post hoc analysis by sex showed that physical activity during leisure time increased by 68 minutes (95% confidence interval 29 minutes to 106 minutes) per week in men (n=296), and 20 minutes (−23 minutes to 63 minutes) per week in women (n=582).
Discussion
The green prescription intervention in general practice is effective in increasing participants' physical activity and improving quality of life over 12 months without evidence of adverse effects. A trend towards decreasing blood pressure also became obvious, but we detected no significant change in the risk of coronary heart disease.
For every 10 green prescriptions written, one person achieved and sustained 150 minutes of moderate or vigorous leisure activity per week, at 12 months. Achieving this amount of activity (using up an additional 1000 kcal/week) is associated with a 20-30% risk reduction in all cause mortality compared with sedentary individuals.16
Limitations
This study did not have sufficient statistical power to detect a change in blood pressure of 1.4 mm Hg as sample size calculations used larger estimates from previous reviews of exercise and blood pressure.17 The clinical significance of such a small change in blood pressure across a population is also questionable. However, a reduction of diastolic blood pressure of 2 mm Hg in an adult population could lower the prevalence of hypertension by 17%, the risk of coronary heart disease by 6%, and the risk of strokes and transient ischaemic attacks by 15%.18 Changes in blood pressure in this study resemble long term changes achieved by other lifestyle interventions such as weight loss or salt reduction programmes.19
Using multiple comparisons to assess the three primary outcomes may incur a risk of detecting an effect where none exists (type I error). However, if predefined multiple outcomes are needed to show several effects multiple comparisons can be justified without the need for adjustment.20 Although a significant increase in leisure energy expenditure could be shown in isolation, ensuring that total energy expenditure had not decreased overall is important. In addition, an attempt was made to detect some of the potential benefits for health and quality of life from a physical activity intervention. Although this study was not powered to perform subanalyses by sex, men tended to increase their activity more than women. More research is needed to clarify the reasons behind sex differences in the success or failure of particular interventions.
Strengths
The findings of this study have widespread generalisability as the study included a socioeconomically diverse sample from a large geographical region, and rates of participation were high. The green prescription intervention is sustainable and has been used by more than 50% of general practitioners in New Zealand.21 This study used a true control group, and the patients prompted their usual general practitioner or nurse to deliver the intervention. Thus it differs from previous studies that did not find a change of outcome of physical activity in the long term and may indicate the importance of prompting by the patient and the role of the usual practitioner as an agent of intervention, as opposed to a visiting activity specialist.22
We used a systematic screening process, few exclusion criteria, self administered questionnaires, objective and electronic health measures, and signed witness statements of results to minimise the risk of recruitment and assessor bias resulting from the lack of blinding. Baseline characteristics were well balanced. As with other physical activity trials, a risk existed of recall or social desirability bias when using self reported physical activity as an outcome measure. However, the physical activity questionnaire used in this trial was validated before the trial against pedometers and seven day diaries among less active adults in general practice. Using questionnaires to record information on physical activity has been shown to be both practical and valid for epidemiological study compared with more objective measures such as motion sensors, heart rate monitoring, and doubly labelled water.23,24 The trial was clustered by practice to reduce the risk of the intervention being contaminated. This technique also meant that study participants were less aware of differences between intervention and control arms, but both were aware that they were part of a study that asked about exercise. As such we suspected that any “social desirability” bias may well apply to the control and intervention groups in similar ways.
Implications
To evaluate cardiovascular benefits, larger samples capable of detecting smaller blood pressure changes and longer follow up periods are recommended. Alternatively, more intensive continuing support may improve compliance and the health benefit, as has been shown elsewhere.4 However, this study has shown that prompting the usual general practitioner for brief advice, coupled with ongoing telephone support, can change people's behaviour with respect to physical activity and improve self rated variables including general health, vitality, role physical, and bodily pain for at least a year. If implemented widely, such a strategy could result in major health benefits for sedentary people.
Footnotes
Funding: The National Heart Foundation of New Zealand, Hillary Commission, Waikato Medical Research Foundation, Royal New Zealand College of General Practitioners, and the University of Auckland.
Competing interests: A minor funder of this study was the Hillary Commission, a publicly and government funded organisation that promotes sport and recreation in New Zealand. The Hillary Commission (now known as SPARC, Sport and Recreation New Zealand) produces resources associated with the green prescription initiative and funds its promotion. This organisation played no part in the design, analysis, or writing of the paper.
Ethical approval: The study was approved by the Waikato Ethics Committee in 1999.
