Abstract
Human parainfluenza viruses (HPIV) were first discovered in the late 1950s. Over the last decade, considerable knowledge about their molecular structure and function has been accumulated. This has led to significant changes in both the nomenclature and taxonomic relationships of these viruses. HPIV is genetically and antigenically divided into types 1 to 4. Further major subtypes of HPIV-4 (A and B) and subgroups/genotypes of HPIV-1 and HPIV-3 have been described. HPIV-1 to HPIV-3 are major causes of lower respiratory infections in infants, young children, the immunocompromised, the chronically ill, and the elderly. Each subtype can cause somewhat unique clinical diseases in different hosts. HPIV are enveloped and of medium size (150 to 250 nm), and their RNA genome is in the negative sense. These viruses belong to the Paramyxoviridae family, one of the largest and most rapidly growing groups of viruses causing significant human and veterinary disease. HPIV are closely related to recently discovered megamyxoviruses (Hendra and Nipah viruses) and metapneumovirus.
INTRODUCTION
Over the last decade, there has been considerable change in both the nomenclature and taxonomic relationships of human parainfluenza viruses (HPIV) (Table 1). These viruses were first discovered in the late 1950s, when three different viruses recovered from children with lower respiratory disease proved to by unique and easily separated from the myxoviruses (influenza virus) they closely resembled. This new family of respiratory viruses grew poorly in embryonated eggs and shared few antigenic sites with influenza virus. In 1959, a fourth virus was found that also met these criteria, and a new taxonomic group was created called “parainfluenza viruses.”
TABLE 1.
Taxonomic relationships of HPIV types within the family Paramyxoviridae
| Subfamily and genus | Species
|
|
|---|---|---|
| Human | Animal | |
| Paramyxovirinae | ||
| Respirovirus | HPIV-1, HPIV-3 | Sendai (mouse PIV-1), bovine PIV-3, simian PIV-10 |
| Rubulavirus | HPIV-2, HPIV-4A, HPIV-4B, Mumps virus | NDV (1), Yucaipa virus (2), Kunitachi virus (5), avian PIV-3, avian PIV-4, avian PIV-6 to PIV-9 |
| La-piedad-Michoacan Mexico porcine virus, simian PIV-5 and PIV-41 | ||
| Morbillivirus | Measles virus | Canine distemper virus, rinderpest virus (bovine), pest-des-petits-ruminants virus, dolphine distemper virus, porpoise distemper virus, phocine distemper virus |
| Megamyxovirus | Hendra virus, Nipah virus | HeV (equine, (bats?), NIV (porcine, bats?) |
| Pneumovirinae | ||
| Pneumovirus | RSV | Bovine RSV, pneumonia virus of mice |
| Metapneumovirus | HMPV | Avian pneumovirus (APV) |
HPIV is genetically and antigenically divided into types 1 to 4. Further major subtypes of HPIV-4 (A and B) (36) and subgroups/genotypes of HPIV-1 (136, 139, 140, 143) and HPIV-3 (292) have been described. HPIV-1 to HPIV-3 are major causes of lower respiratory infections in infants, young children, the immunocompromised, the chronically ill, and the elderly (22, 70, 86, 87, 115, 116, 237, 254, 381). These medium-sized viruses are enveloped, and their genomes are organized on a single negative-sense strand of RNA. The majority of their structural and biological charactertistics are similar, but they each have adapted to infect humans at different ages and cause different diseases. These viruses belong to the Paramyxoviridae family, which is a large rapidly growing group of viruses that cause significant human and veterinary disease. In fact, this virus family is one of the most costly in terms of disease burden and economic impact to our planet. Recently discovered members of the Paramyxoviridae (megamyxoviruses [Hendra and Nipah viruses] and metapneumovirus) emphasize this point (53, 254, 265, 360).
(Portions of this article have been rewritten from reference 143a with permission.)
VIROLOGY BASICS
There are now two genera of HPIV, Respirovirus (HPIV-1 and HPIV-3) and Rubulavirus (HPIV-2 and HPIV-4). Both genera (paramyxoviruses) can be separated morphologically from influenza virus (myxoviruses) by their nonsegmented thick nucleocapsids (17 nm versus 9 nm) (43, 196). Other genera of the Paramyxoviridae can be physically distinguished from HPIV by the absence of a neuraminidase (morbilliviruses, e.g., measles virus and distemper virus) or a thiner nucleocapsid (pneumoviruses, e.g., respiratory syncytial virus [RSV], or metapneumoviruses). The megamyxoviruses are still being described but appear more closely related to morbilliviruses phylogenetically than to the HPIV.
Structural Organization
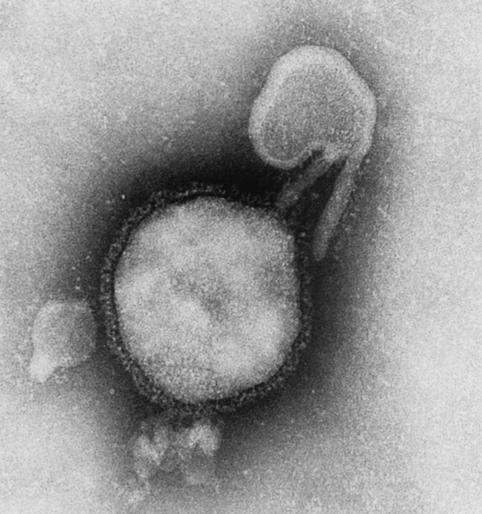
By electron microscopy, HPIV are demonstrated to be pleomorphic enveloped viruses (Fig. 1). Their envelope is derived from the host cell that they last infected. This family of viruses are medium sized, between 150 and 250 nm, but much larger virions or virus aggregates have been reported (159, 196, 197). Virus particles usually contain single-stranded RNA with negative polarity (complementary to mRNA). Virions with a positive polarity have been reported, but these are thought to be noninfectious (196). The HPIV genome contains approximately 15,000 nucleotides (343, 376). These are organized to encode at least six common structural proteins (3′-N-P-C-M-F-HN-L-5′) (349). During the last decade, reverse genetic systems were developed that demonstrated a “rule of six” for HPIV. Simply stated, this means that the most efficient replication and transcription of HPIV takes place when the genome is divisible by 6, although exceptions have been found (77, 151, 199).
FIG. 1.
Electron micrograph of HPIV-3. Surface glycoproteins are easily visualized. Magnification, ×275,000.
Electrophoresis demonstrates great similarity in protein size between the four major HPIV types except for the phosphoprotein (P). HPIV-2 and HPIV-4 have a phosphoprotein with a molecular weight (MW) of 49,000 to 53,000 versus 83,000 to 90,000 for HPIV-1 and HPIV-3 (59, 70, 203, 313, 339, 343, 376, 396). The largest HPIV protein is the “large” (L) nucleocapsid protein (polymerase, MW 175,000 to 251,000), followed by P (HPIV-1 and HPIV-3). These two viral proteins and the nucleocapsid protein (N or NP) [MW 66,000 to 70,000] are closely associated with the viral RNA (vRNA). Two surface glycoproteins are found in all HPIV: the hemagglutinin-neuraminidase (HN) (MW 69,000 to 82,000) and the fusion protein (Fo) (MW 60,000 to 66,000). Finally, the membrane protein (M) (MW 28,000 to 40,000) is strongly associated with and found just beneath the viral membrane. It is important to note that some of these proteins undergo extensive posttranslational modification (e.g., glcosylation or phosphorylation) and the MW as calculated from cloning and sequencing data can differ considerably from that seen on gel electrophoresis. The P gene of some paramyxoviruses produces many small nonstructural proteins from multiple overlapping reading frames. Additional editing of the mRNA may occur to produce these proteins. For example, HPIV-1, HPIV-2, and HPIV-3 encode a nonstructural protein (C) (234, 274, 339). HPIV-2 (and maybe HPIV-3) has an additional nonstructural protein (V), which HPIV-1 does not contain (79, 234, 335). This protein appears to have several actions. It binds N and may play a role in regulating viral replication (375). However, the V protein distribution (nuclei and cytoplasm) does not appear to be similar to that of the N or P protein (cytoplasmic granules) within virus infected cells (269). Recent work suggests that slowing the cell cycle might be one way the V protein favors viral replication (215). In addition, it may be involved in Rubulavirus inhibition of the interferon response by inducing the degradation of STAT1 and/or STAT2 (60, 119, 188, 268). The C protein of PIV-1 (Sendai virus) may perform the same function (268). This interferon interaction with V and C proteins may be important in determining the host range for some HPIV. HPIV-3 appears to have a unique nonstructural protein, D, which is a chimera between the upstream half of P and a second internal open reading frame (209).
vRNA, together with the N, P, and L proteins, form the nucleocapsid core of HPIV. The N binds to the vRNA (one N protein to six nucleotides), making a template that allows the L (RNA-dependent RNA polymerase) and P proteins to transcribe and eventually replicate the HPIV genome (43). The P protein of HPIV is probably a homotrimer (64). The surface glycoproteins (HN and F) interact with the M protein, which may direct their insertion and aggregation at specific cell membrane locations. The M protein also appears to play a role in attracting completed nucleocapsids to areas of infected cell membrane that will soon become viral envelope and may be involved in viral budding (51, 57, 209, 283).
The HN protein is found on the lipid envelope of HPIV and infected cells (136, 280, 351). There it most probably exists as a tetramer and functions in virus-host cell attachment via sialic acid receptors, suggesting that it has neuraminidase activity (important for virus release from cells). There are significant differences in the number of HN glycosylation sites between HPIV types and among strains within one type (139, 140, 143). This may be part of the strategy used by HPIV to escape immune detection. The terminal sialic acid sequences important for HN binding of HPIV are just beginning to be worked out (345). It appears that HPIV-1 HN is more limited in its binding than HPIV-3 HN, which may be important for host and tissue range. It is the binding of the HN protein to receptors on red blood cells that creates the well-recognized hemagglutination or hemadsorption of paramyxoviruses. Elegant work by Moscona and Paluso has demonstrated that the HN-cell receptor interaction is specific and complex. It involves both surface glycoproteins and varies between HPIV types. F protein-mediated cell fusion is affected by the affinity of the HPIV-3 HN to its receptor(s) (251). In addition, cell-to-cell fusion requires a minimum density of receptors which is greater than the density needed for virus membrane-cell membrane fusion (infection). The enzymatic removal of sialic acid receptors from HPIV can create persistently infected tissue cultures. This is one explanation for HPIV-3 persistence in vitro, but in vivo persistence may have additional mechanisms. Persistent infection with HPIV-2 appears to use a different mechanism (2).
As mentioned above, the HPIV F protein is integral in virus-host cell membrane fusion. It is this fusion of membranes which allows the viral nucleocapsid to enter and infect a host cell. Also, this protein is needed in membrane fusion between host cells (syncytial formation) and causes hemolysis. Initially an inactive precursor (F0) is made, which must be cleaved by an endopeptidase to yield the active F protein, which is composed of two disulfide-linked molecules (F1 and F2). The new N terminus on F1 is highly hydrophobic and is thought to make the first contact with the lipid membrane during virus-cell fusion. Furin and Kex2 have been proposed as the enzymes responsible for this proteolytic cleavage in humans (278), but trypsin is most frequently used in vitro. The host range and virulence of HPIV is strongly influenced by the enzymes that cleave the Fo precuror. The ability of the F protein to independently induce both fusion and hemolysis varies among the different HPIV types. HPIV-1, HPIV-2, and HPIV-3 in vitro require both HN and F for fusion and hemolysis (80, 252, 278, 395). The structure and location of the physical interactions between the HN and F proteins responsible for their functional interactions, including fusion promotion, oligomer formation, and cell surface expression, are still being determined (143, 275, 347, 397).
Viral Replication
The first event in viral reproduction is the fusion of the virus and host cell lipid membranes. This is followed by the expulsion of the HPIV nucleocapsid into the cytoplasm of the cell. Once in the cytoplasm, transcription takes place by using virus-specific RNA-dependent RNA polymerase (L protein). Cellular ribosomal machinery then translates the viral mRNAs into viral proteins. These direct the full-length replication of the virus genome, first into a positive-sense RNA strand and then into the appropriate negative strand. Once produced, these single negative-sense strands of RNA are then encapsidated with NP and may be used in further rounds of transcription and replication or may be packaged for export as a new virion (196, 197).
Interactions with the Environment
Environmental conditions such as temperature, humidity, pH, and the composition of the storage fluid easily affect HPIV. Viral survival markely decreases at temperature above 37°C, until at 50°C almost all virus is inactivated within 15 min (401). Room temperature storage of myxoviruses has demonstrated considerable survival variability by decreasing titers by >50% in as little as 2 h or as long as 1 week, but this rate averages closer to hours than days (16, 127, 131, 354, 401). HPIV have their greatest stability at 4°C or if frozen (e.g., −70°C). Even thought freezing causes loss of infectivity and virus destruction (>90% at times), the small amount of infectivity that is left must be sufficient for virus recovery (279, 401). HPIV-1 can be recovered even after 26 years of being frozen (−70°C), with a recovery rate greater then 90% (K. J. Henrickson, unpublished data). The addition of several reagents (e.g., 0.5% bovine serum albumin, skim milk, 5% dimethyl sulfoxide, or 2% chicken serum) to HPIV prior to freezing has been shown to prolong survival (47, 165, 401). In addition, optimal stability of HPIV occurs at physiologic pH (7.4 to 8.0), while infectivity is rapidly lost at pH 3.0 to 3.4 (131, 132), under low humidity (244), and with virus desiccation (6, 29). HPIV and all myxoviruses are inactivated by ether (5).
Serotypes
HPIV has four predominant serotypes. Serologic and antigenic analysis of all of the species within the Paramyxovirinae subfamily demonstrates four basic genera (Table 1): (i) HPIV-1, HPIV-3, Sendai virus, and bovine PIV-3; (ii) HPIV-2, HPIV-4, mumps virus, and simian viruses 5 and 41; (iii) measles and distemper viruses (136, 298, 301, 356); and (iv) the new megamyxoviruses. The HPIV all induce variable levels of heterotypic antibody during infection and have common antigens. This often makes it impossible to determine whether serologic positivity represents specific amnestic responses or cross-reactions to similar antigens on different HPIVs. However, specific hyperimmune animal serum (e.g., hamster or guinea pig) can usually differentiate between these viruses in standard hemagglutinin inhibition (HI), hemadsorption inhibition (HAdI), complement fixation, or neutralization tests or enzyme-linked immunosorbent assay (ELISA) (37, 317).
Two major subtypes of HPIV-4 (A and B) were discovered shortly after this virus was first identified 40 years ago. HAdI and neutralization assays could easily distinguish these subtypes, but complement fixation could not (36). During the same decade, several HPIV-2 strains were isolated that could be differentiated serologically from the type stain (272), and then about 10 years ago studies demonstrated significant antigenic variation between different HPIV-2 clinical isolates (302). At about the same time, strains of HPIV-1 were reported that could be separated from the type strain by ELISA, HI, and neutralization assays (143). Molecular analyses of all four types have demonstrated more antigenic and genetic heterogeneity than was initially appreciated (136, 139, 140, 143, 200, 201, 356, 362, 398). In fact, the data suggest that all four major HPIV serogroups (HPIV-1 to HPIV-4) have subgroups or populations that have unique antigenic and genetic characteristics. Even HPIV-4 subtypes A and B demonstrate this variability (201). The variability and changes seen in HPIV suggest an evolutionary pattern similar to that of influenza B virus. Polyclonal serologic testing can detect most HPIV strains using common “type” antigens, but subgroups of HPIV-1 (A, C, and D) and HPIV-3 have been reported with progressive antigenic change (143). In addition, HPIV-1 strains isolated over the last 12 years demonstrate persistent antigenic and genetic differences compared to the 1957 type strain, including differences between genotypes within the same epidemic and same geographic location (136, 139, 140, 143, 200). This progressive antigenic change (although slow) will cause standard reference sera raised to HPIV isolates from the 1950s, or antigen prepared from these same “type” strains, to not universally react in routine serologic assays in the future. Examples of this have already occurred, leading to failure of commercial diagnostic products. Investigators now often use more recent strains of HPIV as sources of antigen or genomic material.
Growth in Cell Culture
A number of primary and secondary cell lines support the growth of HPIV. The most common are LLC-MK2, Vero, CV-I, primary cynomologus and rhesus monkey kidney, Wish, HMV-II, HEp-2, MDCK, BHK, HeLa, primary human embryo, KB, Am, HEB′ L929, and HEF (19, 96, 112, 223, 250, 252, 271, 311, 324). HPIV can also replicate in organ cultures from mouse, guinea pig, ferret, and human fetal respiratory epithelium (204). Primary monkey kidney tissue culture is more sensitive to initial isolation of HPIV-1 and HPIV-2 than is LLC-MK2 culture but is prone to foamy virus contamination. If contamination occurs, it does not usually interfere with HPIV detection.
HPIV are isolated more easily in epithelial cell lines than in fibroblast cell lines. The addition of an exogenous protease (trypsin) to the cell culture medium facilitates virus recovery for some serotypes and strains of HPIV. All HPIV need to have their F0 protein cleaved and activated into F1 and F2 for efficient growth in cell culture. Cell lines vary in their ability to produce the apporgriate proteases. For example, HPIV-3 grows efficiently in PMK cells and to high titer in LLC-MK2 cells with serum-free medium, but the addition of trypsin allows increased infectivity in HEp-2 cells (311). HPIV-1, HPIV-2, and HPIV-4 demonstrate greater replication in Vero cells in the presence of trypsin (249, 323). HPIV-1 has a strict and specific requirement for trypsin or a trypsin-like protease in LLC-MK2 cells. HPIV-1, HPIV-2, and HPIV-3 all can be recovered in PMK cells (e.g., cynomologus and rhesus monkey cells) without trypsin (11). However, there is variability between species of PMK cells and the ability to efficiently grow HPIV because the addition of trypsin increases viral recovery in African green monkey PMK cells (138).
CPE
PMK cells rarely show cytopathic effects (CPE) when infected with the majority of HPIV isolates. A small number of HPIV-2 and HPIV-3 clinical isolates may demonstrate focal rounding and destruction, elongated cells, and occasional syncytia on initial isolation. All HPIV demonstrate greater CPE on adaption to a particular cell line, with HPIV-3 being the most aggressive. Well-adapted strains of HPIV-3 can destroy more than 50% of a tissue culture monolayer by the third day.
Host Range
HPIV can infect many different animals both naturally and under experimental conditions. Asymptomatic infection can be induced in hamsters, guinea pigs, and adult ferrets by all four HPIV types (37, 47, 174, 233, 304). However, fatal disease is caused by infection with HPIV-1 to HPIV-3 in newborn ferrets (233). Interestingly, HPIV-3 causes clinically asymptomatic infection in cotton rats and hamsters, but on autopsy significant respiratory pathology and virus replication can be demonstrated (193, 290). HPIV-3 induces hyperreactivity in the tracheas of guinea pigs and neonatal hydrocephalus in hamsters whose mothers were intervenously inoculated (35, 346). Primates are easily infected with HPIV, but almost all infections are asymptomatic. Chimpanzees, macaques, and squirrel, owl, patas, and rhesus monkeys have been asymptomatically infected with HPIV-3 or HPIV-4 (202, 337, 363), and only marmosets have developed symptomatic upper respiratory infections (URI) with HPIV-3 and Sendai virus (133).
There are numerous PIV closely related to HPIV that have adapted to other mammalian species. HPIV-1 has antigenic, genetic, and pathophysiologic homology to Sendai virus, which infects mice, hamsters, and pigs (47, 169, 293). Simian viruses 5 and 41 are related to HPIV-2 and infect primates (161, 243, 298). Another virus related to both HPIV-2 and simian virus 5 is canine parainfluenza virus (CP2), which causes croup and lower respiratory infection (LRI) in dogs (15, 282). Bovine PIV-3 has been associated with “shipping fever” in cattle, and is antigenically related to HPIV-3 (387). This virus or similar viruses may also infect horses, sheep, goats, water buffaloes, deer, dogs, cats, monkeys, guinea pigs, rats, and pigs (1, 91, 225, 290). Some PIV can infect nonmammalian species. A rubulovirus, Newcastle disease virus, infects poultry, penguins, and other birds and has been responsible for conjunctivitis in bird handlers and laboratory workers (3, 28, 264). There have been reports of human infections by some of the other nonhuman PIV, but these have not been well established (21, 161, 298, 387).
Viral Antigens
Whole virus and chemically or physically disrupted HPIV can be used to yield many useful antigens. The membrane-associated proteins HN, F, and M can be separated from the nuceocapsid (N, L, P, and RNA) by treatment with various detergents (or ether) and ultracentrifugation. Dialysis and column chromatography can then be used for further purification and separation. Many of the genes for the structural proteins of HPIV have been cloned, and the viral proteins have been produced in appropriate expression vectors, but these are not available commercially. The above methods produce useful individual HPIV antigens for most laboratory purposes. In addition, the HPIV membrane can be disrupted by buffer with 0.5% Triton X-100 to yield an antigenic preparation that works well in ELISA. Sodium dodecyl sulfate-treated whole virus works well in polyacrylamide gel electrophoresis and Western blot analysis. HPIV treated with NP-40 to disrupt the viral membrane produces a reagent that works well in radioimmune precipitation. Whole undisrupted virus (no detergent) is useful for laboratory work involving unmodified surface glycoproteins (HN and F), for example hemagglutination, HI, HAdl, and neuraminidase assays.
Viral Reagents
Polyclonal or monoclonal antibodies can be made using any portion of HPIV. The intranasal inoculation of whole virus into guinea pigs or hamsters produces a specific hyperimmune serum that works well in standard serologic tests (37). Prior to immunization, animals need to be screened for naturally occurring (cross-reacting) PIV antibody and then kept isolated. A repeat (booster) immunization should be given 2 to 3 weeks following the initial antigenic priming. Low-level heterotypic antibody production often is produced, and the commercial animal antiserum that has been available to HPIV-1 and HPIV-3 has had problems with cross-reactivity to HPIV-2. If more specific antiserum is being made using viral subunits, then adjuvants may need to be used and immunizations are usually intermuscular, intradermal, or intravenous. Monoclonal antibodies (MAbs) have been produced to all four major serotypes of HPIV and are commercially available. Usually these MAbs are very specific, although minor cross-reactivity has been reported (136). These serologic reagents can be used for virus detection in ELISA, immunofluorescence (IF) assays, HI, HAdl, complement fixation, Western blotting, radioimmunoprecipitation, and neutralization assays. HPIV antigen detection using a modification of the ELISA technique (time-resolved fluorometry) may be more sensitive than standard ELISA (147). However, as described above, HPIV antigenic variation is occurring steadily and many MAbs no longer bind and/or function in ELISA or in HI or neutralization assays. Assays utilizing MAbs may in the future need to routinely contain multiple different antibodies for maximum sensitivity.
