Abstract
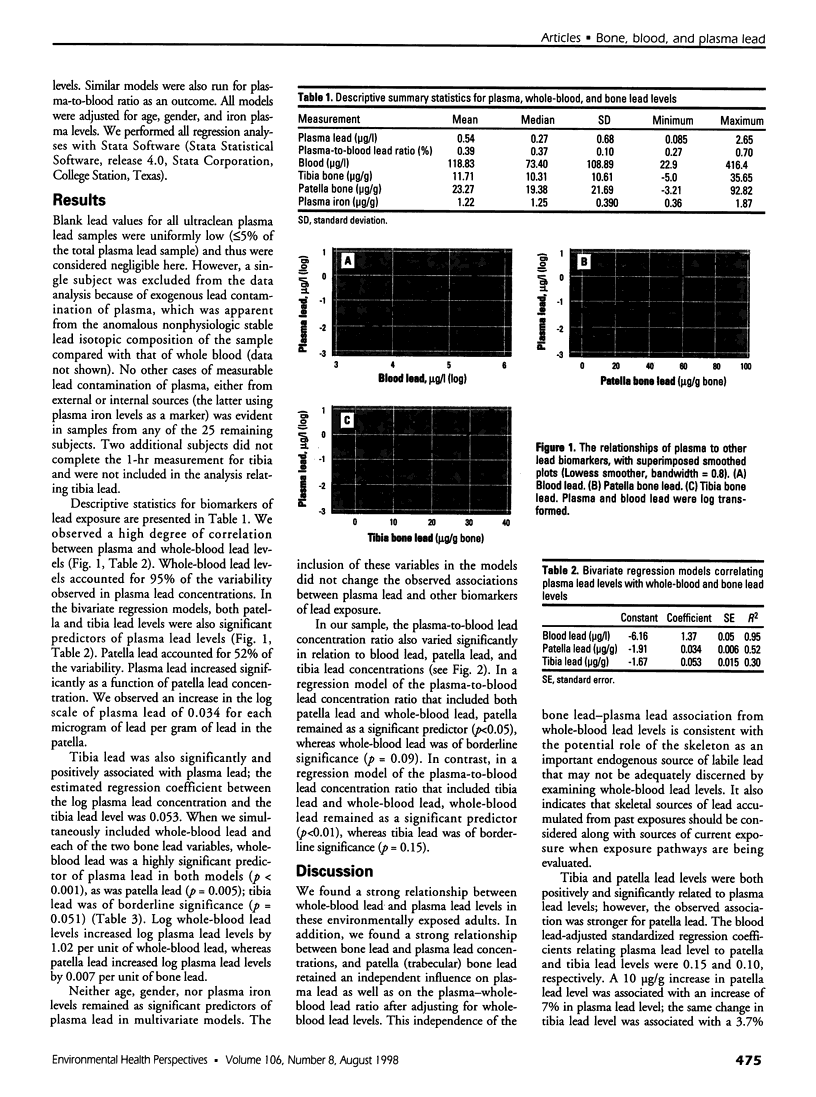
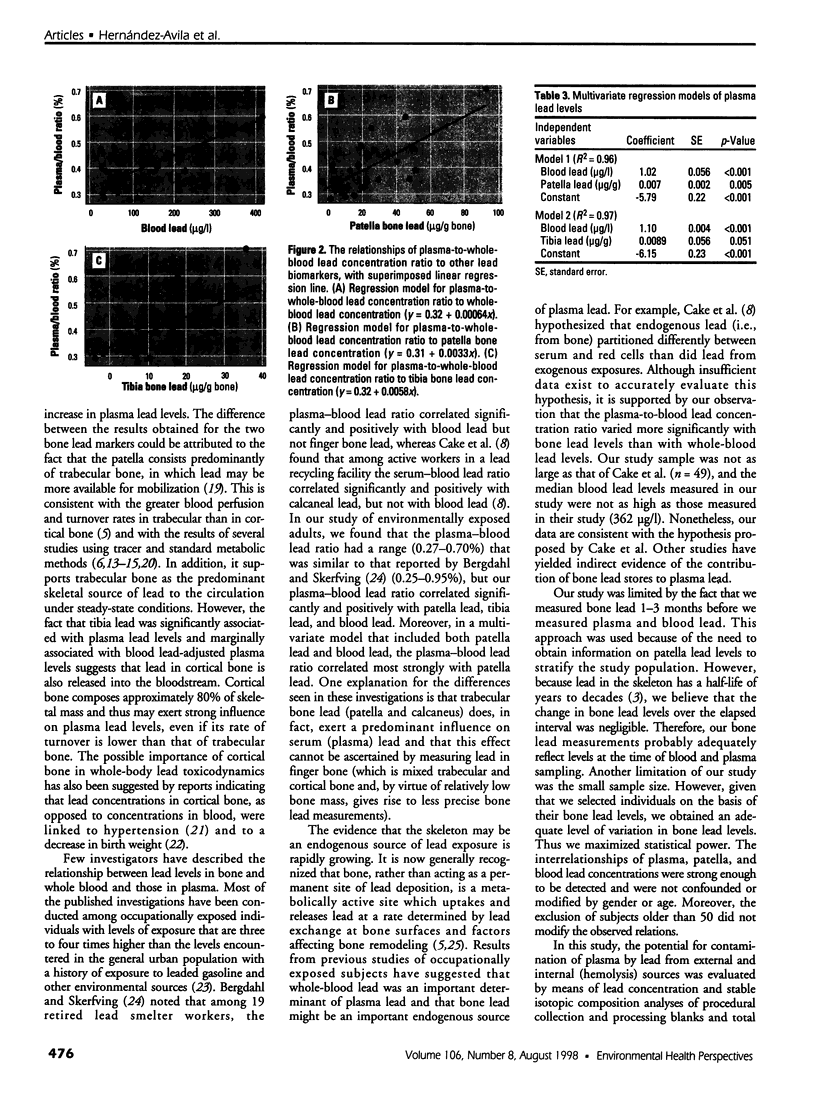
There is concern that previously accumulated bone lead stores may constitute an internal source of exposure, particularly during periods of increased bone mineral loss (e.g., pregnancy, lactation, and menopause). Furthermore, the contribution of lead mobilized from bone to plasma may not be adequately reflected by whole-blood lead levels. This possibility is especially alarming because plasma is the main circulatory compartment of lead that is available to cross cell membranes and deposit in soft tissues. We studied 26 residents of Mexico City who had no history of occupational lead exposure. Two samples of venous blood were collected from each individual. One sample was analyzed by inductively coupled plasma-magnetic sector mass spectrometry for whole-blood lead levels. The other sample was centrifuged to separate plasma, which was then isolated and analyzed for lead content by the same analytical technique. Bone lead levels in the tibia and patella were determined with a spot-source 109Cd K-X-ray fluorescence instrument. Mean lead concentrations were 0.54 microg/l in plasma, 119 microg/l in whole blood, and 23.27 and 11.71 microg/g bone mineral in the patella and tibia, respectively. The plasma-to-whole-blood lead concentration ratios ranged from 0.27% to 0.70%. Whole-blood lead level was highly correlated with plasma lead level and accounted for 95% of the variability of plasma lead concentrations. Patella and tibia lead levels were also highly correlated with plasma lead levels. The bivariate regression coefficients of patella and tibia on plasma lead were 0.034 (p<0. 001) and 0.053 (p<0.001), respectively. In a multivariate regression model of plasma lead levels that included whole-blood lead, patella lead level remained an independent predictor of plasma lead level (ss = 0.007, p<0.001). Our data suggest that although whole-blood lead levels are highly correlated with plasma lead levels, lead levels in bone (particularly trabecular bone) exert an additional independent influence on plasma lead levels. It will be important to determine whether the degree of this influence increases during times of heightened bone turnover (e.g., pregnancy and lactation).