References
- 1.Centers for Disease Control and Prevention. Physical activity and health: a report of the surgeon general. Atlanta: US Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion; 1996. [Google Scholar]
- 2.Spirduso WW, Cronin DL. Exercise dose-response effects on quality of life and independent living in older adults. Med Sci Sports Exerc. 2001;33(6 suppl):S598–S608. doi: 10.1097/00005768-200106001-00028. ; discussion S609-10. [DOI] [PubMed] [Google Scholar]
- 3.Ministry of Health. Taking the pulse—1996-97 New Zealand health survey. Wellington: MoH; 1998. www.moh.govt.nz/moh.nsf/ea6005dc347e7bd44c2566a40079ae6f/d7b3cf1eee94fefb4c25677c007ddf96 (accessed 4 Mar 2003). [Google Scholar]
- 4.The Writing Group for the Activity Counseling Trial Research Group. Effects of physical activity counseling in primary care. JAMA. 2001;286:677–687. doi: 10.1001/jama.286.6.677. [DOI] [PubMed] [Google Scholar]
- 5.Halbert JA, Silagy CA, Finucane PM, Withers RT, Hamdorf PA. Physical activity and cardiovascular risk factors: effect of advice from an exercise specialist in Australian general practice. Med J Aust. 2000;173:84–87. doi: 10.5694/j.1326-5377.2000.tb139250.x. [DOI] [PubMed] [Google Scholar]
- 6.Stevens W, Hillsdon M, Thorogood M, McArdle D. Cost-effectiveness of a primary care based physical activity intervention in 45-74 year old men and women: a randomised controlled trial. Br J Sports Med. 1998;32:236–241. doi: 10.1136/bjsm.32.3.236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Arroll B, Jackson R, Beaglehole R. Validation of a three-month physical activity recall questionnaire with a seven-day food intake and physical activity diary. Epidemiology. 1991;2:296–299. doi: 10.1097/00001648-199107000-00011. [DOI] [PubMed] [Google Scholar]
- 8.McHorney CA, Ware JE, Jr, Raczek AE. The MOS 36-item short-form health survey (SF-36): II. Psychometric and clinical tests of validity in measuring physical and mental health constructs. Med Care. 1993;31:247–263. doi: 10.1097/00005650-199303000-00006. [DOI] [PubMed] [Google Scholar]
- 9.Campbell MK, Mollison J, Steen N, Grimshaw JM, Eccles M. Analysis of cluster randomized trials in primary care: a practical approach. Fam Pract. 2000;17:192–196. doi: 10.1093/fampra/17.2.192. [DOI] [PubMed] [Google Scholar]
- 10.Kerse N. Health promotion and older people: a general practice intervention study. University of Melbourne. 1998. (PhD thesis). [Google Scholar]
- 11.Kerry S, Bland J. Intracluster correlation coefficient in cluster randomisation. BMJ. 1998;316:1455. doi: 10.1136/bmj.316.7142.1455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ainsworth BE, Haskell WL, Leon AS, Jacobs DR, Jr, Montoye HJ, Sallis JF, et al. Compendium of physical activities: classification of energy costs of human physical activities. Med Sci Sports Exerc. 1993;25:71–80. doi: 10.1249/00005768-199301000-00011. [DOI] [PubMed] [Google Scholar]
- 13.Anderson KM, Odell PM, Wilson PW, Kannel WB. Cardiovascular disease risk profiles. Am Heart J. 1990;121:293–298. doi: 10.1016/0002-8703(91)90861-b. [DOI] [PubMed] [Google Scholar]
- 14.D'Agostino RB, Russell MW, Huse DM, Ellison RC, Silbershatz H, Wilson PW, et al. Primary and subsequent coronary risk appraisal: new results from the Framingham study. Am Heart J. 2000;139:272–281. doi: 10.1067/mhj.2000.96469. [DOI] [PubMed] [Google Scholar]
- 15.Lamonte MJ, Ainsworth BE. Quantifying energy expenditure and physical activity in the context of dose response. Med Sci Sports Exerc. 2001;33(6 suppl):S370–S378. doi: 10.1097/00005768-200106001-00006. ; discussion S419-20. [DOI] [PubMed] [Google Scholar]
- 16.Lee IM, Skerrett PJ. Physical activity and all-cause mortality: what is the dose-response relation? Med Sci Sports Exerc. 2001;33(6 suppl):S459–S471. doi: 10.1097/00005768-200106001-00016. ; discussion S493-4. [DOI] [PubMed] [Google Scholar]
- 17.Halbert JA, Silagy CA, Finucane P, Withers RT, Hamdorf PA, Andrews GR. The effectiveness of exercise training in lowering blood pressure: a meta-analysis of randomised controlled trials of 4 weeks or longer. J Hum Hypertens. 1997;11:641–649. doi: 10.1038/sj.jhh.1000509. [DOI] [PubMed] [Google Scholar]
- 18.Cook NR, Cohen J, Hebert PR, Taylor JO, Hennekens CH. Implications of small reductions in diastolic blood pressure for primary prevention. Arch Intern Med. 1995;155:701–709. [PubMed] [Google Scholar]
- 19.Effects of weight loss and sodium reduction intervention on blood pressure and hypertension incidence in overweight people with high-normal blood pressure. The Trials of Hypertension Prevention Collaborative Research Group. Arch Intern Med. 1997;157:657–667. [PubMed] [Google Scholar]
- 20.Perneger TV. What's wrong with Bonferroni adjustments. BMJ. 1998;316:1236–1238. doi: 10.1136/bmj.316.7139.1236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Intercontinental Medical Statistics Health (NZ) Limited. Green prescriptions in general practice. Auckland: IMS NZ; 1999. [Google Scholar]
- 22.Harland J, White M, Drinkwater C, Chinn D, Farr L, Howel D. The Newcastle exercise project: a randomised controlled trial of methods to promote physical activity in primary care. BMJ. 1999;319:828–832. doi: 10.1136/bmj.319.7213.828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sobngwi E, Mbanya JC, Unwin NC, Aspray TJ, Alberti KG. Development and validation of a questionnaire for the assessment of physical activity in epidemiological studies in Sub-Saharan Africa. Int J Epidemiol. 2001;30:1361–1368. doi: 10.1093/ije/30.6.1361. [DOI] [PubMed] [Google Scholar]
- 24.Philippaerts RM, Westerterp KR, Lefevre J. Doubly labelled water validation of three physical activity questionnaires. Int J Sports Med. 1999;20:284–289. doi: 10.1055/s-2007-971132. [DOI] [PubMed] [Google Scholar]