EPIDEMIOLOGY AND CLINICAL FEATURES
HPIV are common community-acquired respiratory pathogens without ethnic, socioeconomic, gender, age, or geographic boundaries. Many factors have been found that predispose to these infections, including malnutrition, overcrowding, vitamin A deficiency, lack of breast feeding, and environmental smoke or toxins (22, 38, 192, 237, 355). There are more than 5 × 106 LRI each year in the United States in children younger than 5 years (70, 116). HPIV-1 to HPIV-3 have been found in as many as one-third of these infections (70, 116, 259). In addition, HPIV cause URI in infants, children, and adults and, to a lesser extent, LRI in the immunocompromised, those with chronic diseases (e.g., heart and lung disease and asthma) and the elderly (86, 87, 115, 116, 207, 259, 381). Less is known about HPIV-4. Young infants and children are clearly infected by this virus, but it is rarely isolated. Serologic surveys have demonstrated that most children between 6 and 10 years of age have evidence of past infection, suggesting mild or asymptomatic primary infections (110). Acute respiratory infections cause 3 to 18% of all admissions to pediatric hospitals, and HPIV can be detected in 9 to 30% of these patients depending on the time of year (38, 75, 259; K. J. Henrickson, S. H. Hoover, K. S. Kehl, and W. Hua, submitted for publication). There are between 500,000 and 800,000 LRI hospitalizations (in persons younger than 18 years) in the United States each year, with approximately 12% being for HPIV-1, HPIV-2, and HPIV-3 infections (322). This is second only to RSV as a cause of hospitalization for viral LRI. Immunity to HPIV is incomplete, and infections occur throughout life; however, less is known about infections in adults. Therefore, the majority of the clinical discussion will focus on children.
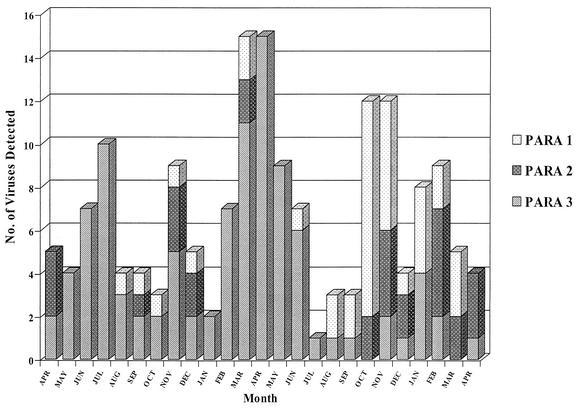
Biennial fall epidemics are the hallmark of HPIV-1 and occur in both hemispheres (38, 232, 259). Reports from the United States have suggested that a minimum of 50% of croup cases are caused by this virus (69, 70, 232). During each HPIV-1 epidemic, an estimated 18,000 to 35,0000 U.S. children younger than 5 years are hospitalized (20, 69, 70, 116, 138, 232, 329, 388). Some of these children have bronchiolitis, tracheobronchitis, pneumonia, and febrile and afebrile wheezing. The majority of infections occur in children aged 7 to 36 months, with a peak incidence in the second and third year of life. HPIV-1 can cause LRI in young infants but is rare in those younger than 1 month. The full burden of HPIV-1 in adults and the elderly has not been determined, but several studies have shown this virus to cause yearly hospitalizations in healthy adults and perhaps play a role in bacterial pneumonias and deaths in nursing home residents (86, 87, 92, 231). HPIV-1, to HPIV-3 have all been found to occur at low levels in most months of the year, similar to RSV and influenza virus (142, 373).
HPIV-2 has been reported to cause infections biennially with HPIV-1 or alternate years with HPIV-1 or to cause yearly outbreaks (20, 75, 259). We see some HPIV-2 activity every year in Milwaukee, Wis. The peak season for this virus is fall to early winter. HPIV-2 causes all of the typical LRI syndromes, but in nonimmunocompromised or chronically ill children croup is the most frequent syndrome brought to medical attention. LRI caused by this virus has been reported much less frequently than with HPIV-1 and HPIV-3. This may be due to difficulties in isolation and detection. As many as 6,000 children younger than 18 years may be hospitalized each year in the United States because of HPIV-2 (Henrickson et al., submitted). About 60% of all HPIV-2 infections occur in children younger than 5 years, and although the peak incidence is between 1 and 2 years of age, significant numbers of infants younger than 1 year are hospitalized each year. HPIV-2 is often overshadowed by HPIV-1 or HPIV-3 infections, yet in any one year or location it can be the most common cause of parainfluenza LRI in young children.
Young infants (younger than 6 months) are particularly vulnerable to infection with HPIV-3. Unlike the other HPIV, 40% of HPIV-3 infections are in the first year of life. Brochiolitis and pneumonia are the most common clinical presentations. Only RSV causes more LRI in neonates and young infants. HPIV-3 has caused outbreaks within neonatal intensive care units, and the natural history of this virus in the neonate is currently being studied (373). Approximately 18,000 infants and children are hospitalized each year in the United States because of LRI caused by HPIV-3. This virus causes yearly spring and summer epidemics in North America and Europe and is somewhat endemic, especially in the immunocompromised and chronically ill. Although the exact reasons for the different seasonality of the HPIV types is unknown, differences in ambient climate conditions have been proposed as one hypothesis (71, 116).
Only a small number of studies have reported on the isolation or epidemiology of HPIV-4 (36, 37, 46, 110, 191). These cases and data are distributed fairly equally between infants younger than 1 year, preschool children, and school age children and adults. Seroprevalence studies have demonstrated that 60 to 84% of infants have significant antibody levels after birth (presumably maternal in origin). These levels drop to 7 to 9% by 7 to 12 months of age and stay low for several years before increasing to about 50% by 3 to 5 years of age. Antibody levels to HPIV-4 continue to rise throughout childhood until approximately 95% of adults have antibody to HPIV-4 A and 75% have antibody to HPIV-4 B (110). Interestingly, the majority of HPIV-4 clinical isolates appear to be subtype B. All of the different respiratory tract syndromes can be caused by HPIV-4. Although hospitalization of infants and young children secondary to HPIV-4 LRI has been reported, serious disease is either rare or difficult to diagnose based on the seroprevelence (216).
Animal PIV have been reported on occasion to infect humans. The majority of evidence to support this hypothesis is serologic, and because of the antigenic relatedness of the respirovirus and rubulavirus genera, it is difficult to substantiate. However, closely related megamyxoviruses (Hendra and Nipah viruses), whose natural host appear to be bats, have recently caused serious epidemics of encephalitis in humans (53, 254, 265). Also, Newcastle disease virus clearly causes human disease and is discussed under “Host range.” Other examples of PIV infecting outside of their usual host range include bovine PIV-3 in humans, HPIV-1 in mice, and mouse PIV-1 (Sendai virus) in African green monkeys (155, 182, 314). These infections are usually asymptomatic.
Clinical Syndromes
HPIV have been associated with every kind of upper and lower respiratory tract illness. However, there is a strong relationship between HPIV-1, HPIV-2, and HPIV-3 and specific clinical syndromes, age of child, and time of year, as described above. Our lack of epidemiologic data on HPIV-4 has so far prevented a clear understanding of the unique clinical niche of this virus.
Croup (acute laryngotracheobronchitis).
Children present with fever, a hoarse barking cough, laryngeal obstruction, and inspiratory stridor. The incidence peaks between 1 and 2 years of age and is more frequent in boys. In Milwaukee, we have found white children to have had a much higher incidence than black children (137). Approximately 10 to 25% of cases of LRI in children younger than 5 years presents as croup (depending on age). The causative agent has been identified in about 50% of croup cases (36 to 74%) (69, 70, 137, 216, 259). HPIV have made up between 56 and 74% of these cases (131), with HPIV-1 (26 to 74%) being the most frequent subtype (69). HPIV-2 and HPIV-3 average around 10% each as etiologic agents. Sampling of a national database (0.5% of total) and community-based estimates have suggested between 27,000 and 66,000 hospitalizations each year in the United States for croup (137, 232; Henrickson et al., submitted). In years when HPIV-1 is not epidemic, HPIV-2 has been found to cause croup outbreaks. Even during HPIV-1-epidemic years, HPIV-2 has been reported to cause >60% of the croup cases in an individual community (232). HPIV-3 has been demonstrated to cause severe croup in an adult (386). RSV, influenza A and B viruses, adenoviruses, rhinoviruses, and, in school age children, Mycoplasma have all been shown to cause croup. A recent retrospective review suggested that influenza virus croup was more severe than parainfluenza virus croup (284).
Bronchiolitis.
The diagnosis of bronchiolitis is unique to pediatrics because of the size of infant's terminal airways. The predominant symptoms include fever, expiratory wheezing, tachypnea, retractions, rales, and air trapping. The peak incidence of bronchiolitis is in the first year of life (81% of cases occur during this period) and then dramatically declines until it virtually disappears by school age. This syndrome is diagnosed in approximately 25 to 30% of LRIs in childhood but makes up a larger percentage in the first year or two of life. At least 90% of cases of bronchiolitis are thought to be viral in origin, and a viral identification rate as high as 83% has been reported (70, 259). Hospitalizations for bronchiolitis have been steadily increasing over the last 20 years in the United States (322). All four types of HPIV can cause bronchiolitis, but HPIV-1 and HPIV-3 have been reported most commonly. Each of these two groups appears to cause 10 to 15% of cases of bronchiolitis in nonhospitalized children. However, in hospitalized children, HPIV-3 causes many more cases than HPIV-1 (three or four times as many) and is second only to RSV as a cause of bronchiolitis and pneumonia in young infants.
Pneumonia.
Pneumonia is classicly diagnosed by the presence of fever and rales and evidence of pulmonary consolidation on physical examination or X ray. Pneumonia is diagnosed in 29 to 38% of children hospitalized with LRI and in 23% treated as outpatients (20, 70, 173, 190, 259). However, since several of these classic LRI syndromes decrease with age, pneumonia causes 83% of hospitalizations of children with LRI older than 5 years. The peak incidence for pneumonia is in the second and third years of life. Recently, at least one-third of pneumonia hospitalizations have been in children with chronic diseases (115; Henrickson et al., submitted). Viruses have been shown to cause up to 90% of these LRI, especially in the first year (66, 70, 156, 205, 262, 270), and this percentage decreases to approximately 50% by school age (70, 173, 205). After 9 to 10 years of age, viruses cause a decreasing but still significant amount of pneumonia in immunocompetent individuals. The percentage of pneumonias with a documented viral etiology eventually declines to about 12% by adulthood (74, 76, 122, 231). HPIV-1 and HPIV-3 each cause about 10% of outpatient pneumonias, but, similar to bronchiolitis, HPIV-3 causes a larger percentage of cases in hospitalized patients. Pneumonia can be caused by both HPIV-2 and HPIV-4, but the incidence of disease is not well described. HPIV-1 infection has been associated with secondary bacterial pneumonias in the elderly (92).
Tracheobronchitis.
Patients with lower respiratory signs and symptoms who do not fit well into the above three syndromes often receive a diagnosis of tracheobronchitis. The most common symptoms include cough and large-airway noise on auscultation (rhonchi), but patients also may have fever and URI. About 20 to 30% of children with LRI receive this diagnosis. The incidence is lower in the first 5 years of life, but tracheobronchitis is fairly evenly diagnosed throughout school age and adolescence. Viral agents make up the majority of etiologies in children (70). More than 25% of the agents identified to cause tracheobronchitis have been HPIVs (HPIV-3 is more common than HPIV-1 or HPIV-2). Several studies have recorded tracheobronchitis as the most common diagnosis in patients with HPIV-4 infections. Also, this diagnosis is used more commonly in patients with chronic diseases (Henrickson et al., submitted).
Any single HPIV can cause more than one of these LRI syndromes to occur simultaneously or progressively in the same child. In 5 to 20% of LRI cases, two viruses can be detected and may be associated with more severe disease (76). HPIV routinely cause otitis media, pharyngitis, conjunctivitis, and coryza (common cold). These URI can occur singly or in any combination with the above-mentioned LRI. Otitis media has been shown to be associated with viral respiratory tract infections in 30 to 60% of cases. Viruses may work synergistically with bacteria to initiate otitis media or prolong symptoms, and occasionally they are found to be the only cause of disease (50). HPIV-3 is the most frequently reported HPIV associated with otitis media (388). HPIV have been found in 1% of middle ear effusions and in 2% of nasopharyngeal secretions in children with acute otitis media (310).
Immunocompromised hosts.
Immunocompromised children and adults appear to be particularly succeptible to developing sever and fatal LRI with HPIV. HPIV-2 has caused giant-cell pneumonia in severe combined immunodeficiency syndrome (SCIDS) (180) and has been found along with HPIV-3 in SCIDS (68, 98, 143, 219, 236) and acute myelomonocytic leukemia (377) and after bone marrow transplantation (BMT) (380). It is common for more than one pathogen to be found in these patients on autopsy, but HPIV alone is found in two-thirds of the cases. Persistent respiratory tract infection and excretion of HPIV-1, HPIV-2, and HPIV-3 have been described in SCIDS (98, 143, 180), with HPIV-3 in a child with DiGeorge syndrome after a thymic transplant (17), and in human immunodeficiency virus-infected children (176, 194, 195). The natural history of HPIV in human immunodeficiency virus-infected children is still largely unknown, but severe disease appears uncommon until they are significantly T-cell deficient (239). HPIV-3 has been associated with acute rejection episodes in renal and liver transplant recipients (67, 146). Solid-organ transplant and BMT patients develop HPIV URI and LRI, including consolidated and interstitial pneumonia (7, 214, 220, 374, 380, 381). HPIV-3 has been the most frequent HPIV type isolated from immunocompromised patients with LRI and is a common cause of fever and neutropenia in children with cancer (9, 224, 266). This virus is persistently shed from BMT patients for up to 4 months without accumulating any mutations (399). Between 5 and 7% of adult BMT and leukemia patients become infected with HPIV-1, HPIV-2, and HPIV-3 (9, 214, 224, 266, 381); approximately 24 to 50% develop pneumonia and 22 to 75% of these will die. A retrospective study found that 41% of pediatric BMT patients with HPIV infection (47% of viral respiratory infections) developed pneumonia and 6% died (224). HPIV has been shown to cause serious LRI and death (8%) in lung transplant recipients up to 5 years after transplantation (367). HPIV-3 has been reported to cause parotitis in children with SCIDS and “common variable” hypogammaglobulinemia (63). Immunocompromised patients have been found to have HPIV infection in other nonrespiratory sites including cerebrospinal fluid (CSF), pericardial fluid, white blood cells, and liver (16), as well as in postmortem cultures of the myocardium and liver (93).
Neurologic disease.
For many decades, PIV have been associated with acute and chronic neurologic disease. Children hospitalized with HPIV have had significant problems with febrile seizures. HPIV-4B appears to have the greatest association (up to 62%), followed by HPIV-3 (17%) and HPIV-1 (7%) (75). HPIV-1 strains were isolated from two patients with multiple sclerosis (213, 242), but evidence of antibody to HPIV-1 in the serum or CSF of MS patients has been lacking (31, 211). One report demonstrated that 2 of 25 CSF samples from MS patients had low positive HI titers to HPIV-1 but 3 of 25 had positive titers to measles virus (12). Similarly, virus cultures and electron microscopy of other MS patients failed to find evidence of HPIV-1. However, HPIV-1 and Sendai virus have been detected using PCR in tissue from the ofactory bulbs of mice (247, 248). Animal PIV related to HPIV-2 have been found in patients with MS and subacute sclerosing panencephalitis (118, 307). Two closely related paramyxoviruses (Hendra and Nipaha viruses) have been shown to cause severe encephalitis and death in children and adults (53, 254, 265). HPIV-3 has been isolated from the CSF of a patient with Guillain-Barré syndrome (309) and adults with demyelinization syndromes (370) and has occasionally been shown to cause meningitis in children (8, 370, 385) and adults (370). HPIV-1, HPIV-2, and HPIV-3 have been isolated from the respiratory tract of children with acute encephalitis (23). In addition, several diseases have been linked to HPIV-3 by serology, including encephalitis, ventriculitis, and cluster headaches in an adult (24, 321). All of these data suggest that some strains of HPIV may have neurotropism in certain hosts. Until more studies are done to clarify the role HPIV plays in human neurologic disease, this possibility will be vastly overshadowed by their significant contribution to respiratory disease.
Other syndromes.
Full-term and premature infants have developed apnea and bradycardia during HPIV infection (235, 241, 321, 328). Two children with adult respiratory distress syndrome were infected with HPIV-1 (157). HPIV-3 has been implicated in supraglottitis and bronchiolitis obliterans (120, 285). HPIV parotitis has been diagnosed in otherwise healthy children infected with HPIV-1 and HPIV-3 (26, 402), in immunocompromised children (381), and in a patient with cystic fibrosis (34). Croup caused by HPIV has been associated with bacterial tracheitis (83, 218). Exacerbations of nephrotic syndrome in children have been linked to viral respiratory infections in general (226). Nonrespiratory tissues are rarely infected with HPIV. However, both immunocompromised patients and children with croup have had documented viremia and disseminated infection (308). Similarly, children and adults with acute non-A, B, C hepatitis have had paramyxovirus-like nucleocapsids found in their liver, giant cells, and syncytia on tissue examination (286). It is possible that HPIV may play a role in this disease. HPIV-3 has been cultured from a 37-year-old man with myopericarditis, and other HPIV types have been diagnosed serologically in patients with myocarditis or peridcarditis (383). Elevated levels of antibodies to HPIV-1 have been reported in patients with systemic lupus erythematosus and Reiter's syndrome (287). However, the differences between the mean antibody titers of the controls and the subjects were only one or two dilutions. Recent work using reverse transcription-PCR (RT-PCR) has demonstrated no evidence of mumps virus P or HN genes in patients with inflammatory bowel disease (168). There does not yet appear to be a clear link established between HPIV and inflammatory or connective tissue disease. There is a relationship between infection with common respiratory pathogens and myalgias and rhabdomyolysis. HPIV-3 has been cultured from a child who died with rhabdomyolysis (359). Also, HPIV-2 has been serologically linked to myalgias and myoglobinuria in an adult (273). HPIV-3 has been cultured from throat and rectal cultures in an adult patient with bloody diarrhea, but other now common gastrointestinal pathogens were not sought (M. D. Aronson, D. Kaminsky, and C. A. Phillips, Letter, Ann. Intern. Med. 81:856-857, 1974). Likewise, respiratory tract symptoms were found in 11% of young children diagnosed with rotavirus gastroenteritis, but the etiology of the respiratory symptoms was not determined (30). No clear role for HPIV in gastroenteritis has been determined.
Nosocomial infections.
Doctors' offices, hospitals, and chronic care facilities are institutions where respiratory viruses are frequently transmitted between patients. The populations at greatest risk for HPIV infection are young preschool children, the immunocompromised, and the elderly (399). Children infected with HPIV-3 will transmit this virus to a minimum of 20% of uninfected control children residing on the same ward (258). About one-third of these will develop mild respiratory symptoms, but some will experience serious LRI and even death (75, 258). Serious sequelae are most common in patients with underlying medical problems. The mean length of hospitalization was increased by many days, even for those with only mild symptoms, because of unnecessary tests and therapies due to their new signs and symptoms. If it is not practical to isolate all children admitted to a particular institution with signs of respiratory infection, then strict handwashing between patients must be enforced and high-risk patients must be cohorted away from these possibly infected patients. In addition, strict rules to limit patient exposure to visitors or staff with respiratory symptoms may help to decrease nosocomial HPIV infections.
Economic burden.
The socioeconomic conditions within a country are the biggest determinants of the ultimate cost of HPIV infection. In undeveloped regions, the cost is in human lives. In the United States, mortality is unusual and the cost of these viruses is seen mostly in health care utilization, hospitalization, lost productivity for parents, and, perhaps, long-term respiratory tract sequelae in children. A parent's lost time both from work and home secondary to HPIV infections has not been quantitated but is considerable. Extrapolations based on hospitalizations a decade ago indicate that the yearly cost of HPIV-1 and HPIV-2 infection could exceed $186 million nationally (138). Another estimate based on a computer generated sampling of a national data base (0.5%) for croup caused by HPIV-1 resulted in an estimate of $30 million per croup epidemic for this subset of disease caused by this one virus (232). Separate and independent extrapolations using more recent data from Children’s Hospital of Wisconsin (CHW) suggest that the yearly cost of hospitalizations for HPIV infections in the United States exceeds $200 million (Henrickson et al., submitted). In addition, this estimate does not take into account URI caused by these viruses, the fact that HPIV-3 causes longer and more costly stays than HPIV-1 or HPIV-2, or the economic burden of infections in adults and immunocompromised patients.
Morbidity and mortality.
Children who were tested years after having croup have demonstrated increased bronchial reactivity (221). Similarly, children with LRI caused by RSV have been shown to have chronic pulmonary abnormalities including decreased gas exchange (128, 187), restrictive lung disease (144, 341), obstructive lung disease, and hyperreactivity (128, 144, 187, 357). Even adults have been reported with long-term lung disease following HPIV LRI (124, 277). These viruses clearly cause acute inflammatory changes directly to airways and also are capable of inducing responses in the immune system (e.g., humoral, cellular cytokine production and interaction with allergens) that lead to acute pulmonary changes (357). The exact role of HPIV or other common respiratory viruses in chronic respiratory illness (e.g., asthma and chronic obstructive pulmonary disease is still being determined. This includes looking at the question of biased selection of susceptible or at-risk individuals (phenotype expression) in long-term follow-up studies. However, persistent changes in lung mechanics and hyperresponsiveness have been demonstrated in animal models of PIV LRI (295, 333), suggesting that HPIV LRI may lead to chronic pulmonary damage in some hosts.
As stated above, mortality induced by HPIV is unusual in developed countries and is seen almost entirely in young infants, the immunocompromised, and the elderly. However, the preschool population in developing countries has considerable risk of HPIV-induced death. Whether by primary viral disease or by facilitating secondary bacterial infections in malnourished children, LRI causes 25 to 30% of the deaths in this age group and HPIV causes at least 10% of the LRI (22).
Mode of Transmission
HPIV transmission has been specifically investigated in only a few studies. Air-sampling experiments have shown that HPIV-1 could be recovered from only 2 of 40 infected children at a distance of 60 cm (238). Therefore, transmission is unlikely to take place by small-particle aerosol spread. Close-contact transmission and surface contamination by RSV takes place by aerosolization of large droplets. Furthermore, contaminated surfaces may then lead to direct self-inoculation (126). It is thought that HPIV is transmitted by similar modalities. HPIV-1, HPIV-2, and HPIV-3 have all been shown to survive for up to 10 h on nonporous surfaces and 4 h on porous surfaces (29). However, HPIV-3 experimentally placed on fingers has been shown to lose more than 90% of its infectivity in the first 10 min and could not be transferred to other fingers (6). Person-to-person spread by direct hand contact appears to be an unlikely means of transmission. However, the amount of virus excreted from an acutely infected child may be more than 10 times greater then that tested (127). HPIV can be efficiently removed from surfaces with most common detergents, disinfectants, or antiseptic agents (29).
Pathogenesis
The pathogenesis of HPIV is still being explored. Respiratory epithelium appears to be the major site of virus binding and subsequent infection. Infection of nervous tissue (olfactory) during intranasal challenge with Sendai virus has been suggested by studies in mice (248). Tissue tropism for HPIVs is known to be directed by the HN protein (see “Structural organization” above). There may be differences between these viruses in where and how they are absorbed and released from respiratory epithelium (polarity) (27). HPIV-3 appears to be absorbed and released more extensively from the apical then the basolateral domains of A549 cells. Viral antigen has been localized to the apical portion of epithelial cells in infected cotton rats (290). Actin and the cytoskeleton have been reported to play roles in transcription, maturation, and the movement of viral glycoproteins to the surface of infected cells. HPIV-3 needs functioning microtubules for efficient release (27). Similarly, HPIV-2 forms filamentous shapes 5 to 15 μm long in polarized epithelial cells, and this formation is dependent on actin (393). HPIV-3 and Sendai virus do not form these shapes. More work needs to be done to better understand these important relationships.