Full text
PDF


Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Aro A. C., Todd A. C., Amarasiriwardena C., Hu H. Improvements in the calibration of 109Cd K x-ray fluorescence systems for measuring bone lead in vivo. Phys Med Biol. 1994 Dec;39(12):2263–2271. doi: 10.1088/0031-9155/39/12/009. [DOI] [PubMed] [Google Scholar]
- Barry P. S., Mossman D. B. Lead concentrations in human tissues. Br J Ind Med. 1970 Oct;27(4):339–351. doi: 10.1136/oem.27.4.339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bergdahl I. A., Skerfving S. Partition of circulating lead between plasma and red cells does not seem to be different for internal and external sources of lead. Am J Ind Med. 1997 Sep;32(3):317–318. doi: 10.1002/(sici)1097-0274(199709)32:3<317::aid-ajim22>3.0.co;2-x. [DOI] [PubMed] [Google Scholar]
- Brommage R., DeLuca H. F. Regulation of bone mineral loss during lactation. Am J Physiol. 1985 Feb;248(2 Pt 1):E182–E187. doi: 10.1152/ajpendo.1985.248.2.E182. [DOI] [PubMed] [Google Scholar]
- Cake K. M., Bowins R. J., Vaillancourt C., Gordon C. L., McNutt R. H., Laporte R., Webber C. E., Chettle D. R. Partition of circulating lead between serum and red cells is different for internal and external sources of lead. Am J Ind Med. 1996 May;29(5):440–445. doi: 10.1002/(SICI)1097-0274(199605)29:5<440::AID-AJIM2>3.0.CO;2-Q. [DOI] [PubMed] [Google Scholar]
- Cavalleri A., Minoia C., Ceroni M., Poloni M. Lead in cerebrospinal fluid and its relationship to plasma lead in humans. J Appl Toxicol. 1984 Apr;4(2):63–65. doi: 10.1002/jat.2550040202. [DOI] [PubMed] [Google Scholar]
- Cavalleri A., Minoia C. Lead level of whole blood and plasma in workers exposed to lead stearate. Scand J Work Environ Health. 1987 Jun;13(3):218–220. doi: 10.5271/sjweh.2060. [DOI] [PubMed] [Google Scholar]
- Everson J., Patterson C. C. "ULtra-clean" isotope diultion/mass spectrometic analyses for lead in human blood plasma indicated that most reported values are artificially high. Clin Chem. 1980 Oct;26(11):1603–1607. [PubMed] [Google Scholar]
- Flegal A. R., Smith D. R. Current needs for increased accuracy and precision in measurements of low levels of lead in blood. Environ Res. 1992 Aug;58(2):125–133. doi: 10.1016/s0013-9351(05)80209-9. [DOI] [PubMed] [Google Scholar]
- González-Cossío T., Peterson K. E., Sanín L. H., Fishbein E., Palazuelos E., Aro A., Hernández-Avila M., Hu H. Decrease in birth weight in relation to maternal bone-lead burden. Pediatrics. 1997 Nov;100(5):856–862. doi: 10.1542/peds.100.5.856. [DOI] [PubMed] [Google Scholar]
- Gulson B. L., Jameson C. W., Mahaffey K. R., Mizon K. J., Korsch M. J., Vimpani G. Pregnancy increases mobilization of lead from maternal skeleton. J Lab Clin Med. 1997 Jul;130(1):51–62. doi: 10.1016/s0022-2143(97)90058-5. [DOI] [PubMed] [Google Scholar]
- Gulson B. L., Mahaffey K. R., Mizon K. J., Korsch M. J., Cameron M. A., Vimpani G. Contribution of tissue lead to blood lead in adult female subjects based on stable lead isotope methods. J Lab Clin Med. 1995 Jun;125(6):703–712. [PubMed] [Google Scholar]
- Hernandez-Avila M., Gonzalez-Cossio T., Palazuelos E., Romieu I., Aro A., Fishbein E., Peterson K. E., Hu H. Dietary and environmental determinants of blood and bone lead levels in lactating postpartum women living in Mexico City. Environ Health Perspect. 1996 Oct;104(10):1076–1082. doi: 10.1289/ehp.961041076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu H., Aro A., Payton M., Korrick S., Sparrow D., Weiss S. T., Rotnitzky A. The relationship of bone and blood lead to hypertension. The Normative Aging Study. JAMA. 1996 Apr 17;275(15):1171–1176. [PubMed] [Google Scholar]