When HPIV infects a cell, the first observable morphologic changes may include focal rounding and increase in size of the cytoplasm and nucleus. HPIV decreases host cell mitotic activity as soon as 24 h after inoculation (204). Other changes that can be observed include single or multilocular cytoplasmic vacuoles, basophilic or eosinophilic inclusions, and the formation of multinucleated giant cells (60, 204). These giant cells (fusion cells) usually occur late in infection and contain between two and seven nuclei. Paramyxoviruses are known to induce apoptosis in tissue culture cells (134). The focal tissue destruction caused by HPIV is usually mild and rapidly repaired and, in many infections, may not even be detectable. Infection in immunocompromised hosts is an exception where giant-cell pneumonia can lead to death. Disease severity has been correlated with HPIV shedding in children (127) but not in adults (352). Species-specific down regulation of mouse smooth muscle receptors have been reported following Sendai virus infection (198). However, virus-induced pathologic features and hyperresponsiveness still occurred in rats even without down regulation. Airway hyperresponsiveness in guinea pigs has been associated with sensory neuropeptide depletion (305).
Persistent infection with active viral replication has been demonstrated both in vitro (tissue culture) and in vivo (human infection) (2, 81, 100, 112, 124, 125, 169, 252, 256, 261). Persistent infections with HPIV do not seem to cause morphologic changes or symptoms (e.g., HPIV-2) (2). However, genetic alterations in HPIV and host cells have been reported (81, 112, 261), as well as decreased numbers of host cell surface sialic acid HN receptors (251). The immune response, or lack thereof, in an infected patient clearly affects the clearance of HPIV and the development of persistent infection (67, 236, 377). It is not known what percentage of HPIV infections lead to persistent infection or how persistence is maintained in human hosts.
Both the HN and F proteins have been shown to be involved with cell membrane fusion, but this appears to be virus (type) specific, with some paramyxoviruses needing only the F protein (162, 251). Furthermore, fusion may demonstrate different kinetics depending on whether it takes place virus to cell or cell to cell (251). Certainly, HPIV host range and virulence are determined in part by the ability of host epithelial cells to enzymatically activate the F protein. Also, the neuraminidase activity of the HN protein may play a role in altering muscarinic receptors, leading to vagus-induced bronchospasm, and can cause HPIV-infected cells to resist infection when challenged with HPIV (viral interference) (103, 104, 154).
The immune mechanisms and pathways involved in local cell injury and tissue damage are largely unknown. HPIV-specific immunoglobulin E (IgE) and histamine may contribute to disease severity in infants (379). During acute infection in guinea pigs, increased numbers of inflammatory cells can be found and airway hyperreactivity and decreased bronchoalveolar cellular superoxide production can be demonstrated (94, 95, 306). Rats with antibody to formalin-inactivated HPIV-3 showed enhanced pulmonary inflammation on challenge. In addition, HPIV-3 induced greater peribronchiolar lymphocyte aggregation and histologic change in one species than in another (290). In closely related hosts, an individual's genetically programmed immunologic response may play an important role in HPIV pathogenesis.
HPIV does not need antibody to directly activate the initial components of complement (366). Complement may interfer with virus-host cell receptor binding. Viral neutralization (in vitro) has been demonstrated by the terminal attack complex of complement directly disrupting the virus membrane. HPIV-1 and other respiratory viruses have been shown to have procoagulant activity that may play a role in cardiovascular disease (368). Also, PIVs have been shown to enhance the appearance of pulmonary edema in hypoxic rats, suggesting that they may be a cause of high-altitude pulmonary edema (39).
Immunology
Host defense against HPIV is mediated largely by humoral immunity to the two surface glycoproteins HN and F (184, 340). Most children are born with neutralizing antibody to all four types of HPIV, but these titers quickly fall during the first 6 months of life. HPIV-3 infects approximately two-thirds of children during their first year of life, causing symptomatic disease in about one-third. Virtually all children by the age of 3-years will demonstrate serologic evidence of infection. Animal studies have shown that antibody to either the HN or the F protein can protect against HPIV-3 challenge but that anti-HN antibodies may play a larger role (340). However, high levels of anti-HN antibody alone do not fully protect infants from LRI (184). Repeated infections are often needed before protection develops. The eventual protection of a child's lower respiratory tract against infection by HPIV-3 may be related to the concomitant increase in the level of anti-F antibody, improved cellular immunity, or both. Antibody-mediated virus neutralization of progeny virus may be more important than antibody reacting with infected host cells (255). The majority of antibody response appears to be IgG1, but 30% of adults have significant rises in IgG3, IgG4, serum IgA, and IgM levels (177). During or shortly after an acute infection with HPIV, most preschool children demonstrate IgM antibody production (361). Immunity to HPIV-1 and HPIV-2 develops later than immunity to HPIV-3, increasing more rapidly during the second and third years of life. It is not until school age that a significant percentage of the general population develops antibody levels to HPIV-4.
Secretory IgA plays an important but not fully defined role in protection against natural infections with HPIV. After natural infection with HPIV, most children and adults develop measurable levels of this antibody (160, 330, 378, 392). This has been shown to be correlated with disease prevention and amelioration in adults (330, 352). However, in infants, secretory IgA levels did not correlate with the ability of nasal secretions to neutralize infection or ameliorate disease (392). Cytotoxic T-lymphocyte responses appear to be important in the clearance of virus from the lower respiratory tract during infections with HPIV-3 (135, 158, 193) and mouse PIV-1 (152, 153, 185). Alpha-beta T cells appear to play a larger role in cell-mediated viral cleance than do gamma-delta or natural killer cells, although all may be involved (73, 152, 228). The human cytotoxic T-lymphocyte response has been shown to be directed to determinants on the HN, P, and NP proteins of HPIV-1 and HPIV-3 (55, 65). However, the viral epitopes important in stimulating this line of defense are still largely unknown. More recently, the cytokines produced by CD4 and CD8 T cells have been found during acute LRI caused by Sendai virus in a mouse model. Interleukin-2 (IL-2), gamma interferon, tumor necrosis factor, IL-6 and IL-10 were all detected in the lungs (245). Similarly, human peripheral blood leukocytes stimulated by Sendai virus have been shown to produce macrophage inflammatory protein 1 alpha, monocyte chemotactic protein 1, tumor necrosis factor alpha, IL-6, and IL-8 (163). Interferon may inhibit HPIV-3 primary transcription (52), and likewise HPIV-3 may inhibit interferon-mediated pathways in T cells, including major histocompatibility complex class II antigen expression (108). Another inflammatory mediator induced by Sendai virus is intercellular cell adhesion molecule 1, which has been shown to be responsible for neutrophil and lymphocyte migration into the lung (334).
One of the many inflammatory mediators produced by HPIV-3-stimulated T-cells is IL-10. This cytokine causes T cells to decrease their proliferation response and helps protect them from virus-mediated apoptosis (327). Children with URI caused by HPIV-3 produce IL-11, which correlates with clinical bronchospasm (84). No long-lasting immunity to URI caused by HPIV ever develops, and infections continue throughout life.
Prevention and Treatment
Field trials of formalin-killed whole HPIV-1, HPIV-2, and HPIV-3 vaccines failed to protect children against natural infection in the late 1960s (48, 105). The majority of children developed antibodies to all three HPIV serotypes, but the levels were considerably lower than those seen following natural infection (105). Additional studies revealed that some of the antibody produced against the inactivated viruses may not have neutralized native virus and that no significant mucosal immunity developed (260). Current approaches to HPIV vaccines include intranasal administration of live attenuated strains, subunit strategies using the HN and F proteins, recombinant bovine/human viruses, and strains engineered using reverse genetics.
HPIV-3 and bovine PIV-3 are antigenically related, and bovine PIV-3 induces resistance in rats and primates to challenge with HPIV-3 (364). In human trials, seropositive adults did not produce significant immune responses to bovine PIV-3, but seronegative volunteers responded quite well to this Jennerian vaccine (54, 62). Vaccine studies of young infants and children have demonstrated the same promising results (182). Further studies evaluating the safety and efficacy of bovine PIV-3 when given as multiple doses and simultaneously with routine childhood immunizations are under way (210). A new approach using recombinant bovine PIV-3 with human F and HN genes and human RSV G and F genes has induced good antibody titers and protection in hamsters and rhesus monkeys (129, 319, 320). Sendai virus is antigenically related to HPIV-1. In another attempt to use the classic Jennerian approach, Sendai virus was tested in primates, in which two doses protected against challenge by HPIV-1 (155).
Antigenically and genetically stable attenuated strains of HPIV-3 have been developed by cold adaption (CA). The stability of these CA vaccine strains is enhanced because of multiple markers of attenuation in tissue culture (19). The initial work with these CA strains showed poor infectivity in older children and adults but protection in weanling hamsters and chimpanzees (54, 61). In addition, evidence of reversion toward the wild type was reported in low-passage strains (54). Higher-passage CA HPIV-3 strains demonstrated immunogenicty and attenuation in younger infants, but symptoms still developed (18). Finally, after further attenuation, a passage of CA HPIV-3 was found that demonstrated good infectivity, immunogenicity, attenuation (no diseases), and stability (78, 183). In addition, CA HPIV-3 appears to be more immunogenic then BPIV-3. CA strains of HPIV-1 and HPIV-2 have also been developed, and initial investigation has demonstrated attenuation in tissue culture and animal models.
Protease activation mutants represent another approach to developing attenuated strains of HPIV. Infection with HPIV requires that the F protein be cleaved by a trypsin-like protease. HPIV strains that are resistant to trypsin cleavage but sensitive to cleavage by another protease may be attenuated in humans (318). Protease activation mutants of Sendai virus have protected mice from lethal challenge infections (230, 349).
The envelope glycoproteins (HN and F) of HPIV-3 have been cleaved from whole virus to create subunit vaccines that have demonstrated efficacy in rats, lambs, mice, and hamsters (4, 246, 300, 303). Many different routes of immunization have been tried, including subcutaneous, intramuscular, and intranasal. No human trials have yet been reported. Subunit vaccines created by cloning HN and F in vaccinia virus and baculovirus vector systems have been used to immunize rats and primates (338, 340, 365). Viral shedding and peak titer were both reduced on subsequent challenge. Reverse genetics are now being used to develop systems able to evaluate current live HPIV-3 vaccines in terms of specific mutations and hopefully introduce specific mutations into wild-type strains in the future (77, 151). An example of this is the production of a recombinant HPIV-3 that contains the HN and F for HPIV-1 and the specific CA mutations found in the L gene of HPIV-3 (348). This vaccine has been found to be protective in hamsters. Sometime over the next decade, one or more of these approaches may produce the first licensed HPIV vaccine.
Agents found to have in vitro antiviral activity against paramyxoviruses include neuraminidase inhibitors (e.g., zanamivir), protein synthesis inhibitors (puromycin), nucleic acid synthesis inhibitors, benzthiazole derivatives, 1,3,4-thiadiazol-2-ylcyanamide, carbocyclic 3-deezaadenosine (Cc3Ado), ascorbic acid, calcium elenolate, and extracts of Sanicula europaea leaves (113, 123, 179, 222, 240, 263, 289, 312, 332, 382, 389-391). None of these compounds or drugs have yet found clinical applications. Potent inhibitors of HPIV syncytium formation in tissue culture have been found by screening hundreds of small synthetic peptides. These peptides, which are to a specific domain on the F protein, may provide a novel approach to the development of antiviral therapies for HPIV (114, 206, 281). Amantadine did not decrease URI disease severity in adult volunteers challenged with HPIV-1 even though it has some anti-HPIV activity at very high concentrations (330). Similarly, ribavirin has both in vitro and in vivo activity against HPIV (32, 326). Furthermore, there have been anecdotal reports of decreased HPIV shedding and clinical improvement when infected immunocompromised patients were treated with aerosolized and oral ribavirin (41, 42, 227, 336). However, a recent review at Fred Hutchinson Cancer center demonstrated that established HPIV-3 pneumonias responded poorly to aerosolized ribavirin (267). Currently there are no antiviral drugs with proven clinical efficacy against HPIV.
There have been several studies demonstrating that nonspecific immunostimulators can protect against challenge infections with paramyxoviruses (e.g., dihydroheptaprenol, N-acetylglucosaminylmuramyl tri- or tetrapeptides, imiquimod, and polyriboinosinic and polyribocytidylic acids) (149, 166, 167, 342). A portion of this protective effect is due to stimulation of endogenous cytokines. Animals have been protected by the direct administration of cytokines (107, 167). Interferon (alpha and gama), human granulocyte colony-stimulating factor, and human IL-1β are a few of the cytokines that have been tested (400). Numerous studies, as summarized in a recent meta-analysis, have demonstrated that oral or systemic steroids are effective at improving symptoms of croup as early as 6 h after treatment (331).
Protection against RSV and other respiratory pathogens has been accomplished by giving high-titer pooled immunoglobulin (56, 325). LRI caused specifically by HPIV may be decreased (40, 288, 350), but little has been reported concerning the use of immunotherapy in HPIV disease. Combined immunotherapy and steroids have been demonstrated to decrease pulmonary virus titer and inflammation in a cotton rat model (291). Immunotherapy may offer a possible theraputic option in patients with severe disease until safe and effective vaccines and antivirals are available.
LABORATORY DIAGNOSIS
Collection and Preparation of Clinical Specimens
The nasopharynx and oropharynx are primary locations of initial HPIV replication. Virus is shed at high titer early in an infection and then sharply declines. Experimental infections in adults have demonstrated that illness usually starts about 3 to 4 days after inoculation and lasts from 3 to 17 days, with an average of 4 days for HPIV-1 and 6 to 13 day for HPIV-2 and HPIV-4 (330, 358). Virus recovery in adults is much more difficult than in children. This is partly due to the several-log-unit increase in viral titer produced by children compared to adults. Children shed virus usually from 3 to 4 days prior to the onset of clinical symptoms until approximately 10 days past (97). However, HPIV-3 has been isolated in children from as early as 6 days before to 6 weeks past the first symptom. Immunocompromised patients and adults (mostly with chronic lung disease) have persistently shed HPIV-1, HPIV-2, and HPIV-3 for many months (124, 257). Throat swabs, nasopharyngeal swabs, nasal washes, and nasal aspiration have all been used successfully to recover HPIV (101, 116, 127, 229, 324). The optimal method of collecting clinical samples for HPIV has not been well studied but depends on the method of detection used (e.g., PCR or tissue culture), the age of the patient, and the general health of the patient (i.e)., immunocompromised or with chronic lung disease). The few studies to yield high rates of viral recovery (HPIV-1 and HPIV-3) used nasal washes or nasal aspirates (127, 384), these methods are therefore recommended even in young infants for optimal virus isolation.
HPIV lose infectivity rapidly when the temperature rises above 4 to 8°C. Specimens (swabs or 2- to 4-ml nasal wash aspirates) should be collected and placed in viral transport medium (2 to 3 ml), either veal infusion broth or minimum essential medium supplemented with some protein source (not serum) such as 0.5% bovine serum albumin. The transport medium should contain antibiotics and antifungal agents to decrease contamination and be buffered to yield a pH of 7.5 to 80 after addition of the clinical sample. Ideally, the specimen in transport medium should be kept at 4°C until tissue culture inoculation. If a delay of more than 24 h is anticipated, the specimen should be frozen. Centrifugation at 1,000 × g prior to inoculation is also helpful in removing debris.
It is rare to have to process nonrespiratory specimens for HPIV. CSF can be directly plated onto tissue culture cells. If it is going to be frozen, transport medium should be added 1:1 prior to freezing. Transport medium with extra antibiotics can be used to dilute stool specimens or for rectal swabs. Standard transport medium can be used to dilute tissue homogenized in a dounce prior to testing.
Serum Samples
The first serum sample (acute phase) should be collected as soon into the person's viral illness as possible. The second serum sample (convalescent phase) should be drawn when the peak antibody production occurs. For neutralizing antibody, this occurs between 3 and 5 weeks after infection. Both samples should have the serum removed as quickly as possible and then be stored at either −70 or −20°C in a non-frost-free freezer. Both the acute- and convalescent-phase samples should be tested at the same time.
Virus Isolation
Tissue culture.
HPIV has the best growth in primary monkey kidney cells. In a telephone survey of clinical virology laboratories, the most popular cell line for growing HPIV was rhesus MK cells. However, this cell line is not always the most sensitive for HPIV, especially for HPIV-2 (96). Cynomolgus and African green monkey cell lines are also used. An easy-to-use secondary cell line (LLC-MK2) is excellent for continued passage and almost as gook as PMK cells for primary isolation. LLC-MK2 cells need trypsin (2 to 3 μg/ml) added to the maintenance medium to recover all HPIV serotypes. Trypsin may be helpful even for PMK cell lines. Both PMK and LLC-MK2 cells may both be required for optimal isolation of HPIV. Most strains of HPIV-4 and even some strains of HPIV-2 and HPIV-3 are detected 10 days or longer after inoculation. PMK cells may start to degenerate between 10 and 14 days, especially if trypsin is in the medium. One method to maximize HPIV recovery is to infect both LLC-MK2 and PMK cell lines and perform initial detection methods (e.g., F and HAd) on the PMK cells. After 10 days, if these tests are negative and further testing of the PMK cells is not possible, the LLC-MK2 cells are in reserve for testing at 2 and 3 weeks.
Isolation in animals.
Eggs are a very poor growth medium for HPIV. It is only after many repeated passages and much presumed antigenic change that HPIV can be detected in embryonated eggs. Only three isolates of HPIV-2 have ever been reported to have undergone primary isolation in eggs (369).
Detection and typing.
CPE is rarely demonstrated during primary isolation of HPIV in tissue culture, and so this is not a reliable or useful method to detect positive cultures. HAd of guinea pig red blood cells directly onto the tissue culture monolayer is the most common method to detect the presence of HPIVs. The respiroviruses are quickly and easily detected using HAd. Most HPIV-1 isolates are detected by day 4 (138), and HPIV-3 takes only a little longer (36, 37, 145). However, the rubulaviruses are much slower. Only 35% of HPIV-2 isolates are HAd positive by day 7 (138), and HPIV-4 may take 3 weeks or longer (36). Interestingly, the neuramindase of HPIV-4 appears to be temperature sensitive because this virus hemadsorbs better at room temperature or 37°C while all of the other serotypes react well at 4°C (37, 110).
IF is the most rapid and accurate method currently available to detect and type HPIV in tissue culture (109, 344, 372). HPIV isolates are detected much faster using this technique than using to HAd, and IF detects positive cultures that never develop HAd. This is especially true for HPIV-2 (138). In addition, further typing of HPIV is unnecessary when IF detection is used. This can save time and money. Tissue culture isolation of HPIV is being done less and less. However, high-risk populations may continue to have a need for this method. A typical testing plan (all year round) would be as follows. IF detection is performed on all inoculated PMK tissue culture cells on days 2 or 3, 4 or 5, and 10 and on MK2 cells on days 14 and 21. A MAb pool reagent could be used such that only a single test had to be done per culture (344). Also, the addition of centrifugation (e.g., shell vial) to the above IF schedule may speed HPIV detection by 1 day or more (296). If desired, HAd could be performed first and then IF could be performed only on those that were positive. It is important to remember that primary screening with HAd will miss some HPIV. Other useful methods of detecting and typing HPIV in tissue culture include HAdI, HI, complement fixation, and neutralization (36, 45, 136). These methods are currently more useful for research purposes since they are time-consuming and costly compared to IF (except HI). On primary isolation, most strains of HPIV do not release enough free virus into the medium to react in the HI assay, limiting the usefulness of this relatively easy assay in clinical virology. Until commercial MAb IF reagents became widely available, HAdI was the method of choice for HPIV serotype identification. This meant that each identification took an additional 3 to 5 days after the culture was identified as positive (37). Although tissue culture is the current “gold standard,” the new molecular assays like PCR are rapidly replacing this time-honored method in clinical virology.
Serologic Diagnosis
There are many methods to detect antibodies to HPIV, including ELISA, radioimmunoassays, HI, complement fixation, western blotting, and neutralization assays. The development of heterologous antibody to closely related HPIV serogroups during any HPIV infection is a persistent problem in trying to make a serological diagnosis of acute HPIV (44, 45). This problem is greatest when trying to separate HPIV-1 infection from HPIV-3 infection, but mumps virus antibody also cross-reacts with these two viruses (99, 178, 212, 371). A large number of children's sera that test positive by ELISA and HI to HPIV-3 will have similar titers to HPIV-1 (K. J. Henrickson, unpublished data). Although the least sensitive of the serologic assays, complement fixation has the smallest number of problems with heterologous cross-reactivity (178). On the other hand, ELISA is by far the most sensitive assay and detects the largest number of titer rises in patients with respiratory illness but is the least specific and detects many dual HPIV antibody titers. HPIV-2 demonstrates the least amount of serologic cross-reactivity (178, 371).
A fourfold rise or drop in titer is generally thought to signify acute infection if the testing is performed at the same time on paired acute- and convalescent-phase serum samples. A positive serologic rise in titer to any of the HPIV types (even if without heterologous antibody demonstrated) only indicates infection with HPIV (47). It should not be used to determine the HPIV serotype. Only virus isolation and typing with MAbs (or molecular identification) can accurately establish the specific serotype.
Direct Examination for Viruses
Electron microscopy can easily demonstrate HPIV (Fig. 1). However, many paramyxoviruses appear the same (e.g., mumps virus). No large study looking at the diagnostic utility of electron microscopy for HPIV infection has been published (72, 175), and less expensive methods of diagnosis have been developed.
Methods to detect HPIV antigen using ELISA, radioimmunoassay, and fluoroimmunoassays have all been developed (147, 148, 315, 317), but none of these are available commercially in the United States. Investigators using these methods have reported sensitivities between 75 and 95% (polyclonal sera), with the MAb-FIA demonstrating slightly higher detection of HPIV-1 and HPIV-2 (94-100%) (147). Most clinical virology laboratories will find these methods difficult to perform until reagents are widely available.
For more than two decades, HPIV has been detected by IF (25, 90, 106, 109, 121, 130, 229, 294, 299, 344, 372, 384). Originally these techniques involved the production of serotype-specific antisera in various animal species by each individual laboratory and subsequent conjugation to fluorescein isothiocyanate. Now most laboratories use of commercially produced MAbs (single or pooled). The detection of HPIV by direct IF staining of clinical material has yielded highly variable and sometimes disappointing results. The best results have been demonstrated for HPIV-3, with most studies reporting sensitivities between 50 and 75% (range, 31 to 100%). In studies that used only commercially available MAbs the sensitivities range between 31 to 93% of culture-positive specimens. Studies detecting HPIV-1 showed sensitivities ranging between 0 and 92%, and those detecting HPIV-2 showed sensitivity ranging between 50 and 100%, with most sensitivities falling between 50 and 83%. Differences in specimen type, collection, processing, reagents (antibody), and testing procedures help explain the reported variability in sensitivities. However, specificity appears to be uniformly excellent. The use of IF to detect HPIV-3 has demonstrated a rate for IF-positive/culture-negative specimens as high as 16%. It is not known whether these are all false positives or positive specimens without viable virus. Results presented by Leland using MAbs for direct detection of HPIV demonstrated a sensitivity of 80% (HPIV-1), 83% (HPIV-2), and 72% (HPIV-3) compared to tissue culture. This same HPIV antigen detection using IF was also shown to have a 4% false-positive rate (D. S. Leland, Abstr. 13th Annu. Clin. Virol. Symp., p. 13-15, 1997). New combined (dual fluorescence) reagents are available, but their sensitivity and specificity do not seem to be significantly different. A recent study using these reagents reported 95% sensitivity for HPIV-1, HPIV-2, and HPIV-3 compared to tissue culture, but a significant number of samples (126 samples; 12% of those that were compared to culture) were deemed inadequate, and thus the true sensitivity is significantly lower than this. The false-positive rate was approximately 5% (208).
The shell vial assay is another method for the rapid identification of HPIV. In this assay, tissue culture is grown on slides and then centrifugation is used initially to speed viral absorption and cell infection. Detected is performed by standard IF of the tissue culture cells, typically at 48 h and 5 days. Although variable results have been reported, the majority of data appear to demonstrate improved detection using this method (164). Influenza virus and RSV are the two viruses most widely studied by this method. Detection of HPIV has been compared using shell vials and standard tissue culture, with sensitivities averaging 84%, but most of the viruses tested were HPIV-3 (276, 296; C. C. Maurer, Abstr. 9th Annu. Clin. Virol. Symp., abstr. M11, 1993).
A new shell vial technique using a mixture of two cell lines, mink lung cells, and A549 cells (R-mix; Diagnostic Hybrids, Athens, Ohio) has been compared to standard tissue culture and rapid antigen tests for detecting community-acquired respiratory viruses but including very few HPIV-positive samples (13; S. Castriciano et al., Abstr. T-17, 18th Annu. Clin. Virol. Symp., abstr. 2002; R. Chua et al., Abstr. 18th Annu. Clin. Virol. Symp. abstr. T-18, 2002; M. Kampert et al., Abstr. 18th Annu. Clin. Virol. Symp., abstr. T-20, 2002; J. Langer et al., Abstr. 18th Annu. Clin. Virol. Symp., abstr. T-21, 2002; R. J. Mitchell et. al., Abstr. 18th Annu. Clin. Virol. Symp., abstr. T-22, 2002; Ostermann et al., Abstr. 18th Annu. Clin. Virol. Symp. abstr. T-23, 2002; J. Dunn et al., Abstr. 18th Annu. Clin. Virol. Symp., abstr. T-24, 2002). Little has been published, but data from the abstracts demonstrated mixed results when the R-Mix cells were stained at 2 or 5 days. Some investigators have shown decreased sensitivity compared to direct IF or tissue culture. The largest study demonstrated a sensitivity for HPIV of 77% (23 of 30 samples) compared to standard tissue culture (J. Dunn et al., Abstr. 18th Annu. Clin. Virol. Symp., Abstr. T-24, 2002).
Standard IF detection is done visually using a fluorescent microscope with appropriate mirrors and filters for fluorescein isothiocyanate. Fluorescence can also be detected using flow cytometry analysis. This automated process analyzes the fluorescent antibody binding to cell surfaces and reports this binding quantitatively. The minimum number of cells needed (2,000 cells), the lengths of time, and the cost make this technique more useful in a research setting.
Genomic Detection
HPIV RNA can be detected directly by performing a Northern hybridization or a dot blot analysis using virus specific DNA probes. This takes many hours to complete, yields less uniform results, and, even with sensitive detection methods, appears to be most useful as a research tool. The amount of HPIV RNA in many clinical samples is not great enough to allow detection without either biological (tissue culture) or molecular amplification. After conversion of RNA into DNA, PCR can be used easily and efficiently to detect small numbers of virus in different fluids. Several studies demonstrating PCR to be sensitive and specific in detecting HPIV have been published (82, 85, 89, 102, 181). A multiplex RT-PCR assay for detecting HPIV-1, HPIV-2, and HPIV-3 was developed in 1995 (89). Currently, there is one commercial multiplex PCR assay available for detecting HPIV-1, HPIV-2, and HPIV-3, along with RSV A, RSV B, influenza A virus, and influenza B virus. This RT-PCR-EHA (Hexaplex; Prodesse, Waukesha, Wis.) has a reported sensitivity of 95 to 100% and a specificity of 97 to 100% compared to tissue culture and yields results in about 7 h (Fig. 2) (14, 33, 88, 142, 150, 189, 217, 395, 397). Real-time PCR methods have been developed for HPIV-1, HPIV-2, and HPIV-3 (Henrickson, unpublished), and reagents for multiplex real-time PCR are available commercially. Recently, protocols for the duplex detection of HPIV-1 and HPIV-3 have been developed for isothermic amplification using nucleic acid sequence-based amplification (J. D. Fox, S. Hibbitts, A. Rahman, R. John, and D. Westmoreland, Abstr. 18th Annu. Clin. Virol. Symp., abstr. T26, 2002). However, to use these protocols, HPIV primers and probes have to be designed by each laboratory, and royalties may have to be paid to the patent holders (Prodesse).
FIG. 2.
HPIV-1, HPIV-2, and HPIV-3 detected by multiplex RT-PCR-EHA (Hexaplex; Prodesse, Inc.) at Children's Hospital of Wisconsin during 2000 to 2002.
REFERENCES
- 1.Afshar, A. 1969. The occurrence of antibodies to parainfluenza 3 virus in sera of farm animals and man in Iran. Br. Vet. J. 125:529-533. [DOI] [PubMed] [Google Scholar]
- 2.Ah-Tye, C., S. Schwartz, K. Huberman, E. Carlin, and A. Moscona. 1999. Virus-receptor interactions of human parainfluenza viruses types 1, 2, and 3. Microb. Pathog. 27:329-336. [DOI] [PubMed] [Google Scholar]
- 3.Alexander, D. J., R. J. Manvell, M. S. Collins, S. J. Brockman, H. A. Westbury, I. Morgan, and F. J. Austin. 1989. Characterization of paramyxoviruses isolated from penguins in Antarctica and sub-Antarctica during 1976-1979. Arch. Virol. 109:135-143. [DOI] [PubMed] [Google Scholar]
- 4.Ambrose, M. W., P. R. Wyde, M. Ewasyshyn, A. M. Bonneau, B. Caplan, H. L. Meyer, and M. Klein. 1991. Evaluation of the immunogenicity and protective efficacy of a candidate parainfluenza virus type 3 subunit vaccine in cotton rats. Vaccine 9:505-511. [DOI] [PubMed] [Google Scholar]
- 5.Andrewes, C. H., F. B. Bang, and F. M. Burnet. 1955. A short description of the myxovirus group (Influenza and related viruses). Virology 1:176-184. [DOI] [PubMed] [Google Scholar]
- 6.Ansari, S. A., V. S. Springthorpe, S. A. Sattar, S. Rivard, and M. Rahman. 1991. Potential role of hands in the spread of respiratory viral infections: studies with human parainfluenza virus 3 and rhinovirus 14. J. Clin. Microbiol. 29:2115-2119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Apalsch, A. M., M. Green, and E. R. Wald. 1995. Influenza and parainfluenza virus infections in pediatric organ transplant recipients. Clin. Infect. Dis. 20:394-399. [DOI] [PubMed] [Google Scholar]
- 8.Arguedas, A., H. R. Stutman, and J. G. Blanding. 1990. Parainfluenza type 3 meningitis. Report of two cases and review of the literature. Clin. Pediatr. 29:175-178. [DOI] [PubMed] [Google Scholar]
- 9.Arola, M., O. Ruuskanen, T. Ziegler, and T. T. Salmi. 1995. Respiratory virus infections during anticancer treatment in children. Pediatr. Infect. Dis. J. 14:690-694. [DOI] [PubMed] [Google Scholar]
- 10.Reference deleted.
- 11.Bando, H., M. Kawano, K. Kondo, M. Tsurudome, H. Komada, M. Nishio, and Y. Ito. 1991. Growth properties and F protein cleavage site sequences of naturally occurring human parainfluenza type 2 viruses. Virology 184:87-92. [DOI] [PubMed] [Google Scholar]
- 12.Barbosa, L. H., and R. Hamilton. 1973. Virological studies with multiple-sclerosis brain tissues. Lancet i:1415-1417. [DOI] [PubMed] [Google Scholar]
- 13.Barenfanger, J., C. Drake, T. Mueller, T. Troutt, J. O'Brien, and K. Guttman. 2001. R-mix cells are faster, at least as sensitive, and marginally more costly than conventional cell lines for the detection of respiratory viruses. J. Clin. Virol. 22:101-110. [DOI] [PubMed] [Google Scholar]
- 14.Barenfranger, J., C. Drake, N. Leon, T. Mueller, and T. Troutt. 2000. Clinical and financial benefits of rapid detection of respiratory viruses: an outcomes study. J. Clin. Microbiol. 38:2824-2828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Baumqartner, W., S. Krakowka, and J. R. Gorham. 1989. Canine parainfluenza virus-induced encephalitis in ferrets. J. Comp. Pathol. 100:67-76. [DOI] [PubMed] [Google Scholar]
- 16.Baxter, B. O., R. B. Couch, S. B. Greenberg, and J. A. Kasel. 1977. Maintenance of viability and comparison of identification methods for influenza and other respiratory viruses of humans. J. Clin. Microbiol. 6:19-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Beard, L. J., E. F. Robertson, and Y. H. Thong. 1980. Parainfluenza pneumonia in DiGeorge syndrome two years after thymic epithelial transplantation. Acta Paediatr. Scand. 69:403-406. [DOI] [PubMed] [Google Scholar]
- 18.Belshe, R. B., R. A. Karron, F. K. Newman, E. L. Anderson, S. L. Nugent, M. Steinhoff, M. L. Clements, M. H. Wilson, E. L. Hall, and E. L. Tierney. 1992. Evaluation of a live attenuated, cold-adapted parainfluerza virus type 3 in children. J. Clin. Microbiol. 30:2064-2070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Belshe, R. B., and F. K. Hissom. 1982. Cold adaptation of parainfluenza virus type 3: induction of three phenotypic markers. J. Med. Virol. 10:235-242. [DOI] [PubMed] [Google Scholar]
- 20.Belshe, R. B., L. P. Van Voris, and M. A. Mufson. 1983. Impact of viral respiratory diseases on infants and young children in a rural an urban area of southern West Virginia. Am. J. Epidemiol. 117:467-474. [DOI] [PubMed] [Google Scholar]
- 21.Ben-Ishai, Z., V. Naftali, A. Avram, and S. Yatziv. 1980. Human infection by a bovine strain of parainfluenza virus type 3. J. Med. Virol. 6:165-168. [DOI] [PubMed] [Google Scholar]
- 22.Berman, S. 1991. Epidemiology of acute respiratory infections in children of deveioning counties. Rev. Infect. Dis. 13:S454-S462. [DOI] [PubMed] [Google Scholar]
- 23.Bitnun, A., E. L. Ford-Jones, M. Petric, D. MacGregor, H. Heurter, S. Nelson, G. Johnson, and S. Richardson. 2001. Acute childhood encephalitis and Mycoplasma pneumoniae. Clin. Infect. Dis. 32:1674-1684. [DOI] [PubMed] [Google Scholar]
- 24.Blanchard, B. M. 1998. Cluster headache associated with parainfluenza virus, preceded and succeeded by migraine. Headache 38:132-134. [DOI] [PubMed] [Google Scholar]
- 25.Blanding, J. G., M. G. Hoshiko, and H. R. Stutrnan. 1989. Routine viral culture for pediatric respiratory specimens submitted for direct immunofluorescence testing. J. Clin. Microbiol. 27:1438.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bloom, H. H., K. J. Johnson, R. Jacobsen, and R. M. Chanock. 1961. Recovery of parainfluenza viruses from adults with upper respiratory illness. Am. J. Hyg. 74:50-59. [Google Scholar]
- 27.Bose, S., A. Malur, and A. K. Banerjee. 2001. Polarity of human parainfluenza virus type 3 infection in polarized human lung epithelial A549 cells: role of microfilament and microtubule. J. Virol. 75:1984-1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Box, P. G., I. G. Furminger, and W. W. Robertson. 1974. Immunizing turkeys against Newcastle disease with oil emulsion killed vaccine. Vet. Rec. 95:371-372. [DOI] [PubMed] [Google Scholar]
- 29.Brady, M. T., J. Evans, and J. Cuartas. 1990. Survival and disinfection of parainfluenza viruses on environmental surfaces. Am. J. Infect. Control 18:18-23. [DOI] [PubMed] [Google Scholar]
- 30.Brandt, C. D., H. W. Kim, W. J. Rodriguez, J. O. Arrobio, B. C. Jeffries, and R. H. Parrott. 1986. Simultaneous infections with different enteric and respiratory tract viruses. J. Clin. Microbiol. 23:177-179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Brown, P., F. Cathala, and D. C. Gajdusek. 1973. Further studies of viral antibodies in the cerebrospinal fluid of patients with multiple sclerosis: vaccinia and parainfluenza type 1 (37422). Proc. Soc. Exp. Biol. Med. 143:828-829. [DOI] [PubMed] [Google Scholar]
- 32.Browne, M. J. 1981. Comparative inhibition of influenza and parainfluenza virus replication by ribavirin cells. Antimicrob. Agents Chemother. 19:712-715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Buckingham, S. C., H. S. Jafri, A. J. Bush, C. M. Carubelli, P. Sheeran, R. D. Hardy, M. G. Ottolini, O. Ramilo, and J. P. DeVincenzo. 2002. A randomized double-blind, placebo-controlled trial of dexamethasone in severe respiratory syncytial virus (RSV) infection: effects on RSV quantity and clinical outcome. J. Infect. Dis. 185:1222-1228. [DOI] [PubMed] [Google Scholar]
- 34.Buckley, J. M., P. Poche, and K. McIntosh. 1972. Parotitis and parainfluenza 3 virus. Am. J. Dis. Child. 124:789.. [DOI] [PubMed] [Google Scholar]
- 35.Buckner, C. K., V. Songsiridej, E. C. Dick, and W. W. Busse. 1985. In vivo and in vitro studies on the use of the guinea pig as a model for virus-provoked airway hyperreactivity. Am. Rev. Respir. Dis. 132:305-310. [DOI] [PubMed] [Google Scholar]
- 36.Canchola, J., A. J. Vargosko, and H. W. Kim. 1964. Antigenic variation among newly isolated strains of parainfluenza type 4 virus. Am. J. Hyg. 79:357-364. [DOI] [PubMed] [Google Scholar]
- 37.Canchola, J. G., R. M. Chanock, B. C. Jeffries, E. E. Christmas, H. W. Kim, A. J. Vargosko, and R. H. Parrott. 1965. Recovery and identification of human myxoviruses. Bacteriol. Rev. 29:496-503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Carballal, G., C. M. Videla, A. Espinosa, V. Savy, O. Uez, M. D. Sequera, V. Knez, P. V. Requeijo, C. R. Posse, and I. Miceli. 2001. Multicentered study of viral acute lower respiratory infections in children from four cities of Argentina, 1993- 1994. J. Med. Virol. 64:167-174. [DOI] [PubMed] [Google Scholar]
- 39.Carpenter, T. C., J. T. Reeves, and A. G. Durmowicz. 1998. Viral respiratory infection increases susceptibility of young rats to hypoxia-induced pulmonary edema. J. Appl. Physiol. 84:1048-1054. [DOI] [PubMed] [Google Scholar]
- 40.Carthew, P., J. Riley, and O. Dinsdale. 1989. Amelioration of established Sendai viral pneumonia in the nude mouse using a monoclonal antibody to the virus fusion protein. Br. J. Exp. Pathol. 70:727-735. [PMC free article] [PubMed] [Google Scholar]
- 41.Chakrabarti, S., K. E. Collingham, K. Holder, C. D. Fegan, H. Osman, and D. W. Milligan. 2001. Pre-emptive oral ribavirin therapy of paramyxovirus infections after haematopoietic stem cell transplantation: a pilot study. Bone Marrow Transplant. 28:759-763. [DOI] [PubMed] [Google Scholar]
- 42.Chakrabarti, S., K. E. Collingham, K. Holder, S. Oyaide, D. Pillay, and D. W. Milligan. 2000. Parainfluenza virus type 3 infections in hematopoetic stem cell transplant recipients: response to ribavirin therapy. Clin. Infect. Dis. 31:1516-1518. [DOI] [PubMed] [Google Scholar]
- 43.Chanock, R. M., and K. McIntosh. 1985. Parainfluenza viruses, p. 1241. In B. N. Fields (ed.), Virology. Raven Press, New York, N.Y.
- 44.Chanock, R. M., R. H. Parrott, J. A. Bell, W. P. Rowe, and R. J. Huebner. 1958. New viruses observed in children with respiratory diseases. Public Health Rep. 73:193-195. [PMC free article] [PubMed] [Google Scholar]
- 45.Chanock, R. M., R. H. Parrott, K. M. Cook, B. E. Andrews, J. E. Bell, T. Reichelerfer, A. K. Kapikian, F. M. Mastrota, and R. J. Huebner. 1958. Newly recognized myxoviruses from children with respiratory disease. N. Engl. J. Med. 258:207-213. [DOI] [PubMed] [Google Scholar]
- 46.Chanock, R. M., and R. H. Parrott. 1965. Acute respiratory disease in infancy and childhood: present understanding and prospects for prevention. E. Mead Johnson Address, October, 1964. Pediatrics 6:21-39. [PubMed] [Google Scholar]
- 47.Chanock, R. M. 1979. Parainfluenza viruses, p. 611-633. In E. H. Lennette (ed.), Diagnostic procedures for viral, rickettsial and chlamydial infections. American Public Health Association, Washington, D.C.