- Landrigan P. J., Todd A. C. Direct measurement of lead in bone. A promising biomarker. JAMA. 1994 Jan 19;271(3):239–240. [PubMed] [Google Scholar]
- Leggett R. W. An age-specific kinetic model of lead metabolism in humans. Environ Health Perspect. 1993 Dec;101(7):598–616. doi: 10.1289/ehp.93101598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manton W. I., Cook J. D. High accuracy (stable isotope dilution) measurements of lead in serum and cerebrospinal fluid. Br J Ind Med. 1984 Aug;41(3):313–319. doi: 10.1136/oem.41.3.313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manton W. I., Cook J. D. High accuracy (stable isotope dilution) measurements of lead in serum and cerebrospinal fluid. Br J Ind Med. 1984 Aug;41(3):313–319. doi: 10.1136/oem.41.3.313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Flaherty E. J. Physiologically based models for bone-seeking elements. I. Rat skeletal and bone growth. Toxicol Appl Pharmacol. 1991 Nov;111(2):299–312. doi: 10.1016/0041-008x(91)90032-a. [DOI] [PubMed] [Google Scholar]
- O'Flaherty E. J. Physiologically based models for bone-seeking elements. IV. Kinetics of lead disposition in humans. Toxicol Appl Pharmacol. 1993 Jan;118(1):16–29. doi: 10.1006/taap.1993.1004. [DOI] [PubMed] [Google Scholar]
- Rabinowitz M. B. Toxicokinetics of bone lead. Environ Health Perspect. 1991 Feb;91:33–37. doi: 10.1289/ehp.919133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rabinowitz M. B., Wetherill G. W., Kopple J. D. Kinetic analysis of lead metabolism in healthy humans. J Clin Invest. 1976 Aug;58(2):260–270. doi: 10.1172/JCI108467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanzgiri U. Y., Bruckner J. V. Effect of Emulphor, an emulsifier, on the pharmacokinetics and hepatotoxicity of oral carbon tetrachloride in the rat. Fundam Appl Toxicol. 1997 Mar;36(1):54–61. doi: 10.1006/faat.1997.2290. [DOI] [PubMed] [Google Scholar]
- Schütz A., Bergdahl I. A., Ekholm A., Skerfving S. Measurement by ICP-MS of lead in plasma and whole blood of lead workers and controls. Occup Environ Med. 1996 Nov;53(11):736–740. doi: 10.1136/oem.53.11.736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silbergeld E. K. Lead in bone: implications for toxicology during pregnancy and lactation. Environ Health Perspect. 1991 Feb;91:63–70. doi: 10.1289/ehp.919163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silbergeld E. K., Sauk J., Somerman M., Todd A., McNeill F., Fowler B., Fontaine A., van Buren J. Lead in bone: storage site, exposure source, and target organ. Neurotoxicology. 1993 Summer-Fall;14(2-3):225–236. [PubMed] [Google Scholar]
- Smith D. R., Ilustre R. P., Osterloh J. D. Methodological considerations for the accurate determination of lead in human plasma and serum. Am J Ind Med. 1998 May;33(5):430–438. doi: 10.1002/(sici)1097-0274(199805)33:5<430::aid-ajim2>3.0.co;2-w. [DOI] [PubMed] [Google Scholar]
- Smith D. R., Osterloh J. D., Flegal A. R. Use of endogenous, stable lead isotopes to determine release of lead from the skeleton. Environ Health Perspect. 1996 Jan;104(1):60–66. doi: 10.1289/ehp.9610460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- deSilva P. E. Determination of lead in plasma and studies on its relationship to lead in erythrocytes. Br J Ind Med. 1981 Aug;38(3):209–217. doi: 10.1136/oem.38.3.209. [DOI] [PMC free article] [PubMed] [Google Scholar]