- 48.Chin, J., R. L. Magoffin, L. A. Shearer, J. H. Schieble, and E. H. Lennette. 1969. Field evaluation of a respiratory syncytial virus vaccine and a trivalent parainfluenza virus vaccine in a pediatric population. Am. J. Epidemiol. 89:449-463. [DOI] [PubMed] [Google Scholar]
- 49.Chonmaitree, T., and K. J. Henrickson. 2000. Detection of respiratory viruses in the middle ear fluids of children with acute otitis media by multiple reverse transcription: polymerase chain reaction assay. Pediatr. Infect. Dis. J. 19:258-260. [DOI] [PubMed] [Google Scholar]
- 50.Chonmaitree, T., M. J. Owen, and V. M. Howie. 1990. Respiratory viruses interfere with bacteriologic response to antibiotic in children with acute otitis media. J. Infect. Dis. 162:546-549. [DOI] [PubMed] [Google Scholar]
- 51.Choppin, P. W., C. D. Richardson, C. D. Merz, W. W. Hall, and A. Scheid. 1981. The functions and inhibition of the membrane glycoproteins of paramyxoviruses and myxoviruses and the role of the measles virus L protein in subacute schlerosing panencphalitis. J. Infect. Dis. 143:352-362. [DOI] [PubMed] [Google Scholar]
- 52.Choudhary, S., B. P. De, and A. K. Banerjee. 2000. Specific phosphorylated forms of glyceraldehydes 3-phosphate dehydrogenase associated with human parainfluenza virus type 3 and inhibit viral transcription in vitro. J. Virol. 74:3634-3641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Choudhary, S., J. Gao, D. W. Leaman, and B. P. De. 2001. Interferon action against human parainfluenza virus type 3: involvement of a novel antiviral pathway in the inhibition of transcription. J. Virol. 75:4823-4831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Clements, M. L., R. B. Belshe, J. King, F. Newman, T. U. Westblom, and E. L. Tierney. 1991. Evaluation of bovine, cold-adapted human and wild-type human parinfluenza type 3 viruses in adult volunteers and in chimpanzees. J. Clin. Microbiol. 29:1175-1182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Cole, G. A., J. M. Katz, T. L. Hogg, K. W. Ryan, A. Portner, and D. L. Woodland. 1994. Analysis of the primary T-cell response to Sendai virus infection in C57BL/6 mice CD4+ T-cell recognition is directed predominantly to the hemagglutinin-neuraminidase glycoprotein. J. Virol. 68:6863-6870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Connor, E., and the PREVENT Study Group. 1997. Reduction of RSV hospitalization among premature infants and infants with bronchopulmonary dysplasia using respiratory syncytial virus immune globulin prophylaxis. Pediatrics 99:93-99. [DOI] [PubMed] [Google Scholar]
- 57.Coronel, E. C., T. Takimoto, G. Murti, N. Varich, and A. Portner. 2001. Nucleocapsid incorporation into parainfluenza virus is regulated by specific interaction with matrix protein. J. Virol. 75:1117-1123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Covalciuc, K. A., K. H. Webb, and C. A. Carlson. 1999. Comparison of four clinical specimen types for detection of influenza A and B viruses by optical immunoassay (FLU OIA Test) and cell culture methods. J. Clin. Microbiol. 37:3971-3974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Cowley, J. A., and R. D. Barry. 1983. Characterization of human parainfluenza viruses. I. The structural proteins of influenza and parainfluenza viruses involving adsorption to erythrocytes. J. Gen. Virol. 64:2117-2125. [DOI] [PubMed] [Google Scholar]
- 60.Craighead, J. E., and B. J. Brennan. 1968. Cytopathic effects of parainfluenza virus type 3 in organ cultures of human respiratory tract tissue. Am. J. Pathol. 52:287-300. [PMC free article] [PubMed] [Google Scholar]
- 61.Crookshanks-Newman, F. K., and R. B. Belshe. 1986. Protection of weanling hamsters from experimental infection with wild-type parainfluenza virus type 3 (para 3) by cold adapted mutants of para 3. J. Med. Virol. 18:131-137. [DOI] [PubMed] [Google Scholar]
- 62.Crowe, J. E. 1995. Current approaches to the development of vaccines against disease caused by respiratory syncytial virus (RSV) and parainfluenza virus (PIV). Vaccine 13:415-421. [DOI] [PubMed] [Google Scholar]
- 63.Cullen, S. J., and J. V. Baublis. 1980. Parainfluenza type 3 parotitis in two immunodeficient children. J. Pediatr. 96:437-438. [DOI] [PubMed] [Google Scholar]
- 64.Curran, J. 1998. A role for the Sendai virus P protein trimer in RNA synthesis. J Virol. 72:4274-4280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Dave, V., J. E. Allan, K. S. Slobod, F. S. Smith, K. W. Ryan, T. Takimoto, U. F. Power, A. Portner, and J. L. Hurwitz. 1994. Viral cross-reactivity and antigenic determinants recognized by human parainfluenza virus type 1-specific cytotoxic T-cells. Virology 199:376-383. [DOI] [PubMed] [Google Scholar]
- 66.Davies, H. D., E. E. Wang, D. Manson, P. Babyn, and B. Shuckett. 1996. Reliability of the chest radiograph in the diagnosis of lower respiratory infections in young children. Pediatr. Infect. Dis. J. 15:600-604. [DOI] [PubMed] [Google Scholar]
- 67.DeFabritus, A. M., R. R. Riggio, O. S. Oavid, L. B. Senterfit, J. S. Cheigh, and K. H. Stenzel. 1979. Parainfluenza type 3 in a transplant unit. JAMA 241:384-386. [PubMed] [Google Scholar]
- 68.Delage, G., P. Brochu, M. Pelletier, G. Jasmin, and N. Lapointe. 1979. Giant-cell pneumonia caused by parainfluenza. J. Pediatr. 94:426-429. [DOI] [PubMed] [Google Scholar]
- 69.Denny, F. H., T. F. Murphy, W. A. Clyde, Jr, A. M. Collier, and F. W. Henderson. 1983. Croup: an 11-year study in a pediatric practice. Pediatrics 71:871-876. [PubMed] [Google Scholar]
- 70.Denny, F. W., and W. A. Clyde, Jr. 1986. Acute lower respiratory infections in nonhospitalized children. J. Pediatr. 108:635-646. [DOI] [PubMed] [Google Scholar]
- 71.de Silva, L. H., and M. J. Cloonan. 1991. Brief report: parainfluenza virus type 3 infections: findings in Sydney and some observations on variations in seasonality world-wide. J. Med. Virol. 35:19-21. [DOI] [PubMed]
- 72.Doane, F. W., N. Anderson, K. Chatiyanonda, R. M. Bannatyne, D. M. McLean, and A. J. Ghodes. 1967. Rapid laboratory diagnosis of paramyxovirus infections by electron microscopy. Lancet ii:751-753. [Google Scholar]
- 73.Doherty, P. C., W. Allan, M. Eichelberger, S. Hou, K. Bottomly, and S. Carding. 1991. Involvement of gamma delta T Cells in respiratory virus infections. Curr. Top. Microbiol. Immunol. 173:291-296. [PubMed] [Google Scholar]
- 74.Dowell, S. F., L. J. Anderson, H. E. Gary, D. D. Erdman, J. F. Plouffe, T. M. File, B. J. Marston, and R. F. Breiman. 1996. Respiratory syncytial virus is an important cause of community-acquired lower respiratory infection among hospitalized adults. J. Infect. Dis. 174:456-462. [DOI] [PubMed] [Google Scholar]
- 75.Downham, M. A., J. McDuillin, and P. S. Gardner. 1974. Diagnosis and clinical significance of parainfluenza virus infections in children. Arch. Dis. Child. 49:8-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Drews, A. L., B. L. Atmar, W. P. Glezen, B. D. Baxter, P. A. Piedra, and S. B. Greenberg. 1997. Dual respiratory virus infections. Clin. Infect. Dis. 25:1421-1429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Durbin, A., J. W. Slew, B. R. Murphy, and P. L. Collins. 1997. Minimum protein requirements for transcription and RNA replication of a minigenome of human parainfluenza virus type 3 and evaluation of the rule of six. Virology 234:74-83. [DOI] [PubMed] [Google Scholar]
- 78.Durbin, A. P., J. Cho, W. R. Elkins, L. S. Wyatt, B. Moss, and B. R. Murphy. 1999. Comparison of the immunogenicity and efficacy of a replication-defective vaccinia virus expressing antigens of human parainfluenza virus type 3 (HPIV3) with those of a live attenuated HPIV3 vaccine candidate in rhesus monkeys passively immunized with PIV3 antibodies. J. Infect. Dis. 179:1345-1351. [DOI] [PubMed] [Google Scholar]
- 79.Durbin, A. P., J. M. McAuliffe, P. L. Collins, and B. R. Murphy. 1999. Mutations in the C, D, and V open reading frames of human parainfluenza virus type 3 attenuate replication in rodents and primates. Virology 261:319-330. [DOI] [PubMed] [Google Scholar]
- 80.Ebata, S. N., M. J. Cote, C. Y. Yang, and K. Dimock. 1991. The fusion and hemagglutinin-neuraminidase glycoproteins or human parainfluenza virus 3 are both required for fusion. Virology 183:437-441. [DOI] [PubMed] [Google Scholar]
- 81.Ebina, T., I. Kamo, M. Homma, and N. Ishida. 1969. Autoradiographic studies of HeLa-S3 cells persistently infected with hemadsorption type 2 virus. Exp. Cell. Res. 57:359-364. [DOI] [PubMed] [Google Scholar]
- 82.Echevarria, J. E., D. D. Erdman, H. C. Meissner, and L. Anderson. 2000. Rapid molecular epidemiologic studies of human parainfluenza viruses based on detect sequencing of amplified DNA from a multiplex RT-PCR assay. J. Virol. Methods 88:105-109. [DOI] [PubMed] [Google Scholar]
- 83.Edwards, K., C. Dundon, and W. A. Altemeier. 1983. Bacterial tracheitis as a complication of viral croup. Pediatr. Infect. Dis. J. 2:390-391. [DOI] [PubMed] [Google Scholar]
- 84.Einarson, C., G. P. Geba, Z. Zhu, M. Landry, and J. A. Alias. 1996. Interleukin-11: stimulation in vivo and in vitro by respiratory viruses and induction of airways hyperresponsiveness. J. Clin. Investig. 97:915-924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Eugene-Ruellan, G., F. Freymuth, C. Bahloul, H. Badrane, A. Vabret, and N. Tordo. 1998. Detection of respiratory syncytial virus A and B and parainfluenza 3 sequences in respiratory tracts of infants by a single PCR with primers targeted to the L-polymerase gene and differntial hybridization. J. Clin. Microbiol. 36:796-801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Falsey, A. R., C. K. Cunningham, W. H. Barker, R. W. Kouides, J. B. Yuen, M. Menegus, L. B. Weiner, C. A. Bonville, and R. F. Betts. 1995. Respiratory syncytial virus and influenza A infections in the hospitalized elderly. J. Infect. Dis. 172:389-394. [DOI] [PubMed] [Google Scholar]
- 87.Falsey, A. R. 1991. Noninfluenza respiratory infection in long-term care facilities. Infect. Control Hosp. Epidemiol. 12:602-608. [DOI] [PubMed] [Google Scholar]
- 88.Fan, J., K. J. Henrickson, and L. L. Savatski. 1998. Rapid simultaneous diagnosis of infections with respiratory syncytial viruses A and B, influenza viruses A and B, and human parainfluenza virus types 1, 2, and 3 by multiplex quantitative reverse transcription-polymerase chain reaction-enzyme hybridization assay (Hexaplex). Clin. Infect. Dis. 26:1397-1402. [DOI] [PubMed] [Google Scholar]
- 89.Fan, J., and K. J. Henrickson. 1996. Rapid diagnosis of human parainfluenza virus type I infection by quantitative reverse transcription-PCR-enzyme hybridization assay. J. Clin. Microbiol. 34:1914-1917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Fedova, D. O., I. Pecenkova-Plachtova, B. Tumova, and M. Bruckova. 1971. Application of the fluorescent antibody method in the diagnosis of M. parainfluenzae. 3. Isolation and identification of M. parainfluenzae on monkey kidney tissue cultures and in nasal and nasopharyngeal swabs. J. Hyg. Epidmiol. Microbiol. Immunol. 15:82-92. [PubMed] [Google Scholar]
- 91.Fenner, F., P. A. Bachmann, E. P. J. Gibbs, A. Murphy, M. J. Studdert, and D. O. White. 1987. In F. Fenner (ed.), Veterinary virology. Academic Press, Inc., Orlando, Fla.
- 92.Fiore, A. E., C. Iverson, T. Messmer, D. Erdman, S. M. Lett, D. F. Talkington, L. J. Anderson, B. Fields, G. M. Carlone, R. F. Breiman, and M. S. Cetron. 1998. Outbreak of pneumonia in a long-term care facility: antecedent human parainfluenza virus 1 infection may predispose to bacterial pneumonia. J. Am. Geriatr. Soc. 46:1112-1117. [DOI] [PubMed] [Google Scholar]
- 93.Fishaut, M., O. Tubergen, and K. Mcintosh. 1989. Cellular response to respiratory viruses with particular reference to children with disorders of cell-mediated immunity. J. Pediatr. 96:179-186. [DOI] [PubMed] [Google Scholar]
- 94.Folkerts, G., M. Janssen, and F. P. Nijkamp. 1990. Parainfluenza-3 induced hyperreactivity of the guinea pig trachea coincides with an increased number of bronchoalveolar cells. Br. J. Clin. Pharmacol. 30:159S-161S. [DOI] [PMC free article] [PubMed]
- 95.Folkerts, G., B. van Esch, M. Janssen, and F. P. Nijkamp. 1990. Superoxide production by broncho-alveolar cells is diminished in parainfluenza-3 virus treated guinea pigs. Agents Actions Suppl. 1 31:139-142. [DOI] [PubMed] [Google Scholar]
- 96.Frank, A. L., R. B. Couch, C. A. Griffin, and B. D. Baxter. 1973. Comparison of different tissue cultures for isolation and quantitation of influenza and parainfluenza viruses. J. Clin. Microbiol. 10:2-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Frank, A. L., L. H. Taber, C. R. Wells, J. M. Wells, W. P. Glezen, and A. Pareues. 1981. Patterns of shedding myxoviruses and paramyxoviruses in children. J. Infect. Dis. 144:433-441. [DOI] [PubMed] [Google Scholar]
- 98.Frank, J. A., Jr., R. W. Warren, J. A. Tucker, J. Zeller, and C. M. Wilfert. 1983. Disseminated parainfluenza infection in a child with severe combined immunodeficiency. Am. J. Dis. Child. 137:1172-1174. [DOI] [PubMed] [Google Scholar]
- 99.Frankova, V., J. Holubova, L. Grubhoffer, and U. Kasova. 1988. Contribution to laboratory diagnosis of mumps and parainfluenza. Acta Virol. 32:503-514. [PubMed] [Google Scholar]
- 100.Fraser, K. B., and J. Anderson. 1966. Persistent non-cytocidal infection of BHK 21 cells by human parainfluenza type 2 virus. J. Gen. Microbiol. 44:47-58. [DOI] [PubMed] [Google Scholar]
- 101.Frayha, J., S. Castriciano, J. Mahony, and M. Chenesky. 1989. Nasopharyogeal swabs and nasopharyngeal aspirates equally effective for the diagnosis of viral respiratory disease in hospitalized children. J. Clin. Microbiol. 27:1387-1389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Freymuth, F., A. Vabret, F. Galateau-Salle, J. Ferey, E. G. Petitjean, E. Gennetay, J. Brouard, M. Jokik, J. F. Duhamel, and B. Guillois. 1997. Detection of respiratory syncytial virus, parainfluenzavirus 3, adenovirus and rhinovirus sequences in respiratory tract of infants by polymerase chain reaction and hybridization. Clin. Diagn. Virol. 8:31-40. [DOI] [PubMed] [Google Scholar]
- 103.Fryer, A. D., E. E. el-Fakahany, and O. B. Jacoby. 1990. Parainfluenza virus type 1 reduces the affinity of agonists for muscarinic receptors in guinea pig lung and heart. Eur. J. Pharmacol. 181:51-58. [DOI] [PubMed] [Google Scholar]
- 104.Fryer, A. D., and O. B. Jacoby. 1991. Parainfluenza virus infection damages inhibitory Mz muscarinic receptors on pulmonary parasympathetic nerves in the guinea-pig. B. J. Pharmacol. 102:267-271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Fulginiti, V. A., J. J. Eller, O. F. Sieber, J. W. Joyner, M. Minamitani, and G. Meiklejohn. 1969. Respiratory virus immunization. 1. A field trial of two inactivated respiratory virus vaccines; an aqueus trivalent parainfluenza virus vaccine and an alum-precipitated respiratory syncytial virus vaccine. Am. J. Epidemiol. 89:435-448. [DOI] [PubMed] [Google Scholar]
- 106.Fulton, R. E., and P. J. Middleton. 1974. Comparison of immunofluorescence and isolation techniques in the diagnosis of respiratory viral infections in children. Infect. Immun. 10:92-101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Fulton, R. N., L. J. Burge, and F. S. McCraken. 1986. Effect of recombitant DNA-derived bovine and human interferons on replication of bovine herpesvirus-1, parainfluenza-3, and respiratory syncytial virus. Am. J. Vet. Res. 47:751-753. [PubMed] [Google Scholar]
- 108.Gao, J., B. P. De, Y. Han, S. Choudhary, R. Ransohoff, and A. K. Banerjee. 2001. Human parainfluenza virus type 3 inhibits gamma interferon induced major histocompatibility complex class II expression directly and by inducing alpha/beta interferon. J. Virol. 75:1124-1131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Gardner, P. S., J. McQuillin, R. McGuckin, and R. K. Ditchburn. 1971. Observations on clinical and immunofluorescent diagnosis of parainfluenza virus infections. Br. Med. J. 2:7-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Gardner, S. D. 1969. The isolation of parainfluenza 4 subtypes A and B in England and serological studies of their prevalence. J. Hyg. 67:545-550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Garten, W., S. Hallenberger, D. Ortmann, W. Schafer, M. Vey, H. Angliker, E. Shaw, and H. D. Klenk. 1994. Processing of viral glycoproteins by the subtilisin-like endoprotease furin and its inhibition by specific peptidylchloroalkylketones. Biochemistry 76:217-225. [DOI] [PubMed] [Google Scholar]
- 112.Genest, P., and P. Daniel. 1966. Genomic modifications in cell line cultures chronically infected with a myxovirus. Proc. Soc. Exp. Biol. Med. 123:722-725. [DOI] [PubMed] [Google Scholar]
- 113.Gergely, L., F. D. Toth, and G. Y. Hadhazy. 1968. Examination in vitro of the virus inhibitory action of a new benzthiazole derivative. Acta Microbiol. Acad. Sci. Hung. 15:145-150. [PubMed] [Google Scholar]
- 114.Ghosh, J. K., and Y. Shae. 1998. A peptide derived from a conserved domain of sendai virus fusion protein inhibits virus-cell fusion. J. Biol. Chem. 273:7252-7259. [DOI] [PubMed] [Google Scholar]
- 115.Glezen, W. P., S. B. Greenberg, R. L. Atmar, P. A. Piedra, and R. B. Cough. 2000. Impact of respiratory virus infections on persons with chronic underlying conditions. JAMA 283:499-505. [DOI] [PubMed] [Google Scholar]
- 116.Glezen, W. P., A. L. Frank, L. H. Taber, and J. A. Kasel. 1984. Parainfluenza virus type 3: seasonality and risk of infection and reinfection in young children. J. Infect. Dis. 150:851-857. [DOI] [PubMed] [Google Scholar]
- 117.Glezen, W. P., F. A. Loda, H. A. Clyde, Jr., R. J. Senior, C. I. Sheaffer, W. G. Conley, and F. W. Denny. 1971. Epidemiologic patterns of acute lower respiratory disease of children in a pediatric group practice. J. Pediatr. 78:397-406. [DOI] [PubMed] [Google Scholar]
- 118.Goswami, K. K., K. R. Cameron, W. C. Russell, L. S. Lange, and D. M. I. Mitchell. 1984. Evidence for the persistence of paramyxoviruses in human bone marrows. J. Gen. Virol. 65:81-88. [DOI] [PubMed] [Google Scholar]
- 119.Gotoh, B., T. Komatsu, K. Takeuchi, and J. Yokoo. 2001. Paramyxovirus accessory proteins as interferon antagonists. Microbiol. Immunol. 45:787-800. [DOI] [PubMed] [Google Scholar]
- 120.Grattan-Smith, T., M. Forer, H. Kilham, and J. Gillis. 1987. Viral supraglottitis. J. Pediatr. 110:434-435. [DOI] [PubMed] [Google Scholar]
- 121.Grauballe, P. C., I. J. Johnsen, and A. Hornsleth. 1974. Rapid diagnosis by immunofluorescence of viral infections associated with the croup syndrome in children. Acta Pathol. Microbiol. Scand. Ser. B 82:41-47. [DOI] [PubMed] [Google Scholar]
- 122.Greenberg, S. B. 1991. Viral pneumonia. Infect. Dis. Clin. North Am. 5:603-621. [PubMed] [Google Scholar]
- 123.Greengard, O., P. Poltoratskaia, E. Leikina, J. Zimmerberg, and A. Moscona. 2000. The anti-influenza virus agent 4-GU-DANA (Zanamivir) inhibits cell fusion mediated by human parainfluenza virus and influenza virus HA. J. Virol. 74:11108-11114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Gross, P. A., R. H. Green, and M. G. Curnen. 1973. Persistent infection with parainfluenza type 3 virus in man. Am. Rev. Respir. Dis. 108:894-898. [DOI] [PubMed] [Google Scholar]
- 125.Gross, P. A., R. H. Green, E. Lerner, and M. G. Cumen. 1974. Immune response in persistent infection. Further studies on persistent respiratory infection in man with parainfluenza type 3 virus. Am. Rev. Respir. Dis. 110:676-681. [DOI] [PubMed] [Google Scholar]
- 126.Hall, C. B., and R. G. Douglas, Jr. 1981. Modes of transmission of respiratory syncytial virus. J. Pediatr. 99:100-103. [DOI] [PubMed] [Google Scholar]
- 127.Hall, C. B., J. M. Geiman, B. B. Breese, and R. G. Douglas, Jr. 1977. Parainfluenza viral infections in children: correlation of shedding with clinical manifestations. J. Pediatr. 91:194-198. [DOI] [PubMed] [Google Scholar]
- 128.Hall, C. B., W. J. Hall, C. L. Gala, F. B. MaGill, and J. P. Leddy. 1984. Long-term prospective study in children after respiratory syncytial virus infection. J. Pediatr. 105:358-364. [DOI] [PubMed] [Google Scholar]
- 129.Haller, A. A., T. Miller, M. Mitiku, and K. Coelingh. 2000. Expression of the surface glycoproteins of human parainfluenza virus type 3 by bovine parainfluenza virus type 3, a novel attenuated virus vaccine vector. J. Virol. 74:11626-11635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Hallsworth, P. G., and P. J. McDonald. 1985. Rapid diagnosis of viral infections with fluorescent antisera. Pathology 17:629-632. [DOI] [PubMed] [Google Scholar]
- 131.Hambling, M. H. 1964. Survival of the respiratory syncytial virus during storage under various conditions. Br. J. Exp. Pathol. 45:647-655. [PMC free article] [PubMed] [Google Scholar]
- 132.Hamparian, V. V., M. R. Hilleman, and A. Ketler. 1963. Contributions to characterization and classification of animal viruses. Proc. Soc. Exp. Biol. Med. 112:1040-1050. [DOI] [PubMed] [Google Scholar]
- 133.Hawthorne, J. D., D. Lorenz, and P. Albrecht. 1982. Infection of marmosets with parainfluenza virus types 1 and 3. Infect. Immun. 37:1037-1041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.He, B., G. Y. Lin, J. E. Durbin, R. K. Durbin, and R. A. Lamb. 2001. The SH integral membrane protein of the paramyxovirus simian virus 5 is required to block apoptosis in MDBK cells. J. Virol. 75:4068-4079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Henderson, F. W. 1979. Pulmonary cell-mediated cytotoxicity in hamsters with parainfluenza virus type 3 pneumonia. Am. Rev. Respir. Dis. 120:41-47. [DOI] [PubMed] [Google Scholar]
- 136.Henrickson, K. J., and L. L. Savatski. 1996. Two distinct human parainfluenza virus type one genotypes detected during the 1991 epidemic. J. Clin. Microbiol. 34:695-700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Henrickson, K. J., S. M. Kuhn, and L. L. Savatski. 1994. Epidemiology and cost of human parainfluenza virus type one and two infections in young children. Clin. Infect. Dis. 18:770-779. [DOI] [PubMed] [Google Scholar]
- 138.Henrickson, K. J., S. M. Kuhn, L. L. Savatski, and J. Sedmak. 1994. Recovery of human parainfluenza virus types one and two. J. Virol. Methods 46:189-206. [DOI] [PubMed] [Google Scholar]
- 139.Henrickson, K. J., and L. Savatski. 1992. Genetic variation and evolution of human parainfluenza virus type 1 hemagglutinin neuraminidase: analysis of 12 clinical isolates. J. Infect. Dis. 166:995-1005. [DOI] [PubMed] [Google Scholar]
- 140.Henrickson, K. J., and L. L. Savatski. 1997. Antigenic structure, function, and evolution of the hemagglutinin-neuraminidase protein of human parainfluenza virus type 1. J. Infect. Dis. 176:867-875. [DOI] [PubMed] [Google Scholar]
- 141.Henrickson, K. J. 1994. Lower respiratory viral infections in immunocompetent children. Adv. Pediatr. Infect. Dis. 9:59-96. [PubMed] [Google Scholar]
- 142.Henrickson, K. J. 1998. Viral pneumonia in children. Semin. Pediatr. Infect. Dis. 9:227-233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Henrickson, K. J. 1991. Monoclonal antibodies to human parainfluenza virus type 1 detect major antigenic changes in clinical isolates. J. Infect. Dis. 164:1128-1134. [DOI] [PubMed] [Google Scholar]
- 143a.Henrickson, K. J. 1999. Human parainfluenza viruses, p. 665-702. In E. H. Lennette (ed.), Laboratory diagnosis of viral infections, Marcel Dekker, Inc., New York, N.Y.
- 144.Henry, R. L., I. G. Hodqes, A. O. Milner, and G. M. Stokes. 1983. Respiratory problems 2 years after acute bronchiolitis in infancy. Arch. Dis. Child. 58:713-716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Herrmann, E. C., and K. A. Hable. 1970. Experiences in laboratory diagnosis of parainfluenza viruses in routine medical practice. Mayo. Clin. Proc. 45:177-188. [PubMed] [Google Scholar]
- 146.Herzog, K. D., S. P. Ounn, M. R. Langham, Jr., and L. M. Marmon. 1989. Association of parainfluenza virus type 3 infection with allograft rejection in a liver transplant recipient. Pediatr. Infect. Dis. J. 8:534-536. [PubMed] [Google Scholar]
- 147.Hierholzer, J. C., P. G. Binglam, R. A. Coombs, K. H. Johansson, L. J. Anderson, and P. K. Haionen. 1989. Comparison of monoclonal antibody time-resolved fluoroimmunoassay with monoclonal antibody capture-biotinylated detector enzyme immunoassay for respiratory syncytial virus and parainfluenza virus antigen detection. J. Clin. Microbiol. 27:1243-1249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Hietala, J., M. Uhari, and H. Tuokko. 1988. Antigen detection in the diagnosis of viral infections. Scand. J. Infect. Dis. 20:595-599. [DOI] [PubMed] [Google Scholar]
- 149.Hill, D. A., S. Baron, and R. M. Chanock. 1969. Sensitivity of common respiratory viruses to an interferon inducer in human cells. Lancet ii:187-188. [DOI] [PubMed] [Google Scholar]
- 150.Hindiyeh, M., D. Hillyard, and K. Carroll. 2001. Evaluation of the Prodesse Hexaplex multiplex PCR assay for direct detection of seven respiratory viruses in clinical specimens. Am. J. Clin. Pathol. 116:218-224. [DOI] [PubMed] [Google Scholar]
- 151.Hoffman, M. A., and A. K. Banerjee. 1997. An infectious clone of human parainfluenza virus type 3. J. Virol. 71:4272-4277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Hogan, R. J., E. J. Usherwood, W. Zhong, A. D. Roberts, R. W. Dutton, A. G. Harmsen, and D. L. Woodland. 2001. Activated antigen-specific CD8+ T cells persist in the lungs following recovery from respiratory virus infections. J. Immunol. 166:1813-1822. [DOI] [PubMed] [Google Scholar]
- 153.Hogan, R. J., W. Zhong, E. J. Usherwood, T. Cookenham, A. D. Roberts, and D. L. Woodland. 2001. Protection from respiratory virus infections can be mediated by antigen-specific CD4+ T cells that persist in the lungs. J. Exp. Med. 193:981-986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Horga, M. A., G. L. Gusella, O. Greengard, N. Poltaratskaia, M. Porotto, and A. Moscona. 2000. Mechanism of interference mediated by human parainfluenza virus type 3 infection. J. Virol. 74:11792-11799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Horowitz, J. L., K. F. Soike, M. Y. Sangster, A. Portner, R. E. Sealy, D. H. Dawson, and C. Coleclough. 1997. Intranasal sendai virus vaccine protects African green monkeys from infection with human parainfluenza virus-type one. Vaccine 15:533-540. [DOI] [PubMed] [Google Scholar]
- 156.Hortal, M., A. Suarez, C. Deleon, M. Estevan, M. C. Mogdasy, J. C. Russi, M. Contera, and M. Meny. 1994. Etiology and severity of community acquired pneumonia in children from Uruguay: A 4 year study. Rev. Inst. Med. Trop. Sao Paulo 36:255-264. [DOI] [PubMed] [Google Scholar]
- 157.Hotez, P. J., B. Goldstein, J. Ziegler, S. A. Doveikis, and M. S. Pasternack. 1990. Adult respiratory distress syndrome associated with parainfluenza virus type I in children. Pediatr. Infect. Dis. J. 9:750-752. [DOI] [PubMed] [Google Scholar]
- 158.Hou, S., P. C. Doherty, M. Zijlstra, and J. M. Katz. 1992. Delayed clearance of Sendai virus in mice lacking class I MHC-restricted CD8+ T cells. J. Immunol. 149:1319-1325. [PubMed] [Google Scholar]
- 159.Howe, C., C. Morgan, C. de Vaux St. Cyr, K. C. Hsu, and H. M. Rose. 1967. Morphogenesis of type 2 parainfluenza virus examined by light and electron microscopy. J. Virol. 1:215-237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Hruskova, J., D. Fedova, L. Syrucek, A. Penningerova, L. Holanova, and V. Berkovicova. 1978. Haemaggiutination inhibition antibodies in nasal secretions of persons after natural parainfluenza virus infection. Acta Virol. 22:203-208. [PubMed] [Google Scholar]
- 161.Hsiung, G. D. 1972. Parainfluenza-5 virus. Infection of man and animal. Prog. Med. Virol. 14:241-274. [PubMed] [Google Scholar]
- 162.Hu, X. L., R. Ray, and R. W. Compans. 1992. Functional interactions between the fusion protein and hemagglutinin-neuraminidase of human parainfluenza viruses. J. Virol. 66:1528-1534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Hua, J., M. J. Liao, and A. Rashidbaigi. 1996. Cytokines induced by Sendai virus in human peripheral blood leukocytes. J. Leukoc. Biol. 60:125-128. [DOI] [PubMed] [Google Scholar]
- 164.Hughes, J. H. 1993. Physical and chemical methods for enhancing rapid detection of viruses and other agents. Clin. Mirobiol. Rev. 6:150-175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Hurrell, J. M. 1967. Methods of storing viruses at low temperatures with particular reference to the Myxovirus group. J. Med. Lab. Technol. 24:30-41. [PubMed] [Google Scholar]
- 166.Iida, J., C. Ishihara, M. MizuLoshi, K. Kitoh, K. Tsukidate, K. Katsu, T. Toyosawa, and I. Azumal. 1990. Prophylactic activity of dihydrohepatrenol, a synthetic polyprenol derivative, against Sendai virus infection in mice. Vaccine 8:376-380. [DOI] [PubMed] [Google Scholar]
- 167.Iida, J., I. Saiki, C. Ishihara, and I. Azuma. 1989. Prophylactic activity against Sendai virus infection and macrophage activation with lipophilic derivatives of H-acetylglucosaminylmuramyl tri- or tetrapeptides. Vaccine 7:225-228. [DOI] [PubMed] [Google Scholar]
- 168.Iizuka, M., H. Saito, M. Yukawa, H. Itou, T. Shirasaka, M. Chiba, F. Fukushima, and S. Watanabe. 2001. No evidence of persistent mumps virus infetction in inflammatory bowel disease. Gut 48:637-641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Iwata, H., M. Tagaya, K. Matsumoto, T. Miyadai, T. Yokochi, and Y. Kimura. 1990. Aerosol vaccination with a sendai virus temperature-sensitive mutant (HVJ-pB) derived from persistently infected cells. J. Infect. Dis. 162:402-407. [DOI] [PubMed] [Google Scholar]
- 170.Jambou, R. C., N. Elango, S. Venkatesan, and P. L. Collins. 1986. Complete sequence of the major nucleocapsid protein gene of human parainfluenza type 3 virus: comparison with other negative strand viruses. J. Gen. Virol. 67:2543-2548. [DOI] [PubMed] [Google Scholar]
- 171.Jambou, R. C., N. Elango, and S. Venkatesan. 1985. Proteins associated with human parainfluenza virus type 3. J. Virol. 56:298-302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Jarvis, W. R., P. J. Middleton, and C. W. Gelfand. 1979. Parainfluenza pneumonia in severe combined immunodeficiency. J. Pediatr. 94:423-425. [DOI] [PubMed] [Google Scholar]
- 173.Jennings, L. C., K. P. Dawson, G. O. Abbott, and J. Allan. 1985. Acute respiratory tract infections of children in hospital: a viral and mycoplasma pneumoniae profile. N. Z. Med. J. 98:582-585. [PubMed] [Google Scholar]
- 174.Johnson, D. P., and R. H. Green. 1973. Viremia during parainfluenza type 3 virus infection of hamsters. Proc. Soc. Exp. Biol. Med. 144:745-748. [DOI] [PubMed] [Google Scholar]
- 175.Joncas, J., L. Berthiaume, and V. Pavilanis. 1969. The structure of the respiratory syncytial virus. Virology 38:493-496. [DOI] [PubMed] [Google Scholar]
- 176.Josephs, S., H. W. Kim, C. D. Brandt, and R. H. Parrott. 1988. Parainfluenza 3 virus and other common respiratory pathogens in children with human immunodeficiency virus infection. Pediatr. Infect. Dis. J. 7:207-209. [PubMed] [Google Scholar]
- 177.Julkunen, I., T. Hovi, I. Seppala, and O. Makela. 1985. Immunoglobulin G subclass antibody responses in influenza A and parainfluenza type 1 virus infection. Clin. Exp. Immunol. 60:130-138. [PMC free article] [PubMed] [Google Scholar]
- 178.Julkunen, I. 1984. Serological diagnosis of parainfluenza virus infections by enzyme immunoassay with special emphasis on purity of viral antigens. J. Med. Virol. 14:177-187. [DOI] [PubMed] [Google Scholar]
- 179.Karagoz, A., N. Arda, N. Goren, K. Nagata, and A. Kuru. 1999. Antiviral activity of Sanicula europaea L. extracts on multiplication of human parainfluenza virus type 2. Phytother. Res. 13:436-438. [DOI] [PubMed] [Google Scholar]
- 180.Karp, O., J. Willis, and C. M. Wilfert. 1974. Parainfluenza virus II and the immunocompromised host. Am. J. Dis. Child. 127:592-593. [DOI] [PubMed] [Google Scholar]
- 181.Karron, R. A., J. L. Froehlich, L. Bobo, R. B. Belshe, and R. H. Yolken. 1994. Rapid detection of parainfluenza virus type 3 RNA in respiratory specimens: use of reverse transcription-PCR-enzyme immunoassay. J. Clin. Microbiol. 32:484-488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Karron, R. A., M. Makhene, and K. Gay. 1996. Evaluation of a live attenuated bovine parainfluenza type 3 vaccine in two-to-six-month old infants. Pediatr. Infect. Dis. J. 15:650-654. [DOI] [PubMed] [Google Scholar]
- 183.Karron, R. A., P. F. Wright, and F. K. Newman. 1995. A live human parainfluenza type 3 virus vaccine is attenuated and immunogenic in healthy infants and children. J. Infect. Dis. 172:1445-1450. [DOI] [PubMed] [Google Scholar]
- 184.Kasel, J. A., A. L. Frank, W. A. Keitel, L. H. Taber, and W. P. Glezen. 1984. Acquisition of serum anribodies to specific viral glycoproteins of parainfluenza virus 3 in children. J. Virol. 52:828-832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Kast, W. M., J. A. Bluestone, M. H. Heemskerk, J. Spaargaren, A. C. Voordouw, J. D. Ellenhort, and C. J. Melief. 1990. Treatment with monoclonal anti-CD3 antibody protects against lethal Sendai virus infection by induction of natural killer cells. J. Immunol. 145:2254-2259. [PubMed] [Google Scholar]
- 186.Kast, W. M., A. H. Bronihorst, P. DeWaal, and C. J. Melief. 1986. Cooperation between cytotoxic and helper T lymphocytes in protection against lethal Sendai virus infection. Protection by T cells is MHC restricted and MHC regulated: a model for MHC-disease associations. J. Exp. Med. 164:723.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Kattan, M., T. G. Keens, J. G. Lapierre, H. Levison, A. C. Bryan, and B. J. Reilly. 1977. Pulmonary function abnormalities in symptom-free children after bronchiolitis. Pediatrics 59:683-688. [PubMed] [Google Scholar]
- 188.Kawano, M., M. Kaito, Y. Kozuka, H. Komada, N. Noda, K. Nanba, M. Tsurudome, M. Ito, M. Nishio, and Y. Ito. 2001. Recovery of infectious human parainfluenza type 2 virus from cDNA clones and properties of the defective virus without V-specific cysteine-rich domain. Virology 284:99-112. [DOI] [PubMed] [Google Scholar]
- 189.Kehl, S. C., and K. J. Henrickson. 2001. Evaluation of the Hexaplex assay for detection of respiratory viruses in children. J. Clin. Microbiol. 39:1696-1701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Kellner, G., T. Popow-Kraupp, M. Kundi, C. Binder, H. Wallner, and C. Kunz. 1988. Contribution of rhinoviruses to respiratory viral infections in childhood. A prospective study in a mainly hospitalized infant population. J. Med. Virol. 25:455-469. [DOI] [PubMed] [Google Scholar]
- 191.Kiligore, G. E., and W. R. Dowdle. 1970. Antigenic characterization of parainfluenza 4A and 4B by the hemagglutination-inhibition test and distribution of HI antibody in human sera. Am. J. Epidemiol. 91:308-316. [DOI] [PubMed]
- 192.Kim, M. R., H. R. Lee, and G. M. Lee. 2000. Epidemiology of acute viral respiratory tract infections in Korean children. J. Infect. 41:152-158. [DOI] [PubMed] [Google Scholar]
- 193.Kimmel, K. A., P. R. Wyde, and W. P. Glezen. 1982. Evidence of a T-cell-mediated cytotoxic response to parainfluenza virus type 3 pneumonia in hamsters. J. Reticuloendothel. Soc. 31:71-83. [PubMed] [Google Scholar]
- 194.King, J. C., A. R. Burke, J. D. Clemens, P. Nair, J. J. Farley, P. E. Vink, S. R. Batlas, M. Rao, and J. P. Johnson. 1993. Respiratory syncytial virus illnesses in human immunodeficiency virus and noninfected children. Pediatr. Infect. Dis. J. 12:733-739. [DOI] [PubMed] [Google Scholar]
- 195.King, J. C. Community respiratory viruses in individuals with human immunodeficiency virus infection. Am. J. Med. 102(3A):19-24. [DOI] [PMC free article] [PubMed]
- 196.Kingsbury, D. W. 1985. Orthomyxo- and Paramyxoviruses and their replication, p. 157. In B. N. Fields (ed.), Virology. Raven Press, New York, N.Y.
- 197.Kingsbury, D. W. 1977. Paramyxoviruses, p. 349-382. In D. P. Nayak (ed.), The molecular biology of animal viruses. Marcel Decker, Inc., New York, N.Y.
- 198.Knott, P. G., P. J. Henry, A. S. McWilliam, P. J. Rigby, L. B. Fernandes, and R. G. Goldie. 1996. Influence of parainfluenza-1 respiratory tract viral infection on endothelin receptor-effector systems in mouse and rat tracheal smooth muscle. Br. J. Pharmacol. 119:291-298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Kolakofsky, D., T. Pelet, D. Garcin, S. Hausmann, J. Curran, and L. Roux. 1998. Paramyxovirus RNA synthesis and the requirement for hexamer genome length: the rule of six revisted. J. Virol. 72:891-899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Komada, H., S. Kusagawa, C. Orvell, M. Tsurudome, M. Nishio, H. Bando, M. Kawano, H. Matsumura, E. Norrby, and Y. Ito. 1992. Antigenic diversity of human parainfluenza virus type 1 isolates and their immunoloigcal relationship with Sendai virus revealed by monoclonal antibodies. J. Gen. Virol. 73:875-884. [DOI] [PubMed] [Google Scholar]
- 201.Komada, H., I. Orstavik, Y. Ito, and E. Nornby. 1990. Strain variation in parainfluenza virus type 4. J. Gen. Virol. 71:1581-1583. [DOI] [PubMed] [Google Scholar]
- 202.Komada, H., M. Tsurudome, H. Bando, M. Nishio, M. Ueda, H. Tsumura, and Y. Ito. 1989. Immunological response of Monkeys infected intranasally with human parainfluenza virus type 4. J. Gen. Virol. 70:3487-3492. [DOI] [PubMed] [Google Scholar]
- 203.Komada, H., M. Tsurudome, M. Ueda, H. Nishio, H. Bando, and Y. Ito. 1989. Isolation and characterization of monoclonal antibodies to human parainfluenza virus type 4 and their use in revealing antigenic relation between subtypes 1A and 4B. Virology 171:28-37. [DOI] [PubMed] [Google Scholar]
- 204.Konovalova, N. G., V. N. Blyumkin, and L. Y. Zakstelskaya. 1967. Action of parainfluenza viruses on the mitotic activity of primary trysinized human embryo kidney cell cultures. Acta Virol. 11:564.. [PubMed] [Google Scholar]
- 205.Korppi, M., P. Halonen, M. Kleemola, and K. Launiala. 1986. Viral findings in children under the age of two years with expiratory difficulties. Acta Paediatr. Scand. 75:457-464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Lambert, D. M., S. Barney, A. L. Lambert, et al. 1996. Peptides from conserved regions of paramyxovirus fusion (F) proteins are potent inhibitors of viral fusion. Proc. Natl. Acad. Sci. USA 93:2186-2191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Lamy, M. E., F. Pouthier-Simon, and E. Debacker-Williame. 1973. Respiratory viral infections in hospital patients with chronic bronchitis. Chest 63:336-341. [DOI] [PubMed] [Google Scholar]
- 208.Landry, M. L., and D. Ferguson. 2000. SimulFluor respiratory screen for rapid detection of multiple respiratory viruses in clinical specimens by immunofluorescence staining. J. Clin. Microbiol. 38:708-711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Langedijk, J. P., F. J. Daus, and J. T. van Oirschot. 1997. Sequence and structure alignment of Paramyxoviridae attachment proteins and discovery of enzymatic activity for a morbillivirus hemagglutinin. J. Virol. 71:6155-6167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210.Lee, M. S., D. P. Greenberg, S. H. Yey, R. Yogev, K. S. Reisinger, J. I. Ward, M. M. Blatter, I. Cho, S. J. Holmes, J. M. Cordova, M. J. August, W. Chen, H. B. Mehta, K. L. Coelingh, and P. M. Mendelman. 2001. Antibody responses to bovine parainfluenza virus type 3 (PIV3) vaccination and human PIV3 infection in young infants. J. Infect. Dis. 184:909-913. [DOI] [PubMed] [Google Scholar]
- 211.Lehrich, J. R., D. G. Arnason, T. C. Fuller, and S. H. Wray. 1974. Parainfluenza, histocompatibility, and multiple sclerosis. Association of parainfluenza antibodies and histocompatibility types in 115 and optic neuritis. Arch. Neurol. 30:327-379. [DOI] [PubMed] [Google Scholar]
- 212.Lennette, E. H., F. W. Jensen, R. W. Guenther, and R. L. Magoffin. 1963. Serologic responses to parainfluenza viruses in patients with mumps virus infection. J. Lab. Clin. Med. 61:780-788. [PubMed] [Google Scholar]
- 213.Lewandowski, L. J., F. S. Lief, I. I. A. Verini, M. M. Pienkowski, V. ter Meule, and H. Koprowski. 1974. Analysis of a viral agent isolated from multiple sclerosis brain tissue: characterization as a parainfluenza virus type 1. J. Virol. 13:1037-1045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.Lewis, V. A., R. Champlin, and J. Englund. 1996. Respiratory disease due to parainfluenza virus in adult bone marrow transplant recipients. Clin. Infect. Dis. 23:1033-1037. [DOI] [PubMed] [Google Scholar]
- 215.Lin, G. Y., and R. A. Lamb. 2000. The paramyxovirus simian virus 5 V protein slows progression of the cell cycle. J. Virol. 74:9152-9166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Lindquist, S. W., A. Darnule, A. Istas, and G. J. Demmler. 1997. Parainfluenza virus type 4 infections in pediatric patients. Pediatr. Infect. Dis. J. 16:34-38. [DOI] [PubMed] [Google Scholar]
- 217.Liolios, L., A. Jenney, D. Spelman, T. Kotsimbos, M. Catton, and S. Wesselingh. 2001. Comparison of a multiplex reverse transcription-PCR-enzyme hybridization assay with conventional viral culture and immunofluorescence techniques for the detection of seven viral respiratory pathogens. J. Clin. Microbiol. 39:2779-2783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.Liston, S. L., R. C. Gehrz, L. C. Siegel, and J. Tilelli. 1983. Bacterial tracheitis. Am. J. Dis. Child. 137:764-767. [DOI] [PubMed] [Google Scholar]
- 219.Little, B. W., W. S. Tihen, J. O. Dickerman, and J. E. Craighead. 1981. Giant cell pneumonia associated with parainfluenza virus type 3 infection. Hum. Pathol. 12:478-481. [DOI] [PubMed] [Google Scholar]
- 220.Ljungman, C. A., C. A. Gleaves, and J. D. Meyers. 1989. Respiratory virus infection in immunocompromised patients. Bone Marrow Transplant. 4:35-40. [PubMed] [Google Scholar]
- 221.Louqhlin, G. M., and L. M. Taussig. 1979. Pulmonary function in children with a history of laryngotracheobronchitis. J. Pediatr. 94:365-369. [DOI] [PubMed] [Google Scholar]
- 222.Luczak, M., M. Korbecki, M. Kobus, and W. Hankiewicz. 1971. Puromycin as an inhibitor of parainfluenza 3 virus multiplication. Acta. Virol. 15:374-380. [PubMed] [Google Scholar]
- 223.Luczak, M., and M. Korbecki. 1970. Comparitive studies on susceptibility of established cell lines to parainfluenza 3 virus. Acta Virol. (Prague) 14:279-284. [PubMed] [Google Scholar]
- 224.Lujan-Zilbermann, J., E. Benaim, X. Tong, D. K. Srivastava, C. C. Patrick, and J. P. DeVincenzo. 2001. Respiratory virus infections in pediatric hematopoietic stem cell transplantation. Clin. Infect. Dis. 33:962-968. [DOI] [PubMed] [Google Scholar]
- 225.Lyon, M., C. Leroux, T. Greenland, J. Chastang, J. Patet, and J. F. Mornex. 1997. Presence of a unique parainfluenza virus 3 strain identified by RT-PCR in visna-maedi virus infected sheep. Vet. Microbiol. 51:95-104. [DOI] [PubMed] [Google Scholar]
- 226.MacDonald, N. E., N. Wolfish, P. McLaine, P. Phipps, and E. Rossier. 1986. Role of respiratory viruses inexacerbations of primary nephrotic syndrome. J. Pediatr. 108:378-382. [DOI] [PubMed] [Google Scholar]
- 227.Malinowski, M. D., and R. W. Hostoffer. 2001. Home care based treatment with short course inhaled ribavirin of parainfluenza in a patient with severe combined immunodeficiency. J. Allergy Clin. Immunol. 107:663. [Google Scholar]
- 228.Mandelboim, O., N. Lieberman, M. Lev, L. Paul, T. I. Arnon, Y. Bushkin, D. M. Davis, J. L. Strominger, J. W. Yewdell, and A. Porgador. 2001. Recognition of haemagglutinins on virus-infected cells by NKp46 activates lysis by human NK cells. Nature 409:1055-1060. [DOI] [PubMed] [Google Scholar]
- 229.Marks, M. I., H. Nagahama, and J. J. Eller. 1971. Parainfluenza virus immunofluorescence. In vitro and clinical application of the direct method. Pediatrics 48:73-78. [PubMed] [Google Scholar]
- 230.Maru, M., M. Haraguchi, K. Sato, K., H. Hotta, and M. Homma. 1992. Evaluation of a protease activation mutant of Sendai virus as a potent live vaccine. Vet. Microbiol. 30:1-12. [DOI] [PubMed] [Google Scholar]
- 231.Marx, A., H. E. Gary, B. J. Marston, D. D. Erdman, R. F. Breiman, T. J. Torok, J. F. Plouffe, T. M. File, and L. J. Anderson. 1999. Parainfluenza virus infection among adults hospitalized for lower respiratory tract infection. Clin. Infect. Dis. 29:134-140. [DOI] [PubMed] [Google Scholar]
- 232.Marx, A., T. J. Torok, R. C. Holman, M. J. Clarke, and L. J. Anderson. 1997. Pediatric hospitalizations for croup (laryngotracheobronchitis): biennial increases associated with human parainfluenza virus 1 epidemics. J. Infect. Dis. 176:1423-1427. [DOI] [PubMed] [Google Scholar]
- 233.Mascoli, C. C., T. A. Gower, F. A. Capilupo, and D. P. Metzger. 1976. Further studies in the neonatal ferret model of infection and immunity to and attenuation of human parainfluenza viruses. Dev. Biol. Stand. 33:384-390. [PubMed] [Google Scholar]
- 234.Matsuoka, Y., J. Curran, T. Pelet, D. Kolakofsky, R. Ray, and R. W. Compans. 1991. The P gene of human parainfluenza virus type 1 encodes P and C proteins but not a cysteine-rich V protein. J. Virol. 65:3406-3410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 235.McCarthy, V. P., J. R. Carlile, P. S. Reichelderfer, and J. S. Clark. 1987. Parainfluenza type 3 in newborns. Pediatr. Infect. Dis. J. 6:217-218. [DOI] [PubMed] [Google Scholar]
- 236.McIntosh, K., S. C. Kurachek, L. M. Cairns, J. C. Burns, and B. Goodspeed. 1984. Treatment of respiratory viral infection in an immunodeficient infant with ribavirin aerosol. Am. J. Dis. Child. 138:305-308. [DOI] [PubMed] [Google Scholar]
- 237.McIntosh, K. 1991. Pathogenisis of severe acute respiratory infections in the developing world: respiratory syncytial virus and parainfluenza viruses. Rev. Infect. Dis. 13:S492-S500. [DOI] [PubMed] [Google Scholar]
- 238.McLean, O. M., R. M. Bannatyne, and K. F. Givan. 1967. Myxovirus dissemination by air. Can. Med. Assoc. J. 96:1449-1453. [PMC free article] [PubMed] [Google Scholar]
- 239.McSherry, G. D. 1996. Human immunodeficiency-virus-related pulmonary infections in children. Semin. Respir. Infect. 11:173-183. [PubMed] [Google Scholar]
- 240.Meindl, P., G. Bodo, P. Palese, J. Schulman, and H. Tuppy. 1974. Inhibition of neuraminidase activity by derivatives of 2-deoxy-2,3-debydro-N-acetyineurmaminic acid. Virology 58:457-463. [DOI] [PubMed] [Google Scholar]
- 241.Meissner, H. C., S. A. Murray, M. A. Kiernan, D. R. Snydman, and K. Mcintosh. 1984. A simultaneous outbreak of respiratory syncytial virus and parainfluenza virus type 3 in a newborn nursery. J. Pediatr. 104:680-684. [DOI] [PubMed] [Google Scholar]
- 242.Meolen, V., H. Koprowski, Y. Iwasaki, K. M. Kackell, and D. Muller. 1972. Fusion of cultured multiple-sclerosis brain cells with indicator cells: presence of nucleocapsids and virions and isolation of parainfluenza-type virus. Lancet ii:1-5. [DOI] [PubMed]
- 243.Miller, R. H., A. R. Pursell, F. E. Mitchell, and K. M. Johnson. 1964. A newly discovered myxovirus (S.V_41) isolated from cell cultures of cynomologus monkey kidney. Am. J. Hyg. 80:365-376. [DOI] [PubMed] [Google Scholar]
- 244.Miller, W. S., and M. S. Artenstein. 1967. Aerosol stability of three acute respiratory disease viruses. Proc. Soc. Exp. Biol. Med. 125:222-227. [DOI] [PubMed] [Google Scholar]
- 245.Mo, X. Y., S. R. Sarawar, and P. C. Doherty. 1995. Induction of cytokines in mice with parainfluenza pneumonia. J. Virol. 69:1288-1291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 246.Morein, B., M. Sharp, B. Sundquist, and K. Simons. 1983. Protein subunit vaccines of parainfluenza type 2 virus: immunogenic effect in lambs and mice. J. Gen. Virol. 64:1557-1569. [DOI] [PubMed] [Google Scholar]
- 247.Mori, I., T. Komatsu, K. Takeuchi, K. Nakakuki, M. Sudo, and Y. Kimura. 1995. Parainfluenza virus type 1 infects olfactory neurons and establishes long-term persistence in the nerve tissue. J. Gen. Virol. 76:1251-1254. [DOI] [PubMed] [Google Scholar]
- 248.Mori, I., K. Nakakuki, and Y. Kimura. 1996. Temperature-sensitive parainfluenza type 1 vaccine virus directly accesses the central nervous system by infecting olfactory neurons. J. Gen. Virol. 77:2121-2124. [DOI] [PubMed] [Google Scholar]
- 249.Morimoto, Y., Y. Doi, and H. Itoh. 1970. Effect of trypsin on reproduction of type 4 parainfluenza virus in vero cell cultures under fluid overlay. Jpn. J. Med. Sci. Biol. 23:1-11. [DOI] [PubMed] [Google Scholar]
- 250.Moriucki, H., T. Oshima, H. Nishimura, K. Ilakamura, N. Katsushima, and Y. Numazaki. 1990. Human malignant melanoma cell line (HMV-II) for isolation of influenza C and parainfluenza viruses. J. Clin. Microbiol. 28:1147-1150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 251.Moscona, A., and R. W. Peluso. 1992. Fusion properties of cells infected with human parainfluenza virus type 3: receptor requirements for viral spread and virus-mediated membrane fusion. J. Virol. 66:6280-6287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 252.Moscona, A., and R. W. Peluso. 1991. Fusion properties of cells persistently infected with human parainfluenza virus type 3: participation of hemagglutinin-neuraminidase in membrane fusion. J. Virol. 65:2773-2777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 253.Moscona, A. I1997. Interaction of human parainfluenza virus type 3 with the host cell surface. Pediatr. Infect. Dis. J. 16:917-924. [DOI] [PubMed] [Google Scholar]
- 254.Mounts, A. W., H. Kaur, U. D. Parashar, T. G. Ksiazek, D. Cannon, J. T. Arokiasamy, L. J. Anderson, M. S. Lye, and the Nipah Virus Nosocomial Study Group. 2001. J. Infect. Dis. 183:810-813. [DOI] [PubMed] [Google Scholar]
- 255.Mozdzanowska, K., M. Furchner, G. Washko, J. Mozdzanowski, and W. Gerhard. 1997. A pulmonary influenza virus infection in SCID mice can be cured by treatment with hemagglutinin-specific antibodies that display very low virus-neutralizing activity in vivo. J. Virol. 71:4347-4355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 256.Muchmore, H. G., A. J. Parkinson, J. E. Humphries, E. N. Scott, D. A. Mclntosh, L. V. Scott, M. K. Cooney, and J. A. Miles. 1981. Persistent parainfluenza virus shedding during isolation at the South Pole. Nature 289:187-189. [DOI] [PubMed] [Google Scholar]
- 257.Reference deleted.
- 258.Mufson, M. A., H. E. Mocega, and H. E. Krause. 1973. Acquisition of parainfluenza 3 virus infection by hospitalized children. I. Frequencies, rates and temporal data. J. Infect. Dis. 128:141-147. [DOI] [PubMed] [Google Scholar]
- 259.Murphy, B., P. D. Phelan, I. Jack, and E. Uren. 1980. Seasonal pattern in childhood viral lower respiratory tract infections in Melbourne. Med. J. Aust. 1:22-24. [DOI] [PubMed] [Google Scholar]
- 260.Murphy, B. R., B. S. Graham, G. A. Prince, et al. 1986. Serum and nasal-wash immunogloblin G and A antibody response of infants and children to respiratory syncytial virus F and G glycoproteins following primary infection. J. Clin. Microbiol. 23:1009-1014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 261.Murphy, D. G., K. Dimock, and C. Y. Kang. 1991. Numerous transitions in human parainfluenza virus 3 RNA recovered from persistently infected cells. Virology 181:760-763. [DOI] [PubMed] [Google Scholar]
- 262.Murphy, T. F., F. W. Henderson, W. A. Clyde, A. M. Collier, and F. W. Denny. 1981. Pneumonia: an eleven year study in a pediatric practice. Am. J. Epidemiol. 113:12-21. [DOI] [PubMed] [Google Scholar]
- 263.Murrell, M. T., M. Porotto, O. Greengard, N. Poltoratskaia, and A. Moscona. 2001. A single amino acid alteration in the human parainfluenza virus type 3 hemagglutinin-neuraminidase glycoprotein confers resistance to the inhibitory effects of zanamivir on receptor binding and neuraminidase activity. J. Virol. 75:6310-6320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 264.Nelson, C. B., B. S. Pomeroy, K. Schrall, W. E. Park, and R. J. Lindeman. 1962. An outbreak of conjunctivitis due to Newcastle disease virus (NDV) occurring in poultry workers. Am. J. Public Health 42:672.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 265.Nichol, S. T., J. Arikawa, and Y. Kawaoka. 2000. Emerging viral diseases. Proc. Natl. Acad. Sci. USA 97:12411-12412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 266.Nicholas, W. G., L. Corey, T. Gooley, C. Davis, and M. Boeckh. 2001. Parainfluenza virus infections after hematopoietic stem cell transplantation: risk factors, response to antiviral therapy, and effect on transplant outcome. Blood 98:573-578. [DOI] [PubMed] [Google Scholar]
- 267.Nichols, W. G., T. Gooley, and M. Boeckh. 2001. Community acquired respiratory syncytial virus and parainfluenza virus infections after hematopoietic stem cell transplantation: The Fred Hutchinson Cancer Research Center experience. Biol. Blood Marrow Transplant. 7:11S-15S. [DOI] [PubMed]
- 268.Nishio, M., M. Tsurudome, M. Ito, M. Kawano, H. Komada, and Y. Ito. 2001. High resistance of human parainfluenza type 2 virus protein-expressing cells to the antiviral and anti-cell proliferative activities of alpha/beta interferons: cysteine-rich V-specific domain is required for high resistance to the interferons. J. Virol. 75:9165-9176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 269.Nishio, M., M. Tsurudome, M. Ito, M. Kawano, S. Kusagawa, H. Komada, and Y. Ito. 1999. Isolation of monoclonal antibodies directed against the V protein of human parainfluenza virus type 2 and localization of the V protein in virus-infected cells. Med. Microbiol. Immunol. 188:79-82. [DOI] [PubMed] [Google Scholar]
- 270.Nohynek, H., J. Eskola, E. Laine, P. Halonen, P. Ruutu, P. Saikku, M. Kleemola, and M. Leinonen. 1991. The causes of hospital-treated acute lower respiratory tract infection in children. Am. J. Dis. Child. 145:618-622. [DOI] [PubMed] [Google Scholar]
- 271.Numazaki, Y., T. Oshima, A. Ohmi, A. Tanaka, Y. Oizumi, S. Komatsu, T. Takagi, M. Karahashi, and N. Ishida. 1987. A microplate method for isolation of viruses from infants and children with acute respiratory infections. Microbiol. Immunol. 31:1085-1095. [DOI] [PubMed] [Google Scholar]
- 272.Numazaki, Y., S. Shigeta, N. Yano, S. Takai, and N. Ishida. 1968. A variant of parainfluenza type 2 virus. Proc. Soc. Exp. Biol. Med. 127:992-996. [DOI] [PubMed] [Google Scholar]
- 273.O'Connor, J. V., and S. K. Iyer. 1982. Myoglobinuria associated with parainfluenza type 2 infection. N. Y. State J. Med. 82:1469-1470. [PubMed] [Google Scholar]
- 274.Ohgimoto, S., H. Bando, M. Kawano, K. Okamoto, K. Kondo, K. M. Tsurudome, M. Nishio, and Y. Ito. 1990. Sequence analysis of P gene of human parainfluenza type 2 virus: P and cysteone-rich proteins are translated by two mRNAs that differ by two nontemplated G residues. Virology 177:116-123. [DOI] [PubMed] [Google Scholar]
- 275.Okamoto, K., M. Tsurudome, S. Ohgimoto, M. Kawana, M. Nishio, H. Komada, M. Ito, Y. akakura, and Y. Ito. 1997. An anti-fusion regulatory protein-1 monoclonal antibody suppresses human parainfluenza virus type 2-induced cell fusion. J. Gen. Virol. 78:83-89. [DOI] [PubMed] [Google Scholar]
- 276.Olsen, M. A., K. M. Shuck, A. R. Sambol, S. M. Flor, J. O'Brien, and B. J. Cabrera. 1993. Isolation of seven respiratory viruses in shell vials: a practical and highly sensitive method. J. Clin. Microbiol. 31:422-425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 277.O'Reilly, J. F. 1930. Adult bronchiolitis and parainfluenza type 2. Postgrad. Med. J. 56:787.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 278.Ortmann, D., M. Ohuchi, H. Angliker, E. Shaw, W. Garten, and K. S. Klenk. 1994. Proteolytic cleavage of wild type and mutants of the F protein of human parainfluenza virus type 3 by two subtilisin-like endoproteases, furin and Kex2. J. Virol. 68:2772-2776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 279.Parkinson, A. J., H. G. Muchmore, L. V. Scott, and J. A. Miles. 1980. Parainfluenza virus isolation enhancement utilizing a portable cell culture system in the field. J. Clin. Microbiol. 11:535-536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 280.Parks, G. D., and R. A. Lamb. 1990. Defective assembly and intracellular transport of mutant paramyxovirus hemagglutinin-neuraminidase proteins containing altered cytoplasmic domans. J. Virol. 64:3605-3616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 281.Pastey, M., T. L. Gower, P. W. Spearman, J. E. Crowe, and B. S. Graham. 2000. A rhoA-derived peptide inhibits syncytium formation induced by respiratory syncytial virus and parainfluenza virus type 3. Nat. Med. 6:35-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 282.Paterson, R. G., R. A. Lamb, B. Moss, and B. R. Murphy. 1987. Comparison of the relative roles of the F and HN surface glycoproteins of the paramyxovirus simian virus 5 in inducing protective immunity. J. Virol. 61:1972-1977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 283.Patterson, S., J. Gross, and J. S. Oxford. 1988. The intracellular distribution of influenza virus matrix protein and nucleoprotein in infected cells and their relationship to haemagglutinin in the plasma membrane. J. Gen. Virol. 69:1859-1872. [DOI] [PubMed] [Google Scholar]
- 284.Peltola, V., T. Heikkinen, and O. Ruuskanen. 2002. Clinical courses of croup caused by influenza and parainfluenza viruses. Pediatr. Infect. Dis. J. 21:76-78. [DOI] [PubMed] [Google Scholar]
- 285.Peramaki, E., I. Salmi, T. Kava, T. Romppanen, and T. Hakkarainen. 1991. Unilateral bronchiolitis oblinterans organizing pnuemonia and bronchoalveolar lavage neurtrophilia in a patient with parainfluenza 3 virus infection. Respir. Med. 85:159-161. [DOI] [PubMed] [Google Scholar]
- 286.Phillips, M. J., L. M. Blendis, S. Poucell, J. Offerson, M. Petric, E. Roberts, G. A. Levy, R. A. Superina, P. D. Greig, and R. Cameron. 1991. Syncytial giant-cell hepatitis. Sporadic hepatitis with distinctive pathological features, a severe clinical course, and paramyxoviral features. N. Engl. J. Med. 324:455-460. [DOI] [PubMed] [Google Scholar]
- 287.Phillips, P. E., and C. L. Christian. 1970. Myxovirus antibody increases in human connective tissue disease. Science 168:982-984. [DOI] [PubMed] [Google Scholar]
- 288.Piga, N., N. Kessler, M. P. Layani, and M. Aymard. 1990. Correlation between the reactivity patterns of monoclonal antibodies to distinct antigenic sites on HN glycoprotein and their protective abilities in Sendai (6/94) virus infection. Arch. Virol. 110:179-193. [DOI] [PubMed] [Google Scholar]
- 289.Porotto, M., O. Greengard, N. Poltoratskaia, M. A. Horga, and A. Moscona. 2001. Human parainfluenza virus type 3 HN-receptor interaction effect of 4-guanidino-Neu5Ae2en on a neuraminidase-deficient variant. J. Virol. 75:7481-7488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 290.Porter, D. D., G. A. Prince, V. G. Hemming, and H. G. Porter. 1991. Pathogenesis of human parainfluenza virus 3 infection in two species of cotton rats: Sigmodon hispidus develops bronchiolitis, while Sigmodon fulviventer develops interstitial pneumonia. J. Virol. 65:103-111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 291.Prince, G. A., and D. D. Porter. 1996. Treatment of parainfluenza virus type 3 bronchiolitis and pneumonia in a cotton rat model using topical antibody and glucocorticosteroid. J. Infect. Dis. 173:598-608. [DOI] [PubMed] [Google Scholar]
- 292.Prinoski, K., M. J. Cote, C. Y. Kang, and K. Dimock. 1992. Evolution of the fusion protein gene of human parainfluenza virus 3. Virus. Res. 22:55-69. [DOI] [PubMed] [Google Scholar]
- 293.Profeta, M. L., F. S. Lief, and S. A. Plotkin. 1969. Enzootic sendai infection in laboratory hamsters. Am. J. Epidemiol. 89:316-24. [DOI] [PubMed] [Google Scholar]
- 294.Puthavathana, P., C. Wasi, U. Kositanont, S. Suwanjutha, T. Chantarojanasiri, W. Kantakamaiakul, P. Kantawateera, and P. ThonDcharoen. 1990. A hospital-based study of acute viral infections of the respiratory tract in Thai children, with emphasis on laboratory diagnosis. Rev. Infect. Dis. 12:S988-S994. [DOI] [PubMed] [Google Scholar]
- 295.Quan, S. F., R. J. M. L. Lemen, D. L. Witten, D. L. Sherrill, R. Grad, R. E. Sobonya, and C. G. Ray. 1990. Changes in lung mechanics and reactivity with age after viral bronchiolitis in beagle puppies. J. Appl. Physiol. 69:2034-2042. [DOI] [PubMed] [Google Scholar]
- 296.Rabalais, G. P., G. G. Stout, K. L. Ladd, and K. M. Cost. 1992. Rapid diagnosis of respiratory viral infections by using a shell vial assay and monoclonal antibody pool. J. Clin. Microbiol. 30:1505-1508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 297.Randall, R. E., and A. Bermingham. 1996. NP:P and NP:V interactions of the paramyxovirus simian virus 5 examined using a novel protein:protein capture assay. Virology 224:121-129. [DOI] [PubMed] [Google Scholar]
- 298.Randall, R. E., and D. F. Young. 1988. Comparison between parainfluenza virus type 2 and simian virus 5: monoclonal antibodies reveal major antigenic differences. J. Gen. Virol. 69:2051-2060. [DOI] [PubMed] [Google Scholar]
- 299.Ray, C. G., and L. L. Minnich. 1987. Efficiency of immunoflourescence for rapid detection of common respiratory viruses. J. Clin. Microbiol. 25:355-357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 300.Ray, R., V. E. Brown, and R. W. Compans. 1985. Glycoproteins of human parainfluenza virus type 3: characterization and evaluation as a subunit vaccine. J. Infect. Dis. 152:1219-1230. [DOI] [PubMed] [Google Scholar]
- 301.Ray, R., and R. W. Compans. 1986. Monoclonal antibodies reveal extensive antigenic differences between the hemagglutinin-neuraminidase glycoproteins of human and bovine parainfluenza 3 viruses. Virology 148:232-236. [DOI] [PubMed] [Google Scholar]
- 302.Ray, R., J. Duncan, R. Quinn, and Y. Matsuoka. 1992. Distinct hemaggutinin and neuraminidase epitopes involved in antigenic variation of recent human parainfluenza virus type 2 isolates. Virus Res. 24:107-113. [DOI] [PubMed] [Google Scholar]
- 303.Ray, R., B. J. Glaze, Z. Moldoveanu, and R. W. Compans. 1988. Intranasal immunization of hamsters with envelope glycoproteins of human parainflueza virus type 3. J. Infect. Dis. 157:648-654. [DOI] [PubMed] [Google Scholar]
- 304.Ray, R., R. Matsuoka, T. L. Burnett, B. J. Glaze, and R. W. Campans. 1990. Human parainfluenza virus induces a type-specific protective immune response. J. Infect. Dis. 162:746-749. [DOI] [PubMed] [Google Scholar]
- 305.Riedel, F., C. Benden, S. Philippou, H. J. Streckert, and W. Marek. 1997. Role of sensory neuropeptides in PIV-3-infection-induced airway hyperresponsiveness in guinea pigs. Respiration 64:211-219. [DOI] [PubMed] [Google Scholar]
- 306.Riedel, F., A. Krause, W. Slenczyka, and C. H. L. Rieger. 1996. Parainfluenza-3-virus infection enhances allergic sensitization in the guinea-pig. Clin. Exp. Allergy 26:603-609. [PubMed] [Google Scholar]
- 307.Robbins, S. J., H. Wrzos, A. L. Kline, R. B. Tenser, and F. Rapp. 1981. Rescue of a cytopathic paramyxovirus from peripheral blood leukocytes in subacute sclerosing panencephalitis. J. Infect. Dis. 143:396-403. [DOI] [PubMed] [Google Scholar]
- 308.Rocchi, G., G. Arangio-Ruiz, V. Giannini, A. M. Jemolo, G. Andreoni, and I. Archetti. 1970. Detection of viraemia in acute respiratory disease of man. Acta Virol. 14:405-407. [PubMed] [Google Scholar]
- 309.Roman, G., C. A. Phillips, and C. M. Poser. 1978. Parainfluenza virus type 3: isolation from CSF of a patient with Guillain-Barré syndrome. JAMA 240:1613-1615. [PubMed] [Google Scholar]
- 310.Ruuskanen, O., M. Arola, T. Heikkinen, and T. Ziegler. 1991. Viruses in acute otitis media: increasing evidence for clinical significance. Pediatr. Infect. Dis. J. 10:425-427. [DOI] [PubMed] [Google Scholar]
- 311.Sabina, L. R., and T. W. Munro. 1969. Effects of trypsin on replication of parainfluenza-3 virus in HEp-2 cell cultures. Can. J. Microbiol. 15:577-582. [DOI] [PubMed] [Google Scholar]
- 312.Saladino, R., C. Crestini, A. T. Palamara, M. C. Danti, F. Manetti, F. Corelli, E. Garaci, and M. Botta. 2001. Synthesis, biological evaluation, and pharmacophore generation of uracil, 4(3H)-pyrimidinone, and uridine derivatives as potent and selective inhibitors of parainfluenza 1 (Sendae) virus. J. Med. Chem. 44:4554-4562. [DOI] [PubMed] [Google Scholar]
- 313.Sanchez, A., and A. K. Banerjee. 1985. Studies on human parainfluenza virus 3: characterization of the structural proteins and in vitro synthesized proteins coded by mRNAs isolated from infected cells. Virology 143:45-54. [DOI] [PubMed] [Google Scholar]
- 314.Sangster, M., F. S. Smith, C. Coleclough, and J. L. Hurwitz. 1995. Human parainfluenza virus type 1 immunization of infant mice protects from subsequent Sendai virus infection. Virology 212:13-19. [DOI] [PubMed] [Google Scholar]
- 315.Sarkkinen, H. K., P. E. Halonen, and A. A. Salmi. 1981. Type-specific detection of parainfluenza viruses by enzyme-immunoassay and radioimmunoassay in nasopharygeal specimens of patients with acute respiratory disease. J. Gen. Virol. 56:49-57. [DOI] [PubMed] [Google Scholar]
- 316.Sarkkinen, H. K., O. Meurman, T. T. Salmi, and H. Puhakka. 1983. Demonstration of viral antigens in middle ear secretions of children with acute otitis media. Acta. Paediatr. Scand. 72:137-138. [DOI] [PubMed] [Google Scholar]
- 317.Sarkkinen, H. K., P. E. Halonen, P. P. Arstiia, and A. A. Salmi. 1981. Detection of respiratory syncytial parainfluenza type 2, and adenovirus antigens by radioimmunoassay and enzyme immunoassay on nasopharyngeal specimens from children with acute respiratory disease. J. Clin. Microbiol. 13:258-265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 318.Scheid, A., and P. N. Choppin. 1976. Protease activation mutants of Sendai virus: Activation of biological properties by specific proteases. Virology 69:265-277. [DOI] [PubMed] [Google Scholar]
- 319.Schmidt, A. C., J. M. McAuliffe, A. Huang, S. R. Surman, J. E. Bailly, W. R. Elkins, P. L. Collins, B. R. Murphy, and M. H. Skiadopoulos. 2000. Bovine parainfluenza virus type 3 (BPIV3) fusion and hemagglutinin-neuraminidase glycoproteins make an important contribution to the restricted replication of BPIV3 in primates. J. Virol. 74:8922-8929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 320.Schmidt, A. C., J. M. McAuliffe, B. R. Murphy, and P. L. Collins. 2001. Recombinant bovine/human parainfluenza virus type 3 (B/HPIV3) expressing the respiratory syncytial virus (RSV) G and F proteins can be used to achieve simultaneous mucosal immunization against RSV and HPIV3. J. Virol. 75:4594-4603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 321.Seidman, D. S., D. Nass, E. Mendelson, I. Shehtman, S. Mashiach, and R. Achiron. 1996. Prenatal ultrasonographic diagnosis of fetal hydrocephalus due to infection with parainfluenza virus type 3. Ultrasound Obstet. Gynecol. 7:52-54. [DOI] [PubMed] [Google Scholar]
- 322.Shay, D. K., R. C. Holman, R. D. Newman, L. L. Liu, J. W. Stout, and L. J. Anderson. 1999. Bronchiolitis-associated hospitalization among US children, 1980-1996. JAMA 282:1440-1446. [DOI] [PubMed] [Google Scholar]
- 323.Shimokata, K., Y. Ito, Y. Nishiyama, and Y. Kimura. 1980. Influence of trypsin on the infectivity and biological properties of parainfluenza type 2 (croup-associated) virus in Vero cells. J. Gen. Virol. 48:407-410. [DOI] [PubMed] [Google Scholar]
- 324.Shimokata, K., Y. Ito, Y. Nishiyama, and Y. Kimura. 1981. Plaque formation by human-origin parainfluenza type 2 virus in established cell lines. Arch. Virol. 67:355-360. [DOI] [PubMed] [Google Scholar]
- 325.Siber, G. R., J. Leszcynski, W. Pena-Cruz, C. Ferren-Gardner, R. Anderson, V. G. Hemming, E. E. Walsh, J. Burns, K. McIntosh, and R. Gonin. 1992. Protective activity of a human respiratory syncytial virus immune globulin prepared from donors screened by microneutralization assay. J. Infect. Dis. 165:456-463. [DOI] [PubMed] [Google Scholar]
- 326.Sidwell, R. W., G. P. Khare, L. B. Allen, J. G. Huffman, J. T. Witkowski, L. N. Simon, and R. K. Robins. 1975. In vitro and in vivo effect of 1-beta-d-ribofuranosyl-1,2,4-triazole-3-carboxamide (ribavirin) on types 1 and 3 parainfluenza virus infections. Chemotherapy 21:205-220. [DOI] [PubMed] [Google Scholar]
- 327.Sieg, S., C. King, Y. Huang, and D. Kaplan. 1996. The role of interleukin-10 in the inhibition of T-cell proliferation and apoptosis mediated by parainfluenza virus type 3. J. Virol. 70:4845-4848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 328.Singh-Naz, N., M. Willy, and N. Riggs. 1989. 1990. Outbreak of parainfluenza virus type 3 in a neonatal nursery. Pediatr. Infect. Dis. J. 9:31-33. [DOI] [PubMed] [Google Scholar]
- 329.Skolnik, N. S. 1989. Treatment of croup. A critical review. Am. J. Dis. Child. 143:1045-1049. [DOI] [PubMed] [Google Scholar]
- 330.Smith, C. B., R. H. Purcell, J. A. Bellanti, and R. M. Chanock. 1966. Protective effect of antibody to parainfluenza type 1 virus. N. Engl. J. Med. 275:1145-1152. [DOI] [PubMed] [Google Scholar]
- 331.Somani, R., and M. J. Evans. 2001. Role of glucocorticoids in treating croup. Can. Fam. Physician 47:733-735. [PMC free article] [PubMed] [Google Scholar]
- 332.Soret, M. G. 1969. Antiviral activity of calcium elenlate on parainfluenza infection of hamsters. Antimicrob. Agents Chemother. 9:160-166. [DOI] [PubMed] [Google Scholar]
- 333.Sorkness, R., R. F. J. Lemanske, and W. L. Castleman. 1991. Persistent airway hyperresponsiveness after neonatal viral bronchiolitis in rats. J. Appl. Physiol. 70:375-383. [DOI] [PubMed] [Google Scholar]
- 334.Sorkness, R. L., H. Mehta, M. R. Kaplan, M. Miyasaka, S. L. Hefle, and R. F. Lemanske. 2000. Effect of ICAM-1 blockade on lung inflammation and physiology during acute viral bronchiolitis in rats. Pediatr. Res. 47:819-824. [DOI] [PubMed] [Google Scholar]
- 335.Southern, J. A., O. Precious, and R. E. Randall. 1990. Two nontemplated nucleotide additions are required to generate the P mRNA of parainfluenza virus type 2 since the RNA genome encodes protein V. Virology 177:388-390. [DOI] [PubMed] [Google Scholar]
- 336.Sparrelid, E., P. Ljungman, E. Ekelof-Andstrom, J. Aschan, O. Ringden, J. Winiarski, B. Wahlin, and J. Andersson. 1997. Ribavirin therapy in bone marrow transplant recipients with viral respiratory tract infections. Bone Marrow Transplant. 19:905-908. [DOI] [PubMed] [Google Scholar]
- 337.Spriggs, M. K., P. L. Collins, E. Tierney, W. T. London, and A. R. Murphy. 1988. Immunization with vaccinia virus recombinants that express the surface glycoproteins of human parainfluenza virus type 3 (PIV3) protects pates monkeys against PIV3 infection. J. Virol. 62:1293-1296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 338.Spriggs, M. K., P. L. Collins, E. Tierney, W. T. London, and B. R. Murphy. 1988. Immunization with vaccinia virus recombinants that express the surface glycoproteins of human parainfluenza virus type 3; (PIV3) protects pates monkeys against PIV3 infection. J. Virol. 62:1233-1236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 339.Spriggs, M. K., and P. L. Collins. 1986. Human parainfluenza virus type 3: messenger RNAs, polypeptide coding assignments, intergenic sequences, and genetic map. J. Virol. 59:646-654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 340.Spriggs, M. K., B. R. Murphy, G. A. Prince, R. A. Olmsted, and P. L. Collins. 1987. Expression of the F and HN glycoproteins of human parainfluenza virus type 3 by recombinant vaccinia viruses: contributions or the individual proteins to host immunity. J. Virol. 61:3416-3423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 341.Stokes, G. M., A. D. Milner, I. G. C. Hodges, and R. C. Groggins. 1981. Lung function abnormalities after acute bronchiolitis. J. Pediatr. 98:871-874. [DOI] [PubMed] [Google Scholar]
- 342.Stokes, J. R., R. L. Sorkness, M. R. Kaplan, W. L. Castleman, M. A. Tomai, R. L. Miller, and R. F. Lamanske. 1998. Attenuation of virus-induced airway dysfunction in rats treated with imiquimod. Eur. Respir. J. 11:324-329. [DOI] [PubMed] [Google Scholar]
- 343.Storey, D. G., K. Dimock, and C. Y. Kang. 1984. Structural characterization of virion proteins and genomic RNA of human parainfluenza virus 3. J. Virol. 52:761-766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 344.Stout, C., M. D. Murphy, S. Lawrence, and S. Julian. 1989. Evaluation of a monoclonal antibody pool for rapid diagnosis of respiratory viral infections. J. Clin. Microbiol. 27:448-452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 345.Suzuki, T., A. Portner, R. A. Scroggs, M. Uchikawa, N. Koyama, K. Matsuo, Y. Suzuki, and T. Takimoto. 2001. Receptor specificities of humanrespiroviruses. J. Virol. 75:4604-4613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 346.Takano, T., M. Ohno, T. Yamano, and M. Shimada. 1991. Congenital hydrocephalus in suckling hamsters caused by transplacental infection with parainfluenza virus type 3. Brain Dev. 13:371-373. [DOI] [PubMed] [Google Scholar]
- 347.Tanabayashi, K., and R. W. Compans. 1996. Functional interaction of paramyxovirus glycoproteins: identification of a domain in Sendai virus HN which promotes cell fusion. J. Virol. 70:6112-6118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 348.Tao, T., M. H. Skiadopoulos, A. P. Durbin, F. Davoodi, P. L. Collins, and B. R. Murphy. 1999. A live attenuated chimeric recombinant parainfluenza virus (PIV) encoding the internal proteins of PIV type 3 and the surface glycoproteins of PIV type 1 induces complete resistance to PIV1 challenge and partial resistance to PIV3 challenge. Vaccine 17:1100-1108. [DOI] [PubMed] [Google Scholar]
- 349.Tashiro, M., and H. Homma. 1985. Protection of mice from wild-type Sendai virus infection by a trypsin-resistant mutant, TR-2. J. Virol. 53:228-234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 350.Tashiro, M., K. Tobita, J. T. Seto, and R. Rott. 1989. Comparison of protective effects of serum antibody on respiratory and systemic infection of Sendai virus in mice. Arch. Virol. 107:85-96. [DOI] [PubMed] [Google Scholar]
- 351.Thompson, S. D., V. G. Laver, K. G. Murti, and A. Portner. 1983. Isolation of a biologically active soluble form of the hemagglutinin-neuraminidase protein of Sendai virus. J. Virol. 62:4653-4660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 352.Tremonti, L. P., J. S. Lin, and G. G. Jackson. 1968. Neutralizing activity in nasal secretions and serum in resistance of volunteers to parainfluenza virus type 2. J. Immunol. 101:572-577. [PubMed] [Google Scholar]
- 353.Tremonti, L. P., and G. G. Jackson. 1969. Study of delayed hypersensitivity to myxoviruses induced by vaccines. Appl. Microbiol. 17:577-583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 354.Treuhaft, M. W., J. M. Soulup, and B. J. Sullivan. 1985. Practical recomendations for the detection of pediatric respiratory syncytial virus infections. J. Clin. Microbiol. 22:270-273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 355.Tsai, H. P., P. P. H. Kuo, C. C. Liu, and J. R. Wang. 2001. Respiratory viral infections among pediatric inpatients and outpatients in Taiwan from 1997 to 1999. J. Clin. Microbiol. 39:111-118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 356.Tsurudome, M., M. Nishio, H. Komada, H. Bando, and Y. Ito. 1989. Extensive antigenic diversity among human parainfluenza type 2 virus isolates and immunological relationships among paramyxoviruses revealed by monoclonal antibodies. Virology 171:38-48. [DOI] [PubMed] [Google Scholar]
- 357.Tuffaha, A., J. E. Gern, and R. F. Lemanske. 2000. The role of respiratory viruses in acute and chronic asthma. Clin. Chest Med. 21:289-300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 358.Tyrrell, D. A., and M. L. Bynoe. 1969. Studies on parainfluenza type 2 and 4 viruses obtained from patients with common colds. Br. Med. J. 1:471-474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 359.Ueda, K., D. A. Robbins, K. Iitaka, and C. C. Linnemann, Jr. 1978. Fatal rhabdomyolysis associated with parainfluenza type 3 infection. Hiroshima J. Med. Sci. 27:99-103. [PubMed] [Google Scholar]
- 360.Van den Hoogen, B., J. C. De Jong, J. Groen, T. Kuiken, R. Groot, R. Fuchier, and D. Osterhaus. 2001. A newly discovered human pneumovirus isolated from young children with respiratory tract disease. Nat. Med. 7:719-724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 361.van der Logt, J. T., A. M. van Loon, and J. van der Veen. 1982. Detection of parainfluenza IgM antibody by hemadsorption immunosorbent technique. J. Med. Virol. 10:213-221. [DOI] [PubMed] [Google Scholar]
- 362.van Wyke Coelingh, K. L., C. C. Winter, and B. R. Murphy. 1985. Antigenic variation in the hemagglutinin-neuraminidase protein of human parainfluenza type 3 virus. Virology 143:569-582. [DOI] [PubMed] [Google Scholar]
- 363.Van Wyke Coelingh, K. L., C. C. Winter, E. L. Tierney, S. L. Hall, W. T. London, H. W. Kim, R. I. I. Chanock, and B. R. Murphy. 1990. Antibody responses of humans and nonhuman primates to individual antigenic sites of the hemagglutinin-neuraminidase and fusion glycoproteins after primary infection or reinfection with parainfluenza type 3 virus. J. Virol. 64:3833-3843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 364.van Wyke Coelingh, K. L., C. C. Hinter, E. L. Tierney, W. T. London, and B. R. Murphy. 1988. Attenuation of bovine parainfluenza virus type 3 in nonnuman primates and its ability to confer immunity to human parainfluenza virus type 3 challenge. J. Infect. Dis. 157:655-662. [DOI] [PubMed] [Google Scholar]
- 365.van Wyke Coelingh, K. L., C. C. Winter, E. E. Jorgensen, and B. R. Murphy. 1987. Antigenic and structural properties of the hemagglutinin-neuraminidase glycoprotein of human parainfluenza virus type 3: sequence analysis of variants selected with monoclonal antibodies which inhibit infectivity, hemagglutination, and neuraminidase activites. J. Virol. 61:1473-1477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 366.Vasantha, S., K. L. Coelingh, B. R. Murphy, R. R. Dourmashkin, C. H. Hammer, M. M. Frank, and L. F. Fries. 1988. Interactions of a nonneutralizing IgM antibody and complement in parainfluenza virus neutralization. Virology 167:433-441. [PubMed] [Google Scholar]
- 367.Vilchez, R. A., K. McCurry, J. Dauber, A. Iacono, R. Keenan, Z. Zeevi, B. Griffith, and S. Kusne. 2001. The epidemiology of parainfluenza virus infection in lung transplant recipients. Clin. Infect. Dis. 33:2004-2008. [DOI] [PubMed] [Google Scholar]
- 368.Visseren, F. L. J., J. J. M. Bouwman, K. P. Bouter, R. J. A. Diepersloot, G. de Groot, and D. W. Erkelens. 2000. Procoagulant activity of endothelial cells after infection with respiratory viruses. Thromb. Haemostasis 84:319-324. [PubMed] [Google Scholar]
- 369.Von Euler, L., F. S. Kantor, and G. D. Hsiung. 1963. Studies of parainfluenza viruses. 1. Clinical, pathological and virological observations. Yale J. Biol. Med. 35:523-533. [PMC free article] [PubMed] [Google Scholar]
- 370.Vreede, R. W., H. Schellekens, and M. IuiJderwijk. 1992. Isolation of parainfluenza virus type 3 from cerebrospinal fluid. J. Infect. Dis. 165:1166.. [DOI] [PubMed] [Google Scholar]
- 371.Vuorinen, T., and O. Meurman. 1989. Enzyme immunoassays for detection of IgG and IgM antibodies to parainfluenza types 1, 2, and 3. J. Virol. Methods 23:63-70. [DOI] [PubMed] [Google Scholar]
- 372.Waner, J. L., N. J. Whitehurst, T. Downs, and O. G. Graves. 1985. Production of monoclonal antibodies against parainfluenza 3 virus and their use in diagnosis by immunofluorescence. J. Clin. Microbiol. 22:535-538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 373.Washburne, J. F., J. A. Bocchini, and R. M. Jamison. 1992. Summertime respiratory syncytial virus infection: Epidemiology and clinical manifestations. South. Med. J. 85:579-583. [DOI] [PubMed] [Google Scholar]
- 374.Wasserman, R., C. S. August, and S. A. Plotkin. 1988. Viral infections in pediatric bone marrow transplant patients. Pediatr. Infect. Dis. J. 7:109-115. [DOI] [PubMed] [Google Scholar]
- 375.Watanabe, N., M. Kawano, M. Tsurudome, M. Nishio, M. Ito, S. Ohgimoto, S. Suga, H. Komada, and Y. Ito. 1996. Binding of the V proteins to the nucleocapsid proteins of human parainfluenza type 2 virus. Scand. J. Microbiol. Immunol. 185:89-94. [DOI] [PubMed] [Google Scholar]
- 376.Wechsler, S. L., D. M. Lambert, M. S. Galinski, B. E. Heineke, and M. W. Pons. 1985. Human parainfluenza virus 3: purification and characterization of subviral components, viral proteins and viral RNA. Virus Res. 3:339-351. [DOI] [PubMed] [Google Scholar]
- 377.Weintrub, P. S., W. M. Sullender, C. Lombard, I. P. Link, and A. Arvin. 1987. Giant cell pneumonia caused by parainfluenza type 3 in a patient with acute myelomonocytic leukemia. Arch. Pathol. 111:569-570. [PubMed] [Google Scholar]
- 378.Welliver, R., D. T. Wong, T. S. Choi, and P. L. Ogra. 1982. Natural history of parainfluenza virus infection in childhood. J. Pediatr. 101:180-187. [DOI] [PubMed] [Google Scholar]
- 379.Welliver, R. C., D. T. Wong, E. J. Middletion, M. Sun, I. I. McCarthy, and P. L. Ogra. 1982. Role or parainfluenza virus-specific IgE in pathogenisis of croup and wheezing subsequent to infection. J. Pediatr. 101:889-896. [DOI] [PubMed] [Google Scholar]
- 380.Wendt, C. H., D. J. Weisdorf, M. C. Jordan, H. H. Balfour, Jr., and M. I. Hertz. 1992. Parainfluenza virus respiratory infection after bone marrow transplantation. N. Engl. J. Med. 326:921-926. [DOI] [PubMed] [Google Scholar]
- 381.Whimbey, E., J. A. Englund, and P. Ljungman. 1997. Community respiratory viral infections in the immunocompromised host. Proceedings of a symposium. Am. J. Med. 102:1-80. [Google Scholar]
- 382.White, L. A., C. Y. Freeman, B. D. Forrester, and W. A. Chappell. 1986. In vitro effect of ascorbic acid on infectivity of herpesviruses and paramyxoviruses. J. Clin. Microbiol. 24:527-531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 383.Wilks, D., and S. M. Burns. 1998. Myopericarditis associated with parainfluenza virus type 3 infection. Clin. Microbiol. Infect. Dis. 17:363-365. [DOI] [PubMed] [Google Scholar]
- 384.Wong, D. T., R. C. Welliver, K. R. Riddlesberger, M. S. Sun, and P. L. Ogra. 1982. Rapid diagnosis of parainfluenza virus infection in children. J. Clin. Microbiol. 16:164-167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 385.Wong, V. K., E. Steinberg, and A. Warford. 1988. Parainfluenza virus type 3 meningitis in an 11-month-old infant. Pediatr. Infect. Dis. J. 7:300-301. [DOI] [PubMed] [Google Scholar]
- 386.Woo, P. C. Y., K. Young, K. W. T. Tsang, C. G. C. Ooi, M. Peiris, and K. Y. Yuen. 2000. Adult croup: a rare but more severe condition. Respiration 67:684-688. [DOI] [PubMed] [Google Scholar]
- 387.Woods, G. T., M. E. Mansfield, G. Cmarik, and K. Sibinovic. 1967. Effect of vaccination against bovine myxovirus parainfluenza-3 before weaning and at the time of weaning on the natural history of respiratory disease in beef calves. Am. Rev. Respir. Dis. 95:278-284. [DOI] [PubMed] [Google Scholar]
- 388.Wright, P. 1984. Parainfluenza viruses, p. 299-310. In R. B. Belshe (ed.), Textbook of human virology. PSG Publishing, Littleton, Mass.
- 389.Wyde, P. R., M. N. Ambrose, H. L. Meyer, and A. E. Gilbert. 1990. Toxicity and antiviral activity of LY253963 against respiratory syncytial and parainfluenza type 3 viruses in tissue culture and in cotton rats. Antiviral Res. 14:237-247. [DOI] [PubMed] [Google Scholar]
- 390.Wyde, P. R., N. N. Ambrose, H. L. Meyer, C. L. Zolinski, and B. E. Gilbert. 1990. Evaluation of the toxicity and antiviral activity of carbocyclic 3-deazaadenosine against resiratory syncytial and parainfluenza type 3 viruses in tissue culture and in cotton rats. Antiviral Res. 14:215-225. [DOI] [PubMed] [Google Scholar]
- 391.Wyde, P. R., D. K. Moore, D. M. Pimentel, and H. A. Blough. 1995. Evaluation of the antiviral activity of N-(phosphonoacetyl)-l-aspartate against paramyxoviruses in tissue culture and against respiratory syncytial virus in cotton rats. Antiviral Res. 27:59-69. [DOI] [PubMed] [Google Scholar]
- 392.Yanagihara, R., and K. Mcintosh. 1980. Secretory immunological response in infants and children to parainfluenza virus types 1 and 2. Infect. Immun. 30:23-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 393.Yao, Q., and R. W. Compans. 2000. Filamentous particle formation by human parainfluenza virus type 2. J. Gen. Virol. 81:1305-1312. [DOI] [PubMed] [Google Scholar]
- 394.Yao, Q., and R. W. Compans. 1996. Peptides corresponding to the heptad repeat sequence of human parainfluenza virus fusion protein are potent inhibitors of virus infection. Virology 223:103-112. [DOI] [PubMed] [Google Scholar]
- 395.Yao, Q., X. Hu, and R. W. Compans. 1997. Association of the parainfluenza virus fusion and hemagglutinin-neuraminidase glycoproteins on cell surfaces. J. Virol. 71:650-656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 396.Yoshida, T., Y. Nakayama, T. Toyoda, K. Nishikawa, M. Hamaguchi, and R. Nagai. 1985. The polypeptides of human parainfluenza 1 (HA-2) virus and their antigenic relationships to those of Sendai virus (HVJ). Microbiol. Immunol. 29:577-582. [DOI] [PubMed] [Google Scholar]
- 397.Yuasa, T., M. Kawano, N. Tabata, et al. 1995. A cell fusion-inhibiting monoclonal antibody binds to the presumed stalk domain of the human parainfluenza type 2 virus hemagglutinin-neuraminidase protein. Virology 206:1117-1125. [DOI] [PubMed] [Google Scholar]
- 398.Yurlova, T. I., M. V. Sverkunova, V. A. Furaeva, V. P. Sukhinin, G. S. Shitikova, D. Fedova, and L. Kunzova. 1991. Studies of natural population variability of parainfluenza viruses during their epidemic circulation. Acta Virol. 35:64-70. [PubMed] [Google Scholar]
- 399.Zambon, M., T. Bull, C. J. Sadler, J. M. Goldman, and K. N. Ward. 1998. Molecular epidemiology of two consecutive outbreaks of parainfluenza 3 in a bone marrow transplant unit. J. Clin. Microbiol. 36:2289-2293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 400.Zhao, H., B. P. De, T. Das, and A. K. Banerjee. 1996. Inhibition of human parainfluenza virus-3 replication by interferon and human MxA. Virology 220:330-338. [DOI] [PubMed] [Google Scholar]
- 401.Zielinska-Jenczylik, J. 1972. The influence of environment on parainfluenza 3 virus anc its replication in tissue cultures. Arch. Immunol. Ther. Exp. 20:525-542. [PubMed] [Google Scholar]
- 402.Zollar, L. M., and M. A. Mufson. 1970. Acute parotitis associated with parainfluenza 3 virus infection. Am. J. Dis. Child. 199:147-148. [DOI] [PubMed] [Google Scholar]